Abstract
Background
Women live longer but experience greater disability than men. The reasons for this gender difference in disability are not well understood.
Objective
Our objectives were to determine if the higher prevalence of disability in women is due to greater incidence of disability, longer duration of disability, or both; and to identify factors that potentially explain these gender differences.
Methods
754 community-living persons aged 70 and older who were nondisabled (required no personal assistance) in four essential ADLs were assessed monthly for disability for up to 6 years. A multi-state extension of the proportional hazards model was used to determine the effects of gender on transitions between states of no disability, mild disability, severe disability and death, and to evaluate potential mediators of these effects.
Results
Women were more likely to make the transition from no disability to mild disability and less likely to make the transitions from mild to no disability and from both mild and severe disability to death. The gender difference in the transitions between no disability and mild disability was largely explained by differences in gait speed and physical activity, but gender difference in transitions to death persisted despite adjustment for multiple potential mediators.
Conclusion
The higher prevalence of disability in women versus men is due to a combination of higher incidence and longer duration, resulting from lower rates of recovery and mortality among disabled women.
Keywords: epidemiology, gender differences, activities of daily living, disability
INTRODUCTION
Across the lifespan, women live longer than men but experience higher rates of disability. Life expectancy for women exceeds that for men by 5.3 years at birth, 3.0 years at age 65, and 1.1 years at age 85.[1] In contrast, women experience greater disability than men of the same age across a wide range of functional measures, including both basic activities of daily living, such as bathing and dressing, and instrumental activities of daily living, such as housework and shopping.[2,3] The reasons for these differences are not fully understood. Previous studies of gender differences in disability incidence have produced contradictory results; some studies have shown higher incidence in women[4,5] while others have shown no gender difference.[6] We set out in the current study to determine the effects of gender on transitions between states of no disability, mild disability, severe disability, and death, and to evaluate potential mediators of these effects. Our objectives were 1) to determine if the higher prevalence of disability in women is due to greater incidence of disability, longer duration of disability, or both, and 2) to identify factors that potentially explain these gender differences.
METHODS
Study population
The study population was drawn from members of an ongoing longitudinal study of 754 community-dwelling persons, aged 70 years or older, who were initially nondisabled (i.e. required no personal assistance) in four basic activities of daily living (ADLs)—bathing, dressing, walking inside the house, and transferring from a chair. The assembly of the cohort from members of a large Medicare HMO, which took place between March 1998 and October 1999, has been described in detail elsewhere.[7] Persons who required greater than 10 seconds to walk back and forth over a 10-foot course as quickly as possible (using an assistive device if needed) were oversampled to ensure a sufficient number of participants at increased risk for ADL disability.[8] The participation rate was 75.2%. The study protocol was approved by the Yale Human Investigation Committee, and all participants gave informed consent.
Data collection
Participants underwent comprehensive in-home assessments at baseline and every 18 months and had monthly telephone interviews for six years. Potential mediators of the effect of gender on functional transitions were evaluated during the comprehensive assessments, which were completed by trained research nurses using standard instruments. In addition to timed gait, data were collected on demographic characteristics, chronic conditions, body mass index (from self-reported height and weight), cognitive status (Mini Mental State Examination),[9] depressive symptoms,[10] habitual physical activity (Physical Activity Scale for the Elderly),[11] and social support (Medical Outcomes Survey).[12] Participants were considered to have slow gait speed if they required greater than 10 seconds to walk back and forth over a 10-foot course (approximately 0.61 m/s ignoring the turn), and to have high depressive symptoms if they scored 16 or greater on the Center for Epidemiologic Studies Depression scale.[10]
During monthly telephone interviews, participants were assessed for disability in the four basic ADL tasks, using standard questions of the form “At the present time, do you need help from another person to [perform the activity]?” 14 Participants who needed help from another person or were unable to complete a task were considered disabled in that ADL. Participants who only required an assistive device were not considered disabled. Complete details regarding the monthly assessments of disability, including formal tests of reliability, have been provided elsewhere.[13,14]
Two hundred thirteen participants (28%) died after a median follow-up of 40 months, and 32 (4%) dropped out of the study after a median follow-up of 21 months. Almost nine percent of the monthly telephone interviews were completed by a proxy respondent. As described elsewhere,[13] the accuracy of these proxy reports for disability was excellent, with Kappa = 1.0.
Multi-state model of disability
Our multi-state model of disability includes four states: no disability, mild disability, severe disability, and death.[15] Transitions are possible among all of the non-decedent states, and from each non-decedent state to death. Disability in one or two ADLs was considered mild, while disability in three to four ADLs was considered severe.[16] An episode of mild or severe disability was defined as a period of one or more consecutive months in the state. We chose to focus on disability in basic ADLs because it is a key determinant of ability to stay in the community. Participants in the no disability category could still have significant functional limitations and difficulty with ADL tasks.
Statistical analysis
Data were available for 99.2% of the 45,481 monthly telephone interviews. Interval missing data on ADL disability were imputed using a method for multiple imputation that accounts for the correlation between repeated measures of disability, as suggested by Allison.[17]
We calculated the rates of each transition, defined as exits from a state per 1000 person-months in that state. Confidence intervals for the transition rates were calculated by bootstrapping, using sampling with replacement on the complete cohort. One thousand samples were drawn, and the 2.5th and 97.5th percentiles were used to form the confidence intervals.
We calculated the average duration of mild and severe disability episodes for each participant. Because the distribution was highly skewed with the majority of participants having short disability episodes, we compared these average durations for men versus women using the Wilcoxon rank-sum test.
We used an extension of the Cox proportional hazard model for repeated events to evaluate the effects of gender and potential mediating factors on the likelihood of subsequent functional transitions.[18] We employed a counting process which used the observed months of state entry and exit as the initiation and termination of the state [19] and estimated the effect of gender and other covariates on the individual transitions by including an interaction term of a dummy variable indicating the transition by each variable.[18] For each of the transitions, we exponentiated the coefficient for the interaction term to get the hazard ratio for each variable.[18] To account for the correlation among observations within participants, we used the robust sandwich variance estimators for standard errors of the coefficients.[20] For the multi-state proportional hazards models, all potential mediators except race were updated as indicated, using data from the comprehensive assessment immediately preceding entry into the state. The Cox model is fairly robust to the distribution of time to event and can be used for non-proportional hazards which may occur with time-dependent variables.[21] Because our models contained time-dependent variables and multiple transition events, standard methods are not available to check the proportional hazards assumption.
To serve as a mediator for the effect of gender on functional transitions, a factor must meet three statistical criteria: 1) be associated with gender; 2) be associated with functional transitions; and 3) decrease the magnitude of the coefficient for gender when included as a covariate in the statistical model.[22] Based on review of the literature to identify factors associated with disability,[8,23,24] recovery,[25-27] and mortality,[24,28] we considered the factors listed in Table 1 as potential mediators. We evaluated gender differences in the potential mediators using chi-square or t-tests as appropriate. We determined the association of the potential mediators that differed significantly by gender with functional transitions using the multi-state proportional hazards model described above. We then determined if including the potential mediators in the model altered the effect of gender on functional transitions.
Table 1.
Baseline characteristics of participants by gender.
| Characteristic | Women (n=487) | Men (n=267) | p-value* |
|---|---|---|---|
| Age, mean ± SD | 78 ± 5 | 79 ± 5 | .34 |
| White, n (%) | 439 (90) | 243 (91) | .70 |
| Living alone, n (%) | 239 (49) | 59 (22) | <.001 |
| Education (years), mean ± SD | 11.8 ± 2.8 | 12.3 ± 3.0 | 0.03 |
| Chronic conditions, mean ± SD† | 1.7 ± 1.2 | 1.7 ± 1.1 | .80 |
| Hypertension, n (%) | 272 (56) | 144 (54) | .61 |
| Arthritis, n (%) | 160 (33) | 67 (25) | .03 |
| Diabetes, n (%) | 84 (17) | 53 (20) | .38 |
| Prior myocardial infarction, n (%) | 69 (14) | 67 (25) | <.001 |
| Non-skin cancer, n (%) | 81 (17) | 43 (16) | .85 |
| Lung disease, n (%) | 53 (11) | 24 (9) | .41 |
| Stroke, n (%) | 38 (8) | 27 (10) | .28 |
| Heart failure, n (%) | 33 (7) | 16 (6) | .68 |
| Prior hip fracture, n (%) | 31 (6) | 3 (1) | <.001 |
| Body mass index, kg/m2, mean ± SD | 27 ± 6 | 26 ± 4 | .03 |
| Self-rated health fair or poor, n (%) | 142 (29) | 69 (26) | 0.33 |
| Cognitive status, mean ± SD‡ | 27 ± 2 | 26 ± 3 | .08 |
| High depressive symptoms, n (%) | 122 (25) | 34 (13) | <.001 |
| Social support, mean ± SD§ | 22 ± 6 | 23 ± 5 | .009 |
| Physical activity, mean ± SD∥ | 81 ± 52 | 107 ± 64 | <.001 |
| Slow gait speed, n (%) | 227 (47) | 95 (36) | .003 |
P-values for the comparison between women and men from chi-square tests for categorical variables and t-tests for continuous variables.
Number of nine self-reported, physician-diagnosed conditions, listed in the table in order of prevalence.
Assessed with the Folstein Mini-Mental State Exam, range 0 to 30 with higher scores representing better cognition.
Assessed with the MOS scale, range 0 to 28 with higher scores representing greater support.
Assessed with the Physical Activity Scale for the Elderly, range 0 to 360 with higher scores representing greater physical activity.
All analyses were performed using SAS version 9.1 (SAS Inc., Cary, NC), and all p-values are two-tailed.
RESULTS
The baseline characteristics of the study participants by gender are shown in Table 1. Women were more likely to live alone, have high depressive symptoms, and have slow gait speed. Women also had less education, higher body mass index, better cognitive status, less social support, and lower levels of physical activity. Although there was no gender difference in the number of chronic conditions, the prevalence of specific conditions did differ by gender, with women having higher prevalence of arthritis and hip fracture and lower prevalence of prior myocardial infarction.
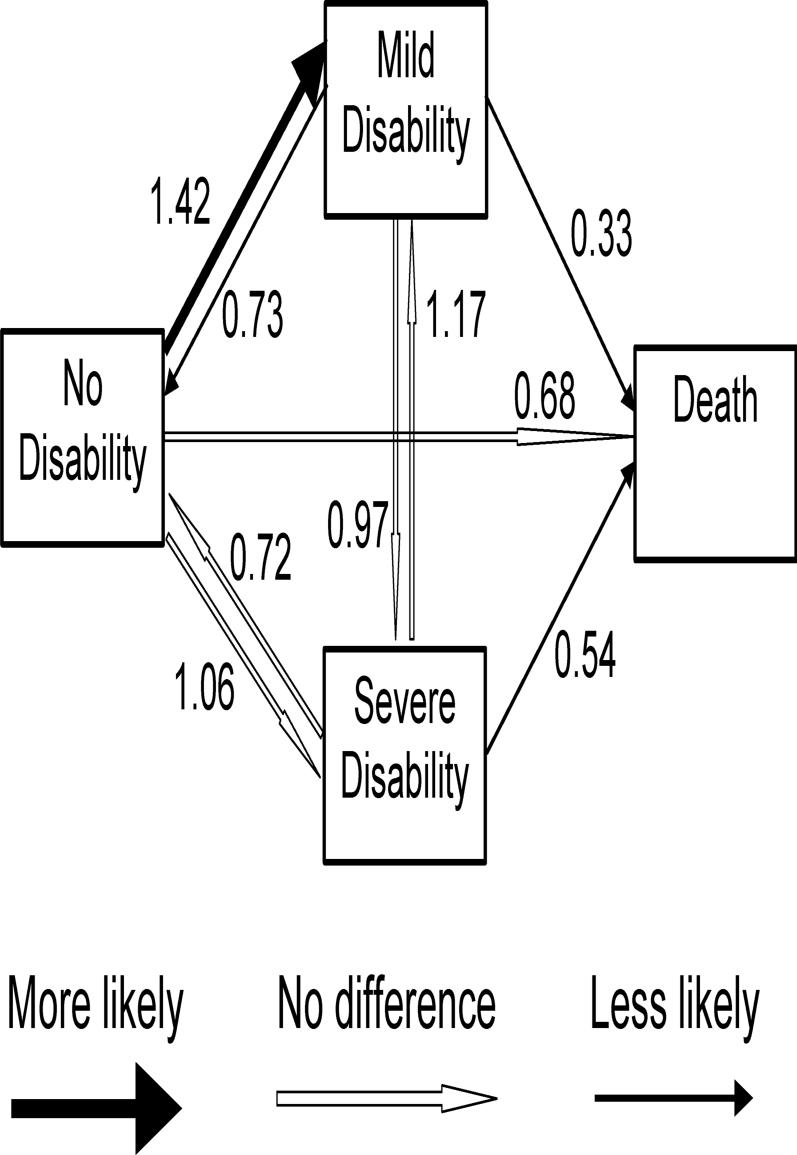
Over the follow-up period, women experienced a median (range) of 3 (0 to 36) transitions while men experienced 2 (0 to 27). The overall rate of transitions was 83 per 1000 person-months of follow-up; rates (95% confidence interval (CI)) were 91 (81−101) and 70 (59−81) for women and men, respectively. For both men and women, rates were highest for transitions from mild to no disability and from severe to mild disability, and lowest for transitions from no disability to death and mild disability to death (Table 2). As shown in Figure 1, women were more likely than men to make the transition from no disability to mild disability (hazard ratio (HR) 1.42, 95% CI 1.11−1.83), and less likely to make the transitions from mild disability to no disability (HR 0.73, 95% CI 0.57−0.94), mild disability to death (HR 0.33, 95% CI 0.17−0.62) and severe disability to death (HR 0.54, 95% CI 0.34−0.85).
Table 2.
Number and rates of transitions by gender.
| Women |
Men |
|||
|---|---|---|---|---|
| Transition | Number | Rate* | Number | Rate* |
| No disability to | ||||
| Mild disability | 921 | 37.3 | 362 | 26.4 |
| Severe disability | 162 | 6.6 | 85 | 6.2 |
| Death | 28 | 1.1 | 23 | 1.7 |
| Total person-months | 24,664 | 13,731 | ||
| Mild disability to | ||||
| No disability | 824 | 214.7 | 315 | 280.7 |
| Severe disability | 329 | 85.7 | 99 | 88.2 |
| Death | 21 | 5.5 | 18 | 16.0 |
| Total person-months | 3,838 | 1,122 | ||
| Severe disability to | ||||
| No disability | 66 | 41.8 | 29 | 53.1 |
| Mild disability | 312 | 197.5 | 93 | 170.3 |
| Death | 77 | 48.7 | 46 | 84.2 |
| Total person-months | 1,580 | 546 | ||
Rates per 1000 person-months in the initial state.
Figure 1.
Effect of gender on functional transitions. Boxes represent the four states and arrows represent the transitions between states. Values represent hazard ratios for the comparison of women versus men. The direction and statistical significance of the associations are shown schematically by the type of arrow (no difference represents p>0.05).
The median (intraquartile range (IQR), mean) values for participants’ average durations of mild disability episodes was 1.9 (1.0−3.1, 3.3) months for women and 1.4 (1.0−2.4, 2.4) months for men, p=0.003. For severe disability episodes, the median (IQR, mean) was 1.6 (1.0−3.0, 3.8) months for women and 1.0 (1.0−2.0, 2.6) months for men, p=0.03.
The effects on functional transitions of the factors meeting the first criterion for mediation (i.e. association with gender) are summarized in Table 3. Given the large number of comparisons, strong associations are denoted by p<0.01 or <0.001. Physical activity and slow gait were strongly associated with both gender and most functional transitions. Depressive symptoms, hip fracture, arthritis, and education were strongly associated with one or two transitions. Prior myocardial infarction, living alone, body mass index, and social support had relatively weak or no association with functional transitions.
Table 3.
Effects of potential mediating factors on functional transitions.*
| No Disability to |
Mild Disability to |
Severe Disability to |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mild Disability | Severe Disability | Death | No Disability | Severe Disability | Death | No Disability | Mild Disability | Death | |
| Physical activity | ↓↓↓ | ↓↓↓ | ↓ | ↑↑↑ | ↓↓↓ | ↑↑↑ | ↑↑↑ | ↑↑↑ | |
| Slow gait | ↑↑↑ | ↑↑↑ | ↓↓↓ | ↑↑ | ↓ | ↓↓ | |||
| High depressive symptoms | ↑↑↑ | ↑↑↑ | |||||||
| Prior hip fracture | ↑↑↑ | ↑ | ↑ | ↑ | |||||
| Arthritis | ↑↑↑ | ↑↑↑ | |||||||
| Greater education | ↓↓ | ↓↓ | |||||||
| Prior myocardial infarction | ↑ | ↑ | ↑ | ||||||
| Living alone | ↓ | ||||||||
| Body mass index | ↓ | ↑ | |||||||
| Social support | |||||||||
The direction of the arrows represents the direction of the effect: up represents increased likelihood of the transition and down, decreased likelihood. The number of arrows represents the statistical strength of the association (↑=p<0.05; ↑↑=p<0.01; ↑↑↑=p<0.001).
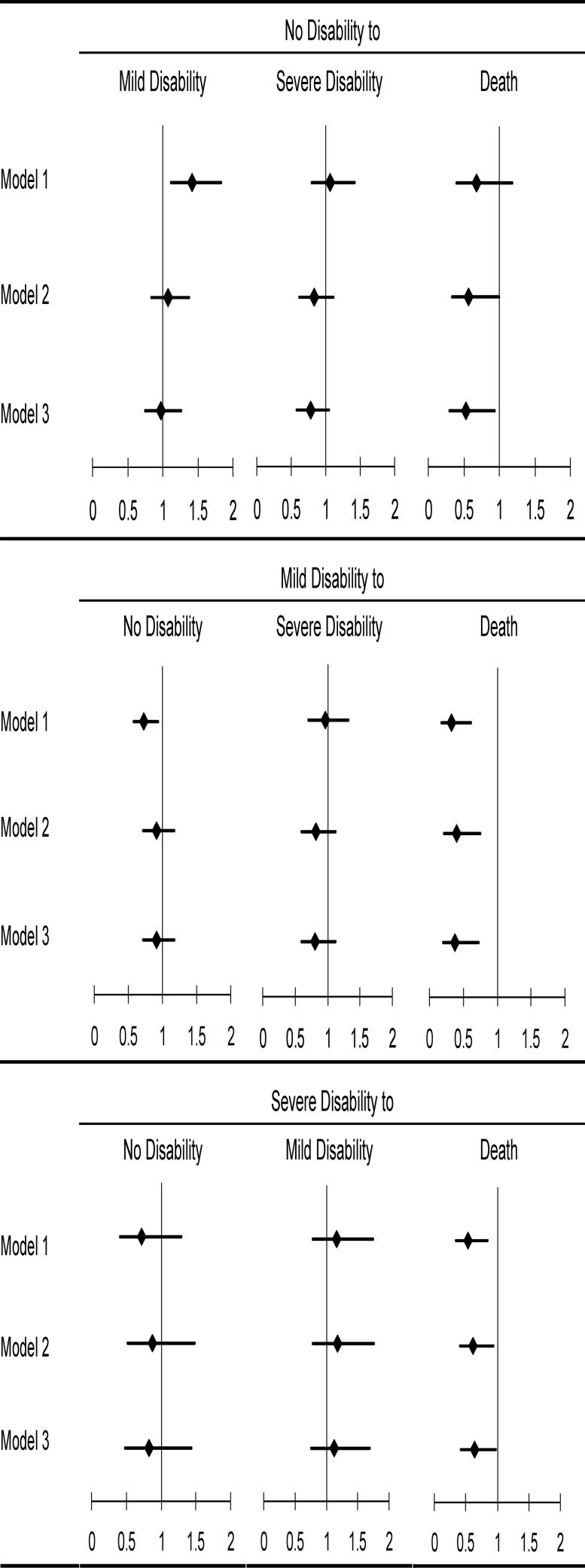
The unadjusted and adjusted associations between gender and each of the functional transitions are shown in Figure 2. We present effect of gender unadjusted (Model 1), adjusted for the two factors most strongly associated with both gender and transitions (Model 2), and adjusted for all factors associated with both gender and transitions (Model 3). In unadjusted analysis, women were more likely to make the transition from no disability to mild disability (HR 1.42, 95% CI 1.11−1.42), but after adjusting for physical activity and slow gait, the effect was no longer statistically significant (HR 1.07, 95% CI 0.83−1.38). Similarly, women were less likely to make the transition from mild disability to no disability in unadjusted analyses (HR 0.73, 95% CI 0.57−0.94), but after adjusting for physical activity and slow gait, this effect became non-significant (HR 0.91, 95% CI 0.71−1.17). Women were less likely to make the transitions from all states to death, although this effect was not statistically significant for the transition from no disability to death. Sequential adjustment for the potential mediators had relatively little effect on the magnitude of the corresponding hazard ratios.
Figure 2.
Unadjusted and adjusted effects of gender on functional transitions. Hazard ratios from multi-state proportional hazard models are presented, with the diamonds representing the point estimates and the lines the 95% confidence intervals. Model 1 is unadjusted. Model 2 is adjusted for physical activity and slow gait. Model 3 is adjusted for physical activity, slow gait, high depressive symptoms, hip fracture, arthritis, and education.
DISCUSSION
We found that the higher prevalence of disability in older women, as compared with men, is attributable to both a higher incidence and a longer duration of disability, resulting from lower rates of recovery and death among disabled older women. While the gender differences in transitions between no disability and mild disability were explained by gender differences in physical activity and gait speed, the differences in transitions to death were not explained by a large array of potential mediators.
Our results confirm those of numerous studies that have reported a higher prevalence of disability among older women than men,[29] although a study of older adults in Sweden found gender differences only among the oldest-old.[30] The literature is less consistent regarding gender differences in the incidence of disability. Our results are consistent with those from the Longitudinal Study of Aging (LSOA) ,[4,29] the National Health Interview Survey (NHIS),[29] and the Established Populations for Epidemiologic Studies of the Elderly (EPESE),[5] which also found that women had a higher incidence of ADL disability. In contrast, there were no gender differences in the incidence of disability in the Alameda County Study,[6] although, given the 6-year interval between assessments, the higher mortality rate for men may account for this finding. These gender differences in incidence rates may be specific to ADL and IADL[29] disability, as studies of mobility disability[31] and physical performance limitations[32] have found no gender differences in incidence rates.
Women in our study had not only a higher incidence of mild disability, but also a lower likelihood of recovery or death once disabled. Women in EPESE were also less likely to recover from ADL disability than men,[5] while women in LSOA were more likely to recover (although the effect was not statistically significant).[29] No gender differences were noted in recovery in several smaller studies with fewer transitions,[25,26,33,34] although a study of recovery from fall-related injuries reported that disabled women were significantly less likely to recover ADL function.[35] The lower risk of mortality among women, independent of disability, has been consistently found across numerous studies.[27,36,37]
Higher prevalence of disability in a population can be due to either higher incidence of disability, longer duration of disability, or a combination of the two. Our monthly assessments of disability allowed us to determine the duration of disability directly, in addition to estimating it with recovery and mortality rates. Women in our cohort experienced longer episodes of disability than men, confirming that the higher prevalence of disability is due to a combination of higher incidence and longer duration.
Numerous explanations have been offered for gender differences in disability prevalence and mortality, including differences in the number and type of chronic medical conditions, in physiologic parameters (for example, differences in hormones or body composition), in reporting of disability, and in health behaviors.[2,3] We found that gender differences in the rates of transitions between no disability and mild disability were explained by differences in gait speed and levels of habitual physical activity. Among LSOA participants, adjustment for age and chronic conditions (particularly cerebrovascular disease and vision impairment) accounted for gender differences in incident disability.[38] Peek and Coward[39] found that gender differences in ADL disability among older persons with arthritis were explained by age and socioeconomic status. Among older adults in the British General Household Survey, gender differences in disability incidence persisted after adjustment for age and socioeconomic status.[40] A study of alumni of the University of Pennsylvania found that gender differences in disability were attributable to differences in chronic health conditions, but not in age, sociodemographic factors, or health behaviors.[41]
In our cohort, women were consistently less likely to make transitions to death, although this difference was not statistically significant among participants with no disability, who had relatively low mortality rates. In a study that included 11 cohorts four developed countries, gender differences in mortality persisted after adjustment for age and a “frailty index,” that represented the proportion of potential symptoms, signs, laboratory abnormalities and disabilities.[42] Among older Japanese adults, substantial gender differences in mortality persisted after adjustment for age, demographic characteristics, social characteristics, health behaviors, health problems, and functional impairments.[43] Women in the Cardiovascular Health Study had lower mortality rates than men even after adjusting for sociodemographic factors, health behaviors, a variety of cardiac risk factors, markers of subclinical cardiovascular disease, functional status, and cognitive status.[28] Interestingly, we found that greater physical activity, which was strongly associated with gender, was associated with decreased mortality among the non-disabled but increased mortality among the disabled. Future research should investigate the reasons for this differential association of physical activity with death and its role in gender differences in death rates.
Our finding that gender differences in incidence and recovery from mild ADL disability were attributable to differences in gait speed and physical activity does not mean that other factors do not play an important role. Differences in gait speed and physical activity are likely intermediate steps in the causal pathway between gender and ADL disability. For example, high depressive symptoms, more common among women than men, were associated with the onset of disability. Depressive symptoms could serve as a mediator of the association between gender and disability incidence, either directly or through effects on physical activity or physical performance. Nevertheless, physical activity and gait speed are both potentially modifiable.[44,45] Interventions to promote physical activity have the potential to decrease disability among high risk older women, directly and through improvements in gait speed.
Several aspects of our analyses warrant comment. First, we have used a self-reported measure of disability. However, two studies comparing self-reported function with observed performance found no gender differences in the reporting of disability.[46,47] Second, we chose to use a categorical measure of disability rather than a continuous measure of functional status. Thus, participants with function near the threshold of requiring help from another person likely required smaller absolute changes in function to make transitions than those far above or below the threshold of disability. However, we feel that the threshold of requiring help from another person has critical implications for an older person's ability to live alone, the burden upon caregivers, and the need for long-term care. Third, because our participants were members of a single health plan in a small urban area, our results may not be generalizable to older persons in other settings. However, our population did reflect the demographic characteristics of persons aged 70 years or older in New Haven county, which are comparable to the United States as a whole.[48] Fourth, the majority of disability episodes in our cohort were brief. Nevertheless, our prior work has demonstrated that even short episodes of disability (i.e. 1−2 months) are strong, clinically relevant predictors of subsequent disability.[49] Fifth, nearly nine percent of our monthly interviews were completed by proxies. While we have demonstrated high reliability for our proxy assessments,[14] previous research suggests that proxies tend to overestimate functional deficits, although this is less true for basic ADLs than other, potentially more subjective measures such as instrumental ADLs, cognitive status, and affective function.[50] Finally, we do not have information on the use of rehabilitative services among our participants. Although use of rehabilitation services would be expected to affect functional transitions, previous research has suggested that rehabilitation utilization does not differ by gender after adjustment for health and functional status.[51]
In conclusion, gender differences in the prevalence of disability are due to a combination of higher incidence and longer duration of disability among older women. Gender differences in incidence of and recovery from mild ADL disability can be explained by differences in physical activity and gait speed, but mortality differences persist despite adjustment for multiple factors. Interventions to promote physical activity and improve gait speed have the potential to decrease disability among older women.
ACKNOWLEDGEMENTS
The authors thank Denise Shepard, Martha Oravetz, Shirley Hannan, Andrea Benjamin, Alice Kossack, Barbara Foster, Shari Lani, Alice Van Wie, and Amy Shelton for assistance with data collection; Dr. Evelyne Gahbauer for data management and programming; Wanda Carr and Geraldine Hawthorne for assistance with data entry and management; Peter Charpentier for development of the participant tracking system; and Joanne McGloin for leadership and advice as the Project Director. The work for this report was funded by Grants R01AG022993 and R37AG17560 from the National Institute on Aging. The study was conducted at Yale's Claude D. Pepper Older Americans Independence Center (P30AG21342). Dr. Hardy was supported by a training grant from the National Institute on Aging (T32AG1934) and a Pfizer/AGS Foundation for Health in Aging Junior Faculty Scholar award. She is currently supported by the Pittsburgh Pepper Center (P30AG024827) and the Hartford Center of Excellence in Geriatric Medicine. Dr. Gill is the recipient of a Midcareer Investigator Award in Patient-oriented Research (K24AG021507) from the National Institute on Aging.
REFERENCES
- 1.Hoyert DL, Kung HC, Smith BL. National Vital Statistics Reports; vol 53 no 15. National Center for Health Statistics; Hyattsville, Maryland: 2005. Deaths: Preliminary Data for 2003. [PubMed] [Google Scholar]
- 2.Newman AB, Brach JS. Gender gap in longevity and disability in older persons. Epidemiol Rev. 2001;23:343–350. doi: 10.1093/oxfordjournals.epirev.a000810. [DOI] [PubMed] [Google Scholar]
- 3.Leveille SG, Resnick HE, Balfour J. Gender differences in disability: evidence and underlying reasons. Aging Clin Exp Res. 2000;12:106–112. doi: 10.1007/BF03339897. [DOI] [PubMed] [Google Scholar]
- 4.Dunlop DD, Hughes SL, Manheim LM. Disability in activities of daily living: patterns of change and a hierarchy of disability. Am J Public Health. 1997;87:378–383. doi: 10.2105/ajph.87.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beckett LA, Brock DB, Lemke JH, Mendes de Leon CF, Guralnik JM, Fillenbaum GG, Branch LG, Wetle TT, Evans DA. Analysis of change in self-reported physical function among older persons in four population studies. Am J Epidemiol. 1996;143:766–778. doi: 10.1093/oxfordjournals.aje.a008814. [DOI] [PubMed] [Google Scholar]
- 6.Strawbridge WJ, Kaplan GA, Camacho T, Cohen RD. The dynamics of disability and functional change in an elderly cohort: results from the Alameda County Study. J Am Geriatr Soc. 1992;40:799–806. doi: 10.1111/j.1532-5415.1992.tb01852.x. [DOI] [PubMed] [Google Scholar]
- 7.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants and health care utilization. Ann Intern Med. 2001;135:313–321. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 8.Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: the role of physical performance. J Am Geriatr Soc. 1995;43:603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. Mini-mental state:” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CESD depression symptoms index. J Aging Health. 1993;5:179–193. doi: 10.1177/089826439300500202. [DOI] [PubMed] [Google Scholar]
- 11.Washburn RA, Smith KW, Jette AM, Janney CA. The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol. 1993;46:153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 12.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32:705–714. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- 13.Gill TM, Hardy SE, Williams CS. Underestimation of disability among community-living older persons. J Am Geriatr Soc. 2002;50:1492–1497. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 14.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 15.Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005;161:575–584. doi: 10.1093/aje/kwi083. [DOI] [PubMed] [Google Scholar]
- 16.Ferrucci L, Guralnik JM, Simonsick EM, Salive M, Corti MC, Langlois J. Progressive versus catastrophic disability: a longitudinal view of the disablement process. J Gerontol A Biol Sci Med Sci. 1996;51:M123–M130. doi: 10.1093/gerona/51a.3.m123. [DOI] [PubMed] [Google Scholar]
- 17.Allison PD. Missing Data. Sage Publications; Thousand Oaks: 2002. [Google Scholar]
- 18.Therneau TM, Grambsch PM. Modeling Survival Data: Extending the Cox Model. Springer-Verlag; New York: 2000. [Google Scholar]
- 19.Prentice RL, Williams BJ, Peterson AV. On the regression analysis of multivariate failure time data. Biometrika. 1981;68:373–379. [Google Scholar]
- 20.Lin DY, Wei LJ. The robust inference for the proportional hazards model. J Am Stat Assoc. 1989;84:1074–1078. [Google Scholar]
- 21.Allison PD. Survival analysis using SAS: A practical guide. SAS Institute Inc.; Cary, NC: 1995. [Google Scholar]
- 22.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158:848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 23.Stuck AE, Walthert JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999;48:445–469. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- 24.Miller ME, Rejeski WJ, Reboussin BA, Ten Have TR, Ettinger WH. Physical activity, functional limitations, and disability in older adults. J Am Geriatr Soc. 2000;48:1264–1272. doi: 10.1111/j.1532-5415.2000.tb02600.x. [DOI] [PubMed] [Google Scholar]
- 25.Gill TM, Robison JT, Tinetti ME. Predictors of recovery in activities of daily living among disabled older persons living in the community. J Gen Intern Med. 1997;12:757–762. doi: 10.1046/j.1525-1497.1997.07161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Predictors of functional recovery one year following hospital discharge for hip fracture: a prospective study. J Gerontol A Biol Sci Med Sci. 1990;45:M101–107. doi: 10.1093/geronj/45.3.m101. [DOI] [PubMed] [Google Scholar]
- 27.Mendes de Leon CF, Beckett LA, Fillenbaum GG, Brock DB, Branch LG, Evans DA, Berkman LF. Black-white differences in risk of becoming disabled and recovering from disability in old age: a longitudinal analysis of two EPESE populations. Am J Epidemiol. 1997;145:488–497. doi: 10.1093/oxfordjournals.aje.a009136. [DOI] [PubMed] [Google Scholar]
- 28.Fried LP, Kronmal RA, Newman AB, Bild DE, Mittelmark MB, Polak JF, Robbins JA, Gardin JM. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. JAMA. 1998;279:585–592. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 29.Crimmins EM, Saito Y, Reynolds SL. Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: the LSOA and the NHIS. J Gerontol B Psychol Sci Soc Sci. 1997;52:S59–71. doi: 10.1093/geronb/52b.2.s59. [DOI] [PubMed] [Google Scholar]
- 30.von Strauss E, Aguero-Torres H, Kareholt I, Winblad B, Fratiglioni L. Women are more disabled in basic activities of daily living than men only in very advanced ages: a study on disability, morbidity, and mortality from the Kungsholmen Project. J Clin Epidemiol. 2003;56:669–677. doi: 10.1016/s0895-4356(03)00089-1. [DOI] [PubMed] [Google Scholar]
- 31.Guralnik JM, LaCroix AZ, Abbott RD, Berkman LF, Satterfield S, Evans DA, Wallace RB. Maintaining mobility in late life. I. Demographic characteristics and chronic conditions. Am J Epidemiol. 1993;137:845–857. doi: 10.1093/oxfordjournals.aje.a116746. [DOI] [PubMed] [Google Scholar]
- 32.Oman D, Reed D, Ferrara A. Do elderly women have more physical disability than men do? Am J Epidemiol. 1999;150:834–842. doi: 10.1093/oxfordjournals.aje.a010088. [DOI] [PubMed] [Google Scholar]
- 33.Hansen K, Mahoney J, Palta M. Risk factors for lack of recovery of ADL independence after hospital discharge. J Am Geriatr Soc. 1999;47:360–365. doi: 10.1111/j.1532-5415.1999.tb03002.x. [DOI] [PubMed] [Google Scholar]
- 34.Michel JP, Hoffmeyer P, Klopfenstein C, Bruchez M, Grab B, d'Epinay CL. Prognosis of functional recovery 1 year after hip fracture: typical patient profiles through cluster analysis. J Gerontol A Biol Sci Med Sci. 2000;55:M508–M515. doi: 10.1093/gerona/55.9.m508. [DOI] [PubMed] [Google Scholar]
- 35.Kempen GI, Sanderman R, Scaf-Klomp W, Ormel J. The role of depressive symptoms in recovery from injuries to the extremities in older persons. A prospective study. Int J Geriatr Psychiatry. 2003;18:14–22. doi: 10.1002/gps.768. [DOI] [PubMed] [Google Scholar]
- 36.Mor V, Wilcox V, Rakowski W, Hiris J. Functional transitions among the elderly: patterns, predictors, and related hospital use. Am J Public Health. 1994;84:1274–1280. doi: 10.2105/ajph.84.8.1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leveille SG, Penninx BW, Melzer D, Izmirlian G, Guralnik JM. Sex differences in the prevalence of mobility disability in old age: the dynamics of incidence, recovery, and mortality. J Gerontol B Psychol Sci Soc Sci. 2000;55:S41–50. doi: 10.1093/geronb/55.1.s41. [DOI] [PubMed] [Google Scholar]
- 38.Dunlop DD, Manheim LM, Sohn MW, Liu X, Chang RW. Incidence of functional limitation in older adults: the impact of gender, race, and chronic conditions. Arch Phys Med Rehabil. 2002;83:964–971. doi: 10.1053/apmr.2002.32817. [DOI] [PubMed] [Google Scholar]
- 39.Peek MK, Coward RT. Gender differences in the risk of developing disability among older adults with arthritis. J Aging Health. 1999;11:131–150. doi: 10.1177/089826439901100201. [DOI] [PubMed] [Google Scholar]
- 40.Arber S, Cooper H. Gender differences in health in later life: the new paradox? Soc Sci Med. 1999;48:61–76. doi: 10.1016/s0277-9536(98)00289-5. [DOI] [PubMed] [Google Scholar]
- 41.Murtagh KNMA, Hubert HBP. Gender differences in physical disability among an elderly cohort. Am J Public Health. 2004;94:1406–1411. doi: 10.2105/ajph.94.8.1406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mitnitski A, Song X, Skoog I, Broe GA, Cox JL, Grunfeld E, Rockwood K. Relative fitness and frailty of elderly men and women in developed countries and their relationship with mortality. J Am Geriatr Soc. 2005;53:2184–2189. doi: 10.1111/j.1532-5415.2005.00506.x. [DOI] [PubMed] [Google Scholar]
- 43.Liang J, Bennett JM, Sugisawa H, Kobayashi E, Fukaya T. Gender differences in old age mortality: roles of health behavior and baseline health status. J Clin Epidemiol. 2003;56:572–582. doi: 10.1016/s0895-4356(03)00060-x. [DOI] [PubMed] [Google Scholar]
- 44.Lopopolo RB, Greco M, Sullivan D, Craik RL, Mangione KK. Effect of therapeutic exercise on gait speed in community-dwelling elderly people: a meta-analysis. Phys Ther. 2006;86:520–540. [PubMed] [Google Scholar]
- 45.King AC, Rejeski WJ, Buchner DM. Physical activity interventions targeting older adults. A critical review and recommendations. Am J Prev Med. 1998;15:316–333. doi: 10.1016/s0749-3797(98)00085-3. [DOI] [PubMed] [Google Scholar]
- 46.Melzer D, Lan TY, Tom BD, Deeg DJ, Guralnik JM. Variation in thresholds for reporting mobility disability between national population subgroups and studies. J Gerontol A Biol Sci Med Sci. 2004;59:1295–1303. doi: 10.1093/gerona/59.12.1295. [DOI] [PubMed] [Google Scholar]
- 47.Merrill SS, Seeman TE, Kasl SV, Berkman LF. Gender differences in the comparison of self-reported disability and performance measures. J Gerontol A Biol Sci Med Sci. 1997;52:M19–26. doi: 10.1093/gerona/52a.1.m19. [DOI] [PubMed] [Google Scholar]
- 48. American FactFinder. In, U. S. Census Bureau, 2003.
- 49.Gill TM, Kurland B. The prognostic effect of prior disability episodes among nondisabled community-living older persons. Am J Epidemiol. 2003;158:1090–1096. doi: 10.1093/aje/kwg237. [DOI] [PubMed] [Google Scholar]
- 50.Magaziner J, Zimmerman SI, Gruber-Baldini AL, Hebel JR, Fox KM. Proxy reporting in five areas of functional status. Comparison with self-reports and observations of performance. Am J Epidemiol. 1997;146:418–428. doi: 10.1093/oxfordjournals.aje.a009295. [DOI] [PubMed] [Google Scholar]
- 51.Kane RL, Finch M, Blewett L, Chen Q, Burns R, Moskowitz M. Use of post-hospital care by Medicare patients. J Am Geriatr Soc. 1996;44:242–250. doi: 10.1111/j.1532-5415.1996.tb00909.x. [DOI] [PubMed] [Google Scholar]