Abstract
BACKGROUND
This study was undertaken to determine the prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization (IVF) treatment.
METHODS
Participants were 1090 consecutive women and men, 545 couples, attending a fertility clinic in Sweden during a two-year period. The Primary Care Evaluation of Mental Disorders (PRIME-MD), based on the Diagnostic and Statistical Manual of Mental Disorders, 4th edn (DSM-IV), was used as the diagnostic tool for evaluating mood and anxiety disorders.
RESULTS
Overall, 862 (79.1%) subjects filled in the PRIME-MD patient questionnaire. Any psychiatric diagnosis was present in 30.8% of females and in 10.2% of males in the study sample. Any mood disorder was present in 26.2% of females and 9.2% of males. Major depression was the most common mood disorder, prevalent in 10.9% of females and 5.1% of males. Any anxiety disorder was encountered in 14.8% of females and 4.9% males. Only 21% of the subjects with a psychiatric disorder according to DSM-IV received some form of treatment.
CONCLUSIONS
Mood disorders are common in both women and men undergoing IVF treatment. The majority of subjects with a psychiatric disorder were undiagnosed and untreated.
Keywords: depression, anxiety, women, men, in vitro fertilization
Introduction
Infertility is a stressful life event and depressive symptoms are normal responses to the life crisis of the infertile couple. Grief reactions are common among infertile females and males, and the mourning process is considered important in order to resolve the infertility crisis (Williams and Zappert, 2006). However, in certain women and men these normal grief reactions are sustained and turn into pathological grief, which is largely consistent with the DSM-IV (Diagnostic and Statistical Manual of Mental Disorders, 4th edn) definition of major depression (Williams and Zappert, 2006).
Among infertile women ∼37% had depressive symptoms on the Beck Depression Inventory (BDI), which was twice as common as in the control group (Domar et al., 1992). At onset of IVF it has been estimated that 19.4% of infertile women had moderate to severe depressive symptoms, whereas 54% were mildly depressed according to the Zung Depression Scale (Demyttenaere et al., 1998). Prior to IVF, 11.6% of females reported depressive symptoms according to BDI, while the frequency was increased to 25.4% following failed IVF (Newton et al., 1990). According to the General Health Questionnaire, depressive symptoms were found in 33 and 43% of females prior to IVF and following IVF, respectively (Lok et al., 2002). Furthermore, anxiety symptoms in infertile women were encountered in 10.6% of women prior to IVF and in 14.2% of women after IVF using the State-Trait Anxiety Inventory (STAI) (Newton et al., 1990). Most studies report on depressive and anxiety symptoms among females, whereas few studies report on these symptoms among men undergoing IVF. The prevalence of depressive symptoms in infertile men according to the BDI varied between 3.5% prior to IVF and 8% after failed IVF (Newton et al., 1990). No elevated scores for anxiety symptoms using the STAI were reported among males in an assessment prior to IVF treatment (Slade et al., 1997).
The variability in assessments of depressive and anxiety symptoms in previous reports is largely determined by differences in the time points of the assessments (before, during and/or after IVF), and methodological issues such as the use of different standardized psychometric self-report instruments and the use of different threshold scores (Williams et al., 2007). One limitation of the use of self-report screening scales is that they can merely suggest the likelihood of a psychiatric disorder, whereas the use of diagnostic interviews can reveal a psychiatric diagnosis (Spitzer et al., 1994). Consequently, the prevalence of clinical psychiatric disorders, based on DSM-IV criteria, is largely unknown among unselected infertile couples. One previous study of Chinese women undergoing assisted reproductive treatment (ART) indicated that the prevalences of major depression and of generalized anxiety disorder (GAD) were 17 and 23.2%, respectively (Chen et al., 2004). A small study compared the prevalence of psychiatric disorders in infertile subjects specifically referred or not referred to psychosomatic care, and found prevalence rates of anxiety and/or depressive disorders in the latter group to be 30% in women and 16.6% in men (Guerra et al., 1998).
Major depression in the general population is two to three times as common in women as in men (Kessler, 2003). The 12-month prevalence of major depression in a Scandinavian population varies between 4.5–9.7% in women and 3–4.1% in men, whereas GAD is prevalent in 1.7–4.3% of women and 0.6–2% of men (Kringlen et al., 2001, 2006). The 12-month prevalence in the US population of any mood disorder is 14.1% in females and 8.5% in males, whereas any anxiety disorder is found among 22.6% of females and 11.8% of men (Kessler et al., 1994). Furthermore, there is a substantial comorbidity between anxiety and depression in both females and males (Kessler et al., 1994, 2005; Breslau et al., 1995). Depressive disorders are also associated with increased reporting of physical symptoms such as headache, fatigue, back pain and bowel complaints (Simon et al., 1999).
Given the lack of information concerning the prevalence of depressive disorders and anxiety disorders in infertile couples, this prospective study was undertaken in order to determine the prevalence of psychiatric disorders in infertile women and men undergoing in vitro fertilization (IVF).
Materials and Methods
Study population
From April 11, 2005, until April 13, 2007, all female and male partners in consecutive couples undergoing IVF or intracytoplasmic sperm injection (ICSI) treatment at the Centre of Reproduction, Uppsala University Hospital, Uppsala, Sweden, were approached concerning participation in the study. In Sweden, a total of 16 clinics were offering ART during the study period. Eight of these clinics are public and the others are private. The Centre of Reproduction at Uppsala University Hospital is public, and infertile couples are offered three IVF treatments free of charge. The waiting period for ART is approximately three months. Couples can seek medical care with or without referral. Couples who are referred for IVF treatment from areas outside Uppsala County are pretreated at the referring clinic. Pretreatment includes follicular stimulation with daily injections of gonadotrophins (in most cases recombinant FSH), either following down-regulation with a gonadotropin-releasing hormone (GnRH) analogue or in combination with a GnRH antagonist, until follicular maturation has been obtained, as monitored by regular examinations with transvaginal ultrasonography. Oocyte retrieval was performed 34–36 h after an injection of 10 000 IU of hCG. Subjects pretreated at their home clinic visit the Centre of Reproduction for the first time on the day of oocyte retrieval. The upper age limit for IVF at the Centre of Reproduction is 40 years for females and 55 years for males.
Study exclusion criteria were (i) inability to read and understand the questionnaire because of language difficulties and (ii) couples undergoing cycles with gamete donation, i.e. oocyte and sperm donation. Furthermore, subjects already evaluated at the time of an earlier IVF treatment during the study period were not approached to participate. Demographic data were collected by asking the subjects to fill in a separate questionnaire with questions on socioeconomic factors. The fertility history was collected from the subjects' medical reports after all subjects had participated in the study.
Psychiatric assessment
Diagnoses of psychiatric status were assessed using the PRIME-MD (Primary Care Evaluation of Mental Disorders) system, which was developed to screen, evaluate and diagnose mental disorders. Given its utility and ease of use, the PRIME-MD system was considered to be a suitable tool for assessing the prevalence of psychiatric disorders in this infertility setting. The PRIME-MD system was constructed to conform to DSM-IV criteria and has been validated for use in the primary care setting. Prior studies have indicated good agreement between PRIME-MD diagnoses and those of independent mental health professionals, with a sensitivity of 83%, a specificity of 88%, a positive predictive value of 80% and an overall accuracy of 86% (Spitzer et al., 1994). Furthermore, a self-administered version of PRIME-MD, the PRIME-MD Patient Health Questionnaire, has been validated for use in obstetric-gynaecologic patients (Spitzer et al., 2000). The original PRIME-MD system, which is fully described elsewhere (Spitzer et al., 1994), consists of two components: a one-page patient questionnaire (PQ) and a 12-page clinician evaluation guide (CEG), which is a structured interview guide to be followed when evaluating the responses on the PQ. The CEG contains modules for mood, anxiety, eating disorders, alcohol abuse, social phobia and obsessive-compulsive disorder. Only those modules that are indicated by the patient on the PQ are evaluated. A modified form of the PRIME-MD PQ, containing 24 questions relating to somatoform disorder, mood disorders, anxiety disorders and eating disorders, was used for this study. The PRIME-MD system evaluates the presence of 20 possible psychiatric disorders, of which 11 were considered in this study. Eight of these 11 correspond to the specific requirements of full DSM-IV diagnoses, where evaluation and treatment are recommended, such as: major depressive disorder, dysthymia, partial remission of major depressive disorder, GAD, panic disorder, obsessive-compulsive disorder, social phobia and bulimia nervosa. Three additional diagnoses are considered to be “subthreshold” diagnoses: minor depressive disorder, anxiety not otherwise specified (NOS) and eating disorder NOS. Subthreshold diagnoses have fewer symptoms than required for a specific DSM-IV diagnosis but are included in the study as they are also associated with considerable disability, as in the case of minor depressive disorders (Beekman et al., 1997). Bipolar disorder, alcohol abuse, somatoform disorders and rule-out diagnoses of mood and/or anxiety due to physical disorder, medication or drugs were not assessed.
Study design
On the day of oocyte retrieval, each eligible subject was asked for consent to participate in the study and to complete and return the PRIME-MD PQ. Along with the PQ they were asked to provide their name, date of birth, telephone number and a signed informed consent form allowing for a telephone interview. Subjects were considered to be screen-positive if a response to any key question indicated a psychiatric disorder. Screen-negative subjects were those whose responses on the PQ did not include items suggesting psychiatric symptoms. To confirm a diagnosis in screen-positive men and women, a telephone interview using a computerized version of the clinical evaluation guide was conducted. As most subjects provided their cell phone numbers, the female and male partners were interviewed separately, on different occasions. In only a few cases were both partners interviewed on the same occasion. In those cases partners were interviewed one after the other, starting with the one who answered the telephone. The telephone interview was conducted 21 days after screening, i.e. after the pregnancy test had been performed. At the time of the telephone interview, the interviewer had no knowledge of the subject or the subject's medical records (including fertility history and treatment outcome). In case of a PRIME-MD diagnosis, the subject was asked about current antidepressant drug therapy and/or psychotherapy (including therapy provided by sources outside the Centre of Reproduction), and any previous history of depression. All subjects with confirmed full DSM-IV diagnosis were offered referral to psychiatric specialist care. The telephone interviews were performed by two of the authors, both of whom had extensive clinical experience in counselling infertile couples and research experience in assessing psychological symptoms in IVF couples. The study was approved by the Ethics Committee, Uppsala University, Uppsala, Sweden.
Statistical analyses
Continuous variables were compared by the use of independent t-tests and are presented as mean ± SD. Frequencies were compared between groups using the chi-square test. All statistical analyses were performed with SPSS 14.0. A P-value <0.05 was considered significant. Demographic and fertility data were compared between subjects with a psychiatric disorder and subjects with no psychiatric disorder; the latter group consisted of screen-negative subjects and screen-positive subjects in whom no psychiatric diagnosis was established during the telephone interview.
Results
Study population
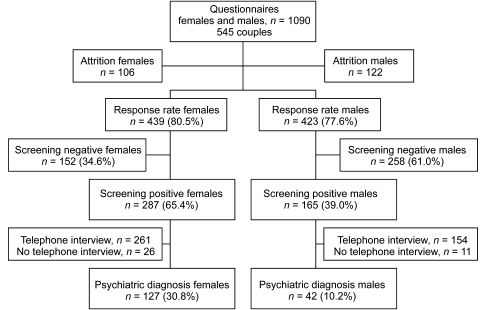
A total of 1102 patients were eligible for the study. Twelve patients were excluded because of language difficulties (inability to read/speak Swedish). Hence, a total of 1090 eligible women and men, 545 couples, were approached for participation in the study (Fig. 1). Of these, 85 females and 93 males (16.3%) did not return their questionnaires, and 50 subjects [21 females and 29 males (4.6%)] answered their questionnaires but were excluded as they did not consent to a follow-up telephone interview. Overall, 862 (79.1%) subjects filled out the PQ and consented to a telephone interview, and the response rates were 439 (80.5%) and 423 (77.6%) among women and men, respectively.
Figure 1:
The study population consisted of screen negative, screen positive and diagnosed subjects, n = 825 (413 females and 412 males).
Among subjects who filled out the PQ, 152 (34.6%) women and 258 (61.0%) men were screen-negative in that they did not trigger any of the key questions for psychiatric disorders. Overall, 452 (52.4%) women and men responded positively to one or more of the key questions for mental disorders and also consented to the follow-up telephone interview. Of these, 26 (5.9%) women and 11 (2.6%) men were screen-positive but could not be reached by telephone within the stipulated 21-day period. Hence, a telephone interview was conducted in 415 cases, and the study sample wherein a possible confirmation of a psychiatric diagnosis could be made consisted of 825 subjects (413 females and 412 males) (Fig. 1).
Pretreatment at referring clinics outside Uppsala county was done in 40.9% (n = 169 couples) of the study population. Demographic and fertility data are given in Table I for female and male subjects who agreed to participate and subjects who did not agree to participate in the study. ICSI treatment and previous IVF/ICSI treatment were more prevalent in men who declined to participate in the study than in men who participated in the study, P < 0.05. Demographic and fertility data are given in Table II for female and male subjects with or without psychiatric disorders. There were no differences between subjects who received a psychiatric diagnosis and the group with no psychiatric diagnosis when analyses were done separately in men and women. However, when both sexes were combined, smoking and unemployment were more common among subjects with a psychiatric diagnosis, P < 0.05.
Table I.
Demographic and fertility data for included women and men versus women and men not included in the study.
| Females, n = 545 |
Males, n = 545 |
|||
|---|---|---|---|---|
| Study group, n = 413 | Not includeda, n = 132 | Study group, n = 412 | Not includeda, n = 133 | |
| Age (years) | 32.9 ± 3.9 | 32.2 ± 4.9 | 34.7 ± 4.8 | 35.3 ± 3.5 |
| BMI (kg/m2) | 24.2 ± 3.9 | 24.3 ± 4.3 | 25.5 ± 3.4 | 26.5 ± 2.8 |
| Duration (months) | 38.6 ± 19.5 | 40.5 ± 23.6 | 38.2 ± 19.5 | 44.4 ± 21.0 |
| Infertility factors, n (%) | ||||
| Female | 122 (29.5) | 31 (23.5) | 123 (29.8) | 30 (22.6) |
| Male | 128 (31.0) | 48 (36.4) | 125 (30.3) | 51 (38.3) |
| Unexplained | 146 (35.4) | 37 (28.0) | 145 (35.2) | 38 (28.6) |
| Otherb | 17 (4.1) | 10 (7.6) | 19 (4.7) | 8 (6.0) |
| Previous pregnancy, n (%) | ||||
| No | 289 (70.0) | 94 (74.6) | ||
| Yes | 124 (30.0) | 32 (25.4) | ||
| Parity, n (%) | ||||
| Nullipara | 374 (90.6) | 118 (90.1) | ||
| Multipara | 39 (9.4) | 13 (9.9) | ||
| IVF | 253 (61.3) | 68 (51.5) | 256 (62.1) | 65 (48.9) |
| ICSI | 160 (38.7) | 58 (44.0) | 156 (37.9) | 62 (46.6)* |
| Previous IVF/ICSI, n (%) | ||||
| No | 308 (74.6) | 91 (68.9) | 312 (75.7) | 86 (64.7) |
| Yes | 105 (25.4) | 41 (31.1) | 100 (24.3) | 47 (35.3)* |
aMissing data; not included n = 6 (4.5%); bother causes or not evaluated. *Significantly different from included males, P < 0.05. BMI, body mass index.
Table II.
Demographic and fertility data for infertile women and men with or without psychiatric diagnosis.
| Female subjects, n = 413 |
Male subjects, n = 412 |
|||
|---|---|---|---|---|
| Psychiatric diagnosis, n = 127 | No psychiatric diagnosis, n = 286 | Psychiatric diagnosis, n = 42 | No psychiatric diagnosis, n = 370 | |
| Age, years | 32.7 ± 4.1 | 32.9 ± 3.7 | 35.5 ± 4.5 | 34.6 ± 4.8 |
| BMI, kg/m2 | 24.7 ± 4.1 | 23.9 ± 4.1 | 26.1 ± 4.4 | 25.5 ± 3.3 |
| Smokers, n (%) | 10 (7.9) | 13 (4.5) | 4 (9.5) | 15 (4.1) |
| Snuff taking status, n (%) | 3 (2.4) | 11 (3.8) | 10 (23.8) | 101 (27.4) |
| University/College, n (%) | 64 (50.4) | 156 (54.5) | 17 (40.5) | 165 (44.6) |
| High school education, n (%) | 63 (49.6) | 130 (45.5) | 25 (59.5) | 205 (55.4) |
| Employee/studenta, n (%)b | 75 (59.1) | 165 (57.7) | 19 (45.2) | 222 (60.0) |
| Unemployeda, n (%)b | 8 (6.3) | 8 (2.8) | 3 (7.1) | 10 (2.7) |
| Duration, months | 38.3 ± 20.2 | 38.8 ± 19.2 | 39.7 ± 20.6 | 38.0 ± 19.4 |
| Infertility factors, n (%) | ||||
| Female | 41 (32.3) | 81 (28.3) | 8 (19.0) | 115 (31.1) |
| Male | 42 (33.0) | 86 (30.1) | 14 (33.3) | 111 (30.0) |
| Unexplained | 41 (32.3) | 105 (36.7) | 17 (40.5) | 128 (34.6) |
| Otherb | 3 (2.4) | 14 (4.9) | 3 (7.1) | 16 (4.3) |
| Previous pregnancy, n (%) | ||||
| No | 81 (63.8) | 208 (72.7) | ||
| Yes | 46 (36.2) | 78 (27.3) | ||
| Parity, n (%) | ||||
| Nullipara | 113 (89.0) | 261 (91.3) | ||
| Multipara | 14 (11.0) | 25 (8.7) | ||
| IVF | 78 (61.4) | 175 (61.2) | 23 (54.8) | 253 (63.0) |
| ICSI | 49 (38.6) | 111 (38.8) | 19 (45.2) | 137 (37.0) |
| Previous IVF/ICSI, n (%) | ||||
| No | 92 (72.4) | 215 (75.2) | 27 (64.3) | 285 (77.0) |
| Yes | 35 (27.6) | 71 (24.8) | 15 (35.7) | 85 (33.0) |
No significant differences were found between the groups. amissing data; a total of 157 (38.0%) females and 158 (38.3%) males (This question was included later in the study); bother causes or not evaluated. BMI, body mass index.
Prevalence of psychiatric disorders
Of the 413 women in the study sample, 127 (30.8%) had one or more psychiatric diagnoses. The corresponding figure for the 412 males was 42 (10.2%). The difference between females and males was significant (P < 0.001). Prevalence rates of psychiatric disorders detected by PRIME-MD in the total sample of women and men are summarized in Table III. In 18 cases (4.4%), both the female and the male within the couple had any psychiatric diagnosis. Comorbidity was common among the 127 females with a psychiatric diagnosis; 46 (36.2%) females had two diagnoses, and 10 (7.9%) females had three or more diagnoses. Of the 42 males with a psychiatric diagnosis, 16 (38.1%) had two diagnoses, and five (11.9%) had three or more diagnoses.
Table III.
Prevalence of psychiatric disorders detected by PRIME-MD.
| Psychiatric disorder | Females, n = 413 (%) | Males, n = 412 (%) |
|---|---|---|
| Any psychiatric diagnosis | 127 (30.8) | 42 (10.2) |
| Threshold diagnoses (full DSM-IV diagnoses)a | 81 (19.6) | 30 (7.3) |
| Subthreshold diagnosesb | 46 (11.1) | 12 (2.9) |
| Any mood disorderc | 108 (26.2) | 38 (9.2) |
| Major depressive disorder | 45 (10.9) | 21 (5.1) |
| Dysthymia | 6 (1.4) | 1 (0.2) |
| Partial remission of major depressive disorder | 25 (6.1) | 8 (1.9) |
| Minor depressive disorder | 35 (8.5) | 9 (2.2) |
| Any anxiety disorderc | 61 (14.8) | 20 (4.9) |
| Anxiety NOS | 46 (11.1) | 16 (3.9) |
| Generalized anxiety disorder | 7 (1.7) | 3 (0.7) |
| Panic disorder | 5 (1.2) | 2 (0.5) |
| Obsessive-compulsive disorder | 8 (1.9) | 1 (0.2) |
| Social phobia | 5 (1.2) | 2 (0.4) |
| Eating disorder NOS | 1 (0.2) | 0 |
aFull DSM-IV diagnoses; major depressive disorder, dysthymia, partial remission of major depressive disorder, generalized anxiety disorder, panic disorder, obsessive-compulsive disorder, social phobia and bulimia nervosa; bsubthreshold diagnoses; minor depressive disorder, anxiety NOS and eating disorder NOS; csubjects can have one or more psychiatric diagnoses within any mood and/or any anxiety disorders.
Full DSM-IV diagnoses (i.e. diagnoses with specific requirements in the DSM-IV, subthreshold diagnoses not included) were present in 111 subjects, 81 (19.6%) women and 30 men (7.3%), while 46 (11.1%) women and 12 (2.9%) men had a subthreshold diagnosis. Among subjects with a full DSM-IV diagnosis only 23 subjects (20.7%) were receiving some form of treatment for their psychiatric condition. Twenty (18%) subjects received some form of psychotherapy, and seven (6.3%) subjects had been prescribed antidepressant treatment with or without psychotherapy. In the study sample, i.e. not only among those who received a psychiatric diagnosis, a total of 89 (10.8%) subjects received counselling during investigation and/or IVF treatment. A total of 78 (46.2%) women and men with psychiatric disorders reported a previous history of depression. Of the subjects with full DSM-IV diagnoses, 49 (60.5%) of the females and 16 (53.3%) of the males reported a previous history of depression. Recurrent thoughts of death were reported by 8 (10.5%) females and 5 (16.7%) males diagnosed with a major depression and of these, 7 females and 3 males were undergoing their first IVF.
Physical symptoms were more common among females and males with a psychiatric diagnosis than in the group without a diagnosis. The frequencies of reported physical symptoms are presented in Table IV. The most common symptoms among females with a psychiatric diagnosis were fatigue, headache, nausea and abdominal pain, whereas fatigue and insomnia were the physical symptoms most commonly reported by men with a psychiatric diagnosis.
Table IV.
Frequency of physical symptoms by prevalence of any PRIME-MD diagnosis.
| Female subjects, n = 413 (%) |
Male subjects, n = 412 |
|||
|---|---|---|---|---|
| Psychiatric diagnosis, n = 127 | No psychiatric diagnosis, n = 286 | Psychiatric diagnosis, n = 42 | No psychiatric diagnosis, n = 370 | |
| Fatigue | 111 (87.4)*** | 171 (59.6) | 31 (73.8)*** | 91 (25.0) |
| Headache | 83 (65.4) ** | 134 (46.9) | 17 (40.5)** | 60 (16.3) |
| Nausea | 71 (55.9)*** | 100 (34.8) | 13 (31.0)** | 39 (10.7) |
| Abdominal pain | 69 (55.6)*** | 96 (33.6) | 8 (19.0)** | 21 (5.7) |
| Bowel complaints | 60 (48.0)*** | 84 (29.3) | 12 (28.6)** | 37 (10.2) |
| Insomnia | 55 (44.0)*** | 58 (20.2) | 23 (54.8)*** | 53 (14.6) |
| Dysmenorrhea | 50 (40.0)* | 88 (30.9) | ||
| Dizziness | 43 (33.9)*** | 49 (17.1) | 9 (21.4)*** | 10 (2.7) |
| Back pain | 38 (29.9)* | 56 (19.5) | 11 (26.2)* | 50 (13.6) |
| Joint or limb pain | 27 (21.8)* | 38 (13.3) | 10 (23.8) ns | 50 (13.7) |
| Palpitations | 21 (16.8)* | 27 (9.4) | 1 (2.4) ns | 7 (1.9) |
| Chest pain | 21 (16.5)** | 17 (5.9) | 6 (14.3)** | 10 (2.7) |
| Sexual problems | 19 (15.1)* | 23 (8.1) | 0 | 5 (1.4) |
| Dyspnea | 7 (5.6)* | 5 (1.7) | 5 (12.2)** | 4 (1.1) |
| Fainting | 4 (3.1)* | 2 (0.7) | 2 (4.8)* | 1 (0.3) |
Not all subjects answered all questions. *P < 0.05 compared with respective control group, chi-square test; **P < 0.01 compared with respective control group, chi-square test; ***P < 0.001 compared with respective control group, chi-square test. ns, not significant.
Discussion
To our knowledge, this is the first study to describe the prevalence of psychiatric disorders in both women and men undergoing IVF treatment. Approximately 30% of the infertile women and 10% of the infertile men in the present study fulfilled criteria for a depressive and/or anxiety disorder, including subthreshold diagnoses. Depressive disorders were more common than in the general population, whereas prevalence rates of anxiety disorder were similar (Kessler et al., 1994; Kringlen et al., 2001, 2006). Major depression was the most prevalent psychiatric disorder in both women and men. The majority of subjects with a psychiatric disorder were undiagnosed and untreated for that disorder, which is also in accordance with what is found in the general population (Kessler et al., 1994; Lépine et al., 1997).
One explanation as to why depression is not always recognized in the infertility setting could be that infertile couples are reluctant to report depressive symptoms to the IVF team. The couples are eager to appear well adjusted, presumably because they fear that IVF treatment will be denied or postponed if psychiatric problems are revealed (Demyttenaere et al., 1998; Williams and Zappert, 2006). Furthermore, the couples tend to have unrealistically high expectations of a successful outcome after the first treatment (Slade et al., 1997; Hammarberg et al., 2001), and their positive attitudes before the start of the first treatment may disguise an ongoing depression.
A major finding of this study was that only a small proportion of those identified with a psychiatric disorder received ongoing treatment. The first choice for treatment of depression in infertile females is psychotherapy rather than pharmacotherapy to avoid both interference with the woman's attempt to conceive and medication interactions (Williams and Zappert, 2006). Cognitive Behavioural Therapy (CBT) has been shown to reduce mental stress in females undergoing IVF (Facchinetti et al. 2004) and has also been demonstrated to be an efficient treatment for depression in other populations (Feldman, 2007). However, availability of CBT may vary considerably between clinics and this may explain why treatment may not be accessible to all patients. Psychotherapy in the form of counselling was received by one-fifth of the subjects with a psychiatric diagnosis and by one in ten of all subjects in this study. This is surprisingly few, as all couples are informed about and offered counselling at their initial visit to the clinic. However, similar low rates of counselling have previously been reported by Boivin et al. (1999), who found that only 11% of females and males received counselling while attending an infertility clinic. Thus, an important task for the IVF team would be not only to identify females and males with depression, but also to assure that adequate treatment is initiated. Furthermore, as waiting times for IVF are being reduced, it is important to offer treatment not only before the first IVF treatment, but also in between treatments.
Somewhat surprisingly, fertility factors such as age of the female, duration of infertility, infertility diagnosis and numbers of previous IVF/ICSI treatments were not associated with psychiatric disorders in this study population. Other factors such as personality traits and coping strategies are presumably more important predictors of psychiatric morbidity than fertility history. This assumption is also corroborated by findings in burn survivors, where personality and coping strategies have been shown to more reliably predict psychological outcome than the severity of the burn injury (Kildal et al., 2004; Willebrand et al., 2004).
On the other hand, fertility factors appear to have influenced readiness to participate in the study. Men who declined to participate more often had male factor infertility than men who participated. As men with male factor infertility have been shown to be more mentally distressed than men in couples with other causes of infertility (Laffont and Edelmann, 1994), it is plausible that the prevalence of psychiatric disorders among male participants in this study has been underestimated.
The prevalence rates of depression and anxiety disorders in the current study may be the result of difficulties involved in dealing with infertility and undergoing IVF treatment. However, it must be emphasized that the prevalence rates of depression and/or anxiety disorders among infertile females in the present study are similar to those found in unselected gynaecological outpatients, where 30.5% suffered from any psychiatric disorder and 10% had a major depression (Sundstrom et al., 2001). Hence, depression and/or anxiety disorders do not appear to be more common in infertile females compared with patients in gynaecologic practice. However the prevalence rates of depression and/or anxiety disorder are higher in infertile females when compared with a population-based study of pregnant women in the second trimester. The prevalence of any depressive disorder in pregnant women was 11.6%, and the prevalence of any anxiety disorder was 6.6% (Andersson et al., 2003).
Comorbidity was often encountered in the present study, where one-third of both females and males with psychiatric disorders had two or more diagnoses. These results are in agreement with previous studies suggesting that depression and anxiety often co-exist (Breslau et al., 1995). Likewise, in analogy with prior findings, physical symptoms were significantly more frequent among females and males with a psychiatric diagnosis than in subjects without a diagnosis (Kroenke and Spitzer, 1998; Sundstrom et al., 2001; Andersson et al., 2003).
There are several limitations to the present study. First, psychiatric diagnoses were based on the use of a screening questionnaire followed by a structured psychiatric interview conducted by telephone. The PRIME-MD interview was primarily designed to be used by primary care physicians, but the use of telephone interviews in this situation is less well studied. However, telephone interviews are commonly used in large-scale population-based studies of psychiatric disorders because of their demonstrated comparability with face-to-face research interviews (Wells et al., 1988; Spitzer et al., 1994; Evans et al., 2004). For this reason, and because almost half of the subjects were living outside of Uppsala, telephone interviews were used for the psychiatric assessments in the present study.
Another limitation of the current study was the choice of time points for assessment of psychiatric disorders, with initial screening on the day of oocyte retrieval and telephone interviews after the IVF treatment. As the subjects completed the first assessment (screening) on the day of oocyte retrieval, it may have been difficult to clearly distinguish previous anxiety from anxiety caused by anticipation of oocyte retrieval procedures and concerns about the outcome of the treatment. However, these time points were chosen because it has previously been shown that anxiety symptoms peak on the day of oocyte retrieval (Boivin et al., 1998), and by screening subjects on this day we increased the sensitivity of the method. Also, by conducting the second assessment three weeks later, after the pregnancy test, it can be assumed that treatment-related transient changes in depressive and anxiety symptoms have declined, thus reducing the risk of false-positive psychiatric diagnoses. Another reason for our choice of time points for the assessments was that almost half of the women were pretreated at referring clinics and did not visit our clinic until the day of oocyte retrieval. If psychiatric assessments had been carried out earlier during the course of IVF treatment, we would have been able to recruit only a very limited population. Undergoing IVF treatment can be extremely stressful for the couple, and psychiatric assessments, whether performed before, during or after treatment, will result in various types of biases that might influence the results.
Other limitations of the study were that substance-related disorders were not assessed and that women and men with language difficulties were excluded. It can be assumed that subjects with foreign backgrounds more often suffer from depression, as heightened depression scores have been reported previously in this group (Beutel et al., 1999).
The limitations of the current study also indicate the need for additional studies of the prevalence of psychiatric disorders in subjects undergoing IVF treatment. For example, in this study three out of four couples were undergoing their first IVF and fewer than one in ten was undergoing their third IVF. It is unclear whether prevalence of psychiatric disorders after the third and for most couples the last IVF is different from subjects who undergo their first IVF. Furthermore, most couples are lost to follow-up after the last IVF, and even less is known about the psychological health of subjects who never conceive following IVF (Hammarberg et al., 2001).
In conclusion, this study suggests that mood disorders, and in particular major depression, are common in infertile women and men undergoing IVF treatment. The majority of subjects with a psychiatric disorder were undiagnosed and untreated. It is an important task for the IVF team not only to identify females and males with depression, but also to assure that adequate treatment is initiated.
Funding
This study was supported by research grants from the Swedish Research Council project K2008-54X-20 642-01-3, the Swedish Council for Working Life and Social Research, project 2007–1955, the Family Planning Foundation and the Foundation of Caring Sciences, Uppsala University.
Acknowledgements
We are grateful to Pernilla Olsson and Sofi Karlberg at the Center of Reproduction for their invaluable help in distributing the questionnaires.
References
- Andersson L, Sundstrom-Poromaa I, Bixo M, Wulff M, Bondestam K, Åstrom M. Point prevalence of psychiatric disorders during the second trimester of pregnancy: a population-based study. Am J Obstet Gynecol. 2003;189:148–154. doi: 10.1067/mob.2003.336. [DOI] [PubMed] [Google Scholar]
- Beekman AT, Deeg DJ, Braam AW, Smit JH, Van Tilburg W. Consequences of major and minor depression in later life: a study of disability, well-being and service utilization. Psychol Med. 1997;27:1397–1409. doi: 10.1017/s0033291797005734. [DOI] [PubMed] [Google Scholar]
- Beutel M, Kupfer J, Kirchmeyer P, Kehde S, Kohn FM, Schroeder-Printzen I, Gips H, Herrero HJ, Weidner W. Treatment-related stresses and depression in couples undergoing assisted reproductive treatment by IVF or ICSI. Andrologia. 1999;31:27–35. [PubMed] [Google Scholar]
- Boivin J, Andersson L, Skoog-Svanberg A, Hjelmstedet A, Collins A, Bergh T. Psychological reactions during in-vitro fertilization: similar response pattern in husbands and wives. Hum Reprod. 1998;11:3262–3267. doi: 10.1093/humrep/13.11.3262. [DOI] [PubMed] [Google Scholar]
- Boivin J, Scanlan LC, Walker SM. Why are infertile patients not using psychosocial counselling? Hum Reprod. 1999;14:1384–1391. doi: 10.1093/humrep/14.5.1384. [DOI] [PubMed] [Google Scholar]
- Breslau N, Schultz L, Peterson E. Sex differences in depression: a role for preexisting anxiety. Psychiatry Res. 1995;58:1–12. doi: 10.1016/0165-1781(95)02765-o. [DOI] [PubMed] [Google Scholar]
- Chen TH, Chang SP, Tsai CF, Juang KD. Prevalence of depressive and anxiety disorders in an assisted reproductive technique clinic. Hum Reprod. 2004;19:2313–2318. doi: 10.1093/humrep/deh414. [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, Bonte L, Gheldof M, Vervaeke M, Meuleman C, Vanderschuerem D, d'Hooghe T. Coping style and depression level influence outcome in in vitro fertilization. Fertil Steril. 1998;69:1026–1033. doi: 10.1016/s0015-0282(98)00089-2. [DOI] [PubMed] [Google Scholar]
- Domar AD, Broome A, Zuttermeister PC, Seibel M, Friedman R. The prevalence and predictability of depression in infertile women. Fertil Steril. 1992;58:1158–1163. [PubMed] [Google Scholar]
- Evans M, Kessler D, Lewis G, Peters TJ, Sharp D. Assessing mental health in primary care research using standardized scales: can it be carried out over the telephone? Psychol Med. 2004;34:157–162. doi: 10.1017/s0033291703008055. [DOI] [PubMed] [Google Scholar]
- Facchinetti F, Tarabusi M, Volpe A. Cognitive-behavioral treatment decreases cardiovascular and neuroendocrine reaction to stress in women waiting for assisted reproduction. Psychoneuroendocrinology. 2004;29:162–173. doi: 10.1016/s0306-4530(02)00170-1. [DOI] [PubMed] [Google Scholar]
- Feldman G. Cognitive and behavioral therapies for depression: overview, new directions, and practical recommendations for dissemination. Psychiatr Clin North Am. 2007;30:29–50. doi: 10.1016/j.psc.2006.12.001. [DOI] [PubMed] [Google Scholar]
- Guerra D, Llobera A, Veiga A, Barri PN. Psychiatric morbidity in couples attending a fertility service. Hum Reprod. 1998;13:1733–1736. doi: 10.1093/humrep/13.6.1733. [DOI] [PubMed] [Google Scholar]
- Hammarberg K, Astbury J, Baker HWG. Women's experience of IVF: a follow-up study. Hum Reprod. 2001;16:374–383. doi: 10.1093/humrep/16.2.374. [DOI] [PubMed] [Google Scholar]
- Kessler RC. Epidemiology of women and depression. J Affect Disord. 2003;74:5–13. doi: 10.1016/s0165-0327(02)00426-3. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kildal M, Willebrand M, Andersson G, Gerdin B, Ekselius L. Personality characteristics and perceived health problems after burn injury. J Burn Care Rehabil. 2004;25:228–235. doi: 10.1097/01.bcr.0000126295.84815.df. [DOI] [PubMed] [Google Scholar]
- Kringlen E, Torgersen S, Cramer V. A Norwegian psychiatric epidemiological study. Am J Psychiatry. 2001;158:1091–1098. doi: 10.1176/appi.ajp.158.7.1091. [DOI] [PubMed] [Google Scholar]
- Kringlen E, Torgersen S, Cramer V. Mental illness in a rural area: a Norwegian psychiatric epidemiological study. Soc Psychiatry Psychiatr Epidemiol. 2006;41:713–719. doi: 10.1007/s00127-006-0080-0. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. Gender differences in the reporting of physical and somatoform symptoms. Psychosom Med. 1998;60:150–155. doi: 10.1097/00006842-199803000-00006. [DOI] [PubMed] [Google Scholar]
- Laffont I, Edelmann RJ. Psychological aspects of in vitro fertilization: a gender comparison. J Psychosom Obstet Gynaecol. 1994;15:85–92. doi: 10.3109/01674829409025633. [DOI] [PubMed] [Google Scholar]
- Lépine J-P, Gastpar M, Mendlewicz J, Tylee A. Depression in the community: the first pan-European study DEPRES (Depression Research in European Society) Int Clin Psychopharm. 1997;12:19–29. [PubMed] [Google Scholar]
- Lok IH, Lee DT, Cheung LP, Chung WS, Lo WK, Haines CJ. Psychiatric morbidity amongst infertile Chinese women undergoing treatment with assisted reproductive technology and the impact of treatment failure. Gynecol Obstet Invest. 2002;53:195–199. doi: 10.1159/000064560. [DOI] [PubMed] [Google Scholar]
- Newton CR, Hearn MT, Yuzpe AA. Psychological assessment and follow-up after in vitro fertilization: assessing the impact of failure. Fertil Steril. 1990;54:879–886. doi: 10.1016/s0015-0282(16)53950-8. [DOI] [PubMed] [Google Scholar]
- Simon GE, von Korff M, Piccinelli M, Fullerton C, Ormel J. An international study of the relation between somatic symptoms and depression. N Engl J Med. 1999;341:1329–1335. doi: 10.1056/NEJM199910283411801. [DOI] [PubMed] [Google Scholar]
- Slade P, Emery J, Lieberman BA. A prospective, longitudinal study of emotions and relationships in in-vitro fertilization treatment. Hum Reprod. 1997;12:183–190. doi: 10.1093/humrep/12.1.183. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV, 3rd, Hahn SR, Brody D, Johnson JG. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA. 1994;272:1749–1756. [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000;183:759–769. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- Sundstrom IM, Bixo M, Bjorn I, Astrom M. Prevalence of psychiatric disorders in gynecologic outpatients. Am J Obstet Gynecol. 2001;184:8–13. doi: 10.1067/mob.2001.108072. [DOI] [PubMed] [Google Scholar]
- Wells KB, Burnam MA, Leake B, Robin LN. Agreement between face-to-face and telephone-administered versions of the depression section of the NIMH diagnostic interview schedule. J Psychiat Res. 1988;22:207–220. doi: 10.1016/0022-3956(88)90006-4. [DOI] [PubMed] [Google Scholar]
- Willebrand M, Andersson G, Ekselius L. Prediction of psychological health after an accidental burn. J Trauma. 2004;57:367–374. doi: 10.1097/01.ta.0000078697.69530.0e. [DOI] [PubMed] [Google Scholar]
- Williams KE, Zappert LN. Psychopathology and psychopharmacology in the infertile patient. In: Covington SN, Hammer Burns L, editors. Infertility Counselling. New York, USA: Cambridge University Press; 2006. pp. 97–116. [Google Scholar]
- Williams KE, Marsh WK, Rasgon NL. Mood disorders and fertility in women: a critical review of the literature and implications for future research. Hum Reprod Update. 2007;13:607–616. doi: 10.1093/humupd/dmm019. [DOI] [PubMed] [Google Scholar]