Abstract
Objective
To estimate racial differences in mortality at 30 days and up to 2 years following a hospital admission for the elderly with common medical conditions.
Data Sources
The Medicare Provider Analysis and Review File and the VA Patient Treatment File from 1998 to 2002 were used to extract patients 65 or older admitted with a principal diagnosis of acute myocardial infarction, stroke, hip fracture, gastrointestinal bleeding, congestive heart failure, or pneumonia.
Study Design
A retrospective analysis of risk-adjusted mortality after hospital admission for blacks and whites by medical condition and in different hospital settings.
Principal Findings
Black Medicare patients had consistently lower adjusted 30-day mortality than white Medicare patients, but the initial survival advantage observed among blacks dissipated beyond 30 days and reversed by 2 years. For VA hospitalizations similar patterns were observed, but the initial survival advantage for blacks dissipated at a slower rate.
Conclusions
Racial disparities in health are more likely to be generated in the posthospital phase of the process of care delivery rather than during the hospital stay. The slower rate of increase in relative mortality among black VA patients suggests an integrated health care delivery system like the VA may attenuate racial disparities in health.
Keywords: Hospital mortality, racial disparities
The 2001 Institute of Medicine report Unequal Treatment declared definitively that quality of health care is often very different between white and minority populations in the United States (Smedley, Stith, and Nelson 2003). Among hospitalized patients, blacks have lower treatment rates than whites across a wide range of conditions, with particularly strong evidence for cardiovascular diseases (Meehan et al. 1995; O'Conner et al. 1999; Shen, Wan, and Perlin 2001; Barnato et al. 2005; Cromwell et al. 2005). To better understand where in the process of care delivery health differences might arise, we described mortality differences by race following hospital admissions.
National efforts to improve hospital care, such as public reporting of standard quality indicators, provide an expectation of health improvements for those populations most vulnerable to poor quality of care such as hospitalized elderly and minority populations (Jha et al. 2005). However, how care received in hospitals or after discharge might relate to observed racial disparities in health is poorly understood (National Center for Health Statistics 2005). Examining how outcomes differ for blacks and whites over longer periods after hospital admission can help us assess at what point in the care process racial differences in observed outcomes are most pronounced. This will allow for more targeted and effective health care system reforms addressing health care disparities.
We estimated racial differences in 30-day mortality following a hospital admission for the medical conditions for which this outcome is endorsed by the Agency for Healthcare Research and Quality (AHRQ) as a hospital quality indicator: acute myocardial infarction (AMI), stroke, hip fracture, congestive heart failure (CHF), gastrointestinal bleeding (GI Bleed), and pneumonia. We also examined changes in mortality up to 2 years after admission to determine the trajectory of the difference in mortality for blacks and whites. Finally, to suggest how health systems may influence patterns of racial differences in mortality, we compared the patterns of racial differences in short- and long-term mortality following hospitalizations occurring in private acute-care hospitals with those occurring in the integrated and federally financed Veterans Administration health care system (VA).
METHODS
The institutional review boards of the Philadelphia VA Medical Center and the University of Pennsylvania approved this study.
Data
Our primary data source was the 1998–2002 Medicare Provider Analysis and Review (MedPAR) File, which contains administrative information for every hospital discharge within the Medicare fee-for-service program. Death dates through 2004 were calculated by linking MedPAR to the Medicare denominator file through 2004 (Centers for Medicare and Medicaid Services 2005). Our secondary data source was the VA Patient Treatment File (PTF) for 1998–2002, which contains the same administrative information as MedPAR but for admissions to VA hospitals. Death dates through 2004 were linked to the PTF from the VA Beneficiary Identification Record Locator System Death File. We used the 2000 U.S. Census data for zipcode-level socioeconomic characteristics of the patients (Geronimus, Bound, and Neidert 1996; Geronimus and Bound 1998; Fiscella and Franks 2001).
Patient Population
We studied mortality outcomes for patients admitted with a principal diagnosis of AMI, stroke, hip fracture, CHF, GI Bleed, or pneumonia. We chose these conditions because their 30-day mortality rates are recommended as quality indicators by AHRQ (2002), mostly because high mortality for these conditions may be associated with deficiencies in the quality of care (Meehan et al. 1995; Rockall et al. 1995; Office of Statewide Health Planning and Development 1996). The principal diagnosis codes used to identify these six conditions are given in the Supplementary Appendix.
We restricted our MedPAR sample to index admissions to an acute care hospital by excluding all subsequent admissions for the same condition within 2 years. We included only black and white elderly Medicare enrollees. Finally, we excluded all patients who resided outside the United States. For VA hospitalizations identified within the PTF, we applied the same exclusion criteria, but also excluded women because they make up only 2 percent of study hospitalizations in the VA.
Variables
Our primary outcome was mortality after a hospital admission. For all mortality outcomes, 30-day mortality, 2-year mortality, and the mortality curves, the time at risk began from the date of admission. Our primary independent variable was black versus white race. We examined three sets of adjustment variables: health risk (age, sex, year of discharge, comorbid conditions), socioeconomic status (median household income, percentage of population with college degrees, and urbanicity of patient's zipcode of residence), and location of care (hospital fixed effects). We used the approach of Elixhauser and colleagues to define the comorbid conditions (Elixhauser et al. 1998; Stukenborg, Wagner, and Connors 2001; Southern, Quan, Ghali, 2004). We included hospital fixed effects to reduce potential bias in within-hospital comparisons of outcomes by accounting for cross-sectional differences between hospitals that affect outcomes. To avoid problems with model convergence, we combined the smallest 20 percent of all hospitals within each state into a single code indicating small hospitals within state, resulting in 3,369 unique hospital indicators.
Analysis
All analyses were conducted separately for each of the six conditions. We analyzed 30-day mortality rates in the Medicare sample as a function of race (black versus white) and the adjustment variables by using an ordinary least-squares linear probability model (Davies et al. 2001). By estimating adjusted marginal probabilities and their p -values rather than odds ratios, this model facilitates exposition and avoids misinterpretation of odds ratios as relative risks when the underlying event is not rare. To understand the influence of health risk, socioeconomic status, and hospital on the association between race and 30-day mortality, we added each type of adjustment variable in sequence and recorded the mortality difference by race for each model. We tested the sensitivity of all results using nonlinear logistic regression models rather than linear regression models.
We conducted two additional analyses to understand short- and long-term mortality patterns. First, in the Medicare sample we estimated detailed race-specific adjusted mortality curves for each condition by estimating a discrete time–mortality curve, with mortality measured at 2, 15, 30, 60, 90, 180, 365, and 730 days, by using ordinary least-squares with controls for health risk, socioeconomic status, and hospital fixed effects. Second, to enable statistical comparisons between short- and long-term mortality, we dichotomized the 2-year mortality curve into only two discrete periods: the short-term postadmission period (within 30 days) and the long-term postadmission period (from 30 to 730 days). Discrete-time logistic regression was used because survival analysis was not computationally feasible given the size of the dataset. This discrete time model of mortality was estimated at 30 and 730 days for the Medicare and VA samples. The comparative analysis was limited to men in both the Medicare and VA samples so that the Medicare and VA samples did not differ on this dimension.
We used SAS software, version 8.2 (SAS Institute Inc., Cary, NC), for data analysis and model estimation.
RESULTS
There were 8,802,808 identified Medicare hospitalizations between 1998 and 2002. Black patients made up 9.1 percent of the sample (Table 1). They were younger than whites (mean age, 77.9 compared with 80.2 years). Blacks had higher rates of admission for stroke, CHF, and GI Bleed but comparable rates of admission for the other conditions. Blacks lived in zipcodes with lower average educational attainment and median household income. They also had more comorbid conditions on average, with a higher prevalence of conditions such as hypertension and diabetes and a lower prevalence of chronic obstructive pulmonary disease. We identified 155,529 VA hospitalizations between 1998 and 2002. Blacks comprised 17.8 percent of this sample (see Supplementary Appendix). The differences in patient characteristics by race in the VA sample were very similar to those found in the Medicare sample.
Table 1.
Baseline Characterstics by Race for Medicare Hospitalization
| Black | White | |
|---|---|---|
| N (%) | 804,745 (9.1) | 7,998,063 (90.9) |
| Conditions, n (%) | ||
| Pneumonia | 212,583 (26.4) | 2,246,623 (28.1) |
| CHF | 204,609 (25.4) | 1,651,235 (20.6) |
| Gl Bleed | 110,147 (13.7) | 889,139 (11.1) |
| Hip fracture | 36,533 (4.5) | 932,954 (11.7) |
| Stroke | 153,161 (19.0) | 1,143,074 (14.3) |
| AMI | 87,712 (10.9) | 1,135,038 (14.2) |
| Age (SD) | 77.9 (8.4) | 80.2 (7.9) |
| Gender (%) | ||
| Male | 38.5 | 41.9 |
| Socieconomic status, mean (SD) | ||
| Percent with college degree | 11.9 (9.0) | 23.3 (14.7) |
| Percent urban | 80.7 (31.7) | 72.5 (35.0) |
| Median household income ($) | 19,893.8 (12865.2) | 28,228.8 (10752.7) |
| Number of comorbidities | 2.4 | 2.1 |
| Comorbidities (%) | ||
| Congestive heart failure | 14.6 | 15.4 |
| Hypertension, complicated | 59.5 | 45.3 |
| Valvular disease | 3.5 | 5.5 |
| Pulmonary circulation disorders | 0.8 | 0.9 |
| Peripheral vascular disorder | 6.7 | 6.2 |
| Paralysis | 3.3 | 2.1 |
| Neurological disorders | 8.3 | 8.4 |
| Chronic pulmonary disease | 21.1 | 27.6 |
| Diabetes | 27.9 | 18.9 |
| Diabetes with chronic complications | 6.2 | 3.4 |
| Hypothyroidism | 4.4 | 9.6 |
| Renal failure | 10.9 | 5.0 |
| Liver disease | 0.8 | 0.8 |
| Chronic peptic ulcer | 0.1 | 0.1 |
| HIV and AIDS | 0.0 | 0.0 |
| Lymphoma | 0.7 | 0.8 |
| Metastatic cancer | 1.9 | 1.7 |
| Solid tumor without metastasis | 2.8 | 2.4 |
| Rheumatoid arthritis/collagen vascular disease | 1.7 | 2.3 |
| Coagulation deficiency | 2.7 | 2.5 |
| Obesity | 3.0 | 1.9 |
| Weight loss | 4.3 | 2.8 |
| Fluid and electrolyte disease | 24.9 | 21.6 |
| Blood loss anemia | 5.2 | 4.2 |
| Deficiency anemia | 16.9 | 12.0 |
| Alcohol abuse | 2.1 | 1.2 |
| Drug abuse | 0.2 | 0.1 |
| Psychoses | 1.7 | 1.7 |
| Depression | 2.0 | 4.6 |
Black Medicare patients had lower unadjusted 30-day mortality than white Medicare patients for five of the six conditions (Table 2), with statistically significant differences for four of the conditions. For example, among those admitted with CHF, 30-day mortality for black patients was 6.5 percent compared with 10.1 percent for white patients ( p<.001). The mortality rate was similar for black and white patients with pneumonia (16.9 percent versus 16.8 percent; p=.239). After adjustment for baseline difference in comorbid conditions, socioeconomic variables, and the hospital where patients received care, black patients had significantly lower 30-day mortality than whites for all six conditions (Table 2, final column). All estimates from the logistic regression model were qualitatively and quantitatively similar to the linear probability model estimates in Table 2.
Table 2.
Thirty-Day Mortality Rate by Race after Medicare Hospital Admission for Common Medical Conditions
| 30-Day Mortality Rates Unadjusted | Model #1 Unadjusted | Model #2 Health Risk† | Model #3 Health Risk† +SES Covariates‡ | Model #4 Health Risk† +SES Covariates‡ +Hospital Fixed Effects | ||
|---|---|---|---|---|---|---|
| Black | White | Racial Difference in 30-Day Mortality Rate (%) (Black–White) | ||||
| Pneumonia | 16.9 | 16.8 | 0.1 | −0.4* | −0.8* | −1.7* |
| CHF | 6.5 | 10.1 | −3.6* | −1.2* | −1.4* | −1.7* |
| Gl Bleed | 6.8 | 7.8 | −1.1* | −0.6* | −0.9* | −1.4* |
| Hip fracture | 6.5 | 8.1 | −1.6* | −2.3* | −2.5* | −2.9* |
| Stroke | 14.6 | 19.5 | −4.9* | −3.6* | −3.9* | −4.2* |
| AMI | 17.9 | 18.2 | −0.2 | −1.1* | −1.7* | −2.6* |
p-value <.05.
Health risk covariates include gender, age, discharge years, and comobidities.
SES covariates included zipcode-level percent urban, median household income, and percent college educated.
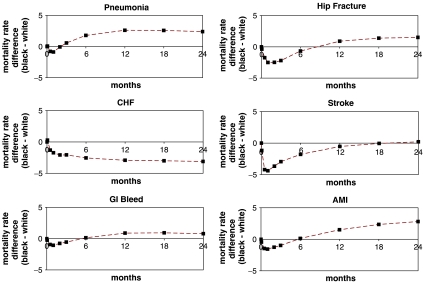
When we examined mortality rates for this group of Medicare patients beyond 30 days after hospitalization, we found that over time, the survival advantage initially observed among blacks dissipated for five of the six conditions (Table 3, Figure 1). By 90 days after hospitalization, blacks admitted for pneumonia had a higher mortality rate; by 180 days, blacks initially admitted with GI Bleed and AMI had higher mortality rates. Finally, by 1 year after hospitalization, mortality rates among patients with hip fracture were higher for blacks; by 2 years, mortality rates were higher among black patients for all conditions except CHF.
Table 3.
Adjusted Mortality Rates by Race after Medicare Hospital Admission for Common Medical Conditions*
| Pneumonia | CHF | Gl Bleed | Hip Fracture | Stroke | AMI | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Black | White | Black | White | Black | White | Black | White | Black | White | Black | White | |
| 30 days | 15.0 | 15.9 | 7.6 | 9.3 | 6.2 | 7.3 | 5.2 | 7.7 | 12.8 | 17.2 | 13.7 | 15.3 |
| 90 days | 25.2 | 24.6 | 15.1 | 17.1 | 12.6 | 13.2 | 12.8 | 15.0 | 19.8 | 22.8 | 18.8 | 19.8 |
| 180 days | 32.9 | 31.1 | 21.7 | 24.3 | 18.5 | 18.3 | 19.9 | 20.5 | 25.5 | 27.3 | 23.9 | 23.8 |
| 1 year | 42.3 | 39.7 | 31.3 | 34.3 | 26.6 | 25.7 | 28.8 | 27.9 | 32.8 | 33.4 | 30.9 | 29.4 |
| 2 years | 53.6 | 51.2 | 44.4 | 47.6 | 37.3 | 36.5 | 40.7 | 39.2 | 42.3 | 42.1 | 39.7 | 36.9 |
Adjusted for the health risk covariates (gender age, discharge years, and comobidities), SES covariates (zipcode-level percent urban, median household income, and percent college educated), and hospital fixed effects.
Figure 1.
Racial Differences in Adjusted Race-Specific Posthospital Admission Mortality Rates among Medicare Patients.
The pattern for VA hospitalizations is similar to Medicare patients at 30 days, with lower 30-day mortality for blacks for the same five conditions (Table 4, panel 1). However, in the long term, although mortality is higher for blacks in the Medicare sample for five conditions, mortality for blacks in the VA is higher only for stroke (Table 4, panel 2). The difference in the increase in the mortality rate of blacks relative to whites between the short and the long term is far smaller among VA than Medicare patients (Table 4, panel 3). Among VA patients, the relative deterioration in outcomes for blacks over time after admission is significant only for hip fracture and stroke (4.6–5.2 percentage points); for Medicare patients, in contrast, the deterioration is large and significant for five of the six conditions (3.6–6.8 percentage points).
Table 4.
Racial Differences in Adjusted† Mortality Rates for Common Medical Conditions after Medicare and VA Hospital Admission among Men
| Condition | Hospital Setting Type | |
|---|---|---|
| Medicare | VA | |
| Panel 1: Racial difference (B–W) in short-term (i.e., 30-day) mortality rate (%) | ||
| Pneumonia | −1.1* | −1.3* |
| CHF | −2.0* | −1.3* |
| Gl Bleed | −1.0* | −0.5* |
| Hip | −3.1* | −2.9* |
| Stroke | −3.0* | −2.1* |
| AMI | −2.0* | −2.7* |
| Panel 2: Racial difference (B–W) in long-term (i.e., 30-days to 2 years) mortality rate (%) | ||
| Pneumonia | 3.3* | 0.3 |
| CHF | −3.0* | −2.8* |
| Gl Bleed | 2.6* | 0.4 |
| Hip | 3.4* | 2.3 |
| Stroke | 3.7* | 2.5* |
| AMI | 4.8* | −1.0 |
| Panel 3: Change in racial difference in short-term and long-term mortality rate (%) | ||
| Pneumonia | 4.3* | 1.6 |
| CHF | −1.1* | −1.6* |
| Gl Bleed | 3.6* | 0.9 |
| Hip | 6.4* | 5.2* |
| Stroke | 6.8* | 4.6* |
| AMI | 6.8* | 1.7 |
p-value <.5.
Adjusted for the health risk covariates (age, discharge years, and comobidities), SES covariates (zipcode-level percent urban, median household income, and percent college educated), and hospital fixed effects.
DISCUSSION
We examined mortality rates among Medicare enrollees and found that for all six common medical conditions, 30-day mortality rates were lower for black Americans than white Americans. However, after hospitalization, the survival advantage initially seen among blacks dissipated, and by the end of 2 years, blacks had higher mortality than whites for five of the six conditions. When we compared this with outcomes within the VA, results were similar at 30 days after admission but long-term mortality did not worsen to the same degree as in the Medicare population for blacks relative to whites. The increases in mortality rates for blacks relative to whites at longer time intervals after hospitalization—and the slower rate at which relative mortality for blacks increased in the integrated VA health care system—suggest that while racial differences in hospital care, if any, do not lead to worse outcomes for blacks within the first 30 days after admission, factors related to care outside the hospital, such as type of social support, quality of ambulatory care, or access to prescription drugs are likely to play an important role in longer-term outcomes.
It is not obvious a priori that 30-day mortality rates would be lower for blacks given the lower life expectancy for blacks (National Center for Health Statistics 2005), prior findings that blacks receive a lower intensity of recommended therapies (Meehan et al. 1995), and some data suggesting that blacks are sicker at admission than whites (Buckle et al. 1992; Ebell et al. 1995; Johnson et al. 1995; Williams et al. 1995; Sonel et al. 2005). Nevertheless, the few non-VA studies that directly examine racial differences in 30-day hospital mortality—mostly for heart failure and AMI in nationwide samples—have also found similar results (Rathore et al. 2003; Barnato et al. 2005). Studies of hospitalizations in the VA also show lower 30-day mortality rates for blacks across a range of conditions ( Jha et al. 2001; Deswal et al. 2004; Volpp et al. 2007) and the lower 30-day mortality rates for blacks older than age 65 in the VA were found to be comparable to non-VA hospitalizations in Pennsylvania and California (Polsky et al. 2007). It is possible that the lower 30-day mortality rates for elderly blacks are due to lower rates of procedures which confer short-term risk (Meehan et al. 1995; Barnato et al., 2005, 2007), differences in the average severity of whites and blacks who access hospital care in ways that are not observable with administrative data, or a “survivorship bias,” in which blacks who survive to age 65 are hardier than whites because the sickest blacks have already died by this point in time. However, a “survivorship bias” would be less compatible with the observed relative worsening in mortality for blacks with increasing time from hospital admission. While we cannot differentiate between these speculative explanations, to our knowledge this is the first study to demonstrate the consistency of the pattern of racial differences in hospital mortality in the elderly population throughout the United States across common conditions.
Several potential factors could explain our findings. First, unmeasured confounders may affect the findings of lower initial mortality rates for blacks. However, adjustments for unbalanced comorbid conditions, socioeconomic status, and hospital selection by race lowered 30-day mortality for blacks relative to whites to a greater degree than observed in the unadjusted analyses and did not modify the relative increases in the mortality rate for blacks from 30 days to 2 years. This suggests that these measured factors do not explain the lower 30-day mortality for blacks, nor can they explain the relative increases in mortality for blacks as time from admission increases. Second, linear and nonlinear adjustment models produced results similar to each other and to unadjusted mortality, suggesting that model choice or specification does not explain the findings.
Although we cannot explain why blacks have lower mortality initially and higher mortality as the time from admission increases, the increasing rates of mortality for blacks may be generated by the greater vulnerability of blacks to environmental factors (more dangerous neighborhoods, impact of poverty, differences in health behaviors), by a fragmented health care system ill-equipped to address these factors, or poor access to high-quality outpatient care (Sherkat et al. 2005; Trivedi et al. 2006). This idea is supported by the comparison of racial differences in mortality over time in the VA and in the non-VA hospital system. In this comparison we see that the VA's integrated health care system, which includes prescription drug coverage with small or nonexistent copayments, may make a difference in the long-term relative mortality risk of blacks for conditions for which coordination of care and access to prescription drugs are important. An alternative explanation is that among the VA population, difference in socioeconomic status, lifestyle, and psychosocial factors between blacks and whites may be less pronounced than in non-VA settings. It is not possible with the available data to determine the relative importance of these factors in explaining the observed differences in mortality over time. Differences in the observed patterns for congestive heart failure compared with other conditions may relate to the fact that it is a chronic condition, which necessitates more frequent hospital readmission than the other conditions. At each hospital admission, patients presumably get a careful workup and revision of their treatment plan as needed. The factors that lead to worsened outcomes for blacks as the amount of time from hospital admission increases thus could be “overridden” by the frequent admissions for patients at high risk for mortality. Our data provide some empirical support for this hypothesis; after adding back in the readmissions excluded from our analytic files, 32.6 percent of patients with a principal diagnosis of heart failure had more than one heart failure admission (38.3 percent for blacks, 31.9 percent for whites) while for other conditions the proportion of patients with more than one admission ranged from 6.1 percent for hip fracture to 10.6 percent for stroke, 14.4 percent for GI Bleed, 14.7 percent for AMI, and 21.4 percent for pneumonia.
The primary limitation of our study is the fact that it is descriptive and does not attempt to identify the mechanism that might explain the pattern of racial differences observed. Our findings do not imply that hospitals discriminate against whites or that discrimination against blacks does not exist. However, describing this robust pattern brings the literature closer to identifying the sources of racial disparities in population-based outcomes, which will aid in the design of effective interventions aimed at ameliorating racial disparities. A second important limitation is the use of administrative data to study health outcomes. These administrative data have only limited measures of health status and socioeconomic status. However, we attempted to overcome these limitations by using a well-validated approach to risk adjustment that has a high degree of ability to discriminate between patients who die and patients who do not (Southern, Quan, and Ghali 2004) and by building on previous studies of racial disparities in outcomes that use administrative data (Jha et al. 2001; Smedley, Stith, and Nelson 2003; Volpp et al. 2007).
Among Medicare enrollees we found black Americans have lower 30-day mortality than white Americans. However, by 2 years after admission, blacks had higher mortality than whites for five of the six study conditions. This relative deterioration of outcomes after discharge for blacks was not as great among patients hospitalized within the VA, which suggests the possibility that an integrated health care delivery system like the VA may attenuate racial disparities in health. Further research should attempt to differentiate between competing explanations for lower 30-day mortality for blacks and the observed patterns of higher mortality for blacks with increasing time from hospital admission. Medical system efforts to reduce racial disparities may need to increasingly focus on post-hospital care and environmental factors rather than hospital-targeted initiatives.
Acknowledgments
Joint Acknowledgement/Disclosure Statement: We thank VA HSR&D IIR 03.070.1 for funding support. The funding agency had no role in reviewing or approving this manuscript. Dr. Volpp was a VA HSR&D Career Development Award recipient at the time of much of this work and received funding support for this project. There are no conflicts of interest or financial disclosures to report.
Disclaimers: None.
Supplementary material
The following supplementary material for this article is available online:
HSR Author Matrix.
ICD-9 Codes for Each Condition.
Baseline Characteristics by Race among Men with Medicare and VA Hospital Admissions.
This material is available as part of the online article from http://www.blackwell-synergy.com/doi/abs/10.1111/j.1475-6773.2008.00837.x (this link will take you to the article abstract).
Please note: Blackwell Publishing is not responsible for the content or functionality of any supplementary materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Agency for Healthcare Research and Quality. AHRQ Quality Indicators–Guide to Inpatient Quality Indicators: Quality of Care in Hospitals–Volume, Mortality, and Utilization. Rockville, MD: Agency for Healthcare Research and Quality; 2002. AHRQ Pub. No. 02-R 0204. [Google Scholar]
- Barnato A E, Chang C H, Saynina O, Garber A M. Influence of Race on Inpatient Treatment Intensity at the End of Life. Journal of General Internal Medicine. 2007;22(3):338–45. doi: 10.1007/s11606-006-0088-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnato A E, Lucas F L, Staiger D, Wennberg D E, Chandra A. Hospital-Level Racial Disparities in Acute Myocardial Infarction Treatment and Outcomes. Medical Care. 2005;43(4):308–19. doi: 10.1097/01.mlr.0000156848.62086.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckle J M, Horn S D, Oates V M, Abbey H. Severity of Illness and Resource Use Differences among White and Black Hospitalized Elderly. Archives of Internal Medicine. 1992;152(8):596–603. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. Denominator File.” [accessed on April 1, 2006]. Available at http://www.cms.hhs.gov/IdentifiableDataFiles/06_DenominatorFile.asp.
- Cromwell J, McCall N T, Burton J, Urato C. Race/Ethnic Disparities in Utilization of Lifesaving Technologies by Medicare Ischemic Heart Disease Beneficiaries. Medical Care. 2005;43(4):330–37. doi: 10.1097/01.mlr.0000156864.80880.aa. [DOI] [PubMed] [Google Scholar]
- Davies S M, Geppert J, McClellan M, McDonald K M, Romano P S, Shojania K G. Refinement of the HCUP Quality Indicators. Technical Review Number 4. Rockville, MD: Agency for Healthcare Research and Quality; 2001. AHRQ Publication No. 01-0035. [PubMed] [Google Scholar]
- Deswal A, Petersen N J, Souchek J, Ashton C M, Wray N P. Impact of Race on Health Care Utilization and Outcomes in Veterans with Congestive Heart Failure. Journal of the American College of Cardiology. 2004;43(5):778–84. doi: 10.1016/j.jacc.2003.10.033. [DOI] [PubMed] [Google Scholar]
- Ebell M H, Smith M, Kruse J A, Drader-Wilcox J, Novak J. Effect of Race on Survival Following In-Hospital Cardiopulmonary Resuscitation. Journal of Family Practice. 1995;40(6):571–7. [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris D R, Coffey R M. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Fiscella K, Franks P. Impact of Patient Socioeconomic Status on Physician Profiles: A Comparison of Census-Derived and Individual Measures. Medical Care. 2001;39(1):8–14. doi: 10.1097/00005650-200101000-00003. [DOI] [PubMed] [Google Scholar]
- Geronimus A T, Bound J. Use of Census-Based Aggregate Variables to Proxy for Socioeconomic Group: Evidence from National Samples. American Journal of Epidemiology. 1998;148(5):475–86. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- Geronimus A, Bound J, Neidert L. On the Validity of Using Census Geocode Characteristics to Proxy Individual Socioeconomic Characteristics. Journal of the American Statistical Association. 1996;91:529–37. [Google Scholar]
- Jha A K, Li Z, Orav E J, Epstein A M. Care in U.S. Hospitals—The Hospital Quality Alliance Program. New England Journal of Medicine. 2005;353(3):265–74. doi: 10.1056/NEJMsa051249. [DOI] [PubMed] [Google Scholar]
- Jha A K, Shlipak M G, Hosmer W, Frances C D, Browner W S. Racial Differences in Mortality among Men Hospitalized in the Veterans Affairs Health Care System. Journal of the American Medical Association. 2001;285(3):297–303. doi: 10.1001/jama.285.3.297. [DOI] [PubMed] [Google Scholar]
- Johnson P A, Goldman L, Orav E F, Garcia T, Pearson S D, Lee T H. Comparison of the Medical Outcomes Study Short-Form 36-Item Health Survey in Black Patients and White Patients with Acute Chest Pain. Medical Care. 1995;33(2):145–60. [PubMed] [Google Scholar]
- Meehan T P, Hennen J, Randford M J, Petrillo M K, Elstein P, Ballard D J. Process and Outcomes of Care for Acute Myocardial Infarction among Medicare Beneficiaries in Connecticut: A Quality Improvement Demonstration Project. Annals of Internal Medicine. 1995;122(12):928–36. doi: 10.7326/0003-4819-122-12-199506150-00007. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health United States 2005 with Chartbook on Trends in the Health of Americans. Washington, DC: Government Printing Office; 2005. [PubMed] [Google Scholar]
- O'Conner G T, Quinton H B, Traven N D, Ramunno L D, Dodds T A, Marciniak T A, Wennberg J E. Geographic Variation in the Treatment of Acute Myocardial Infarction: The Cooperative Cardiovascular Project. Journal of the American Medical Association. 1999;281(7):627–33. doi: 10.1001/jama.281.7.627. [DOI] [PubMed] [Google Scholar]
- Office of Statewide Health Planning and Development. Second Report of the California Hospitals Outcomes Project, May 1996. Acute Myocardial Infarction. Sacramento, CA: Office of Statewide Health Planning and Development; 1996. [Google Scholar]
- Polsky D, Lave J, Klusaritz H, Jha A, Pauly M V, Cen L, Xie H, Stone R, Chen H, Volpp K G. Is Lower 30-Day Mortality Post-Hospital Admission among Blacks Unique to the Veterans Affairs Health Care System? Medical Care. 2007;54(11):1083–9. doi: 10.1097/MLR.0b013e3180ca960e. [DOI] [PubMed] [Google Scholar]
- Rathore S S, Foody J M, Wang Y, Smith G L, Herrin J, Masoudi F A, Wolfe P, Havranek E P, Ordin D L, Krumholz H M. Race, Quality of Care, and Outcomes of Elderly Patients Hospitalized with Heart Failure. Journal of the American Medical Association. 2003;289(19):2517–24. doi: 10.1001/jama.289.19.2517. [DOI] [PubMed] [Google Scholar]
- Rockall T A, Logan R F, Devlin H B, Northfield T C. Variation in Outcome after Acute Upper Gastrointestinal Hemorrhage. The National Audit of Acute Upper Gastrointestinal Hemorrhage. Lancet. 1995;346(8971):346–50. doi: 10.1016/s0140-6736(95)92227-x. [DOI] [PubMed] [Google Scholar]
- Shen J J, Wan T T, Perlin J B. An Exploration of the Complex Relationship of Socioecological Factors in the Treatment and Outcomes of Acute Myocardial Infarction in Disadvantaged Populations. Health Services Research. 2001;36(4):710–32. [PMC free article] [PubMed] [Google Scholar]
- Sherkat D E, Kilbourne B S, Cain V A, Hull P C, Levine R S, Husaini B A. Explaining Race Differences in Mortality among the Tennessee Medicare Elderly: The Role of Physician Services. Journal of Health Care for the Poor & Underserved. 2005;16(4, Suppl. A):50–63. doi: 10.1353/hpu.2005.0130. [DOI] [PubMed] [Google Scholar]
- Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- Sonel A F, Good C B, Mulgund J, Roe M T, Gibler W B, Smith S C, Cohen M G, Pollack C V, Ohman E M, Peterson E D. Racial Variations in Treatment and Outcomes of Black and White Patients with High-Risk Non-ST-Elevation Acute Coronary Syndromes: Insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guideline?) Circulation. 2005;111(10):1225–32. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- Southern D A, Quan H, Ghali W A. Comparison of the Elixhauser and Charlson/Deyo Methods of Comorbidity Measurement in Administrative Data. Medical Care. 2004;42(4):355–60. doi: 10.1097/01.mlr.0000118861.56848.ee. [DOI] [PubMed] [Google Scholar]
- Stukenborg G J, Wagner D P, Connors A F. Comparison of the Performance of Two Comorbidity Measures, with and without Information from Prior Hospitalizations. Medical Care. 2001;39:727–39. doi: 10.1097/00005650-200107000-00009. [DOI] [PubMed] [Google Scholar]
- Trivedi A N, Zaslavsky A M, Schneider E C, Ayanian J Z. Relationship between Quality of Care and Racial Disparities in Medicare Health Plans. Journal of the American Medical Association. 2006;296(16):1998–2004. doi: 10.1001/jama.296.16.1998. [DOI] [PubMed] [Google Scholar]
- Volpp K G, Stone R, Jha A K, Lave J, Pauly M V, Klusaritz H, Chen H, Cen L, Brucker N, Polsky D. Is Thirty-Day Hospital Mortality Really Lower for Black Veterans Compared with White Veterans? Health Services Research. 2007;42(4):1613–31. doi: 10.1111/j.1475-6773.2006.00688.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams J F, Zimmerman J E, Wagner D P, Hawkins M, Knaus W A. African-American and White Patients Admitted to the Intensive Care Unit: Is There a Difference in Therapy and Outcome? Critical Care Medicine. 1995;23(4):626–36. doi: 10.1097/00003246-199504000-00009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
HSR Author Matrix.
ICD-9 Codes for Each Condition.
Baseline Characteristics by Race among Men with Medicare and VA Hospital Admissions.