Abstract
Case report
A 32-year-old African male presented with 10 hours of severe back pain. Initial computed tomography scan of the back showed no abnormality, and initial laboratory investigations were consistent with rhabdomyolysis. Despite stopping potential causative medications, aggressive intravenous hydration, and urine alkalinization, his creatinine kinase continued to steadily climb. Thirty-six hours after admission, a magnetic resonance imaging of his back was done because of new swelling over the right paraspinal muscles and loss of sensation in this region. Marked swelling of the right erector spinae muscles was observed, and right and left compartment pressure measurements were 108 and 21 mm Hg, respectively. He had urgent fasciotomy after which his rhabdomyolysis and pain recovered.
Conclusion
Our case highlights the need for early consideration of compartment syndrome as a possible cause of back pain in the setting of rhabdomyolysis. Rhabdomyolysis can present in the absence of late complications such as neurological and vascular compromise.
KEY WORDS: occult compartment syndrome, nonresolving rhabdomyolysis, spinae muscles, fasciotomy, neurological and vascular compromise
INTRODUCTION
There are many causes of rhabdomyolysis, including infection, drugs/toxins, electrolyte abnormalities, surgery, trauma, or compression.1–4 Compartment syndrome can cause rhabdomyolysis from severe muscle compression and swelling within a closed, rigid boundary (compartment) formed by connective tissue and bone. It results in impairment of neurovascular systems, muscle ischemia, and tissue death. Compartment syndrome most often occurs in the extremities; however, it has rarely occurred in the paraspinal muscles.5–8 It is prudent to consider compartment syndrome as a potential cause of rhabdomyolysis in the setting of back pain, even before the onset of late complications such as neurological and vascular compromise because of the benefits of early surgical intervention. We discuss the case of a patient who presented with a nonresolving rhabdomyolysis and an initially occult erector spinae muscle compartment syndrome.
CASE REPORT
A 32-year-old man of African origin presented to the emergency department with excruciating right lower back pain which radiated down the posterior side of his right leg. He had done weight-lifting exercises that primarily involved the use of the back muscles, and the pain began 9 hours subsequently. Medication use included antihistamines and pseudoephedrine for an upper respiratory tract infection 1 week before presentation and creatine supplements for body building starting 3 weeks before presentation. He denied the use of heroin, cocaine, and amphetamines; however, he had 0.8 liters of alcohol intake in the 2 weeks before presentation. There was no history of back pain or other medical problems.
Initial physical examination revealed marked tenderness over the right paraspinal muscles but no erythema, swelling, or signs of trauma. Passive and active ranges of motion were limited because of his back and leg pain. Straight leg raise was positive on the right at 25° elevation, and there was contralateral pain with left straight leg raise. Sensation was intact and plantar responses were normal.
Admission laboratory investigations were as follows: white blood cell count (WBC), 9.0 × 109/L; serum creatinine, 102 μmol/L (1.15 mg/dL); serum creatinine kinase (CK), 9,209 U/L; aspartate aminotransferase (AST), 327 U/L; alanine aminotransferase (ALT), 61 U/L; lactate dehydrogenase (LDH), 969 U/L; and amylase, 38 U/L. The computed tomography (CT) scan of the spine was normal and showed no muscle swelling or vertebral fractures (Fig. 1).
Figure 1.
CT scan of the spine and paraspinal muscle showing no swelling or hematoma.
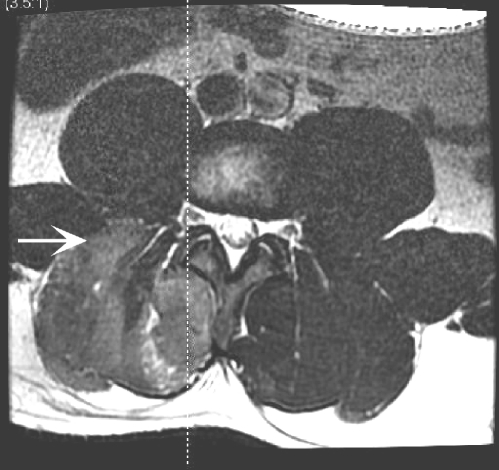
The patient was admitted for treatment of rhabdomyolysis and further evaluation of his back pain. Intravenous saline was administered at 150–200 mL/hour, and the pain was treated with opioid analgesia. The creatine and pseudoephedrine supplements were discontinued. Despite these measures, his CK rose to 38,000 U/L and his back pain worsened over the next 24 hours. A magnetic resonance imaging study (MRI) was ordered to rule out structural causes of back and leg pain with rising CK. There was no evidence of disk herniation or spinal fracture, and the spinal column was normal. However, there was marked edema and swelling in his right erector spinae muscle complex from the L3 level to the L5/S1 disk space (Fig. 2). At 36 hours after admission, he developed new swelling over the right paraspinal muscles on physical examination with reduced sensation over the involved muscles.
Figure 2.
Preoperative MRI (T2 weighted, axial L3)—right-sided paraspinal muscle diameter (white horizontal arrow) and increased edema and signal density (white diagonal arrow).
Forty-eight hours after admission, compartment pressures of both erector spinae muscles were measured using a 14-gauge angiocatheter (BD Medical—Medical Surgical Systems, Sandy, UT, 84070, USA) which was connected to an arterial line set-up.9 The resulting pressures in the right and left erector spinae muscles were 108 and 21 mm Hg, respectively. The CK at this time was 72,820 U/L, and the other peak laboratory values are presented in Table 1. The patient was taken to the operating room immediately. A fasciotomy was performed, and once the compartment was released, the color of the muscle changed dramatically from gray to pink. The fascia was not repaired and skin closure was completed.
Table 1.
Comparison of Acute Compartment Syndrome Findings between Cases
| Characteristics | Carr et al.5 | Difazio et al.6 | Kitajima et al.7 | Khan et al.8 | Present report |
|---|---|---|---|---|---|
| History | |||||
| Age (yrs) | 24 | 27 | 25 | 35 | 32 |
| History of exercise-induced pain | 2-yr history | None | Several-month history | 10-yr history | None |
| Precipitant | Downhill skiing | Downhill skiing | Surfing | Downhill skiing | Weight lifting |
| Physical examination | |||||
| Loss of lumbar lordosis | Yes | Not stated | Not stated | Yes | Yes |
| Paraspinal muscle | Bilateral | Bilateral | Not stated | Bilateral | Right paraspinal muscle |
| Tenderness | L3–L4 | T12–L5 | Left lumbar paraspinal muscle | Bilateral paraspinal muscles | T6–L3 on right only |
| Sensory loss | Not stated | Yes | Yes | Yes | Yes |
| Straight leg raise | Exacerbated pain | Exacerbated pain | Not stated | No exacerbation | Exacerbated pain |
| Investigations | |||||
| WBC (×109/L) | 23 | 9 | 8.6 | 9.8 | 9 |
| Amylase (U/L) | 65 | 140 | 39 | 39 | 38 |
| AST (U/L) | 365 | 565 | 193 | 804 | 608 |
| CK (U/L) | 5,465 | 60,000 | 21,440 | 48,550 | 72,820 |
| LDH (U/L) | Not stated | Not stated | 505 | 3,823 | 2,089 |
| CT scan | Swelling of paraspinal muscles | Not done | Not done | Swelling of paraspinal muscles | Normal |
| MRI (paraspinal muscles) | Not done | Bilateral increased signal | Increased signal left | Bilateral increased signal | Increased signal right |
| Compartment pressures (mmHg) | Not done | Left 80, right 70 | Left 14–16, right 4–5 | Left 26, right 44 | Left 21, right 108 |
Reference numbers are beside the study author’s name.
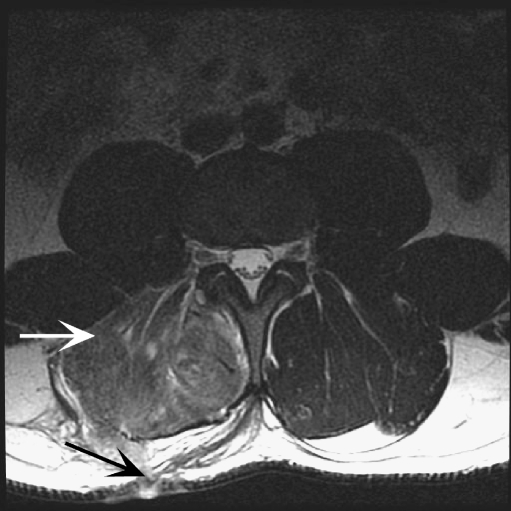
Subsequent to the fasciotomy, the CK fell to 3,683 U/L at 5 days postoperatively and his pain improved such that he was able to walk and his requirement for pain medication reduced markedly. A hemoglobin electrophoresis for sickle cell trait was negative. Fourteen days later, at outpatient clinic follow-up, he had full range of motion and was able to exercise again. His follow-up laboratory investigations were: serum CK, 500 U/L; AST, ALT, and ALP were 28, 42, and 66 U/L, respectively; LDH, 269 U/L; and WBC, 5.6 × 109/L. A repeat MRI at 6 weeks showed reduction in the swelling of the right erector spinae muscle complex (Fig. 3).
Figure 3.
Postoperative MRI (T2 weighted, axial L3)—6 weeks after fasciotomy (black diagonal arrow) with decrease in muscle diameter and edema and right paraspinal compartment decompression (white horizontal arrow).
DISCUSSION
Our patient presented with an initially occult acute paraspinal compartment syndrome and nonresolving rhabdomyolysis. Acute compartment syndrome of the paraspinal muscles has been reported in various settings including trauma or surgery2,10–11 and in nontraumatic situations5–8 (Table 1). In our patient, compartment syndrome was likely induced by weight-lifting exercises. Clinical and laboratory features of the previously reported cases of acute paraspinal muscle compartment syndrome are shown in Table 1. All cases occurred in males between ages 24 and 35 years of age. Physical signs reported include loss of lumbar lordosis5–8 and sensory loss over the affected muscles.6–8 All cases had elevated serum CK and AST,5–8 and 1 study had elevated WBC count and amylase.5
Chronic exertional compartment syndromes have been well documented. However, acute exertional compartment syndrome is less common. The pathophysiology is the same: repetitive and intense muscle activity causing edema within a confined fascial space. This acute edema impedes lymphatic and possibly venous drainage which, under normal circumstances, recedes on completion of the activity. With acute compartment syndrome, the edema remains after cessation of activity allowing for increase in compartmental pressure. It is likely that the pressure within the fascial space becomes such that blood supply to the muscle is compromised to the extent that ischemia of the muscle occurs, resulting in rhabdomyolysis.
The boundaries of the lumbar paraspinal compartment are: portions of the sacrum and iliac crests, the lumbardorsal and thoracolumbar fasciae, iliolumbar ligaments, transverse processes, intertransverse muscles, ligaments, and vertebral laminae.5 The sciatic nerve (L4–5, S1–3) is formed at the lower margin of the piriformis muscle and emerges into the buttock lying on the ischium.12 “Sciatica” usually occurs when one of the aforementioned nerve roots is compressed as it exits its foramen. Pain may be perceived as coming from anywhere along the sciatic nerve regardless of the actual site of injury. A paraspinal compartment syndrome could cause sciatica-type symptoms if the nerves were affected at the point of exit from the neural foramina.
In our patient, it is still plausible that antihistamines, creatine supplements, alcohol use dehydration, or a viral illness1 may have caused rhabdomyolysis; however, clinically, it seems unlikely that such conditions resulted in a localized presentation and the rhabdomyolysis only started to resolve after fasciotomy. A hemoglobin electrophoresis was negative for sickle cell trait. In addition, alcohol use (0.8 liters) and creatine supplement utilization occurred 2 and 3 weeks before admission, respectively. The patient denied the use of cocaine, heroin, and amphetamines; however, urine and serum toxicology screens were not sent. Even in the setting of crush injuries and trauma, there is a reduction in CK in the majority of patients in response to intravenous hydration and urine alkalinization.13 In our patient, despite aggressive hydration and stopping all inciting medications, the CK continued to increase steadily, which raised the suspicion for an ongoing, unidentified source of the rhabdomyolysis.
In previous studies of acute compartment syndrome where CT scans were done, these scans showed marked muscle swelling.5,8 This was not present in our patient, so the compartment syndrome either developed between the CT scan and MRI (1.5 days) or the CT may have missed early muscle swelling. In the light of the MRI findings, a careful rereview of the original CT scan did not show swelling or hematoma. It is surprising to note that the initial CT scan did not show evidence of muscle swelling given that the intracompartment pressure in the affected muscle in our patient were higher than any of those reported in this muscle group.6–8 Measurement of compartment pressures is the current gold standard in terms of diagnosing acute compartment syndrome. Future directions of investigation might include the assessment of whether CT scan or MRI compare in sensitivity and specificity to compartment pressure measurements in the erector spinae muscles.
Acute compartment syndrome is associated with pain, muscle damage, and renal failure. The authors suggest that diagnosis of this condition in the erector spinae muscle complex requires a high index of suspicion, MRI, and measurement of compartment pressures.6–8 In cases of compartment syndrome of this muscle group, medical management alone has resulted in recovery but with persistent exercise-induced pain.5–6 Therefore, management should include urgent surgical intervention to prevent long-term sequelae of compartment syndrome.7–8,11 Our case highlights the need for early consideration of compartment syndrome as a possible cause of back pain in the setting of rhabdomyolysis. Rhabdomyolysis can present in the absence of late complications such as neurological and vascular compromise.
Acknowledgements
The authors wish to thank Drs. Logan Moodley, Shabbir Alibhai, Jeff Singh, and Alicia Fernandez for their insightful suggestions.
Conflict of Interest Drs. Minnema, Quraishi, and Prakash have no conflicts of interest. Dr. Fehlings holds the Krembil Chair in Neural Repair and Regeneration. Dr. Neligan held the Wharton Chair until June 2007. Funds donated by families to The University of Toronto are allocated by the respective chairs for research and faculty recruitment.
References
- 1.Vanholder R, Sever MS, Erek E, Lamiere N. Rhabdomyolysis. J Am Soc Nephrol. 2000;11:1553–61. doi: 10.1681/ASN.V1181553. [DOI] [PubMed] [Google Scholar]
- 2.Ferreira J, Galle C, Aminian A, et al. Lumbar paraspinal rhabdomyolysis and compartment syndrome after abdominal aortic aneurysm repair. J Vasc Surg. 2003;37(1):198–201. doi: 10.1067/mva.2003.108. [DOI] [PubMed] [Google Scholar]
- 3.Foster M. Rhabdomyolysis in lumbar spine surgery: a case report. Spine. 2003;28(14):276–8. doi: 10.1097/00007632-200307150-00030. [DOI] [PubMed] [Google Scholar]
- 4.Odeh M. The role of reperfusion induced injury in the pathogenesis of the crush syndrome. N Engl J Med. 1991;324:1417–22. doi: 10.1056/NEJM199105163242007. [DOI] [PubMed] [Google Scholar]
- 5.Carr D, Gilbertson L, Frymoyer J, Krag M, Pope M. Lumbar paraspinal compartment syndrome. A case report with physiologic and anatomic studies. Spine. 1985;10:816–20. doi: 10.1097/00007632-198511000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Difazio FA, Barth RA, Frymoyer JW. Acute lumbar paraspinal compartment syndrome. J Bone Joint Surg. 1991;73:1101–1103. [PubMed] [Google Scholar]
- 7.Kitajima I, Tachibana S, Hirota Y, Nakamichi K. Acute paraspinal muscle compartment syndrome treated with surgical decompression. Am J Sports Med. 2002;30(2):283–5. doi: 10.1177/03635465020300022301. [DOI] [PubMed] [Google Scholar]
- 8.Khan RJ, Fick DP, Guier CA, Menolascino MJ, Neal MC. Acute paraspinal compartment syndrome. J Bone Joint Surg Am. 2005;87(5):1126–8. doi: 10.2106/JBJS.D.02133. [DOI] [PubMed] [Google Scholar]
- 9.Boody AR, Wongworawat MD. Accuracy in the measurement of compartment pressures: a comparison of three commonly used devices. J Bone Joint Surg Am. 2005;87(11):2415–22. doi: 10.2106/JBJS.D.02826. [DOI] [PubMed] [Google Scholar]
- 10.Sava J, Moelleken A, Waxman K. Cardiac arrest caused by reperfusion injury after lumbar paraspinal compartment syndrome. J Trauma. 1999;46(1):196–7. doi: 10.1097/00005373-199901000-00035. [DOI] [PubMed] [Google Scholar]
- 11.Osamura N, Takahashi K, Endo M, Kurumaya H, Shima I. Lumbar paraspinal myonecrosis after abdominal vascular surgery: a case report. Spine. 2000;25(14):1852–4. doi: 10.1097/00007632-200007150-00019. [DOI] [PubMed] [Google Scholar]
- 12.McMinn RMH. Last’s Anatomy—Regional and Applied. 9. New York: Churchill Livingstone; 1995. [Google Scholar]
- 13.Gunal AI, Celiker H, Dogukan A, et al. Early and vigorous fluid resuscitation prevents acute renal failure in the crush of catastrophic earthquakes. J Am Soc Nephrol. 2004;15:1862–1867. doi: 10.1097/01.ASN.0000129336.09976.73. [DOI] [PubMed] [Google Scholar]