Abstract
Background
Most colorectal cancers develop from adenomatous polyps. National guidelines recommend surveillance colonoscopy within 5 years after such polyps are removed.
Objective
To determine whether surveillance colonoscopy can be increased among overdue patients by reminders to their primary physicians.
Design
Randomized, controlled trial of patient-specific reminders mailed to 141 physicians in 2 Massachusetts primary care networks during April, 2006.
Patients
Seven hundred seventeen patients who had colorectal adenomas removed during 1995 through 2000 and no follow-up colonoscopy identified via automated review of electronic records through March, 2006.
Measurements and Main Results
The use of colonoscopy and detection of new adenomas or cancer were assessed at 6 months by a blinded medical record review in all patients. Among 358 patients whose physicians received reminders, 33 (9.2%) patients underwent colonoscopy within 6 months, compared with 16 (4.5%) of 359 patients whose physicians did not receive reminders (P = 0.009). In prespecified subgroups, this effect did not differ statistically between 2 primary care networks, elderly and nonelderly patients, or women and men (all P > 0.60 by Breslow–Day test). New adenomas or cancer were detected in 14 (3.9%) intervention patients and 6 (1.7%) control patients (P = 0.06), representing 42.4% and 37.5% of patients who underwent colonoscopy in each group, respectively. Despite using advanced electronic health records to identify eligible patients, 22.5% of enrolled patients had a prior follow-up colonoscopy ascertained only by visual record review, and physicians reported 27.9% of intervention patients were no longer active in their practice.
Conclusions
Among patients with prior colorectal adenomas, physician reminders increased the use of surveillance colonoscopy, but better systems are needed to identify eligible patients (ClinicalTrials.gov ID number NCT00397969).
KEY WORDS: colorectal neoplasms, adenomatous polyps, colonic polyps, colonoscopy, quality of health care, primary health care, randomized controlled trials, Massachusetts
Colorectal cancer is the second leading cause of cancer mortality in the United States. In 2006, more than 55,000 people died from colorectal cancer, accounting for about 10% of all cancer-related deaths in both women and men.1 Most colorectal cancers arise in adenomatous polyps that can progress to colorectal cancer over 8 to 10 years if not removed,2 and removing these polyps via colonoscopy reduces the incidence of colorectal cancer.3–5 National guidelines have recommended that patients with adenomas undergo surveillance colonoscopy within 5 years.6
Appropriate follow-up of abnormal cancer-screening tests requires effective communication between primary physicians and specialist physicians, communication between physicians and patients, and systems for coordinating and tracking care. To fulfill “the promise of cancer screening,” patients with potentially premalignant lesions such as colorectal adenomas must receive appropriate follow-up testing to monitor them for recurrent abnormalities.7 Health care organizations, therefore, need systems to monitor whether patients return for colonoscopy when appropriate and to remind physicians when patients are due for this procedure. Ideally, these systems would use automated data from colonoscopy and pathology reports to provide ongoing monitoring and decision support to physicians. The objective of this randomized study was to assess whether rates of surveillance colonoscopy could be increased by physician reminders for patients with prior adenomas who were overdue for this procedure.
METHODS
Setting and Participants
The study protocol was registered with the ClinicalTrials.gov database (ID number NCT00397969) and approved by the human studies committees of Harvard Medical School, Brigham and Women’s Hospital, and Harvard Vanguard Medical Associates. Because the researchers had no contact with patients and primary physicians decided whether to recommend colonoscopy, these committees authorized a waiver of patient consent. Physicians were informed that their participation in the study was voluntary and confidential.
Patients were potentially eligible for the study if they had 1 or more adenomas detected by colonoscopy at Brigham and Women’s Hospital from 1995 through 2000, did not have a follow-up colonoscopy documented in electronic clinical data during 2001 through March 2006, and had an active attending physician in a primary care practice affiliated with Brigham and Women’s Hospital or Harvard Vanguard Medical Associates, an integrated group practice.
Among patients who had a colorectal adenoma removed during 1995 through 2000, about half received their primary care from 12 hospital-affiliated practices, including 5 hospital-based offices, 5 community-based offices, and 2 community health centers. Since 2000, all primary physicians at these sites have used the Longitudinal Medical Record, an internally developed electronic health record. The other half of patients received their primary care from Harvard Vanguard Medical Associates, an integrated group practice with 14 local health centers. Since 1999, all physicians in this latter group have used the EpicCare electronic health record. Both electronic record systems have been used in prior studies of ambulatory quality of care.8–14
Patients who had colorectal polyps removed via flexible sigmoidoscopy or colonoscopy during 1995 through 2000 were ascertained from the electronic endoscopy database maintained by the hospital’s gastroenterology division. To identify patients who had adenomatous polyps, endoscopy data were linked to the hospital’s electronic pathology reports. A text-searching program was developed to scan pathology reports for key words of adenoma or adenomatous polyp. Key words of carcinoma and adenocarcinoma were also identified to exclude patients with colorectal cancer.
To confirm the accuracy of the automated text searching of pathology reports, 2 investigators (Ayanian and Sequist) visually inspected these reports for random samples of 100 patients with adenomas and 100 patients without adenomas. The sensitivity of the automated search was 99% (1 false-negative report with the plural term adenomas), and the specificity was 99% (1 false-positive report with the phrase no adenomas).
Patients who had follow-up colonoscopies performed at the hospital between 2001 and March 2006 were identified from the hospital’s endoscopy database. Automated electronic data from the hospital and integrated group practice were used to identify follow-up colonoscopies performed outside of the hospital. In addition, electronic records were used to identify primary physicians for eligible patients in 2006 and to exclude patients who died before 2006.
Randomization and Intervention
After eligible patients with active primary physicians were identified, we randomized patients to have their primary physicians receive patient-specific reminders recommending surveillance colonoscopy. Randomizations were stratified within the 2 health care organizations and each physician. We chose to randomize patients rather than health care organizations or physicians because patient-level randomization maximized our statistical power to detect an intervention effect, making it a within-physician rather than between-physician effect and therefore statistically independent of random variations in physicians’ effectiveness in promoting surveillance colonoscopy.
To balance the intervention and control groups by patients’ age, sex, and time since prior colonoscopy, we performed 20 randomizations of the cohort using SAS statistical software and selected the randomization that provided the most even balance of these 3 characteristics, as defined by the maximum difference between treatment and control groups on the numbers of eligible patients in the age, sex, and time categories. After the randomization but immediately before the intervention mailing, we learned that 47 primary physicians of 82 patients (42 allocated to the intervention and 40 allocated to the control group) at the integrated medical group had left the organization. We excluded these 82 patients a priori from the intervention mailing and all subsequent analyses because they did not meet the prespecified requirement to have an active primary physician to assess their clinical appropriateness for colonoscopy.
For patients allocated to the intervention group, a letter was sent via interoffice mail to their primary physicians in late April 2006 to notify the physicians about the potential need for colonoscopy among their patients in the intervention group. The mailings included personally addressed letters to the patients recommending colonoscopy and encouraging them to call their physician’s office to schedule the procedure. If physicians determined colonoscopy was clinically indicated, they could mail these letters to their patients. A template of the letter that physicians could edit was also available in the electronic health record.
A response form was included in the mailings to physicians, asking them to report whether they intended to send a reminder letter or call each of their patients in the intervention group to recommend colonoscopy. They were also asked for reasons a patient should not have this procedure (deceased, severe comorbid illness, advanced age, had follow-up colonoscopy since 2000, or no longer active in the physician’s practice). Physicians who did not respond to the initial letter within 1 month were sent a second cover letter, response form, and reminder letters addressed to their patients. After the 6-month observation period, an identical mailing was sent to the physicians of patients in the control group to ensure their physicians were aware of the potential need for colonoscopy if clinically appropriate.
Outcomes
The primary study outcome was the proportion of patients receiving colonoscopy during the 6-month observation period (May 1–October 31, 2006) in the intervention and control groups. The secondary outcome was the proportion of patients with a new adenoma or cancer detected during this period. Colonoscopies were ascertained from automated extracts of the electronic health records of Brigham and Women’s Hospital and Harvard Vanguard Medical Associates by data analysts who were blinded to the patients’ allocation to the intervention or control groups.
To verify the accuracy of colonoscopy data and ascertain histologic findings of associated polypectomies or biopsies, 2 resident physicians who were blinded to the patients’ randomization status visually reviewed the electronic health records of all patients for the 6-month observation period. Furthermore, to identify patients who underwent a colonoscopy procedure from January 2001 through March 2006 that was missed by the automated review of electronic records when patients’ eligibility was ascertained, these physicians also visually reviewed all patients’ medical records for this preceding period. Patients who underwent a colonoscopy during this earlier period would have been ineligible for our study if their prior procedure was evident with automated record review, but they were included in our intention-to-treat analysis.
Statistical Analysis
We compared the distributions of age, sex, and years since prior colonoscopies for the intervention and control groups in the full cohort and within each of the 2 participating health care organizations. To assess intervention effects, we compared the proportions of patients who underwent colonoscopy and who had a new adenoma or cancer detected in the intervention and control groups using the Cochran–Mantel–Haenszel chi-square test to adjust for randomization by patients’ age, sex, and health care organization. To assess the consistency of intervention effects between these 3 respective pairs of strata, we compared a priori stratified subgroup analyses of colonoscopy use by patients’ age (<65 versus ≥65 years), sex, and health care organization, using the Breslow–Day test.
In descriptive analyses, we assessed responses reported by physicians to reminders for patients in the intervention group. For both the intervention and control groups, we analyzed the proportions of patients who had colonoscopy during January 2001 through March 2006 that was only detected by a visual review of electronic medical records after the 6-month observation period was completed. SAS statistical software (version 8.2, Cary, NC, USA) was used for all analyses, and two-tailed P values are reported for all statistical tests.
RESULTS
Patient Characteristics
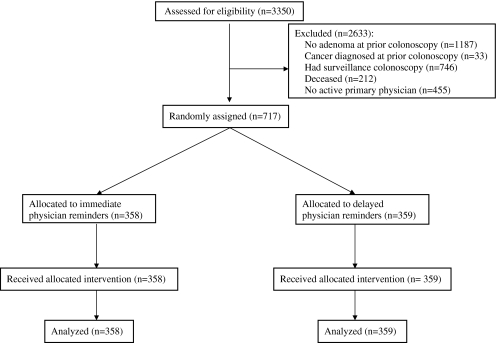
From the hospital’s endoscopy database, we identified 3,350 patients who had a colonoscopy with polypectomy performed during 1995 through 2000 but did not have a subsequent colonoscopy recorded during 2001 through March 2006 (Fig. 1). Of these 3,350 patients, we excluded 2,633 patients who were ineligible for the following reasons: (1) 1,187 patients who did not have an adenoma on the pathology report from their initial colonoscopy, (2) 33 patients who had colorectal cancer on their initial colonoscopy, (3) 746 patients who had a subsequent colonoscopy noted in the electronic records of the integrated group practice, (4) 212 patients listed as deceased in electronic records, and (5) 455 patients who did not have an active primary physician listed in electronic records.
Figure 1.
Study flow diagram.
The remaining 717 patients comprised the study cohort, including 375 patients in the hospital-affiliated practices and 342 patients in the integrated group practice. Among these 717 patients, 358 were randomized to the intervention group and 359 to the control group. No statistically significant differences were noted between the 2 groups in their age, sex, or time elapsed since the index colonoscopy (Table 1).
Table 1.
Characteristics of Patients with Prior Colorectal Adenomas by Randomized Group and Site of Primary Care
| Patient characteristics | Intervention* | Control† | P value‡ |
|---|---|---|---|
| Full cohort | N = 358 | N = 359 | |
| Mean age in years (SD) | 69.2 (12.0) | 69.2 (12.3) | 0.98 |
| Age ≥65 years (%) | 223 (62.3) | 226 (63.0) | 0.85 |
| Female sex (%) | 161 (45.0) | 171 (47.6) | 0.48 |
| Mean years since prior colonoscopy (SD) | 6.7 (1.3) | 6.8 (1.3) | 0.45 |
| Hospital-affiliated practices | N = 187 | N = 188 | |
| Mean age in years (SD) | 69.2 (11.2) | 69.0 (12.2) | 0.92 |
| Age ≥65 years (%) | 114 (61.0) | 111 (59.0) | 0.70 |
| Female sex (%) | 100 (53.5) | 101 (53.7) | 0.96 |
| Mean years since prior colonoscopy (SD) | 6.5 (1.2) | 6.6 (1.4) | 0.19 |
| Integrated group practice | N = 171 | N = 171 | |
| Mean age in years (SD) | 69.3 (13.0) | 69.4 (12.4) | 0.94 |
| Age ≥65 years (%) | 109 (63.7) | 115 (67.3) | 0.49 |
| Female sex (%) | 61 (35.7) | 70 (40.9) | 0.32 |
| Mean years since prior colonoscopy (SD) | 6.9 (1.4) | 6.9 (1.3) | 0.84 |
*Patients whose primary care physicians received mailings about the potential need for surveillance colonoscopy immediately before the 6-month observation period
†Patients whose primary care physicians received mailings about the potential need for surveillance colonoscopy after the 6-month observation period
‡Using the Student’s t test for mean age and years since prior colonoscopy and the Pearson χ2 test for dichotomous age and sex
Use of Colonoscopy and Detection of New Adenomas
Among the 358 patients whose physicians received reminders, 33 (9.2%) underwent colonoscopy within 6 months, compared with 16 (4.5%) of the 359 patients whose physicians did not receive reminders (P = 0.009). Consistent with this overall effect, colonoscopy rates for intervention patients were about double those of control patients in all prespecified subgroups defined by health care organization, patient age, and sex (Table 2). The magnitude of this effect did not differ statistically within each pair of subgroups (all P > 0.60 by Breslow–Day test).
Table 2.
Completion of Follow-up Colonoscopy within 6 Months by Randomized Group
| Intervention* | Control† | P value | ||
|---|---|---|---|---|
| Full cohort | 33/358 (9.2%) | 16/359 (4.5%) | 0.009‡ | |
| Pre-specified subgroups | ||||
| Hospital-affiliated practices | 16/187 (8.6%) | 8/188 (4.3%) | 0.07‡ | 0.92§ |
| Integrated group practice | 17/171 (9.9%) | 8/171 (4.7%) | 0.06‡ | |
| Patients Age <65 | 14/135 (10.4%) | 7/133 (5.3%) | 0.10‡ | 0.91§ |
| Patients Age ≥65 | 19/223 (8.5%) | 9/226 (4.0%) | 0.04‡ | |
| Women | 18/161 (11.2%) | 8/171 (4.7%) | 0.02‡ | 0.61§ |
| Men | 15/197 (7.6%) | 8/188 (4.3%) | 0.16‡ | |
*Patients whose primary physicians received mailings about the potential need for surveillance colonoscopy immediately before the 6-month observation period
†Patients whose primary physicians received mailings about the potential need for surveillance colonoscopy after the 6-month observation period
‡Using the Cochran-Mantel-Haenszel χ2 test to adjust for patients’ site of care, age, and sex in the full cohort and within each prespecified subgroup
§Using the Breslow–Day test for comparisons of intervention effects between pairs of subgroups defined by site of care, age, and sex
New adenomas or cancer were detected in 14 (3.9%) of the intervention patients and 6 (1.7%) of the control patients (P = 0.06). Among the 33 patients in the intervention group and 16 patients in the control group who underwent colonoscopy, 42.4% and 37.5% of these patients, respectively, had new adenomas detected. High-risk pathologic findings (adenomas ≥1.0 cm, ≥3 adenomas, high-grade dysplasia, or adenocarcinoma) were detected in 4 intervention patients and 3 control patients during the 6-month observation period, including 1 cancer in each group.
In the visual review of all electronic health records after the observation period, 161 (22.5%) of the 717 study patients were found to have had a colonoscopy during January 2001 through March 2006 that was not ascertained from electronic data before the intervention, including 75 (20.9%) of 358 patients in the intervention group and 86 (24.0%) of 359 patients in the control group. These 161 patients included 112 (29.9%) of 375 patients in the hospital-affiliated practices and 49 (14.3%) of 342 patients in the integrated group practice. If these patients had been excluded a priori from our study, the rates of colonoscopy in the intervention and control groups would have been slightly higher (11.7% and 5.9%, respectively, P = 0.01).
Responses to mailed letters were received from 119 (84.4%) of 141 physicians who cared for 269 (75.1%) of 358 patients in the intervention group. Among these 269 patients, physicians intended to recommend colonoscopy for 100 patients (37.2%) but not for the other 169 patients. This latter group included 14 (5.2%) who were deceased, 48 (17.8%) who had already completed surveillance colonoscopy, 32 (11.9%) who were not appropriate for colonoscopy because of severe comorbid illness, advanced age, or prior refusal, and 75 (27.9%) who were no longer active in their practice.
DISCUSSION
In this randomized controlled study, the use of surveillance colonoscopy for patients with prior colorectal adenomas increased during the 6 months after patient-specific reminders were provided to their primary physicians. The intervention was similarly effective in practices affiliated with an academic medical center and an integrated group practice, as well as for elderly and nonelderly patients and for women and men. New adenomas or cancer were detected in about 40% of all patients who underwent surveillance colonoscopy.
Prior randomized studies have assessed the effect of personalized reminders from physicians to their patients to promote cancer screening, but these studies have typically focused on average-risk patients rather than the higher-risk patients we studied.15 Most studies of strategies to encourage appropriate follow-up of abnormal cancer-screening tests have focused on Pap tests and mammograms.16,17 One study of patients with abnormal fecal occult blood tests reported increased rates of complete diagnostic evaluations with colonoscopy or flexible sigmoidoscopy and barium enema after an educational outreach program and patient-specific reminders were provided to physicians.18 Our study builds on this prior research by using electronic clinical databases of health care organizations to identify eligible patients and by focusing on long-term follow-up of adenomatous polyps instead of more immediate follow-up of other abnormal cancer-screening tests.
Our study had several limitations that may have contributed to the relatively small absolute increase in use of colonoscopy after our physician reminders. First, we did not contact patients in this study directly to recommend surveillance colonoscopy or to assess their reasons for not having this procedure.
Second, we determined from a post-hoc visual review of medical records that nearly 25% of patients had actually had a follow-up colonoscopy before our intervention. This finding was more common in the hospital-affiliated practices than in the integrated medical group because more procedures were performed outside the hospital-affiliated system and thus recorded only in physicians’ notes but not in coded formats accessible by an automated review.
Third, by surveying physicians of patients in the intervention group, we learned that more than 25% of patients were no longer active in the physicians’ practices. These patients had typically not seen their former physicians for more than 5 years, and the physicians often lacked current address information to contact them about the need for surveillance colonoscopy. This finding highlights the challenge of ensuring appropriate follow-up over the extended time period required for surveillance of colorectal adenomas and the corresponding need for information systems that facilitate communication among gastroenterologists, primary physicians, and patients.
Fourth, 112 of 141 physicians who received reminders for patients in the intervention group also had patients in the control group. These physicians may have been more likely to recommend colonoscopy to their patients in the control group, particularly if the latter patients had office visits during the 6-month observation period. However, this effect was probably minimal because less than 20% of patients in the control group had an office visit during this period, and physicians had no other mechanism to identify patients who were due for surveillance colonoscopy.
Our findings may not be generalizable to other health care settings. We studied the primary care networks of 2 large health care organizations with well-established electronic health record systems in 1 state.19 Thus, the effects of physician and patient reminders for surveillance colonoscopy should be assessed in other geographic areas and health care organizations, such as smaller physician groups.20 Nonetheless, our study has important implications for efforts to monitor and improve the quality of colorectal cancer screening.
Because we encountered challenges in using electronic clinical data to identify patients who needed follow-up colonoscopies, other organizations should strive to bolster the accuracy of requisite data in electronic records when implementing reminders to physicians about patients who appear due for surveillance colonoscopy. Recent studies of patients with coronary artery disease or congestive heart failure have found that automated reviews of electronic records are accurate for some but not all quality indicators.21,22 Similarly, we found that adenomatous polyps could be detected by an automated review of electronic pathology reports with a very high degree of accuracy, but our ability to ascertain colonoscopies was much less effective because many procedures were only recorded in the physicians’ notes. We also found that electronic data were incomplete for identifying patients who had left physicians’ practices or died during the preceding 5 years. Reminder systems, whether electronic or paper based, may be more effective if gastroenterologists or primary physicians prospectively identify and monitor patients who will need surveillance colonoscopy when adenomas are initially detected, rather than relying on retrospective electronic data linkages 5 to 10 years later as our study did.
Recent surveys of primary physicians, gastroenterologists, and general surgeons suggest many physicians may be recommending surveillance colonoscopy too frequently for low-risk patients, such as those with only hyperplastic polyps or a single small adenoma,23,24 thereby straining available resources for colonoscopic screening and surveillance.25 Patients with 3 or more adenomas, any adenoma greater than or equal to 1.0 cm, or any high-grade dysplasia face the greatest risk of developing colorectal cancer.26 Thus, reminder systems to promote this procedure should focus on these high-risk patients who are most likely to benefit from colonoscopy in the absence of severe comorbid illnesses.27–29
Because patients who have had colorectal adenomas remain at increased risk of developing recurrent adenomas and colorectal cancer, effective systems are needed to remind physicians and patients of prior abnormal findings so that clinically appropriate patients undergo surveillance colonoscopy. Our study provides a model with important lessons for other health care organizations considering the use of electronic clinical data to identify patients in need of this procedure, monitor whether they are receiving it, and remind primary physicians about its appropriate use.
Acknowledgments
We are grateful to David H. Stockwell, M.D., M.P.H. for advice on the study design; Julie Fiskio and James Morrissey for providing electronic data from Brigham and Women’s Hospital and Harvard Vanguard Medical Associates, respectively; Deborah Collins for coordinating the study mailings to physicians and tabulating their responses; Asaf Bitton, M.D. and Jeffrey Kullgren, M.D., M.P.H. for reviewing medical records; and Robert E. Wolf, M.S. for assisting with statistical analyses. This study was supported by a grant (R21-CA112365) from the National Cancer Institute.
Conflict of Interest None disclosed.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006;56:106–130. doi: 10.3322/canjclin.56.2.106. [DOI] [PubMed] [Google Scholar]
- 2.Toribara NW, Sleisenger MH. Screening for colorectal cancer. N Engl J Med. 1995;332:861–867. doi: 10.1056/NEJM199503303321306. [DOI] [PubMed] [Google Scholar]
- 3.Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med. 1993;329:1977–1981. doi: 10.1056/NEJM199312303292701. [DOI] [PubMed] [Google Scholar]
- 4.Citarda F, Tomaselli G, Capocaccia R, Barcherini S, Crespi M. Efficacy in standard clinical practice of colonoscopic polypectomy in reducing colorectal cancer incidence. Gut. 2001;48:812–815. doi: 10.1136/gut.48.6.812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winawer SJ, Zauber AG, O’Brien MJ, et al. Randomized comparison of surveillance intervals after colonoscopic removal of newly diagnosed adenomatous polyps. The National Polyp Study Workgroup. N Engl J Med. 1993;328:901–906. doi: 10.1056/NEJM199304013281301. [DOI] [PubMed] [Google Scholar]
- 6.Winawer S, Fletcher R, Rex D, et al. Colorectal cancer screening and surveillance: clinical guidelines and rationale-Update based on new evidence. Gastroenterology. 2003;124:544–560. doi: 10.1053/gast.2003.50044. [DOI] [PubMed] [Google Scholar]
- 7.Yabroff KR, Washington KS, Leader A, Neilson E, Mandelblatt J. Is the promise of cancer-screening programs being compromised? Quality of follow-up care after abnormal screening results. Med Care Res Rev. 2003;60:294–331. doi: 10.1177/1077558703254698. [DOI] [PubMed] [Google Scholar]
- 8.Maviglia SM, Teich JM, Fiskio J, Bates DW. Using an electronic medical record to identify opportunities to improve compliance with cholesterol guidelines. J Gen Intern Med. 2001;16:531–537. doi: 10.1046/j.1525-1497.2001.016008531.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sequist TD, Gandhi TK, Karson AS, et al. A randomized trial of electronic clinical reminders to improve quality of care for diabetes and coronary artery disease. J Am Med Inform Assoc. 2005;12:431–437. doi: 10.1197/jamia.M1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shah NR, Seger AC, Seger DL, et al. Improving acceptance of computerized prescribing alerts in ambulatory care. J Am Med Inform Assoc. 2006;13:5–11. doi: 10.1197/jamia.M1868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Linder JA, Chan JC, Bates DW. Evaluation and treatment of pharyngitis in primary care practice: the difference between guidelines is largely academic. Arch Intern Med. 2006;166:1374–1379. doi: 10.1001/archinte.166.13.1374. [DOI] [PubMed] [Google Scholar]
- 12.Pereira AG, Kleinman KP, Pearson SD. Leaving the practice: effects of primary care physician departure on patient care. Arch Intern Med. 2003;163:2733–2736. doi: 10.1001/archinte.163.22.2733. [DOI] [PubMed] [Google Scholar]
- 13.Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166:675–681. doi: 10.1001/archinte.166.6.675. [DOI] [PubMed] [Google Scholar]
- 14.Sequist TD, Marshall R, Lampert S, Buechler EJ, Lee TH. Missed opportunities in the primary care management of early acute ischemic heart disease. Arch Intern Med. 2006;166:2237–2243. doi: 10.1001/archinte.166.20.2237. [DOI] [PubMed] [Google Scholar]
- 15.Stone EG, Morton SC, Hulscher ME, et al. Interventions that increase use of adult immunization and cancer screening services: a meta-analysis. Ann Intern Med. 2002;136:641–651. doi: 10.7326/0003-4819-136-9-200205070-00006. [DOI] [PubMed] [Google Scholar]
- 16.Yabroff KR, Kerner JF, Mandelblatt JS. Effectiveness of interventions to improve follow-up after abnormal cervical cancer screening. Prev Med. 2000;31:429–439. doi: 10.1006/pmed.2000.0722. [DOI] [PubMed] [Google Scholar]
- 17.Bastani R, Yabroff KR, Myers RE, Glenn B. Interventions to improve follow-up of abnormal findings in cancer screening. Cancer. 2004;101:1188–1200. doi: 10.1002/cncr.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Myers RE, Hyslop T, Gerrity M, et al. Physician intention to recommend complete diagnostic evaluation in colorectal cancer screening. Cancer Epidemiol Biomarkers Prev. 1999;8:587–593. [PubMed] [Google Scholar]
- 19.Jha AK, Ferris TG, Donelan K, et al. How common are electronic health records in the United States? A summary of the evidence. Health Aff (Millwood) 2006;25:w496–w507. doi: 10.1377/hlthaff.25.w496. [DOI] [PubMed] [Google Scholar]
- 20.Simon SR, Kaushal R, Cleary PD, et al. Physicians and electronic health records: a statewide survey. Arch Intern Med. 2007;167:507–512. doi: 10.1001/archinte.167.5.507. [DOI] [PubMed] [Google Scholar]
- 21.Persell SD, Wright JM, Thompson JA, Kmetik KS, Baker DW. Assessing the validity of national quality measures for coronary artery disease using an electronic health record. Arch Intern Med. 2006;166:2272–2277. doi: 10.1001/archinte.166.20.2272. [DOI] [PubMed] [Google Scholar]
- 22.Baker DW, Persell SD, Thompson JA, et al. Automated review of electronic health records to assess quality of care for outpatients with heart failure. Ann Intern Med. 2007;146:270–277. doi: 10.7326/0003-4819-146-4-200702200-00006. [DOI] [PubMed] [Google Scholar]
- 23.Mysliwiec PA, Brown ML, Klabunde CN, Ransohoff DF. Are physicians doing too much colonoscopy? A national survey of colorectal surveillance after polypectomy. Ann Intern Med. 2004;141:264–271. doi: 10.7326/0003-4819-141-4-200408170-00006. [DOI] [PubMed] [Google Scholar]
- 24.Boolchand V, Olds G, Singh J, Singh P, Chak A, Cooper GS. Colorectal screening after polypectomy: a national survey study of primary care physicians. Ann Intern Med. 2006;145:654–659. doi: 10.7326/0003-4819-145-9-200611070-00007. [DOI] [PubMed] [Google Scholar]
- 25.Brown ML, Klabunde CN, Mysliwiec P. Current capacity for endoscopic colorectal cancer screening in the United States: data from the National Cancer Institute Survey of Colorectal Cancer Screening Practices. Am J Med. 2003;115:129–133. doi: 10.1016/S0002-9343(03)00297-3. [DOI] [PubMed] [Google Scholar]
- 26.Winawer SJ, Zauber AG, Fletcher RH, et al. Guidelines for colonoscopy surveillance after polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer and the American Cancer Society. Gastroenterology. 2006;130:1872–1885. doi: 10.1053/j.gastro.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 27.Noshirwani KC, Stolk RU, Rybicki LA, Beck GJ. Adenoma size and number are predictive of adenoma recurrence: implications for surveillance colonoscopy. Gastrointest Endosc. 2000;51:433–437. doi: 10.1016/S0016-5107(00)70444-5. [DOI] [PubMed] [Google Scholar]
- 28.Saini SD, Kim HM, Schoenfeld P. Incidence of advanced adenomas at surveillance colonoscopy in patients with a personal history of colon adenomas: a meta-analysis and systematic review. Gastrointest Endosc. 2006;64:614–626. doi: 10.1016/j.gie.2006.06.057. [DOI] [PubMed] [Google Scholar]
- 29.Gross CP, McAvay GJ, Krumholz HM, Paltiel AD, Bhasin D, Tinetti ME. The effect of age and chronic illness on life expectancy after a diagnosis of colorectal cancer: implications for screening. Ann Intern Med. 2006;145:646–653. doi: 10.7326/0003-4819-145-9-200611070-00006. [DOI] [PubMed] [Google Scholar]