Abstract
Context
Growing evidence suggests that most forms of distrust are multidimensional, including domains of technical competence and value congruence. Prior measures of health care system distrust have not reflected this multidimensional structure and may be limiting research into the role of health care system distrust in health and health care in the US.
Objective
To develop a revised a scale of health care system distrust.
Design
Three phase study, including focus groups, pilot testing and a cross-sectional telephone survey.
Participants
A total of 404 individuals recruited directly from the Greater Philadelphia area or through the University of Pennsylvania Health System.
Results
Multilevel consensus coding of focus group transcripts identified 2 primary domains of competence and values with the values domain having subthemes of honesty, motives, and equity. Iterative testing of the initial 76 items led to a final scale of 9 items with a Cronbach’s alpha of 0.83. Factor analysis demonstrated a 2-factor structure, corresponding to the domains of values and competence. The values subscale (5 items) had a Cronbach’s alpha of 0.73 and the competence subscale (4 items) had a Cronbach’s alpha of 0.77. These psychometric properties were similar among African Americans and Whites.
Conclusions
A novel 9-item scale of Health Care System Distrust with high reliability allows the assessment of the 2 primary domains of distrust (values and competence) and may facilitate research in this area.
KEY WORDS: health care system, technical competence, distrust, values
INTRODUCTION
In recent years, a growing body of theoretical and empirical evidence suggests that health care related distrust may impede individuals from seeking appropriate medical care, adhering to medical recommendations, and maintaining continuity of care.1–5 Moreover, health care distrust is commonly cited as an important contributor to racial disparities in health and health care, an issue that has become a national priority for health research and health care delivery.6–10 Although evidence from other disciplines would suggest that social or institutional trust may play a particularly important role in these relationships, most prior studies of health care have examined trust in personal physicians—a type of interpersonal trust.11 Relatively few studies have examined institutional or social forms of health care–related distrust, such as distrust of the health care system.
The ability to measure a relatively abstract concept such as institutional trust remains an important barrier to research in this area. Prior studies of institutional trust in health care often use a variety of instruments that focus on a single type of institution, e.g., health insurer or hospital, and provide relatively limited insight into attitudes about the health care system as a whole.7,11–14 Our prior scale of Health Care System Distrust assessed general beliefs about the health care system but had relatively low reliability and was more closely tied to scales of provider trust rather than formative work around institutional trust.15
A fundamental concern about prior measures of health care–related trust and distrust is that they have been unable to identify more than a single dimension of distrust. These unidimensional measures stand in contrast to the widespread support in the literature for the multidimensional nature of trust and distrust—both in the area of health care and in other areas of society. Furthermore, this empirical and theoretical evidence not only supports the concept of trust as multidimensional, but is increasingly converging on a model of 2 primary dimensions—one related to perceptions of value congruence and the second to perceptions of competence. This model, initially proposed by Hovland, Janis, and Kelley16 has been supported by multiple studies in health care17–22 and in other areas 23–30—and also has the benefit of making conceptual sense. If trust is defined as the belief that some entity will act in one’s interest in the future, trust then requires the perception that the entity is capable of doing what is needed (technical competence) and the perception that that the entity wants to do what is needed (value congruence).
Given this background, the purpose of this study was to revise our prior scale to develop a multidimensional instrument to assess Health Care System Distrust. Specifically, making content validity our priority, we sought to use qualitative methodologies to initially define scale content and then use quantitative processes to solidify and further define the emergent themes. In this work, we particularly focused on whether we could identify dimensions corresponding to the concepts of technical competence and value congruence, whether these dimensions were supported by psychometric testing, and whether the content generated through qualitative processes included domains other than technical competence and value congruence.
METHODS
We conducted a 3-phase study to develop a revised scale of health care system distrust. In the first phase, we explored understanding and acceptance of our conceptual model of distrust and generated scale items through focus groups. In the second phase, we constructed, revised, and tested 75 items using expert opinion and think-aloud exercises. In the third phase, we piloted 26 potential items in a telephone survey to establish the psychometric characteristics of the final scale. Additional details of each phase are described below.
Phase 1. Focus Groups We held a total of 12 focus groups with 115 individuals of diverse racial/ethnic backgrounds from the greater Philadelphia area. Six groups were conducted in Spanish. We wanted to insure that we included topics/issues important to Hispanics, in the event their ideas and experiences were different from those of other backgrounds. Development of a Spanish version of the instrument was planned for later, pending successful development in English.
The script for the focus group guided the discussion through 4 topics: 1) definition of a health care system and its multiple components; 2) consideration of whether trust and distrust were opposite ends of 1 continuum or distinct domains; 3) elements/actions that lead to and are associated with distrust; and 4) elements/actions that are associated with trust. Conversations for all groups were audiotaped and transcribed. The technique of Multilevel Consensus Coding was used to identify themes and refine the conceptual model.31 Each transcript was read by at least 3 of the study investigators, each of whom identified major themes and subthemes. Investigator meetings were used to review these themes and subthemes and resolve differences in coding or interpretation.
Phase 2: Item Reduction In the second phase, we pilot tested the 75 items derived in Phase I interviews with 34 patients in waiting rooms of primary care practices. Item retention was based on cognitive testing (including think-aloud exercises), response distributions, and domain/dimension representation. Specifically, patients were invited to complete a written survey while they were waiting. If they agreed, a trained research assistant sat with them as they completed the survey going through each item to see if the questions were confusing, hard to answer, ambiguously or strangely worded, or redundant, and asking if the respondent had suggestions for better wording. In some cases, the respondent was asked to give the question in their own words, as a validity check. Later, all research assistants met to discuss the feedback that had been received. Preliminary item statistics, looking at the percent of who chose each option, were also conducted with the goal of deleting items with little or no variability as such items would not be helpful for future predictive studies. The study team reviewed the think-aloud results and preliminary item statistics and made decisions for item retention balancing the goals of creating a brief instrument yet retaining items that appeared to fit the themes identified in the focus groups and our conceptual model.
Phase 3: Psychometric Analyses and Further Item Reduction In the third phase, we conducted a telephone survey to explore the psychometric characteristics of the final scale (reported here) and to test hypotheses about the relationship between distrust and race.32 We selected a random sample of 845 individuals over the age of 18 who had been seen at a primary care practice or emergency department with the University of Pennsylvania Health System in the past 3 years. Individuals were eligible if they spoke English and were able to complete a 15-minute interview. From this sample, 264 participated in the interview, 118 refused to participate, 192 were never reached, 49 were not eligible, and 222 numbers were disconnected, for a response rate of 45.8%. From the 264 interviews, 9 participants did not provide information on race/ethnicity and were excluded from the study population, leaving a final sample of 255 participants. Responders were slightly more likely to be women, older and insured.32
The telephone interviews were spread over days of the week and times of the day. The telephone interviewers were racially diverse, but no attempt was made to match respondent and interviewer race. The primary measures were: a) Health Care System Distrust, the 26-item scale resulting from Phase 2, b) the Physician Trust Subscale of the Primary Care Assessment Survey, c) a global item assessing trust in the health care system, and d) a global item assessing general social trust from the General Social Survey.33 Data for Race/Ethnicity were based on items from the 2000 US Census survey, wherein participants were asked first about Hispanic ethnicity and then about their racial background. For the purposes of this analysis, we categorized participants as black-non Hispanic, white-non Hispanic, Hispanic, or other.
Analyses began with examining item level response options, looking at missing data and item response distributions. Subsequently, we went through iterative sequences of item selection/reduction analyses involving examination of item–item and item–total correlations, Cronbach alpha coefficients, and rotated factor structures for subsets of items. These analyses were completed first in the overall sample and then within each racial subgroup. Data analysis was performed using STATA 8.2.
RESULTS
Phase 1 Table 1 provides a summary of the demographic characteristics of the 115 focus group participants. About 70% of the focus group participants were women, with an overall average age of 47.4 years. By design, we included participants who self-defined as Black, Latino, and White. We achieved a planned distribution in race/ethnicity and a reasonably broad distribution in education. The results of the groups demonstrated that: (1) the term “health care system” was understood by participants with the most common definition including hospitals, community clinics, labs, insurance companies, and drug companies; (2) competence and values were key domains of health care system distrust with dimensions of honesty, motives, and equity within the domain of values; and (3) issues of communication/interpersonal skills were also important but were more closely tied to the immediate sense of satisfaction with the encounter than enduring distrust. Concern about confidentiality or privacy was cited by only a few participants. Using the focus group transcripts and previously published scales, we then developed 75 items encompassing the domains of values and competence and the dimensions within the values domain.
Table 1.
Phase I Focus Group Participant Characteristics
| Total # | Mean age | Education | ||||
|---|---|---|---|---|---|---|
| <HS | HS Grad | < College | ≥College | |||
| Male | 33 | 49.6 | 6 | 5 | 11 | 11 |
| Black | 19 | 40.2 | 3 | 4 | 6 | 6 |
| Latino | 6 | 62.4 | 3 | 1 | 0 | 2 |
| White | 5 | 61.0 | 0 | 0 | 2 | 3 |
| Other | 3 | 57.0 | 0 | 0 | 3 | 0 |
| Female | 82 | 46.4 | 22 | 23 | 17 | 20 |
| Black | 25 | 47.4 | 1 | 8 | 9 | 7 |
| Latino | 43 | 45.8 | 21 | 14 | 4 | 4 |
| White | 13 | 46.5 | 0 | 1 | 3 | 9 |
| Other | 1 | 48.0 | 0 | 0 | 1 | 0 |
| Overall | 115 | 47.4 | 28 | 28 | 28 | 31 |
Important decisions by the study team that overlaid the content were: item stems would be presented as declarative statements; some, but not all, item stems would include the term health care system; response options would ask for endorsement of stems on a 5-point scale ranging from strongly disagree to strongly agree; stems would be presented so that sometimes an “agree” response would signal more health care system distrust and for some stems a disagree would signal distrust; items would be framed in the present tense and using the third person (i.e., “patients”). During this phase the study team also arrived at a definition of health care system distrust to be placed in the introduction of the instrument: “By Health Care System I mean: hospitals, community clinics, and labs as well as organizations involved in health such as insurance companies and drug companies. I am not including people such as doctors, nurses, specialists, x-ray technicians, medicines, or office staff. I am just talking about the organizations that are a part of your health care.”
Phase 2 In Phase 2, we reduced the set of items from 75 to 26 through 1-on-1 patient interviews and investigator team review, polling, and discussion. Items were deleted for 1 or more of the following reasons: 1) little or no variability in responses; 2) cognitive interviews suggested the item was not well understood or that people could answer for themselves but had no idea how the content applied to others; or 3) the study team was dissatisfied with the wording or redundancy of the item.
Phase 3 In Phase 3, we conducted a cross-sectional survey of 255 individuals to select the final scale. The sample was comprised of 144 (56%) Black, 92 (36%) White, and 19 (8%) respondents from other ethnic/racial groups. The mean age of the respondents was 47.8 years (range 22–75). There were expected differences in education (p < .0005) and household income (p < .0005) with higher levels of both reported by whites (Table 2).
Table 2.
Phase 3 Survey participant characteristics
| Overall | Blacks | Whites | Other | p value | |
|---|---|---|---|---|---|
| (n = 255) | (n = 144) | (n = 92) | (n = 19) | ||
| Mean age, yrs. (range) | 47.8 (22–75) | 46.9 (22–75) | 49.0 (31–69) | 48.3 (31–66) | .16 |
| Female (%) | 73.3 | 80.4 | 63.3 | 66.7 | .004 |
| Education (%) | |||||
| Less than high school | 41.8 | 62.0 | 14.3 | 22.2 | <.0005 |
| High school degree | 23.9 | 28.9 | 17.6 | 16.7 | |
| College degree or higher | 34.3 | 9.1 | 68.2 | 61.1 | |
| Household Income (%) | |||||
| < $20,000 | 21.2 | 32.6 | 6.5 | 5.3 | <.0005 |
| $20,000–$59,999 | 34.5 | 43.8 | 18.5 | 42.1 | |
| $60,000 or higher | 27.9 | 7.6 | 58.7 | 31.6 | |
| Missing | 16.5 | 16.0 | 16.3 | 21.0 | |
Based on the sequential iterative item analyses, a scale of Health Care System Distrust including 8 items was initially selected (Table 3—excluding item 7). This scale had relatively high internal consistency with a Cronbach’s alpha of 0.83 and item total correlations of 0.5–0.7. Principal components analysis supported the existence of 2 subscales consistent with the hypothesized domains of competence (Cronbach alpha 0.77) and values (Cronbach alpha 0.73). Items 1, 3, 4, and 6 had rotated loadings of 0.42–0.80 on the first factor. Items 2, 5, 8, and 9 had rotated loadings of 0.48–0.83 on the second factor (Table 3). All of the items had loadings less than 0.4 on the other factor except for item 4, which also loaded on the values factor. However, because it was conceptually closer to the competence factor, it was retained in the competence subscale score. Review of the 8 item scale demonstrated that the subtheme of equity was no longer represented in the scale and that a single item was included that began with the stem “Patients...” rather than “The health care system...”. Thus, an additional item (item 7) that began with the stem “Patients...” and mapped to the equity subtheme was added to the scale to create the final 9-item scale. Item 7 was conceptually part of the values domain and was included in that subscale. The final Cronbach’s alphas were 0.85 for the 9-item scale and 0.75 for the 5-item values subscale. The minimum score for the full scale was 9 and for both subscales was 5. The maximum score for the full scale was 45, 25 for the values subscale, and 20 for the competence subscale.
Table 3.
Rotated Factor Loadings Overall and by Race
| Overall | Black | White | |||||
|---|---|---|---|---|---|---|---|
| Full scale | C | V | C | V | C | V | |
| 1. The Health Care System does its best to make patients’ health better* | C | .77 | .21 | .76 | .17 | .78 | .21 |
| 2. The Health Care System covers up its mistakes | V | .32 | .63 | .37 | .65 | .38 | .68 |
| 3. Patients receive high quality medical care from the Health Care System* | C | .80 | .15 | .86 | −.04 | .84 | .22 |
| 4. The Health Care System makes too many mistakes | C | .42 | .57 | .50 | .44 | .40 | .67 |
| 5. The Health Care System puts making money above patients’ needs | V | .38 | .48 | .61 | .47 | .05 | .66 |
| 6. The Health Care System gives excellent medical care* | C | .80 | .20 | .79 | .09 | .80 | .22 |
| 7. Patients get the same medical treatment from the Health Care System, no matter what the patient’s race or ethnicity*# | V | .64 | .31 | .52 | .34 | .60 | .43 |
| 8. The Health Care System lies to make money | V | .29 | .76 | .18 | .78 | .48 | .63 |
| 9. The Health Care System experiments on patients without them knowing | V | .05 | .83 | −.14 | .80 | .24 | .77 |
* Item is reverse scored
# Item added after factor analysis
Items are answered on a scale where 1 = strongly disagree and 5 = strongly agree
C competence, V values
Factor analysis among both major racial subgroups demonstrated the same 2 factor structure as in the overall sample with similar patterns of factor loadings across the items (Table 3). The overall scale and the 2 subscales had relatively high internal consistency among whites (α: 0.87 overall scale, 0.79 competence subscale, 0.77 values subscale) and among African Americans (α: 0.82 overall scale, 0.77 competence subscale, 0.73 values subscale). Disattenuated correlations between the subscales were 0.88 for the total group, 0.71 for whites, and 0.97 for African Americans.
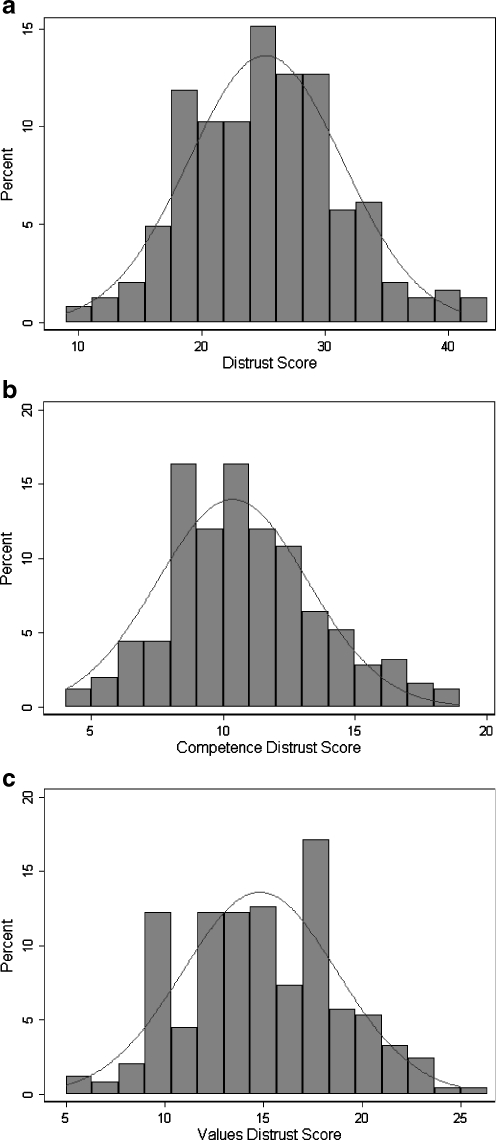
Scores on the overall scale and the 2 subscales were normally distributed (Fig. 1). Within the total group, the values and competence subscale scores were inversely correlated with the Physician Trust Subscale of the Primary Care Assessment Survey (Pearson Correlation Coefficients [PCC] −0.30 and −0.33), a global item assessing trust in the health care system (PCC −0.42 and −0.55) and a global item assessing general social trust from the General Social Survey (PCC −0.35 and −0.27). Parallel results were seen within African Americans: correlations with the Physician Trust Subscale of the Primary Care Assessment Survey (PCC −0.30 and −0.38), the global item assessing trust in the health care system (PCC −0.46 and −0.49) and a global item assessing general social trust from the General Social Survey (PCC −0.38 and −0.37), for the values and competence subscales, respectively. Among whites, the values and competence subscale scores also inversely correlated with the Physician Trust Subscale of the PCAS (PCC −0.25 and −0.30), and a global item assessing trust in the health care system (PCC −0.38 and −0.56) but less so with the global item assessing general social trust from the General Social Survey (PCC −0.20 and −0.09).
Figure 1.
Distribution of Health Care System Distrust total score (a) and Competence (b) and Values (c) domains.
DISCUSSION
Although health care–related distrust may be an important contributor to problems in health and health care in the US, the empirical evidence about distrust is limited and often conflicting. In this study, we present a revised scale of health care system distrust that includes 2 primary domains (values and competence). Multiple focus groups with individuals representing various sociodemographic strata replicated our earlier findings that the construct of “the health care system” enjoys a shared understanding.15 More importantly for extending empirical work in the field, the text from the focus groups and the follow-up psychometric analyses suggest quite strongly that health care system distrust is comprised of the 2 domains. Importantly, the domains were observed for both samples of black and white respondents. Moreover, scores on the scales were related as expected to scores on measures of physician trust, a global item assessing trust in the health care system, and a global item assessing general social trust, lending support for construct validity of the revised scale.
There are some limitations to the study that should be noted. First, the data were collected in 1 geographic area. Although we have no hypotheses regarding why responses might be different in other parts of the country, this will ultimately need to be investigated. Second, because our ultimate focus is on racial disparities and the role distrust may play, we have not focused on other potentially important correlates, such as insurance status or health. Again, future investigations will be useful for unsorting the complex linkages. Third, we included Hispanics in the content generation phase (and did not find many unique issues), but there are many other ethnic and immigrant groups to consider.
Overall, the novel contribution of this work is that we revised and improved our original Health Care System Distrust Scale, by expanding the content generation component and specifically linking the content to the dominant conceptual model of health care trust and distrust. Content analyses, group consensus processes, and psychometric analyses confirmed the presence of 2 main factors aligned with values and competence. We anticipate this revised scale will be useful in helping understand multiple issues related to racial disparities, as well as open up new lines of study regarding, for example, stability of Health Care System Distrust, interventions to change Health Care System Distrust, and an understanding of what types of interactions with the health care system are most potent for changing reported levels of distrust.
Acknowledgments
Alex Quistberg provided valuable assistance with the Spanish-speaking focus groups. This work was supported by R01 HG02689 from the National Human Genome Research Institute and a Research Scholar Grant from the American Cancer Society.
Conflict of Interest None disclosed.
References
- 1.Whetten K, Leserman J, Whetten R, et al. Exploring lack of trust in care providers and the government as a barrier to health service use. Am J Public Health. 2006;96(4):716–21. doi: 10.2105/AJPH.2005.063255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe R, Calnan M. Trust relations in health care: developing a theoretical framework for the “new” NHS. Journal of Health Organization & Management. 2006;20(5):376–96. doi: 10.1108/14777260610701777. [DOI] [PubMed] [Google Scholar]
- 3.Armstrong K, Rose A, Peters N, Long JA, McMurphy S, Shea JA. Distrust of the health care system and self-reported health in the United States. [See comment] J Gen Intern Med. 2006;21(4):292–7. doi: 10.1111/j.1525-1497.2006.00396.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mollborn S, Stepanikova I, Cook KS. Delayed care and unmet needs among health care system users: when does fiduciary trust in a physician matter? Health Serv Res. 2005;40(6 Pt 1):1898–917. doi: 10.1111/j.1475-6773.2005.00457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thom DH, Hall MA, Pawlson LG. Measuring patients’ trust in physicians when assessing quality of care.[see comment] Health Aff. 2004;23(4):124–32. doi: 10.1377/hlthaff.23.4.124. [DOI] [PubMed] [Google Scholar]
- 6.Halbert CH, Armstrong K, Gandy OH, Jr., Shaker L. Racial differences in trust in health care providers. Arch Intern Med. 2006;166(8):896–901. doi: 10.1001/archinte.166.8.896. [DOI] [PubMed] [Google Scholar]
- 7.Boulware LE, Cooper LA, Ratner LE, LaVeist TA, Powe NR. Race and trust in the health care system. Public Health Reports. 2003;118(4):358–65. doi: 10.1016/S0033-3549(04)50262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African-American and white cardiac patients. Med Care Res Rev. 2000;57(1):146–61. doi: 10.1177/107755800773743637. [DOI] [PubMed] [Google Scholar]
- 9.Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington DC: The National Academies Press; 2002. [PubMed] [Google Scholar]
- 10.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W. The Group-Based Medical Mistrust Scale: psychometric properties and association with breast cancer screening. Prev Med. 2004;38(2):209–18. doi: 10.1016/j.ypmed.2003.09.041. [DOI] [PubMed] [Google Scholar]
- 11.Hall MA. Researching medical trust in the United States. Journal of Health Organization & Management. 2006;20(5):456–67. doi: 10.1108/14777260610701812. [DOI] [PubMed] [Google Scholar]
- 12.Goold SD, Fessler D, Moyer CA. A measure of trust in insurers. Health Serv Res. 2006;41(1):58–78. doi: 10.1111/j.1475-6773.2005.00456.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balkrishnan R, Dugan E, Camacho FT, Hall MA. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41(9):1058–64. doi: 10.1097/01.MLR.0000083743.15238.9F. [DOI] [PubMed] [Google Scholar]
- 14.Hall MA, Camacho F, Lawlor JS, Depuy V, Sugarman J, Weinfurt K. Measuring trust in medical researchers. Med Care. 2006;44(11):1048–53. doi: 10.1097/01.mlr.0000228023.37087.cb. [DOI] [PubMed] [Google Scholar]
- 15.Rose A, Shea J, Armstrong K. Development of the health care system distrust scale. J Gen Intern Med. 2004;19:57–63. doi: 10.1111/j.1525-1497.2004.21146.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hovland C, Janis I, Kelley H. Communication and Persuasion. New Haven, CT: Yale University Press; 1953. [Google Scholar]
- 17.Jacobs EA, Rolle I, Ferrans CE, Whitaker EE, Warnecke RB. Understanding African Americans’ views of the trustworthiness of physicians. J Gen Intern Med. 2006;21(6):642–7. doi: 10.1111/j.1525-1497.2006.00485.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thom D, Campbell B. Patient–physician trust: an exploratory study. J Fam Pract. 1997;44:169–76. [PubMed] [Google Scholar]
- 19.Wright EB, Holcombe C, Salmon P. Doctors’ communication of trust, care, and respect in breast cancer: qualitative study. BMJ. 2004;328(7444):864. doi: 10.1136/bmj.38046.771308.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hupcey JE, Miller J. Community dwelling adults’ perception of interpersonal trust vs. trust in health care providers. J Clin Nurs. 2006;15(9):1132–9. doi: 10.1111/j.1365-2702.2006.01386.x. [DOI] [PubMed] [Google Scholar]
- 21.Hall MA, Camacho F, Dugan E, Balkrishnan R. Trust in the medical profession: conceptual and measurement issues. Health Serv Res. 2002;37(5):1419–39. doi: 10.1111/1475-6773.01070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Klostermann BK, Slap GB, Nebrig DM, Tivorsak TL, Britto MT. Earning trust and losing it: adolescents’ views on trusting physicians. J Fam Pract. 2005;54(8):679–87. [PubMed] [Google Scholar]
- 23.Barber B. The Logic and Limits of Trust. New Jersey: Rutgers University Press; 1983. [Google Scholar]
- 24.Gambetta D. Trust: Making and Breaking Cooperative Relations. Oxford: Basil Blackwell; 1990. [Google Scholar]
- 25.Fukuyama F. Trust: the social virtues and the creation of prosperity. New York, NY: Free Press; 1995. [Google Scholar]
- 26.Lewicki RJ, McAllister D, Bies RH. Trust and distrust: new relationships and realities. Acad Manage Rev. 1998;23(3):438–58. doi: 10.2307/259288. [DOI] [Google Scholar]
- 27.Kramer RM. Trust and distrust in organizations: emerging perspectives, enduring questions. American Review of Psychology. 1999;50:569–98. doi: 10.1146/annurev.psych.50.1.569. [DOI] [PubMed] [Google Scholar]
- 28.Parker S, Parker G. Why do we trust our congressman? J Polit. 1993;55:442–53. doi: 10.2307/2132274. [DOI] [Google Scholar]
- 29.Poortinga W, Pidgeon NF. Prior attitudes, salient value similarity, and dimensionality: toward an integrative model of trust in risk regulation. J Appl Soc Psychol. 2006;36(7):1674–700. doi: 10.1111/j.0021-9029.2006.00076.x. [DOI] [Google Scholar]
- 30.Earle TC, Siegrist M. Morality information, performance information, and the distinction between trust and confidence. J Appl Soc Psychol. 2006;36(2):383–416. [Google Scholar]
- 31.Jenkins G, Merz JF, Sankar P. A qualitative study of women's views on medical confidentiality. J Med Ethics. 2005;31(9):499–504. doi: 10.1136/jme.2004.010280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.ArmstrongK,McMurphyS,DeanL, et al. Differences in the Patterns of Health Care System Distrust between Blacks and Whites. JGIM. (in press). DOI 10.1007/s11606-008-0561-9. [DOI] [PMC free article] [PubMed]
- 33.Kawachi I, Kennedy B, Glass R. Social capital and self-related health: a contextual analysis. Am J Public Health. 1999;89(8):1187–93. doi: 10.2105/ajph.89.8.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]