Abstract
Background
The Accreditation Council for Graduate Medical Education resident work hour limitations were implemented in July, 2003. Effects on faculty are not well understood.
Objective
The objective of this study was to determine the effects of the resident work hour limitations on the professional lives of faculty physicians.
Design and Participants
Survey of faculty physicians at three teaching hospitals associated with university-based internal medicine and surgery residency programs in Seattle, Washington. Physicians who attended on Internal Medicine and Surgery in-patient services during the 10 mo after implementation of work hour limitations were eligible for participation (N = 366); 282 physicians (77%) returned surveys.
Measurements
Participants were asked about the effects of resident work hour limitations on aspects of their professional lives, including clinical work, research, teaching, and professional satisfaction.
Results
Most attending physicians reported that, because of work hour limitations, they spent more time on clinical work (52%), felt more responsibility for supervising patient care (65%), and spent less time on research or other academic pursuits (51%) and teaching residents (72%). Reported changes in work content were independently associated with the self-reported probability of leaving academic medicine in the next 3 y.
Conclusions
Resident work hour limitations have had large effects on the professional lives of faculty. These findings may have important implications for recruiting and retaining faculty at academic medical centers.
KEY WORDS: resident work hours, faculty, physician turnover, academics, surgeons, internal medicine, graduate medical education, resident duty hours
INTRODUCTION
The Accreditation Council for Graduate Medical Education resident work hour limitations (WHLs) were implemented in July, 2003.1 Although effects of WHLs on residents have begun to be defined,2 effects on the professional lives of attending physicians (attendings) in academic settings are not well understood. It has been hypothesized that WHLs may shift clinical work from residents to attendings, potentially curtailing their academic productivity, lowering career satisfaction, and contributing to decisions to leave academic medicine.3 Such consequences are of particular concern given data suggesting that many faculty seriously consider leaving academic medicine.4,5 There is evidence that protected time for research is an important factor for career satisfaction among faculty and that there is an inverse correlation between career satisfaction and physician departure rates.6,7
The effects of WHLs on faculty teaching are also unknown. A shift of clinical responsibility from residents to faculty could enhance teaching by contributing to increased faculty presence and involvement. On the other hand, faculty and residents might feel the need to forfeit educational activities to meet their clinical responsibilities and comply with WHLs.3 To the extent that faculty assume the care of patients themselves, there may be lost opportunities for teaching.8
We surveyed faculty from a university department of Internal Medicine and department of Surgery. Our objectives were to determine attendings’ perceptions of the effects of WHLs on their professional lives. We hypothesized that WHLs might increase clinical time and perception of responsibility for patient care while decreasing time for the traditional academic pursuits of research and teaching. We further hypothesized that these changes might be associated with decreased long-term commitment to academic medicine.
METHODS
Participants
The study included attendings at the three major teaching hospitals affiliated with the University of Washington (UW): the University of Washington Medical Center, Harborview Medical Center (a county hospital), and Puget Sound Veterans’ Affairs Medical Center.
Internists All physicians who had attended on a general Internal Medicine service or 1 of 10 subspecialty services (cardiology, endocrinology, gastroenterology, geriatric medicine, hematology/oncology, infectious disease, neurology, pulmonary/critical care medicine, nephrology, and rheumatology) from July 1, 2003 to April 30, 2004 were identified (N = 323). Twenty-eight were subsequently excluded because contact information was not available (n = 7), they had left the UW (n = 14), or they did not have contact with residents (n = 7). The total eligible physicians was 295.
Surgeons All faculty in the UW Department of Surgery who had clinical responsibility (i.e., not full-time research faculty), including general surgery and six subspecialties (cardiothoracic, trauma, pediatric, plastic, transplantation, and vascular surgery), were included. All surgeons based at the Seattle VA Puget Sound Healthcare System were also included (with additional represented subspecialties of orthopedics, urology, ophalmology, otolaryngology, and neurosurgery). All surgical services at UW teaching hospitals participate in resident training. The total eligible physicians was 71.
The UW Human Subjects Institutional Review Board Approved all study procedures.
Data Collection
Survey items presented in this manuscript were part of a larger survey about faculty perception of effects of resident WHLs. In June and July of 2004, we distributed a 103-item, self-administered, anonymous survey simultaneously by mail and internet. Non-respondents received 3 e-mail reminders and 1 additional mailing.
We developed questions exploring effects of WHLs on the work life of attendings (see Appendix). These included questions about effects of WHLs on time spent on clinical work, research, and teaching. Because we felt that time was not the only measure of clinical involvement, we also asked about the effect of WHLs on attendings’ sense of responsibility for the supervision of patient care. Questions were phrased in a neutral fashion with response options allowing participants to indicate either an increase or decrease. Faculty who were in their first year of attending were excluded from the item asking for quantification of change in hours before and after WHLs. Finally, we developed a question to assess the overall probability of leaving academic medicine, similar to items used by other investigators.4,9–12
Survey questions were pilot-tested with subspecialty fellows and modified before administration.
Statistical Analysis
Effects of WHLs were examined for bivariate associations with demographic and professional characteristics. These were gender, age (dichotomized as less than 45 years vs 45 years and older), specialty (Surgery vs Internal Medicine), subspecialization within Surgery or Internal Medicine (vs being a “generalist”), being a clinician-educator (spending more than 50% of work time in inpatient or outpatient clinical work), being an intensivist (spending more than 50% of attending time in an ICU), working long hours (an average of more than 80 hours per week during 1 mo of in-patient attending), and being new faculty (first year attending). Since the time spent attending on in-patient clinical services varied widely among internists, this variable (categorized as 4 weeks or less, 8 weeks or less, or greater than 8 weeks) was also included in analysis.
We defined being at risk for leaving academic medicine as reporting a more than 40% probability of leaving within 3 y, based on the assumption that this would identify physicians whose long-term commitment was tenuous and whose retention might be easily affected by policy changes. We assessed bivariate associations between demographic and professional characteristics and being at risk for leaving academic medicine.
In addition, we assessed bivariate associations with four effects of WHLs which we hypothesized might affect faculty retention: increased clinical time; increased responsibility for supervising the care of patients; decreased time for research and other academic pursuits; and decreased time for teaching. We used t tests for continuous variables and chi-square or Fisher exact tests for dichotomous variables. We also conducted multivariate logistic regressions for these 4 effects and a fifth multivariate logistic regression evaluating factors associated with risk of leaving academic medicine that included these 4 effects as input variables where they demonstrated a bivariate association (p value ≤ .10) for risk of leaving. Gender and specialty was included in all models. In addition, all demographic and professional variables that showed an association (p value ≤ .10) with the dependent variable in bivariate analysis were included.
We considered a two-sided p value ≤ .05 statistically significant, and a two-sided p value ≤ .10 a trend toward statistical significance.
RESULTS
Respondent Characteristics
Surveys were sent to 295 Internal Medicine and 71 Surgery attendings for a total of 366 eligible participants; 282 returned surveys (response rate 77%). Response rate was higher for surgeons than for internists (87% vs 73%; p = .01). Among Internists, the generalists were more likely to respond than subspecialists (80% vs 64%; p = .005). Exactly one third of attendings chose to complete web-based rather than mailed surveys. Table 1 summarizes characteristics of respondents.
Table 1.
Characteristics of Respondents
| N* (% respondents) | |
|---|---|
| Demographic Characteristics | |
| Female | 77 (28) |
| Age | – |
| <45 y | 128 (47) |
| 45–54 y | 94 (34) |
| 55–64 y | 45 (16) |
| >65 y | 9 (3) |
| Professional Characteristics | |
| Surgeon (vs Internist) | 62 (22) |
| Generalist (vs subspecialist) | 92 (33) |
| Clinician-educator (>50% professional time clinical) | 106 (40) |
| Intensivist (>50% attending time in ICU) | 54 (20) |
| Long work hours (greater than 80 h per week during most recent month attending) | 53 (20) |
| New faculty (first year attending at UW teaching hospitals) | 34 (12) |
| Time spent attending on clinical service since implementation of WHLs (internists only, N = 209)† | |
| 1–4 wk | 69 (33) |
| 5–8 wk | 69 (33) |
| >8 wk | 71 (34) |
| Type of teaching hospital where usually attend | – |
| County | 87 (32) |
| University | 98 (36) |
| VA | 60 (22) |
| Multiple | 27 (10) |
*Total N is 282. Percentages refer to respondents to individual survey items, and in some cases reflect missing responses.
†Data for Internists only reported. All Surgeons reported greater than 8 weeks, and the large majority (93%) reported greater than 16 weeks.
Clinical Time
Figure 1 shows reported effects of work hour limitations on aspects of attendings’ professional life. Fifty-two percent of all respondents reported that their clinical work time had increased since July, 2003 at least partly because of WHLs, while 45% reported no change and 3% reported a decrease. Among Internists, the generalists were more likely than subspecialists to report an increase (68% vs 47%; p = .007), and this association retained a trend toward significance in multivariate analysis (OR, 1.7; 95% CI, 1.0–3.1). There was no association between reporting an increase in clinical work time because of the WHLs and any other demographic or professional characteristic. Figure 2 shows the distribution of the change in hours among the 52% of respondents reporting an increase (31% “partly” due to WHLs and 21% “mostly/entirely”). The median reported increase was 5–8 hours per week.
Figure 1.
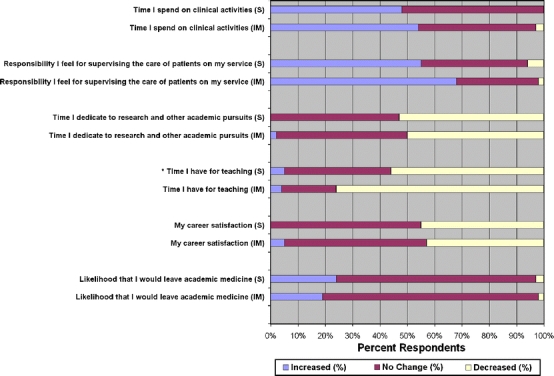
Reported effects of work hour limitations on professional life. The figure shows the proportion of respondents for Surgery (S) and Internal Medicine (IM) reporting effects of work hour limitations on aspects of professional life. The blue bars represent the proportion reporting an increase because of the work hour limitations, the red bars represent the proportion reporting no change, and the yellow bars represent the proportion reporting a decrease. * p ≤ 0.05 for surgery vs medicine.
Figure 2.
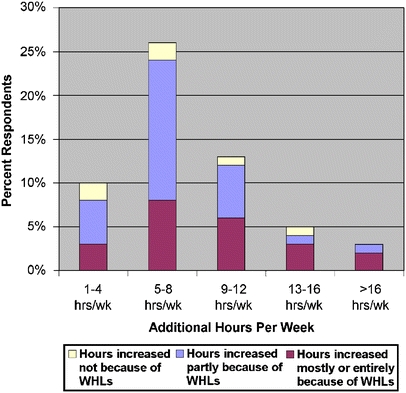
Additional clinical work hours reported by attending physicians. The figure shows the distribution of additional clinical hours reported by attending physicians. Red bars indicate the percent of total respondents reporting an increase “mostly or entirely because of WHLs, blue bars indicate those reporting an increase “partly” because of WHLs. The yellow bars indicate those reporting an increase not attributed to WHLs.
Responsibility Felt for Supervising Patient Care
The majority (65%) of attendings reported they felt increased responsibility for supervising residents’ care of patients because of WHLs, while 32% reported no change and 3% reported a decrease (Fig. 1). Women were more likely than men to report an increased sense of responsibility (83% vs 58%; p < .001). There was a trend for Internists to be more likely to feel increased responsibility than surgeons (68% vs 55%; p = .06); however, in a multivariate analysis, only being a woman retained an independent association (OR, 3.4; 95% CI, 1.7–6.7).
Research/Academic Time
Fifty-one percent of attendings reported that the WHLs had caused them to spend less time on research/academic pursuits, while 48% reported no change and 1% reported an increase. There was no significant difference in response by specialty. Women were more likely to report a decrease in research/academic time than men (63% vs 47%, p = .02; OR, 0.5; 95% CI, 0.3–0.9). There was a trend for clinician-educators to be more likely than their colleagues to report a decrease (55% vs 44%; p = .08); however, this association was reversed on multivariate analysis (OR, 0.5; 95% CI, 0.3–0.9).
Time Teaching Residents
The majority of attendings (72%) reported that the WHLs had caused them to spend decreased time teaching residents, while 24% reported no change and 4% reported an increase. Internists were more likely than surgeons to report a decrease (76% vs 56%, p = .002; OR, 2.4; 95% CI, 1.3–4.4). Table 2 shows responses to specific questions about teaching. Internists were more likely than surgeons to report a decrease in length of attending rounds because of WHLs (61% vs 23%; p < .001); an increase in the focus put on getting work done during attending rounds (68% vs 51%; p < .001); and a decrease in the time spent preparing for teaching (40% vs 23%; p = .01). Surgeons were more likely to report a decrease in willingness to give residents autonomy (59% vs 41%; p = .04).
Table 2.
Reported Effects of Work Hour Limitations on Teaching
| Aspect of Teaching | Increased (%) | No change (%) | Decreased (%) | p value for surgeons vs internists | |
|---|---|---|---|---|---|
| Length of attending rounds | Surgeons (N = 61) | 13 | 64 | 23 | <0.001 |
| Internists (N = 211) | 11 | 28 | 61 | ||
| Focus I put on getting work done, rather than teaching, during attending rounds | Surgeons (N = 61) | 51 | 49 | 0 | <0.001 |
| Internists (N = 211) | 68 | 21 | 11 | ||
| Time I spend preparing for teaching | Surgeons (N = 61) | 0 | 77 | 23 | 0.01 |
| Internists (N = 199) | 3 | 57 | 40 | ||
| My motivation to teach well | Surgeons (N = 62) | 3 | 68 | 29 | 0.89 |
| Internists (N = 200) | 5 | 65 | 30 | ||
| My willingness to give residents autonomy | Surgeons (N = 61) | 2 | 39 | 59 | 0.04 |
| Internists (N = 201) | 1 | 58 | 41 | ||
Total N is 282. Number (N) and percentages (%) refer to respondents to individual survey items, and in some cases reflect missing responses.
Career Satisfaction
Fifty-three percent of attendings reported no change in career satisfaction attributable to WHLs, while 44% reported a decrease and 3% reported an increase. There was no difference by specialty. Attendings who worked long hours were more likely to report a decrease in career satisfaction (57% vs 40%; p = 0.03). Older attendings were also more likely to report a decrease in career satisfaction (49% vs 37%; p = 0.04), while faculty in their first year of attending were less likely to report a decrease (27% vs 46%; p = 0.04).
Likelihood of Leaving Academic Medicine
Seventy-eight percent of attendings reported no change in likelihood of leaving academic medicine because of WHLs, while 20% of attendings reported an increased likelihood of leaving and 2% reported a decreased likelihood of leaving because of WHLs. Attendings working long hours were more likely than their colleagues to report an increased likelihood of leaving academic medicine because of WHLs (28% vs 18%; p = .10).
Long-term Commitment to Academic Medicine and Association with Effects of Work Hour Limitations
Sixty-seven percent of attendings reported that the probability they would leave academic medicine within the next 3 y was 20% or less, 17% reported a 21–40% probability of leaving, and 16% reported more than 40% probability of leaving (considered “at risk” for leaving). Attendings working long hours were more likely to be at risk for leaving than their counterparts (27% vs 14%; p = .02), and there was a trend for women to be more likely to be at risk for leaving than men (22% vs 13%; p = .06). Intensivists were less likely to be at risk for leaving (8% vs 15%; p = 0.05).
Table 3 shows associations between perceived effects of WHLs and being at risk for leaving. Attendings were significantly more likely to be at risk for leaving academic medicine if they perceived a decrease in time for research/academic pursuits (22% vs 9%; p = 0.004) or increased responsibility for supervising patient care (20% vs 7%; p = 0.005) because of WHLs. There was no statistically significant association between perceiving increased clinical time or decreased teaching time and being at risk for leaving academic medicine.
Table 3.
Attending Long-Term Commitment to Academic Medicine, by Reported Effects of Work Hour Limitations on Professional Life and Teaching
| Reported effects of work hour limitations* | Percent at risk for leaving academic medicine† | |
|---|---|---|
| Percent | P value | |
| Clinical time increased (N = 119) | 17 | 0.31 |
| Clinical time unchanged/decreased (N = 108) | 12 | |
| Responsibility for supervising care of patients increased (N = 177) | 20 | 0.005 |
| Responsibility for supervising care of patients unchanged/decreased (N = 96) | 7 | |
| Research/academic time decreased (N = 137) | 22 | 0.004 |
| Research/academic time unchanged/increased (N = 133) | 9 | |
| Time for teaching residents decreased (N = 195) | 16 | 0.74 |
| Time for teaching residents unchanged/increased (N = 77) | 14 | |
*For each reported effect of work hour limitations, N refers to the number of respondents who also completed the question about likelihood of leaving academic medicine
†Being “at risk” for leaving academic medicine defined as reporting a greater than 40% probability of leaving academic medicine within 3 years
Table 4 shows results from multivariate analysis to investigate predictors of being at risk for leaving academic medicine. Perceiving that the WHLs had caused an increase in responsibility for supervising the care of patients (OR, 3.3; 95% CI, 1.3–8.8) and a decrease in research/academic time (OR, 2.7; 95% CI, 1.2–6.2), both remained independent predictors for being at risk for leaving academic medicine. Other independent predictors were working long hours (OR, 3.3; 95% CI, 1.4–7.7) and being an intensivist (OR, 0.2; 95% CI, 0.1–0.8). Specialty and gender did not maintain their associations with being at risk for leaving academic medicine.
Table 4.
Attending Long-Term Commitment to Academic Medicine: *Multivariate Analysis
| At risk for leaving academic medicine OR (95% CI)† | |
|---|---|
| Responsibility for supervising care of patients increased because of work hour limitations | 3.3 (1.3–8.8) |
| Worked >80 hr/wk on most recent hospital service | 3.3 (1.4–7.7) |
| Research/academic time decreased because of work hour limitations | 2.7 (1.2–6.2) |
| Intensivist (>50% attending time in ICU) | 0.2 (0.1–0.8) |
| Surgeon | 2.1 (0.9–5.1) |
| Female | 1.5 (0.6–3.4) |
*All independent variables included in the logistic regression are shown. Variables included were those which showed bivariate association with being at risk for leaving academic medicine (p ≤ 0.10), in addition to specialty (surgery vs. internal medicine).
†Being “at risk” for leaving academic medicine defined as reporting a greater than 40% probability of leaving academic medicine within 3 years
DISCUSSION
We found that most Internal Medicine and Surgery attending physicians at one academic medical center perceive resident WHLs to have increased their clinical work hours and their sense of responsibility for supervising patient care, and to have decreased time for research and teaching. These observations suggest that WHLs have had considerable impact on faculty’s professional lives.
Median reported increases in clinical work hours because of WHLs were between 5–8 hours per week when supervising hospital based rotations. This is consistent with the limited existing literature, which has suggested modest effect of WHLs on faculty work hours.13–15 Total hours worked, however, does not fully reflect the impact of WHLs on clinical work life. While 52% of our respondents reported an increase in hours of clinical work, more (65%) reported an increased sense of responsibility for supervising patient care—possibly reflecting the common perception that attendings must close gaps in continuity of care generated by WHLs. Other authors have shown that, despite small changes in work hours, faculty perceive large differences in the content of their clinical work, with a shift toward activities traditionally performed by residents.13–15 This increased involvement in patient care may divert energy that previously was focused on academic work or teaching. It could be argued that a heightened sense of responsibility for supervising residents may lead to safer and higher quality care, correcting a previous inadequacy. Alternatively, it could be argued that the increased involvement by attendings only adequately—or even incompletely—compensates for changes in resident work. Regardless of the end result on patient care, the association between perception of increased supervisory responsibility and probability of leaving academic medicine suggests that attendings find their increased supervisory responsibility problematic.
In our study, the most common perceived effect of WHLs was on teaching, with almost 3 quarters of attendings reporting a decrease in time spent teaching residents. It is possible that attendings focused on formal teaching sessions in their responses and that the decrease might be partially offset by opportunities for informal teaching generated by attendings’ increased involvement in clinical work. Nevertheless, with time for teaching already threatened by service requirements in many institutions,16 the perception that WHLs have generated further erosion is troubling. Our findings suggest that Internists perceive a particularly large impact on their ability to teach. Internists were more than twice as likely as surgeons to report a decrease in the time they spent teaching residents. This may reflect the fact that much of surgical teaching occurs in the operating room or in conferences, which is relatively protected time.
Women also appear to perceive a special impact of WHLs. Women were more than twice as likely as men to report a decrease in time for research or other academic pursuits because of WHLs and more than three times as likely to report an increased sense of responsibility for supervising patient care. It is unclear why. Possibilities include a difference in departmental support for women’s academic activities, in the way men and women prioritize work activities, or in work flexibility induced by home responsibilities.
Importantly, a large proportion of attendings (44%) report that WHLs caused a decrease in career satisfaction, and one in five attendings report that because of WHLs, they are more likely to leave academic medicine. Consistent with this finding, perceiving decreased research/academic time was strongly associated with reporting a higher likelihood of leaving academic medicine, as was perceiving increased supervisory responsibility for clinical care. The association is not necessarily causal and may reflect the potential confounder that attendings with preexisting concerns about these issues might be more likely both to report effects of WHLs and to be dissatisfied with their current position. Nevertheless, these findings support the concern that WHLs may affect faculty retention in the academic medical system. Academic faculty often accept considerably lower remuneration than their colleagues in private practice specifically to engage in non-clinical professional activities. If time for such activities is reduced, it is perhaps not surprising that career satisfaction and commitment to academic medicine may decrease.
Several other published studies have addressed the effects of WHLs on the professional life of attending physicians.8,13–15,17–19 To our knowledge, only 3 have included non-surgical faculty.8,17,18 A large single-institution survey of all faculty (248 respondents)17 and a smaller national study of Internal Medicine faculty (111 respondents)8 both reported decreased time or satisfaction with teaching among more than half of respondents and increased clinical time and decreased job satisfaction in more than a third of respondents. A multi-institutional survey of family medicine faculty found that 20% were considering leaving academic medicine because of WHLS.18 Surveys of surgical faculty have suggested increased involvement in clinical work,13–15 despite little or no change in work hours.14,15,19 In the largest survey of surgical faculty, most reported decreased time for teaching (67%) and decreased work satisfaction (55%).13 Two studies suggested a decrease in time for research and academic productivity.13,15 These results are generally consistent with our findings, although in one study, surgeons were more likely than non-surgeons to report decreased time for teaching;17 this difference may reflect comparison with non-surgical specialties other than Internal Medicine, or institutional differences in specialties’ adaptation to WHLs.
Our study contributes to existing literature by providing more detail about perceived effects of WHLs, particularly on teaching. It is relatively large, includes both surgeons and Internists and has an excellent response rate for a physician survey.20 However, our study also has limitations. First, results from 3 hospitals that are affiliated with a single academic institution may not be generalizable. Institutions have undoubtedly varied in their responses to WHLs, for example, in compliance with WHLs, protection of operating room time for surgical residents, and number of physician extenders employed to help offset the impact of WHLs. Second, effects of WHLs on attendings’ work life were assessed by self-perception rather than objective outcomes such as measurement of actual work hours, academic productivity, or faculty retention rates. Future studies should evaluate such outcomes and, where possible, compare to similar metrics before initiation of WHLs. Third, because our study is cross-sectional, we are unable to determine the causal pathway between variables that are statistically associated. Fourth, our study describes initial reactions to WHLs during the first year of implementation. Subsequent adaptations by faculty and institutions and possible changes in resident compliance with WHLs may have affected attendings’ perceptions of the impact of WHLs on their professional lives.
Our study adds to a growing body of literature, which suggests that attending physicians perceive WHLs to have increased their clinical responsibility at the expense of those academic endeavors that have traditionally distinguished academic medicine from other practice environments. It might be argued that more clinical involvement by attending physicians is not an entirely unwelcome effect. However, implications for the quality of research, the training of physicians, and the recruitment, burnout, and retention of faculty must be considered carefully. It may be, for example, that criteria for promotion in academic medicine should change to reflect the shifting focus of attending physicians to patient care rather than research. Further study is justified as part of efforts to identify how both resident education and faculty satisfaction and productivity can be promoted simultaneously.
Acknowledgements
The authors thank the attending physicians at UW-affiliated hospitals and Drs. William J. Bremner, Joyce E. Wipf, Carlos A. Pellegrini, and Karen D. Horvath for their support. They thank Ms. Tetana E. Oguara and Ms. Siobhan C. Brown for their technical assistance. Dr. Goitein thanks Drs. Leonard D. Hudson and Diane P. Martin for their mentorship. Investigators received salary support from their institutions and grant support as described below, but these sources were not involved in design and conduct of the study; in collection, management, analysis, and interpretation of data; or in preparation, review, or approval of the manuscript. During this research, Dr. Goitein was a fellow in Pulmonary/Critical Care Medicine at the University of Washington in Seattle, and received a National Research Service Award training grant from the Agency for Healthcare Research and Quality. Dr. Shanafelt is Assistant Professor of Medicine and received institutional support from the Mayo Clinic in Rochester, MN. During this research, Dr. Nathens was Associate Professor of Surgery in the Division of Trauma and General Surgery at the University of Washington, and received institutional support from Harborview Medical Center. Dr. Curtis is Professor of Medicine in the Division of Pulmonary and Critical Care at the University of Washington and was funded by a K24 Award from the National Heart Lung and Blood Institute. None of the authors had financial conflicts of interest. Dr. Goitein had full access to all the data and takes responsibility for its integrity and the accuracy of the analysis. In addition to salary support from individual institutions, Dr. Goitein received support from a National Research Service Award training grant from the Agency for Healthcare Research and Quality, and Dr. Curtis received support from a K24 Award from the National Heart Lung and Blood Institute.
Conflict of Interest None disclosed.
Appendix
Selected Survey Questions
Table 5.
Survey Questions Concerning Perceived Effects of Work Hour Limitations on Professional Life, and a Separate Survey Question About Overall Likelihood of Leaving Academic Medicine
| Question | Possible responses |
|---|---|
| Questions regarding perceived effects of work hour limitations | |
| How does the amount of time you spent on clinical activities when on inpatient service this year compare to the time you spent before July 1, 2003? | a. No change |
| b. Increase | |
| c. Decrease | |
| Please estimate how many additional/fewer hours per week: | a. 1–4 hr/wk |
| b. 5–8 hr/wk | |
| c. 9–12 hr/wk | |
| d. 13–16 hr/wk | |
| e. >16 hr/wk | |
| Is this change in your hours because of the work hour limitations? | a. No |
| b. Yes, partly | |
| c. Yes, mostly | |
| d. Yes, entirely | |
| Please state the effect of the work hour limitations on the following factors of your life (5 separate questions): | a. Greatly decrease |
| 1. The responsibility I feel for supervising the care of patients on my service | b. Somewhat decrease |
| 2. The amount of time I dedicate to research and other academic pursuits | c. No change |
| 3. The amount of time I spend teaching residents | d. Somewhat increase |
| 4. My career satisfaction | e. Somewhat decrease |
| 5. The likelihood that I would leave academic medicine | |
| Please state the effect of the work hour limitations on the following components of education on inpatient services (5 separate questions): | a. Greatly decrease |
| 1. The length of attending rounds | b. Somewhat decrease |
| 2. The focus I put on getting work done, rather than teaching, during attending rounds | c. No change |
| 3. The time I spend preparing for teaching | d. Somewhat increase |
| 4. My motivation to teach well | e. Somewhat decrease |
| 5. My willingness to give residents autonomy | |
| Question regarding likelihood of leaving academic medicine | |
| What is the probability that you will leave academic medicine within the next three years? | a. 0–20% |
| b. 21–40% | |
| c. 41–60% | |
| d. 61–80% | |
| e. 81–100% | |
References
- 1.Report of the ACGME Work Group on Resident Duty Hours. Chicago: Accreditation Council for Graduate Medical Education; 2002 June 11.
- 2.Fletcher KE, Underwood W 3rd, Davis SQ, Mangrulkar RS, McMahon LF Jr, Saint S. Effects of work hour reduction on residents’ lives: a systematic review. JAMA. 2005;294(9):1088–100. [DOI] [PubMed]
- 3.Weinstein DF. Duty hours for resident physicians–tough choices for teaching hospitals. N Engl J Med. 2002;347(16):1275–8. [DOI] [PubMed]
- 4.Lowenstein SR, Fernandez G, Crane LA. Medical school faculty discontent: prevalence and predictors of intent to leave academic careers. BMC Med Educ. 2007;7(1):37. [DOI] [PMC free article] [PubMed]
- 5.Schindler BA, Novack DH, Cohen DG, et al. The impact of the changing health care environment on the health and well-being of faculty at four medical schools. Acad Med. 2006;81(1):27–34. [DOI] [PubMed]
- 6.Landon BE, Reschovsky JD, Pham HH, Blumenthal D. Leaving medicine: the consequences of physician dissatisfaction. Med Care. 2006;44(3):234–42. [DOI] [PubMed]
- 7.Demmy TL, Kivlahan C, Stone TT, Teague L, Sapienza P. Physicians’ perceptions of institutional and leadership factors influencing their job satisfaction at one academic medical center. Acad Med. 2002;77(12 Pt 1):1235–40. [DOI] [PubMed]
- 8.Reed DA, Levine RB, Miller RG, et al. Effect of residency duty-hour limits: views of key clinical faculty. Arch Intern Med. 2007;167(14):1487–92. [DOI] [PubMed]
- 9.Coyle YM, Aday LA, Battles JB, Hynan LS. Measuring and predicting academic generalists’ work satisfaction: implications for retaining faculty. Acad Med. 1999;74(9):1021–7. [DOI] [PubMed]
- 10.Bergus GR, Randall CS, Winniford MD, Mueller CW, Johnson SR. Job satisfaction and workplace characteristics of primary and specialty care physicians at a bimodal medical school. Acad Med. 2001;76(11):1148–52. [DOI] [PubMed]
- 11.Buckley LM, Sanders K, Shih M, Hampton CL. Attitudes of clinical faculty about career progress, career success and recognition, and commitment to academic medicine. Results of a survey. Arch Intern Med. 2000;160(17):2625–9. [DOI] [PubMed]
- 12.Pathman DE, Konrad TR, Williams ES, Scheckler WE, Linzer M, Douglas J. Physician job satisfaction, dissatisfaction, and turnover. J Fam Pract. 2002;51(7):593. [PubMed]
- 13.Coverdill JE, Finlay W, Adrales GL, et al. Duty-hour restrictions and the work of surgical faculty: results of a multi-institutional study. Acad Med. 2006;81(1):50–6. [DOI] [PubMed]
- 14.Winslow ER, Berger L, Klingensmith ME. Has the 80-hour work week increased faculty hours? Curr Surg. 2004;61(6):602–8. [DOI] [PubMed]
- 15.Klingensmith ME, Winslow ER, Hamilton BH, Hall BL. Impact of resident duty-hour reform on faculty clinical productivity. Curr Surg. 2006;63(1):74–9. [DOI] [PubMed]
- 16.Ludmerer K. Time to Heal: American Medical Education from the Turn of the Century to the Era of Managed Care. New York: Oxford University Press; 1999.
- 17.Vanderveen K, Chen M, Scherer L. Effects of resident duty-hours restrictions on surgical and nonsurgical teaching faculty. Arch Surg. 2007;142(8):759–64. (discussion 764–6). [DOI] [PubMed]
- 18.Choby B, Passmore C. Faculty perceptions of the ACGME resident duty hour regulations in family medicine. Fam Med. 2007;39(6):392–8. [PubMed]
- 19.Malangoni MA, Como JJ, Mancuso C, Yowler CJ. Life after 80 hours: the impact of resident work hours mandates on trauma and emergency experience and work effort for senior residents and faculty. J Trauma. 2005;58(4):758–61. (discussion 761–2). [DOI] [PubMed]
- 20.Kellerman SE, Herold J. Physician response to surveys. A review of the literature. Am J Prev Med. 2001;20(1)61–7. [DOI] [PubMed]


