Abstract
Background
Physician treatment of cardiovascular risk factors may be affected by specific types of patient comorbidities.
Objectives
To examine the relationship between discordant comorbidities and LDL-cholesterol management in hypertensive patients not previously treated with lipid-lowering therapy; to determine whether the presence of cardiovascular (concordant) conditions mediates this relationship.
Design
We performed a retrospective cohort study of 1,935 hypertensive primary care patients (men >45 years of age, women >55 years of age) with documented elevated low-density lipoprotein (LDL) cholesterol and no lipid-lowering therapy at baseline. The outcome was guideline-consistent hyperlipidemia management defined as optimal value on repeat LDL cholesterol testing or initiation of lipid-lowering therapy. Using generalized estimating equations (GEE), we examined the association of concordant and discordant comorbidities with guideline-consistent hyperlipidemia management over a 2-year follow-up period, adjusting for patient characteristics.
Results
Guideline-consistent hyperlipidemia management was achieved in 1,236 patients (64%). In the fully adjusted model, each additional discordant condition resulted in a 19% lower adjusted odds ratio of guideline-consistent hyperlipidemia management (p < 0.001) when compared with no discordant conditions. The dampening effect of discordant conditions on guideline-consistent management persisted even in the presence of concordant conditions, but each additional concordant condition was associated with a 37% increase in the adjusted odds of guideline-consistent hyperlipidemia management (p < 0.001).
Conclusions
In this cohort of hypertensive primary care patients, the number of conditions discordant with cardiovascular risk was strongly negatively associated with guideline-consistent hyperlipidemia management even in patients at the highest risk for cardiovascular events and cardiac death.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0647-4) contains supplementary material, which is available to authorized users.
KEY WORDS: hyperlipidemia, quality of care, comorbidity
INTRODUCTION
Recent studies have reported that up to 45% of recommended health care is not received.1,2 These findings have highlighted the need for improved physician adherence to clinical practice guidelines and better methods to measure guideline adherence.3 However, both clinicians and researchers have expressed concern that widespread application of clinical practice guidelines may have unintended negative consequences for complex patients.4–9 The role of one aspect of complexity, the presence of comorbid conditions, has been a point of particular contention, with several recent studies indicating that patients with many comorbid conditions actually receive better quality care, while other studies conclude that these patients receive poorer care.10–16 A possible explanation for these conflicting findings is that comorbidity affects quality of care differently depending on the target condition and the nature of the comorbid condition(s).17,18 For example, a physician caring for a patient with diabetes may focus the clinical encounter on cardiovascular risk reduction. In contrast, the presence of osteoarthritis may direct the physician towards management of a patient’s functional status and need for pain management.
To further evaluate this concept, we looked at the impact of different types of comorbidities on management of hyperlipidemia. We were interested in assessing whether the presence of discordant comorbidities (i.e., conditions with treatment goals different than cardiovascular treatment goals 17) was associated with lower levels of guideline-consistent management of hyperlipidemia. To better understand the relationship between type of comorbidity and quality, we also investigated the role of comorbid conditions that increase cardiovascular risk (i.e., concordant conditions that would focus the physician on initiation of lipid-lowering therapy). We hypothesized that an increasing burden of discordant conditions would be associated with a decline in quality of care, defined as failure to initiate lipid-lowering therapy or attainment of guideline-based low density lipoprotein (LDL) cholesterol targets. Additionally, we hypothesized that this effect would persist even in the presence of conditions that increase cardiovascular risk.
METHODS
Study Sample
We identified adults (≥18 years old) with three or more visits (between 1 January 2003 and 8 February 2005) to physicians in six primary care practices (one family medicine and six general internal medicine) affiliated with an academic medical center in Philadelphia, PA. We selected men ≥ age 45 and women ≥ age 55 (age thresholds consistent with The Third Report of the National Cholesterol Education Program Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (NCEP-ATPIII)’s definition of a “major risk factor” for cardiovascular disease.19 Hypertension was defined as the presence of one or more of the following criteria: (1) two or more visits with an elevated blood pressure as defined by The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure (JNC-VI)20; (2) two or more visits with an outpatient diagnosis of hypertension; (3) one outpatient visit with a diagnosis of hypertension and one visit with an elevated blood pressure; or (4) at least one antihypertensive prescription with a diagnosis of hypertension.
From this cohort, we identified patients with suboptimal LDL cholesterol as defined by NCEP-ATPIII guidelines19: (1) LDL cholesterol ≥100 mg/dl in patients with diabetes, coronary artery disease or coronary heart disease equivalent conditions (stroke, other cerebral vascular disease, peripheral vascular disease) or (2) ≥130 mg/dl for all other patients (since all patients in the study had at least two risk factors for cardiovascular disease and thus an LDL cholesterol goal of <130 mg/dl.19 We excluded persons with current or previous prescriptions for lipid-lowering therapy during or after the year 2002. Previous lipid-lowering therapy was defined as a prescription for a lipid reduction medication anytime from the calendar year 2002 until the index visit. Patients with liver dysfunction were also excluded from analysis as liver disease may be a contraindication to use of lipid-lowering therapy.
Data Collection
Patient data collection began in 2002, when study practices installed the EPIC electronic medical record in all six study practices. EPIC provides information on patient demographics, insurance status, past medical history, physiologic measures, clinical diagnoses, laboratory test and imaging results, and prescribed medications. The index visit was defined as the enrollee’s first visit during the study period (1 January 2003-8 February 2005). Patients were followed for a minimum of 6 months and a maximum of 2 years after the index visit. Once lipid-lowering therapy was initiated or target LDL cholesterol was achieved, the patient was censored. If neither of these outcomes was achieved, we examined all visits until the end of the study period.
Outcome
The outcome measure of guideline-consistent hyperlipidemia management was defined as either: (1) initiation of lipid-lowering therapy at any time during the follow-up period or (2) achievement of acceptable LDL cholesterol (as defined by NCEP guidelines19 on repeat measurement.
Measures of Concordant and Discordant Comorbidities
Study patients’ clinical conditions were defined using ICD-9-CM coded conditions at all electronic medical record documented encounters prior to and including the index visit. We used ICD-9-CM codes because they allow for the most uniform identification of comorbidities, even those comorbidities not associated with the use of specific medications or recorded objective findings. Concordant conditions (excluding hypertension and hyperlipidemia) consisted of: diabetes, coronary artery disease, coronary artery disease equivalent (i.e., stroke, other cerebral vascular disease, peripheral vascular disease) or renal insufficiency (serum creatinine >2 mg/dl). For each patient, we created a variable for the sum of concordant comorbidities, ranging from zero to four. Heart failure and valvular heart disease were considered as covariates because they have several alternative pathophysiologic mechanisms that might not focus physician attention on hyperlipidemia management.
Discordant comorbidity burden was calculated from an adapted version of Elixhauser’s comorbidity measure21, an index that uses ICD-9-CM-codes to identify 29 specified conditions associated with inpatient resource use and mortality. We selected discordant conditions from the Elixhauser set, added common diseases and symptoms seen in more than 5% of ambulatory encounters in the study population (e.g., osteoarthritis, nausea/vomiting/dizziness, diarrhea/constipation, esophageal reflux/ulcer disease, headache) and deleted concordant comorbidities. For each patient, we created a variable that summed the discordant comorbidities, resulting in a single score (ranging from zero to eight or more). Appendix A, which can be found online, lists all included conditions.
Covariates
Patient demographic and socioeconomic variables included sex, race, age and insurance type. Median neighborhood income was determined by linking patient zip code to 2000 US census tract data (we did not have individual income data). Missing race was assigned using a single imputation method based upon patient zip code. The number of patient primary care visits during the study period was included as a covariate because patients with more visits had more opportunities for lipid management.
The number of antihypertensive medications in the patient’s regimen was used to estimate medication burden as patients with an increasing number of medications may be less likely to begin lipid-lowering therapy. To ensure an accurate count of the number of medications for each patient, we assessed each previous, original antihypertensive prescription for the number of pills prescribed, the number of daily doses and the number of refills given.
Statistical Analysis
The patient was the unit of analysis. Descriptive statistics were generated at the index visit. Bivariate and multivariate relationships between dependent and independent variables were examined using generalized estimating equations (GEE) accounting for clustering of patients within providers. Concordant and discordant condition counts were included in all models. In a separate model, we examined the relationship between concordant and discordant conditions using an interaction term. To better examine this relationship, we separately stratified analyses by the presence of a concordant condition. We assumed an exchangeable correlation matrix for all GEE models and included both key predictors (comorbidity variables) and potential confounders for adjustment. All statistical analyses were performed using Stata statistical software (version 9, College Station, TX).
Institutional Review Board Approval
The study received expedited review by the University of Pennsylvania’s institutional review board. Because of the retrospective nature of the study, the board granted a waiver of HIPAA authorization.
RESULTS
Of 15,708 patients diagnosed with hypertension who had three or more visits to a study site, 11,309 met our study age criteria. Of these patients, 4,141 had suboptimal LDL cholesterol values prior to the index visit (i.e., the first visit following a finding of suboptimal LDL cholesterol). We further restricted our analyses to the 2,060 patients (50% of those with high LDL cholesterol) with at least 6 months of follow-up and without a history of lipid-lowering therapy from calendar year 2002 until the index visit. After exclusion of 125 patients with liver dysfunction, 1,935 patients remained in the cohort. Race was imputed for 183 of these patients.
The majority of study patients were African-American with an annual income of less than $35,000 (Table 1). Forty-one percent of patients had no concordant comorbidities other than hyperlipidemia and hypertension, while 19% had two or more additional concordant comorbidities. Discordant comorbidities were common–94% of patients had at least one discordant condition, while 27% of the sample had more than four discordant conditions. The mean number of patient visits during the study period was 9.38. Ninety-eight percent of patients had 20 or fewer visits. Over the period of observation, guideline-consistent hyperlipidemia management was achieved in 1236 patients (64%). Of these, 26% were managed at the index visit, and 57% were managed in four visits or fewer.
Table 1.
Patient and Provider Characteristics
| Number of patients (%) N = 1,935 | |
|---|---|
| Demographic | |
| Sex | |
| Female | 1,266 (65.4) |
| Race | |
| Black | 1,105 (61.5) |
| Age | |
| <60 years | 478 (24.7) |
| 60–69 years | 618 (31.9) |
| 70–79 years | 540 (27.9) |
| >80 years | 299 (15.5) |
| Insurance | |
| Commercial insurance | 1,091 (56.4) |
| Medicare | 651 (33.6) |
| Medicaid | 177 (9.2) |
| Self pay or unknown | 16 (0.8) |
| Income | |
| <$25,000/year | 423 (21.9) |
| $25–35,000/year | 625 (32.3) |
| $35–70,000/year | 734 (37.9) |
| >70,000/year | 153 (7.9) |
| Clinical | |
| Number of concordant comorbidities | |
| 0 | 786 (40.6) |
| 1 | 774 (40.0) |
| 2 | 287 (14.8) |
| 3 or more | 88 (4.6) |
| Number of discordant comorbidities | |
| 0 | 113 (5.8) |
| 1 | 264 (13.6) |
| 2 | 326 (16.8) |
| 3 | 399 (20.6) |
| 4 | 311 (16.1) |
| 5 | 218 (11.3) |
| 6 | 139 (7.2) |
| 7 | 88 (4.6) |
| ≥8 | 77 (4.0) |
| Number of previous anti-hypertensive medications | |
| 0 | 463 (23.9) |
| 1 | 628 (32.5) |
| 2 | 530 (27.4) |
| 3 or more | 314 (16.2) |
| Patient visits | |
| Mean number of patient visits | 9.38 (range: 5–32) |
In the fully adjusted GEE regression model, each additional discordant condition resulted in 19% lower adjusted odds of guideline-consistent hyperlipidemia management (p < 0.001) when compared with none (Table 2). Patients with seven or more discordant conditions had 88% lower adjusted odds of guideline-consistent hyperlipidemia management compared with patients with no discordant conditions (Fig. 1). Compared to patients with no concordant conditions and with adjustment for the presence of discordant conditions, each additional concordant condition was associated with a 37% increase in the adjusted odds of guideline-consistent hyperlipidemia management of LDL cholesterol (p < 0.001). The presence of three or more concordant conditions was associated with greater than three-fold adjusted odds of guideline-consistent hyperlipidemia management of LDL cholesterol management when compared with patients without any concordant conditions (p < 0.001) (Fig. 2). We found no interaction between number of concordant and discordant comorbidities. Stratified analysis showed a consistent relationship between guideline-consistent hyperlipidemia management and the number of discordant comorbidities in the presence or absence of a concordant condition (Table 2). The full model is shown in Appendix B, which can be found online.
Table 2.
Adjusted Associations between Patient Comorbidities and LDL Management*
| Number of discordant conditions | Number of concordant conditions | |
|---|---|---|
| Adjusted odds [95% CI] | Adjusted odds [95% CI] | |
| Combined model: | ||
| All patients (n = 1,935) | 0.81 [0.77–0.85] | 1.37 [1.21–1.56] |
| Stratified models: | ||
| No concordant conditions (n = 828) | 0.82 [0.75–0.89] | — |
| One or more concordant conditions (n = 1,149) | 0.81 [0.75–0.86] | — |
*Adjusted for race, sex, age, income (based on census tract), insurance type, number of visits, number of antihypertensive medications, presence of heart failure, presence of valvular heart disease
Figure 1.
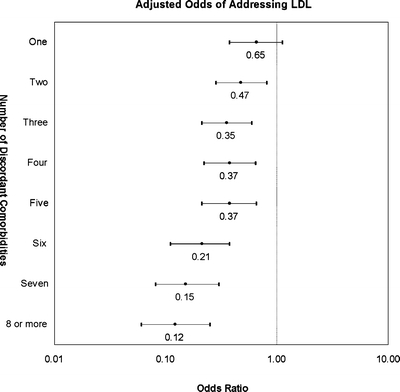
Appropriate management of elevated LDL cholesterol over 2-year follow-up. Number of discordant comorbidities vs. adjusted odds of management. Reference group is no discordant comorbidities. Model adjusted for race, sex, age, income (based on census tract), insurance type, number of visits, number of antihypertensive medications, presence of heart failure, presence of valvular disease, and number of concordant conditions.
Figure 2.
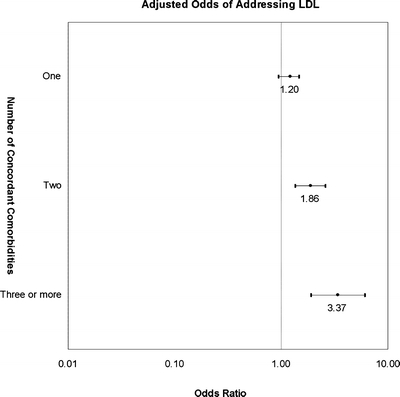
Appropriate management of elevated LDL cholesterol over 2-year follow-up. Number of concordant comorbidities vs. adjusted odds of management. Reference group is no concordant comorbidities. Model adjusted for race, sex, age, income (based on census tract), insurance type, number of visits, number of antihypertensive medications, presence of heart failure, presence of valvular disease, and number of discordant conditions.
DISCUSSION
We found a distinct association between discordant comorbidities and a composite endpoint of initiating lipid-lowering therapy or achieving a desirable LDL cholesterol level in this cohort of primary care patients with hypertension and elevated LDL cholesterol. Increasing numbers of discordant conditions decreased the adjusted odds of guideline-consistent hyperlipidemia management, a finding that persisted despite the presence of conditions that increase the risk of cardiovascular events or death. An increasing number of concordant conditions was associated with increased likelihood of guideline-consistent hyperlipidemia management regardless of the number of discordant conditions. These results are consistent with the hypothesis that the type of comorbidity may have different effects on guideline-consistent hyperlipidemia management and that competing demands may negatively affect the quality of cardiovascular risk management even in the patients for whom it is most indicated.
The theory that different types of comorbidities have varying impacts on cardiovascular risk reduction has been previously suggested, 17,18 but few studies have addressed the separate roles of concordant and discordant conditions.22 Most research on the impact of comorbidity on cardiovascular risk reduction has combined concordant and discordant comorbidities. Several studies concluded that comorbidity may improve quality of care; others found that comorbidity detracts from quality.10-16 A recent example, a study by Higashi et al.,10 found that the presence of multiple medical conditions was associated with improved quality of care across many diseases and many quality indicators. The comorbidity measure used, however, was a simple count of conditions that did not distinguish between concordant and discordant comorbidity. This study also combined many quality measures that may exhibit various relationships with comorbid conditions. By separating discordant and concordant conditions and examining a single target condition, we were able to uncover distinctive effects that may have been obscured or confounded in Higashi’s study.
Our findings are supported by several studies that have separately investigated concordant and discordant patient comorbidities. Some have reported the positive impact of separate concordant comorbidities on the management of cardiovascular risk factors,23,24 whereas others have found negative impacts of individual discordant comorbidities on management of these risk factors.25–27 We believe this is the first study to examine the concurrent, separate, and linear contributions of concordant and discordant comorbidities on management of a single cardiovascular risk factor.
An increased likelihood of guideline-consistent hyperlipidemia management for patients with more concordant conditions is expected because coronary artery disease or its risk equivalent is a strong motivator for lipid management. The finding that an increasing number of discordant conditions (which may reflect competing demands) was associated with failure to manage high LDL cholesterol is more alarming. To confirm the consistency of this relationship, we tested for an interaction between concordant and discordant conditions. When no significant interaction was observed, we stratified our analyses to separately examine patients with and without concordant conditions and found very similar results for both groups. Our robust findings seem to indicate that discordant conditions may indeed be a significant barrier to high quality care.
However, our comorbidity measure did not allow us to determine the severity of a given discordant condition or identify clinically dominant conditions. Therefore, we were not able to distinguish between patients receiving poor quality care and those for whom initiation of therapy was not indicated. Conditions that are clinically dominant eclipse the management of all other conditions because they occupy a preponderance of the physician or patient’s time or affect a patient’s life expectancy.17 Because the inability to determine severity of a given condition is a weakness of ICD-9-CM-based comorbidity measures, 28–36 future research should focus on methods to determine whether specific, severe comorbidities are driving the observed relationship between the number of discordant conditions and guideline-consistent care for LDL cholesterol management.
The outcome used in this study (i.e., guideline-consistent care) was not a performance measure because we did not designate a time frame for initiation of therapy or achievement of the LDL cholesterol goal. However, our study may inform future construction of performance measures for hyperlipidemia management. It has been argued that a possible unintended consequence of population-based quality measures is that they may penalize physicians who care for complex patients.4–9 Our findings strengthen the argument that quality measures should account for patient preferences, type of comorbidity and clinical complexity.
This study has some limitations. We examined 1,935 patients from an urban population receiving care in six primary care clinics affiliated with a single academic medical center. It is also notable that we selected a population known to be receiving poor quality care at baseline (i.e., they were known to have high LDL cholesterol, but were not taking medications). Therefore, the generalizability of observed results is limited. While all prescriptions written by primary care providers should have been documented in EPIC, we were not able to identify prescriptions written by specialists who do not use EPIC. We also were not able to identify patients managed with lifestyle interventions. To account for this discrepancy, however, we included achievement of guideline-consistent LDL cholesterol as an outcome. We used follow-up of 6 months to 2 years as our analytical time frame because it allowed clinicians adequate opportunity to institute management even in complex patients, and analyses were adjusted for number of visits per patient during the time frame. However, patients with longer follow-up periods may have presented differential opportunities to receive treatment or achieve LDL cholesterol goals. We also were not able assess cases in which patients were lost to follow-up. Some patients for whom we have incomplete data may have transitioned to an outside primary care practice before the end of the study period or may have died. As we stated above, our inability to determine severity of disease is a point that warrants further study. Another limitation was our inability to determine those patients for whom lipid-lowering therapy was absolutely contraindicated. To attempt to account for some contraindications to therapy, we excluded patients with liver disease from the analysis. Additionally, previous work has shown that few patients have documented contraindications to lipid-lowering therapy.37 We faced the challenge that NCEP ATP III guidelines19 are not clear on the best approach for management of lipids in patients older than 85 years. Because quality measurement does not consider this exception (failure to manage high LDL cholesterol in this group is still considered to be “poor quality care”), we applied guideline criteria uniformly regardless of age. Notably, less than 4% of our cohort was over the age of 85. Another limitation is that we examined the association between comorbid conditions and initiation of medication for a single target condition. The observed relationships may differ for other conditions or other types of interventions. Finally, our measure of comorbidity was not a complete measure of patient complexity because we were not able to account for other factors such as poor adherence, patient preferences, or social barriers to care.
Among our cohort of primary care patients with hypertension and elevated LDL cholesterol, the nature of the comorbid conditions was associated with the likelihood of LDL cholesterol management. Patients with an increasing number of discordant conditions were less likely to receive guideline-consistent care even in the presence of cardiovascular disease or risk equivalent. Although some patients with a strong preference to reduce medication burden or with reduced life expectancy may make a decision not to start lipid-lowering therapy, most patients, particularly those with cardiovascular disease, should be receiving guideline-consistent care for hyperlipidemia. Programs that help set priorities for the medical encounter should be considered to help focus physicians and patients on the important task of cardiovascular risk reduction.
Electronic supplementary material
Below is the link to the electronic supplementary material.
(DOC 36.5 kb)
Acknowledgements
Funding Supported by Pfizer Inc. and the Robert Wood Johnson Foundation Clinical Scholars Program
Conflicts of Interest Funding for this project was provided by an unrestricted grant from Pfizer Inc. The University of Pennsylvania provided the mechanism for administration of this grant. Investigators at the University of Pennsylvania and Pennsylvania State University performed the analyses. By contract, the investigators retain the right to publish results and manuscripts without approval from Pfizer Inc. Dr. Lagu is funded by The Robert Wood Johnson Foundation Clinical Scholars Program.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-008-0647-4) contains supplementary material, which is available to authorized users.
Contributor Information
Tara Lagu, Phone: 215-756-2733, FAX: 215-573-2742, Email: lagutc@gmail.com.
Mark G. Weiner, Email: mweiner@mail.med.upenn.edu.
Christopher S. Hollenbeak, Email: chollenb@hes.hmc.psu.edu.
Susan Eachus, Email: susan.eachus@gmail.com.
Craig S. Roberts, Email: craig.roberts@pfizer.com.
J. Sanford Schwartz, Email: schwartz@wharton.upenn.edu.
Barbara J. Turner, Email: bturner@mail.med.upenn.edu.
References
- 1.McGlynn EA, Asch SM, Adams J, et al.. The quality of health care delivered to adults in the United States.[see comment]. N Engl J Med. 2003;348(26):2635–45. [DOI] [PubMed]
- 2.Higashi TMD, Shekelle PGMDP, Solomon DHMD, et al. The Quality of Pharmacologic Care for Vulnerable Older Patients. [Miscellaneous]. In: Annals of Internal Medicine May 4 2004;140(9):714–720. [DOI] [PubMed]
- 3.Rosenthal MB, Frank RG. What is the empirical basis for paying for quality in health care? Med Care Res Rev. 2006;63(2):135–57. [DOI] [PubMed]
- 4.Werner RM, Asch DA. Clinical concerns about clinical performance measurement. Annals of Family Medicine. 2007;5(2):159–63. [DOI] [PMC free article] [PubMed]
- 5.Hayward RA. Performance measurement in search of a path.[comment]. N Engl J Med. 2007;356(9):951–3. [DOI] [PubMed]
- 6.McMahon LF Jr., Hofer TP, Hayward RA. Physician-level P4P–DOA? Can quality-based payment be resuscitated? American Journal of Managed Care. 2007;13(5):233–6. [PubMed]
- 7.Boyd CM, Darer J, Boult C, Fried LP, Boult L, Wu AW. Clinical practice guidelines and quality of care for older patients with multiple comorbid diseases: implications for pay for performance.[see comment]. JAMA. 2005;294(6):716–24. [DOI] [PubMed]
- 8.Durso SC. Using clinical guidelines designed for older adults with diabetes mellitus and complex health status.[see comment]. JAMA. 2006;295(16):1935–40. [DOI] [PubMed]
- 9.Tinetti ME, Bogardus ST Jr., Agostini JV. Potential pitfalls of disease-specific guidelines for patients with multiple conditions. N Engl J Med. 2004;351(27):2870–4. [DOI] [PubMed]
- 10.Higashi T, Wenger NS, Adams JL, et al.. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356(24):2496–504. [DOI] [PubMed]
- 11.Glynn RJ, Monane M, Gurwitz JH, Choodnovskiy I, Avorn J. Aging, comorbidity, and reduced rates of drug treatment for diabetes mellitus. J Clin Epidemiol. 1999;52(8):781–90. [DOI] [PubMed]
- 12.Chaudhry SI, Berlowitz DR, Concato J. Do age and comorbidity affect intensity of pharmacological therapy for poorly controlled diabetes mellitus?[see comment]. J Am Geriatr Soc. 2005;53(7):1214–6. [DOI] [PubMed]
- 13.McLaughlin TJ, Soumerai SB, Willison DJ, et al.. The effect of comorbidity on use of thrombolysis or aspirin in patients with acute myocardial infarction eligible for treatment.[see comment]. J Gen Intern Med. 1997;12(1):1–6. [DOI] [PMC free article] [PubMed]
- 14.Min LC, Wenger NS, Fung C, et al.. Multimorbidity is associated with better quality of care among vulnerable elders.[see comment]. Med Care. 2007;45(6):480–8. [DOI] [PubMed]
- 15.Desai MM, Rosenheck RA, Druss BG, Perlin JB. Mental disorders and quality of diabetes care in the veterans health administration. Am J Psychiatr. 2002;159(9):1584–90. [DOI] [PubMed]
- 16.Heflin MT, Oddone EZ, Pieper CF, Burchett BM, Cohen HJ. The effect of comorbid illness on receipt of cancer screening by older people.[see comment]. J Am Geriatr Soc. 2002;50(10):1651–8. [DOI] [PubMed]
- 17.Piette JD, Kerr EA. The impact of comorbid chronic conditions on diabetes care. Diabetes Care. 2006;29(3):725–31. [DOI] [PubMed]
- 18.Piette JD, Richardson C, Valenstein M. Addressing the needs of patients with multiple chronic illnesses: the case of diabetes and depression. American Journal of Managed Care. 2004;10(2 Pt 2):152–62. [PubMed]
- 19.Expert Panel on Detection EaToHBCiA. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III).[see comment]. JAMA. 2001;285(19):2486–97. [DOI] [PubMed]
- 20.Anonymous. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure.[see comment][erratum appears in Arch Intern Med 1998 Mar 23;158(6):573]. Arch Intern Med. 1997;157(21):2413–46. [DOI] [PubMed]
- 21.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data.[see comment]. Med Care. 1998;36(1):8–27. [DOI] [PubMed]
- 22.Kerr EA, Heisler M, Krein SL, et al.. Beyond comorbidity counts: how do comorbidity type and severity influence diabetes patients’ treatment priorities and self-management?[see comment]. J Gen Intern Med. 2007;22(12):1635–40. [DOI] [PMC free article] [PubMed]
- 23.Asch SM, McGlynn EA, Hiatt L, et al.. Quality of care for hypertension in the United States. BMC Cardiovascular Disorders. 2005;5(1):1. [DOI] [PMC free article] [PubMed]
- 24.Rodondi N, Peng T, Karter AJ, et al.. Therapy modifications in response to poorly controlled hypertension, dyslipidemia, and diabetes mellitus.[see comment]. Ann Intern Med. 2006;144(7):475–84. [DOI] [PMC free article] [PubMed]
- 25.Ciechanowski PS, Katon WJ, Russo JE, Hirsch IB. The relationship of depressive symptoms to symptom reporting, self-care and glucose control in diabetes. Gen Hosp Psych. 2003;25(4):246–52. [DOI] [PubMed]
- 26.Redelmeier DA, Tan SH, Booth GL. The treatment of unrelated disorders in patients with chronic medical diseases.[see comment]. N Engl J Med. 1998;338(21):1516–20. [DOI] [PubMed]
- 27.Krein SL, Heisler M, Piette JD, Makki F, Kerr EA. The effect of chronic pain on diabetes patients’ self-management.[see comment]. Diabetes Care. 2005;28(1):65–70. [DOI] [PubMed]
- 28.Fisher ES, Whaley FS, Krushat WM, et al.. The accuracy of Medicare’s hospital claims data: progress has been made, but problems remain. Am J Public Health. 1992;82(2):243–8. [DOI] [PMC free article] [PubMed]
- 29.Iezzoni LI. Using administrative diagnostic data to assess the quality of hospital care. Pitfalls and potential of ICD-9-CM. Int J Technol Assess Health Care. 1990;6(2):272–81. [DOI] [PubMed]
- 30.Jollis JG, Ancukiewicz M, DeLong ER, Pryor DB, Muhlbaier LH, Mark DB. Discordance of databases designed for claims payment versus clinical information systems. Implications for outcomes research.[see comment]. Ann Intern Med. 1993;119(8):844–50. [DOI] [PubMed]
- 31.Romano PS, Mark DH. Bias in the coding of hospital discharge data and its implications for quality assessment. Med Care. 1994;32(1):81–90. [DOI] [PubMed]
- 32.Farley JF, Harley CR, Devine JW. A comparison of comorbidity measurements to predict healthcare expenditures. Am J Managed Care. 2006;12(2):110–9. [PubMed]
- 33.Fishman PA, Goodman MJ, Hornbrook MC, Meenan RT, Bachman DJ, O’Keeffe Rosetti MC. Risk adjustment using automated ambulatory pharmacy data: the RxRisk model.[see comment]. Med Care. 2003;41(1):84–99. [DOI] [PubMed]
- 34.Gilmer T, Kronick R, Fishman P, Ganiats TG. The Medicaid Rx model: pharmacy-based risk adjustment for public programs. Med Care. 2001;39(11):1188–202. [DOI] [PubMed]
- 35.Perkins AJ, Kroenke K, Unutzer J, et al.. Common comorbidity scales were similar in their ability to predict health care costs and mortality. J Clin Epidemiol. 2004;57101040–8. [DOI] [PubMed]
- 36.Pietz K, Petersen LA. Comparing self-reported health status and diagnosis-based risk adjustment to predict 1- and 2 to 5-year mortality. Health Serv Res. 2007;42(2):629–43. [DOI] [PMC free article] [PubMed]
- 37.Kerr EA, Smith DM, Hogan MM, et al.. Building a better quality measure: are some patients with ‘poor quality’ actually getting good care? Med Care. 2003;41(10):1173–82. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(DOC 36.5 kb)


