Abstract
BACKGROUND
Percutaneous coronary intervention (PCI) is performed in many patients with stable coronary artery disease, despite evidence of little clinical benefit over optimal medical therapy.
OBJECTIVE
To examine physicians’ beliefs, practices, and decision-making regarding elective PCI.
DESIGN
Six focus groups, three with primary care physicians and three with cardiologists. Participants discussed PCI using hypothetical case scenarios. Transcripts were analyzed using grounded theory, and commonly expressed themes regarding the decision-making pathway to PCI were identified.
PARTICIPANTS
Twenty-eight primary care physicians and 20 interventional and non-interventional cardiologists in Butte County, Orange County, and San Francisco Bay Area, California, in 2006.
RESULTS
A number of factors led primary care physicians to evaluate non-symptomatic or minimally symptomatic patients for coronary artery disease and refer them to a cardiologist. The use of screening tests often led to additional testing and referral, as well as fear of missing a coronary stenosis, perceived patient expectations, and medicolegal concerns. The end result was a cascade such that any positive test would generally lead to the catheterization lab, where an “oculostenotic reflex” made PCI a virtual certainty.
CONCLUSIONS
The widespread use of PCI in patients with stable coronary artery disease—despite evidence of little benefit in outcomes over medical therapy—may in part be due to psychological and emotional factors leading to a cascade effect wherein testing leads inevitably to PCI. Determining how to help physicians better incorporate evidence-based medicine into decision-making has important implications for patient outcomes and the optimal use of new technologies.
Electronic Supplementary Material
The online version of this article (doi:10.1007/s11606-008-0706-x) contains supplementary material, which is available to authorized users.
KEY WORDS: percutaneous coronary intervention, focus groups, physician decision-making, qualitative study
INTRODUCTION
Coronary artery disease (CAD) is the leading cause of morbidity and mortality in the United States and is a major cause of rising health care costs, with estimated direct and indirect costs of $142.5 billion in 2003.1 Recent technological advances, such as computed tomography (CT) angiography and electron beam CT (EBCT), have allowed detection of coronary atherosclerosis in asymptomatic patients, also known as screening. Some physicians have called for increased screening of patients with intermediate cardiac risk by Framingham criteria.2–4 Aggressive direct marketing to the public and extensive media coverage5 have also increased public demand for new cardiac screening tests.6,7 The increase in testing of asymptomatic persons has paralleled a rise in revascularization rates,8,9 particularly with percutaneous coronary interventions (PCI), with over 1.2 million PCIs done in the United States in 2003.10
Despite the ability to identify subclinical disease, current evidence does not show benefit of PCI for patients with asymptomatic or minimally symptomatic CAD. Trials have demonstrated no decrease in risk of mortality or myocardial infarction (MI) after PCI, compared to optimal medical therapy, in patients with stable CAD.11–14 PCI can provide symptomatic relief for patients with angina, but in one study, 23% of patients undergoing PCI were asymptomatic, and of those patients almost two-thirds reported no change in or worse quality of life.15
Despite the evidence that PCI does not decrease the risk of future cardiac events when added to optimal medical therapy, rates of PCI have risen by 326% in the past decade, and a significant number of patients with stable CAD undergo PCI.16 It is not known what factors lead physicians to consistently recommend PCI over optimal medical therapy in patients with stable CAD. Since quantitative studies alone cannot explore in depth the clinical reasoning behind the decision to refer patients to PCI, we chose to conduct focus groups to assess the attitudes, beliefs, and practices of physicians that lead to the current pattern of diagnosis and treatment for patients with stable CAD.
METHODS
Study Design and Setting
We conducted six focus groups throughout California in rural, suburban, and urban areas between April and September 2006. We chose to conduct focus groups because it is a useful methodology to explore complex, rapidly changing phenomena and for exploratory studies in areas in which previous literature is limited.17 The study was approved by the University of California San Francisco Committee on Human Research.
Recruitment
We used network sampling (recommendations from other physicians) and purposeful sampling (selecting for certain characteristics) strategies to ensure that thought leaders from the community and diverse viewpoints would be represented. Cardiologists and primary care physicians (PCP) were recruited via recommendations from local physicians in leadership positions in the American College of Cardiology and the Society for Cardiovascular Angiography and Interventions, although membership in either organization was not required for participation. For PCP groups, internists and family practitioners were invited; for cardiologist groups, interventional and noninterventional cardiologists were invited. Physicians were recruited from solo, group, and academic practice settings. All respondents were accepted. Invitations were sent to a total of 275 physicians (148 PCPs, 127 cardiologists). A heterogeneous group of 28 PCPs and 20 cardiologists participated (Table 1). All participants gave written, informed consent.
Table 1.
Characteristics of Focus Group Members
| Characteristic | Total (%) | Butte County (rural) | Orange County (suburban) | SF Bay area (urban) |
|---|---|---|---|---|
| Primary care physicians | 28 | 6 | 10 | 12 |
| Male | 21 (75) | 5 | 9 | 7 |
| Family practice | 7 (25) | 3 | 3 | 1 |
| Internal medicine | 21 (75) | 3 | 7 | 11 |
| Mean age in years (range) | 47.1 (32–68) | 44.5 | 46.7 | 48.9 |
| Mean years in practice (range) | 16.4 (3–36) | 13.9 | 16.0 | 18.1 |
| Type of practice | ||||
| Academic | 3 (11) | 0 | 0 | 3 |
| Multi-specialty group | 12 (43) | 4 | 6 | 2 |
| Solo, other | 13 (46) | 2 | 4 | 7 |
| Cardiologists | 20 | 7 | 4 | 9 |
| Male | 18 (90) | 6 | 4 | 7 |
| Interventional cardiologist | 7 (35) | 3 | 1 | 3 |
| Mean age in years (range) | 55.5 (35–85) | 54 | 60.5 | 53.5 |
| Mean years in practice (range) | 26.1 (1–54) | 23.4 | 27.3 | 28 |
| Type of practice | ||||
| Academic | 3 (15) | 0 | 3 | 0 |
| Multi-specialty group | 14 (70) | 5 | 1 | 8 |
| Solo | 3 (15) | 2 | 0 | 1 |
Focus Groups
PCPs and cardiologists were interviewed in separate groups to encourage frank discussion. All groups were led by one or more of the authors. Focus groups were semi-structured, with the moderator using a focus group guide and three hypothetical case scenarios to facilitate discussion (Appendix, available online).18 All scenarios represented cases where the available evidence suggested no outcome benefit from PCI (Table 2). The cases were pilot tested on cardiology fellows and general internal medicine fellows from the University of California, San Francisco for clarity and representation of common clinical scenarios, and were modified based on their feedback. The participants were presented with each case scenario one step at a time and were asked what they would do at each step. In all scenarios, the patient had one or more significant coronary stenoses found after cardiac catheterization. The moderator invited participation from all group members, and provided factual data when necessary, including data from relevant clinical trials, to assist group members in interpreting the case scenarios and to stimulate discussion.
Table 2.
Hypothetical Case Scenarios Presented to Focus Group Participants
| Three case scenarios |
|---|
| Case 1 |
| History: 45-year-old asymptomatic man with a family history of MI, who presents after a calcium scan showed a score of 745 |
| Diagnostic test results: Exercise treadmill test. The patient goes 11 minutes on the Bruce protocol and has 1–2 mm ST depression at peak exercise |
| Catheterization results: Tight lesion in his left anterior descending artery |
| Case 2 |
| History: 55-year-old woman smoker complains of a sharp pain in her chest. It is not associated with exercise, and occurs mostly in the evening |
| Diagnostic test results: Exercise SPECT showed decreased tracer uptake in the anteroseptal region |
| Catheterization results: Tight lesions in her proximal right coronary artery and posterior descending artery |
| Case 3 |
| History: 60-year-old man presents because he gets tired more easily in the evenings. He has no chest pain or shortness of breath |
| Diagnostic test results: Exercise treadmill test with thallium imaging. The patient goes 6 minutes on the Bruce protocol and achieves 70% of maximum predicted heart rate. The EKG shows 1/2 mm ST depressions and thallium images show mild reversibility in the inferolateral region with a normal ejection fraction |
| Catheterization results: 70% focal lesion in the left circumflex artery |
MI = myocardial infarction; SPECT = single positron emission computed tomography; EKG = electrocardiogram
Data Analysis
Discussions were audiotaped and transcribed. Analysis was done according to grounded theory, a qualitative method in which data are categorized and explanatory theories emerge from the data.19 Transcripts and notes were independently read and coded by two investigators (GAL, RFR) using QSR N-VIVO 7.0 software (QSR International, Doncaster, Australia). The constant comparison method was used for coding, applying codes identified in the first transcript to subsequent transcripts, and adding codes as new themes emerged.20 The coded data from the two investigators (GAL, RFR) was then combined and organized into major themes. The major themes were then discussed, revised, and agreed upon by all three investigators. The transcripts were then reviewed and re-coded on the basis of the major themes. Two methods of triangulation were used to reduce bias in the analysis: investigator triangulation (multiple investigators attended the focus groups and/or reviewed the transcripts) and disciplinary triangulation (the investigators represented different areas of expertise).21 A set of common themes seen throughout all focus groups was extracted from the coding and agreed upon by all investigators.
Respondent Validation
To validate our findings, each participant was sent a summary of major themes from their own focus group and asked to rate their agreement with the summary points.22
RESULTS
We report only major themes appearing in all groups. Based on group summaries sent to the participants, 27 of 28 PCPs strongly agreed or agreed with the summary; one PCP did not respond. Eighteen of 20 cardiologists strongly agreed or agreed with the summary; one cardiologist neither agreed nor disagreed with the summary, and one cardiologist disagreed with the summary.
The Role of Screening Tests
Although PCPs disagreed about the utility of new screening tests such as EBCT or CT angiography, they all agreed they would not order testing for patients with a low pre-test probability of CAD. However, if a patient self-referred for a screening test, physicians were uncomfortable not doing additional testing, regardless of their opinions about the value of EBCT results. “Unfortunately now he has this test result [from EBCT] that we probably wouldn’t have ordered, but you can’t ignore it, you have to do something,” remarked one PCP. Cardiologists also debated the use of EBCT and CT angiography as screening tests, and while there was disagreement about the appropriate use of these tests, they took a “positive” screening result such as a high calcium score as evidence of CAD and proceeded to recommended further testing and aggressive treatment.
The Role of Fear and the Preference for Intervention
Fear of missing a coronary lesion that may later cause problems for a patient was commonly cited as a reason for further testing by both PCPs and cardiologists, particularly in younger patients. “I had a friend who was 42, healthy, and dropped dead after jogging one day. I’m always afraid to miss a ‘widow-maker’ lesion, and those are the lesions you worry most about,” said one PCP. Because of anxiety about missing lesions, action was perceived to be better than inaction. In addition, cardiologists appeared to regard using only medical therapy to treat a patient with a significant lesion as providing substandard care. They generally believed that opening a stenosed artery was beneficial, regardless of the patient’s symptom status and despite their recognition that the procedure did not prevent MI or death.
Perception of Patient Expectations
PCPs felt that patients believe there are benefits to having a test and this made them more willing to order tests. “People want more tests. Tests are a good thing. I don’t think people think about all the possible results—they get tests for reassurance,” said one PCP. “Some huge percentage of people would want to be screened for a disease even if nothing can be done about it. It reminds us of what expectations are,” remarked another PCP. Both PCPs and cardiologists also believed that a patient wanted and expected additional testing after any positive or equivocal test result, stating that the additional testing would help relieve patient anxiety.
Cardiologists stated that they were also influenced by the perception that patients preferred the less invasive PCI procedure over surgery, leading them to recommend PCI in most situations. The cardiologists raised this point even though medical therapy would have been a more appropriate comparison than surgery for the patients in the cases. “Everyone said PCI, but I think it depends whether his lesions are amenable—are you going to send this asymptomatic guy for CABG?” one cardiologist said.
Non-clinical Issues: Medicolegal Liability and Financial Incentives
PCPs cited medicolegal liability as a reason for referral to a cardiologist. “In the back of all of our minds are the legal concerns here. Even doing a stress echo without cardiology follow-up opens somebody up to potential disaster,” said one PCP. This concern prompted referral even if the PCP thought medical management was appropriate. “We would feel more comfortable treating patients medically if we weren’t worried about being sued. If the cardiologist tells me it’s okay to treat him medically then I feel the burden’s been taken off me, whereas if I make that decision and the patient has an MI, what kind of risk am I putting myself at?” said one PCP.
Participants in all groups placed greater weight on the risk of not intervening than on the risk of complications from procedures when making treatment decisions. “Look, if you didn’t do something and something happened, you’d be sued. If you put in a stent and there’s an event, that’s a typical, expected complication,” stated a cardiologist.
The payment structure of health care was also mentioned as an important factor in physician decision-making. There were several points of view from which finances entered the discussion—the patient and their out of pocket costs, the payer, and the physician. Several PCPs felt that some patients would prefer a procedure to medical therapy because the costs of a PCI would be fully covered under their insurance plan while medications often involved out-of-pocket costs. In addition, PCPs felt that the treatment recommendation of PCI or medical therapy was often influenced by the type of practice the cardiologist was a part of (i.e., fee-for-service versus managed care). Cardiologists in our groups did not extensively discuss the financial incentives related to PCI; however, one cardiologist practicing in a capitated environment noted that he routinely recommended PCI for patients with stable CAD even though he would not benefit financially.
The Cascade Effect of Testing
All of the above reasons influenced physicians to order more testing, which would eventually lead to a referral to a cardiologist and an intervention. Regardless of whether they would have ordered the test in the first place, PCPs stated that they felt obligated to refer patients to a cardiologist after any positive or equivocal workup for CAD. “It’s a game of hot potato where the calcium score is 745, what are you going to do with it? I wouldn’t be comfortable until a cardiologist has seen this. This guy’s wife has bought him much more than a CT scan—she’s bought him the entrée into the whole garden path of tests...any kind of equivocal result and I think he’s going to be in the cath lab,” said one PCP. The tendency to refer patients with positive tests to cardiologists was also due in part to a concern that their own knowledge base was not up to date. One PCP said, “I’m far enough out of residency now that I don’t know what the latest evidence is. That’s why I send the patient to the cardiologist—I assume they know the correct thing to do.” PCPs stated that they did not have any input into treatment decisions after referral, and expected cardiologists to make appropriate recommendations for treatment.
Among the cardiologists, although there was acknowledgment that PCI was an invasive procedure with risks, PCI was the recommended treatment for all amenable stenoses. “Generally I consent the patients for cath and PCI at the same time. You don’t want to expose the patient to extra risk by sticking their groin again. You already have the sheath in, so mostly you just go ahead and do it,” said one cardiologist.
The “Oculostenotic Reflex”
Cardiologists referred to “the oculostenotic reflex,”23 which guaranteed that if an amenable lesion was found in the catheterization laboratory, all patients (even asymptomatic) would receive a stent. This action was based on the strong belief that PCI benefited patients with stable CAD. “Since 1970 we’ve had a drop in mortality, so even if we don’t have the clinical data, whatever we’re doing has worked,” said one cardiologist.” Even when challenged about the lack of benefit of adding PCI to optimal medical therapy in preventing future cardiac events, most cardiologists still felt that any patient with a significant coronary stenosis should get PCI, even while acknowledging the evidence. “We all agree that we don’t know if we’re doing the right thing, but if there’s a lesion, we’ll fix it,” remarked a cardiologist. Another added, “Because we’ve gotten to the cath lab, even though I can’t connect any of the dots that make any sense in terms of explaining [the reason for the procedure] to somebody, the likelihood is that patient leaves the cath lab with an open artery, if it’s technically doable at low risk.” This chasm between knowledge and behavior was present throughout all the group discussions, and was acknowledged even by salaried cardiologists in our groups.
DISCUSSION
We found that psychological and emotional factors played an important role, often prevailing over evidence from clinical trials, in physician decision-making for patients with stable CAD. Despite physician knowledge that the current available evidence shows that PCI does not prevent MI or death in patients with stable CAD, their statements suggested that they often downplayed or even ignored this evidence when making decisions about testing and treatment for patients with CAD. In addition, the ease and availability of PCI, along with the perceived low risk of the procedure, led physicians to recommend PCI even for patients in whom clinical benefit has not been clearly demonstrated.
Our data suggest that the initial test begins a cascade effect, first described by Mold and Stein in 1986 (Fig. 1).24 Faced with any positive test result, no matter how low the patient’s risk of CAD, physicians were uncomfortable without recommending further testing, referral, or procedure, which ultimately led to PCI. Physicians reported finding it difficult to interrupt the cascade. In addition, both PCPs and cardiologists endorsed a firm belief that PCI would prevent the MI and death from a “widow-maker lesion,” citing the “open-artery hypothesis (the notion that an open artery is better than a stenosed artery),”25 and thus they believed that stenoses should be opened, regardless of functional significance.
Figure 1.
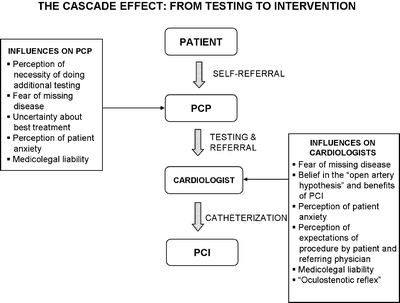
Cascade effect of screening for coronary artery disease. Representation of pathway from initial patient contact to percutaneous coronary intervention (PCI), based on results from focus groups of primary care physicians and cardiologists. Reasons for the use of PCI in asymptomatic or minimally symptomatic patients are listed for each step in the pathway.
In addition, the potential consequences of an invasive procedure had less emotional impact than the potential consequences of missing disease, such that physicians felt that doing an invasive procedure was almost always better for the patient. Acknowledging the tension between the available evidence and their feelings of what was best, physicians tended to justify a non-evidence-based approach (“I know the data shows there is no benefit, but”) by focusing on the ease of PCI and belief that an open artery was better while minimizing the risks of PCI. The above traits of physicians—the tendency for action, the belief in their decisions, the reliance on results and first hand experience rather than book knowledge—were previously described by Eliot Freidson in 1970 in his description of the clinical mentality,26 and suggest that simply providing evidence to physicians is not likely to change these long-standing behaviors from contributing to the cascade effect.
Both PCPs and cardiologists cited patients’ expectations as a major reason for further testing and treatment, even if the physician did not think further testing was necessary. Prior research suggests physician perceptions of patient preferences for more testing may be correct. Sox and colleagues found that patients with nonspecific chest pain felt that care was “better than usual” if they had diagnostic testing compared with no diagnostic testing,27 while Schwartz and colleagues found that 87% of patients thought that routine screening tests for cancer were a good idea, and that 86% of patients would have a free total-body CT scan if offered.28 This enthusiasm for testing, coupled with direct-to-consumer advertising for cardiac screening and media accounts of “life-saving” tests,5 may lead to increased patient demand. In addition, most patients erroneously believe that PCI can prevent future MI,29 which may lead to patient pressure for intervention. The above factors contribute to the perception among both PCPs and cardiologists that a test or procedure is the preferable course of action, particularly for avoiding malpractice lawsuits (although no data exist to support this theory) and pleasing patients. Paradoxically, greater use of tests has not been shown to equate to better outcomes for patients.30,31
Financial incentives also may help drive the expanded use of PCI. Previous studies have shown that payment mechanism and financial incentives can influence physician behavior and resource use.32–34 Given the current level of fee-for-service reimbursement for procedures, this may subtly encourage the use of PCI for patients with stable CAD, even though this possibility was not extensively discussed in our groups. The structure of the health care system itself may also encourage use of cardiac procedures; for example, the opening of cardiac specialty hospitals has been associated with an increased rate of cardiac catheterization and PCI.35 In addition, a recent systematic review found that studies that supported widespread use of drug-eluting stents (DES), compared with those that did not, were more likely to be of lower quality, from the United States, and industry sponsored, suggesting that market influences may play a role in the rapid expansion of unproven technologies.36 Aligning payment incentives to the appropriateness of physician decisions may help physicians use PCI more prudently. However, even physicians in our group who had no financial incentive to recommend PCI (e.g., PCPs and salaried cardiologists) tended to recommend treatment with PCI. This suggests that there may be a cultural bias toward technology overuse beyond financial incentives that affects physician behavior.
There are some limitations to our study. Our results reflect the opinions of the participants, who may have been affected by types of response bias in which participants may alter or conceal their opinions due to discomfort with some aspect of the group or moderator, may give responses they believe the interviewer wants to hear, and may avoid discussing controversial topics. However, the high level of participation, enthusiasm, and debate during our groups make these biases less likely, although certain controversial topics, such as the financial incentives to physicians for PCI, were not as widely discussed as other topics by our participants. Also, we were unable to obtain data on physicians who declined to participate, so the extent of selection bias is unknown. However, we conducted multiple focus groups in rural, suburban, and urban areas with physicians from several types of practices and consistent themes emerged, making it more likely that the opinions expressed reflect those of the general population of PCPs and cardiologists in California, although generalizability to other parts of the United States and to other countries may be limited. We used hypothetical clinical scenarios as a basis for discussion, which may not exactly mimic real-life clinical practice, and we presented only a few of many possible case scenarios. However, using clinical vignettes can provide valid measurements of the quality of care provided by physicians, particularly when focusing on processes of care.37–39 Exploring patients’ viewpoints could give further insight into physician decision-making; however, patient interviews were beyond the scope of this study. Finally, while qualitative methods provide in-depth insight into the process of physician decision-making, outcome measurements are necessary to assess the impact of physician decisions.
New technologies have led to the ability to diagnose and treat CAD even at early, asymptomatic stages and have led to the widespread use of PCI in populations for which benefits in quality of life and mortality have not been demonstrated. Our results show that PCPs play a key role in initiating the cascade to PCI. Many factors other than scientific evidence are operative in leading mildly or asymptomatic patients toward coronary angiography and PCI. These factors appear to be more powerful than evidence from clinical trials. This calls for more ways to ensure consistent incorporation of evidence into clinical decision-making. Building the evidence base lays the foundation, but alone often does not lead to change in physician behavior. Future work should focus on helping physicians balance clinical evidence, psychological and emotional factors, patient expectations, and use of the latest technologies to obtain optimal patient outcomes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgments
Drs. Lin, Dudley, and Redberg had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding/Support: This study was funded by the Blue Shield of California Foundation. Dr. Lin is supported by a Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant (T32).
Conference Presentations: Data from this study were presented at the Society of General Internal Medicine 30th Annual Meeting, Toronto, Ontario, April 25–28, 2007 and at the American Heart Association Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke Conference, Washington, D.C., May 10–11, 2007.
Financial Disclosures: Dr. Redberg serves as a member of the CV Therapeutics Women’s Advisory Board. Drs. Lin and Dudley report no financial disclosures.
Role of the Sponsor: The Blue Shield of California Foundation had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
We wish to thank the physicians who participated in our focus groups. We also wish to thank Janet Wright, MD, Morton Kern MD, Greg Thomas MD, Joshua Cohen MD, Gordon Fung, MD, Andrew Michaels MD and Ralph Brindis, MD, the UCSF Cardiology Fellows and General Internal Medicine Fellows for their feedback on case scenarios and assistance in suggesting physicians. We also acknowledge the assistance of Stephen Crane, Luciana Garcia, and Eunice Chee in setting up the focus groups.
Conflict of Interest: None disclosed.
Footnotes
Funding/Support: This study was funded by the Blue Shield of California Foundation. Dr. Lin is supported by a Ruth L. Kirschstein National Research Service Award (NRSA) Institutional Research Training Grant (T32).
Conference Presentations: Data from this study were presented at the Society of General Internal Medicine 30th Annual Meeting, Toronto, Ontario, April 25–28, 2007 and at the American Heart Association Quality of Care and Outcomes Research in Cardiovascular Disease and Stroke Conference, Washington, D.C., May 10–11, 2007.
Electronic Supplementary Material
The online version of this article (doi:10.1007/s11606-008-0706-x) contains supplementary material, which is available to authorized users.
References
- 1.Mensah GA, Brown DW. An overview of cardiovascular disease burden in the United States. Health Aff (Millwood). 2007;26(1):38–48. [DOI] [PubMed]
- 2.Lepor NE. Screening CT-Coronary angiography: ready for prime time? Rev Cardiovasc Med. 2006;7:198–204. [PubMed]
- 3.Naghavi M, Falk E, Hecht HS, et al. From vulnerable plaque to vulnerable patient-Part III: executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol. 2006;98(2A):2H–15H, Jul 17. [DOI] [PubMed]
- 4.Greenland P, Smith SC, Grundy SM. Improving coronary heart disease risk assessment in asymptomatic people: role of traditional risk factors and non-invasive cardiovascular tests. Circulation. 2001;104:1863–7. [DOI] [PubMed]
- 5.Gorman C, Park A. How new heart-scanning technology could save your life. Time; 2005; Aug. 28. [PubMed]
- 6.Lee TH, Brennan TA. Direct-to-consumer marketing of high-technology screening tests. N Engl J Med. 2002;346:529–31. [DOI] [PubMed]
- 7.Taylor AJ, O’Malley PG. Self-referral of patients for electron-beam computed tomography to screen for coronary artery disease. N Engl J Med. 1998;339(27):2018–20. [DOI] [PubMed]
- 8.Wennberg DE, Birkmeyer JD, Birkmeyer NJO, et al. The Dartmouth Atlas of Cardiovascular Care. Chicago: AHA Press; 1999.
- 9.Wennberg DE, Kellett MA, Dickens JD, Malenka DJ, Keilson LM, Keller RB. The association between local diagnostic testing intensity and invasive cardiac procedures. JAMA. 1996;275:1161–4. [DOI] [PubMed]
- 10.American Heart Association. Heart Disease and Stroke Statistics - 2006 Update. Dallas, TX: American Heart Association; 2006.
- 11.Boden WE, O’Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503–16. [DOI] [PubMed]
- 12.Bucher HC, Hengstler P, Schindler C, Guyatt GH. Percutaneous transluminal coronary angioplasty versus medical treatment for non-acute coronary heart disease: a meta-analysis of randomised controlled trials. BMJ. 2000;321:73–7. [DOI] [PMC free article] [PubMed]
- 13.Katritsis DG, Ioannidis JP. Percutaneous coronary intervention versus medical therapy in nonacute coronary artery disease. Circulation. 2005;111:2906–12. [DOI] [PubMed]
- 14.Pitt B, Waters D, Brown WV, et al. Aggressive lipid-lowering therapy compared with angioplasty in stable coronary artery disease. Atorvastatin versus Revascularization Treatment Investigators. N Engl J Med. 1999;341:70–6. [DOI] [PubMed]
- 15.Spertus JA, Salisbury AC, Jones PG, Conaway DG, Thompson RC. Predictors of quality-of-life benefit after percutaneous coronary intervention. Circulation. 2004;110:3789–94. [DOI] [PubMed]
- 16.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics-2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115(5):e69–e171. [DOI] [PubMed]
- 17.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311:42–5. [DOI] [PMC free article] [PubMed]
- 18.Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. Thousand Oaks, CA: Sage Publications, Inc.; 2002.
- 19.Glaser B, Strauss A. The Discovery of Grounded Theory. Chicago: Aldine; 1967.
- 20.Strauss A, Corbin J. Basics of Qualitative Research: Grounded Theory Procedures and Techniques. Newbury Park, CA: Sage Publications; 1990.
- 21.Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34:1189–208. [PMC free article] [PubMed]
- 22.Barbour RS. Checklists for improving rigour in qualitative research: a case of the tail wagging the dog? BMJ. 2001;322:1115–7. [DOI] [PMC free article] [PubMed]
- 23.Topol EJ, Nissen SE. Our occupation with coronary luminology: the dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333–42. [DOI] [PubMed]
- 24.Mold JW, Stein HF. The cascade effect in the clinical care of patients. N Engl J Med. 1986;314(8):512–4. [DOI] [PubMed]
- 25.Kim CB, Braunwald E. Potential benefits of late reperfusion of infarcted myocardium. The open artery hypothesis. Circulation. 1993;88(5 Pt 1):2426–36. [DOI] [PubMed]
- 26.Freidson E. Profession of Medicine: A Study of the Sociology of Applied Knowledge. New York: Harper and Row; 1970.
- 27.Sox HC, Margulies I, Sox CH. Psychologically mediated effects of diagnostic tests. Ann Intern Med. 1981;95:680–5. [DOI] [PubMed]
- 28.Schwartz LM, Woloshin S, Fowler FJ, Welch HG. Enthusiasm for cancer screening in the United States. JAMA. 2004;291:71–8. [DOI] [PubMed]
- 29.Holmboe ES, Fiellin DA, Cusanelli E, Remetz M, Krumholz HM. Perceptions of benefit and risk of patients undergoing first-time elective percutaneous coronary revascularization. JGIM. 2000;15(9):632–7. [DOI] [PMC free article] [PubMed]
- 30.Fisher ES, Welch HG. Avoiding the unintended consequences of growth in health care. JAMA. 1999;281:446–53. [DOI] [PubMed]
- 31.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in Medicare spending. Part 2: Health outcomes and satisfaction with care. Ann Intern Med. 2003;138:273–87. [DOI] [PubMed]
- 32.Hickson GB, Altemeier WA, Perrin JM. Physician reimbursement by salary or fee-for-service: effect on physician practice behavior in a randomized prospective study. Pediatrics. 1987;80(3):344–50, Sep. [PubMed]
- 33.Hillman AL, Pauly MV, Kerstein JJ. How do financial incentives affect physicians’ clinical decisions and the financial performance of health maintenance organizations? N Engl J Med. 1989;321(2):86–92, Jul 13. [DOI] [PubMed]
- 34.Shen J, Andersen R, Brook R, Kominski G, Albert PS, Wenger N. The effects of payment method on clinical decision-making: physician responses to clinical scenarios. Med Care. 2004;42(3):297–302, Mar. [DOI] [PubMed]
- 35.Nallamothu BK, Rogers MAM, Chernew ME, Krumholz HM, Eagle KA, Birkmeyer JD. Opening of specialty cardiac hospitals and use of coronary revascularization in Medicare beneficiaries. JAMA. 2007;297:962–8. [DOI] [PubMed]
- 36.Ligthart S, Vlemmix F, Dendukuri N, Brophy JM. The cost-effectivenss of drug-eluting stents: a systematic review. CMAJ. 2007;176(2):199–205. [DOI] [PMC free article] [PubMed]
- 37.Dresselhaus TR, Peabody JW, Luck J, Bertenthal D. An evaluation of vignettes for predicting variation in the quality of preventive care. J Gen Intern Med. 2004;19(10):1013–8, Oct. [DOI] [PMC free article] [PubMed]
- 38.Peabody JW, Luck J, Glassman P, Dresselhaus TR, Lee M. Comparison of vignettes, standardized patients, and chart abstraction: a prospective validation study of 3 methods for measuring quality. JAMA. 2000;283(13):1715–22, Apr 5. [DOI] [PubMed]
- 39.Peabody JW, Luck J, Glassman P, et al. Measuring the quality of physician practice by using clinical vignettes: a prospective validation study. Ann Intern Med. 2004;141(10):771–80, Nov 16. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.


