Summary
What is already known about the topic?
Highly active antiretroviral therapy has dramatically decreased morbidity and mortality and improved the quality of life in persons with HIV
Medication-taking self-efficacy beliefs may predict medication adherence in persons with HIV.
Depressive symptoms and perceived social support consistently influence medication-taking self-efficacy beliefs
What this paper adds.
Depressive symptoms mediated the prediction of medication-taking self-efficacy by perceived social support.
Medication adherence self-efficacy mediated the prediction of self-reported medication adherence by perceived social support and depressive symptoms as self-efficacy theory suggests.
This study provides researchers with increased understanding of the mediating role of medication-taking self-efficacy beliefs between selected psychological variables and self-reported medication adherence in persons with HIV.
Background
To date, only a few studies have examined the mediating role of self-efficacy on the relationship between depressive symptoms or perceived social support and medication adherence in persons with HIV.
Objectives
The purpose of this study was to examine the impact of perceived social support, depressive symptoms and medication-taking self-efficacy on self-reported medication adherence in persons with HIV. A proposed comprehensive model included three mediation hypotheses in order to examine the mediating roles of medication-taking self-efficacy and depressive symptoms
Method
Baseline data from “Adherence to Protease Inhibitors” were used. The 215 persons with HIV aged 19–61 (mean= 40.7, SD= 7.58) were recruited from multiple sites in Pittsburgh, PA (USA) and through self-referral. The participants were assessed using the Beck Depression Inventory, Interpersonal Support Evaluation List, the Medication Taking Self-Efficacy Scale, and the modified Morisky Self-report Medication Taking Scale. Structural equation modeling (EQS version 6.1) was used. The Satorra-Bentler Scaled χ2 test statistics (S-B χ2), comparative fit index (CFI), and the Standardized Root Mean Squared Residual (SRMR) were used to assess the fit of a comprehensive model including three mediation hypotheses.
Results
A comprehensive model with the three hypotheses showed a good model fit (S-B χ2 (24, N=215) = 69.06, p<.001; CFI=0.95; SRMR=0.057). Medication adherence self-efficacy fully mediated the prediction of self-reported medication adherence by perceived social support and depressive symptoms. Depressive symptoms partially mediated the prediction of medication-taking self-efficacy by perceived social support
Conclusions
The findings of this study provide researchers with increased understanding of the mediating role of medication-taking self-efficacy beliefs between selected psychological variables and self-reported medication adherence in persons with HIV. Future studies need to test the moderating effect of gender, ethnicity and risk factors for HIV on this model and the intervention effect of self-efficacy beliefs using longitudinal data.
Keywords: Mediation, medication-taking self-efficacy, highly active antiretroviral therapy regimen adherence
1. Introduction
Highly active antiretroviral therapy (HAART) has dramatically decreased morbidity and mortality and improved the quality of life in persons with HIV infection; however, these benefits of HAART are dependent upon adherence to medication (Hsu et al., 2001; Simoni et al., 2002). Studies have shown that the optimal adherence rate of 95% for HAART is rare (Lewis and Abell, 2002; Read et al., 2003). Therefore, researchers have sought to identify factors influencing medication adherence in order to develop interventions to enhance medication adherence(Hsu et al., 2001; Simoni et al., 2002).
Evidence has been accumulating that medication-taking self-efficacy beliefs, a person’s confidence to adhere medication regimen, predict HAART regimen adherence (Godin et al., 2005; Malcolm et al., 2003; Murphy et al., 2003). Psychosocial factors such as perceived social support and mood affect medication self-efficacy beliefs in persons with HIV(Simoni et al., 2006; Simoni et al., 2002; Weaver et al., 2005). Perceived supportive relationships and a positive mood increased self-efficacy beliefs(Power et al., 2003; van Servellen and Lombardi, 2005); while decreases in self-efficacy beliefs have been noted due to the moderating effects of the presence of depressive symptoms (Ferguson et al., 2002; Simoni et al., 2006).
The mechanism to influence medication self-efficacy remains unclear; yet, studies have found that greater perceived social support may augment a person’s optimism and coping strategies, and that enhanced optimism and coping predicted medication adherence (Godin et al., 2005; Weaver et al., 2005). Moreover, increased perceived social support may improve a person’s self-esteem, diminish one’s hopelessness, and reduce cognitive impairment or forgetfulness resulting from depression (Simoni et al., 2006).
Investigators have demonstrated that non-clinical levels of depression can be buffered by perceived social support (Jia et al., 2004; Schrimshaw, 2003; Simoni et al., 2006). In a sample of 332 women infected with HIV, Gielen and colleagues (2001) found that those with a larger social support network had better mental health and quality of life. Depressive symptoms mediated the relationship between quality of life and social support in men with HIV (Jia et al., 2004). HIV infected women who lacked a social support source experienced a high, yet non-clinical level of depressive symptoms (Schrimshaw, 2003). Simoni and colleagues (2006) have evaluated a 3-month social support intervention with 136 persons with HIV. Their conceptual model was derived from their pilot study (n=50) examining mediation effects of affective factors and self-efficacy beliefs between perceived social support and HAART regimen adherence (Simoni et al., 2002). They found that less social support predicted an increased non-clinical level of depression, and higher depression predicted lower medication self-efficacy beliefs.
Testing mediation models is important in experimental and non-experimental studies as these models provide researchers with significant insight into a definitive and plausible causal mechanism for designing effective intervention studies (Shrout and Bolger, 2002). Researchers are showing a rising interest in the mechanism between psychological factors (e.g., depressive symptoms and perceived social support) and specific behavior outcomes (e.g., medication adherence) in studies of patients with HIV/AIDS (Jia et al., 2004; Simoni et al., 2006; Weaver et al., 2005). To date, however, only a few studies have examined the mediating role of self-efficacy on the relationship between depressive symptoms or perceived social support and medication adherence in person with HIV (PWHIV).
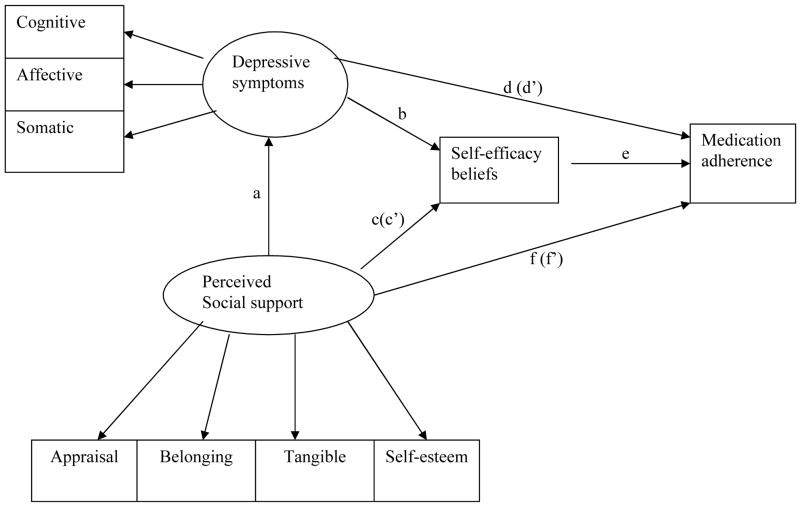
The purpose of this study was to examine the impact of perceived social support, depressive symptoms and medication-taking self-efficacy on self-reported medication adherence in persons with HIV. A proposed comprehensive model included three mediation hypotheses in order to examine the mediating roles of medication-taking self-efficacy and depressive symptoms. The hypotheses were: 1) medication-taking self-efficacy will mediate the negative relationship between depressive symptoms and self-reported medication adherence, 2) medication-taking self-efficacy will mediate the positive relationship between perceived social support and self-reported medication adherence, and 3) depressive symptoms will mediate the positive relationship between perceived social support and medication-taking self-efficacy in PWHIV (see Figure 1).
Figure 1. The conceptual model of this study.
*parentheses indicate the changes of the relationship between independent and dependent variables after adjusting for a mediator
2. Methods
This study used baseline data collected from participants enrolled in the clinical trial “Adherence to Protease Inhibitors” (NIH R01 NR04749). Social cognitive and self-efficacy theories provided the framework for the larger study which was designed to test the effectiveness of a telephone-delivered medication adherence intervention for PWHIV over time. The study was approved by the University of Pittsburgh Institutional Review Board.
2.1. Sample
Two-hundred fifteen participants were recruited from HIV/AIDS primary care clinics located in a predominantly urban setting and through self-referral. The inclusion criteria for the study were (1) 18 years of age or older, (2) the ability to read and understand English, (3) being without HIV dementia as determined by the HIV dementia scale (Power et al., 1995), and (4) having access to a telephone.
2.2. Procedure
All enrolled participants provided informed written consent. Although participants completed study measures at baseline, at 12 weeks (post intervention), and at four other time points for the larger study, only baseline data were used for the current study. The Beck Depression Inventory-II (Beck and Steer, 1987), the Interpersonal Support Evaluation List (Cohen et al., 1985), the HIV Medication-Taking Self-Efficacy Scale (Cha et al., 2004), and one item from the modified Morisky Self-report Medication-Taking Scale (Morisky et al., 1986) were used to assess the variables in this study.
2.3. Instruments
Depressive symptoms were assessed using the Beck Depression Inventory-II (BDI-II), a 21-item instrument used to screen for major depression for clinical purposes (Beck and Steer, 1987). Items reflect cognitive, affective, and somatic symptoms of depression according to four levels of severity (Johnson et al., 2006). The item responses range from 0 to 3 and the possible range of scores on the BDI-II is 0 to 63. Scores less than 13 indicate minimal to no depressive symptoms; scores greater than 29 indicate severe level of depressive symptoms. Scores ranging from 14 to19 and 20 to 28 indicate mild and moderate levels of depressive symptoms, respectively. The Cronbach’s alpha for the BDI-II was .92 in a study using 500 psychiatric outpatients (Kalichman et al., 1995). In this study, the Cronbach’s alpha for the BDI-II was .91, and the Cronbach’s alphas for the cognitive, affective, and somatic subscales were .85, .74, and .83, respectively.
Perceived social support was assessed with the Interpersonal Support Evaluation List instrument (ISEL). The 40-item ISEL measures perceived availability of potential social support (Cohen et al., 1985). The ISEL was developed originally to assess overall functional support and four separate functions of social support: appraisal, belonging, tangible, and self-esteem (Cohen et al., 1985). The appraisal subscale measures the availability of persons to discuss concerns; the belonging subscale measures the perceived availability of persons with spending time to do something; the tangible subscale measures perceived availability of material aid and the self-esteem subscale measures the perceived positive feelings people have about themselves compared to others. Twenty items regarding social relationships are positively worded, while the remaining items are stated in a negative manner. The item responses range from 0 to 3. Reverse coding is applied to items that are negatively stated and items are totaled to yield summary scores. Higher scores indicate greater perceived social support. Cronbach’s alphas for the total scale range from .88 to .90 in the general population (Cohen et al., 1985). In the present study, the Cronbach’s alphas for appraisal, belonging, tangible, and self-esteem subscales were .89, .89, .90, and .82, respectively. The Cronbach alpha’s for the total ISEL was .96.
Medication-taking self-efficacy was assessed with the self-efficacy beliefs subscale of the HIV Medication-Taking Self-Efficacy Scale (HIV SES). This instrument was developed by Erlen and colleagues for the larger study to measure one’s self-efficacy beliefs regarding the taking of antiretroviral therapy. Participants are asked to rate their level of confidence using a 10-point Likert scale (not confident [1] to totally confident [10]). The 17 items of the self-efficacy beliefs subscale provide an assessment of the degree of confidence that individuals have under particular conditions regarding their ability to adhere to the medication regimen. The Cronbach’s alpha of the self-efficacy beliefs subscale was .96 (Cha et al., 2004).
Medication adherence was assessed with one item from the modified Morisky Self-report Medication Taking Scale. The item uses a dichotomous response (yes=0, no=1). In regard to their adherence participants are asked to identify whether they missed any doses of their HIV medication over the past two weeks.
2.4. Data Analysis Procedure
Prior to data analysis, the dataset was examined for data accuracy, the amount and pattern of missing responses, and outliers with SPSS for Windows version 12.0 (SPSS, Inc, Chicago, IL). The original dataset consisted of 217 subjects; however, two subjects were omitted for the final data analysis because they had more than 20% missing data on more than one instrument. Because of extremely low scores on the HIV SES, one subject was identified as a univariate outlier. However, this subject was included in the final data analysis, as the subject did not alter the results. As a preliminary step, descriptive statistics and Pearson product moment correlations were computed.
Structural equation modeling requires an adequate sample size based on model complexity. The ideal ratio of number of subjects to number of free parameters is 20:1; but a realistic target ratio is a10:1 (Kline, 1998). Accordingly, the retained 215 subjects was sufficient sample size to test our comprehensive model with 21 free parameters using structural equation modeling.
The analysis for mediation was performed through the bootstrap method using EQS 6.1 for Windows (Bentler and Wu, 2002) and SPSS for windows version 12.0. Recent studies have found that the bootstrap method is a more accurate and powerful method to examine mediation in terms of measuring an indirect effect than the Sobel test when data are skewed and the sample size is less than 400 (Preacher and Hayes, 2004; Shrout and Bolger, 2002) as the Sobel test uses Z-scores that assume normal distribution of the data. Given this, robust methods and the bootstrap method were used for estimation because the data in the current study were not normally distributed, and the sample size was below 400.
The direct effect was assessed using a regression coefficient and Z-test. One thousand bootstrap replications were performed to create a bootstrap sample for estimating the indirect effect of mediation analyses. The indirect effect was assessed with a 95% confidence interval (CI) of the indirect effect in the empirical sampling distribution. When a 95% confidence interval includes 0, then the indirect effect will not be significant.
The individual hypotheses (Hypothesis 1, 2, and 3) were examined prior to examining model fits of the comprehensive model (see Figure 1). The three hypotheses were combined into one model to find a parsimonious model to explain the mediation roles of medication adherence self-efficacy and depressive symptoms on self-reported medication taking adherence in persons with HIV. The results of the Wald test (for dropping parameters) and Lagrange Multiplier test (LM test; for adding parameters) enabled the researchers to find a parsimonious model. The Satorra-Bentler Scaled χ2 test statistics (S-B χ2), comparative fit index (CFI), and the Standardized Root Mean Squared Residual (SRMR) were used to assess the fit of a comprehensive model including three mediation models. The CFI indicates the proportion in the improvement of the overall fit of the researcher’s model relative to a null model that has no relationships among observed variables (Kline, 1998). A CFI of .95 or greater indicates a good fit and is less affected by sample size. The SRMR refers to the standardized difference between the observed covariance and predicted covariance. An SRMR of .08 or lower indicates a good fit (Hu and Bentler, 1999; Kline, 1998).
3. Findings
The sample of 215 was predominantly male (n=145; 67.4%) and white (n=134, 62.3%). The mean age was 40.66 years (SD=5.58; range=19–61). Nearly half of the participants (n=102, 47.4%) lived alone. Only 65 (30.2%) participants were currently employed. Eleven participants (5.1%) had no form of health care insurance. More than half of the participants reported that they experienced some financial difficulty meeting their basic needs. Approximately 39% (n=83) of the participants reported that they were taking anti-depressant medication. When asked about HIV medication-taking, more than one-third of the participants experienced problems taking their medication; however, only 65 participants used various aids to remind them to take their medication (see Table 1).
Table 1.
Sample characteristics (n=215)
| Characteristics | n (%) |
|---|---|
| Age (years) | |
| Mean | 40.7 |
| SD | 5.6 |
| Median | 40.0 |
| Range | 19– 61 |
|
| |
| Present living status | |
| Live alone | 102 (47.4) |
| Living with other adults | 111 (52.1) |
| Living with child(ren) | 47 (22.1) |
|
| |
| Current employment | |
| Employed | 65 (30.2) |
| Not employed | 15 (7.0) |
| Disabled | 120 (55.8) |
| Other | 15 (7.0) |
|
| |
| Current Health insurance | |
| Medicare | 74 (34.4) |
| Medicaid | 45 (20.9) |
| SSI | 49 (22.8) |
| VA | 18 (8.4) |
| No insurance | 11 (5.1) |
|
| |
| Perceived financial status to meet basic need | |
| Meets basic need | 92 (42.8) |
| Does not meet basic needs | 123 (57.2) |
|
| |
| Taking depression medication | |
| Yes | 83 (38.6) |
| No | 132 (61.4) |
|
| |
| Having problems taking HIV medication | |
| Yes | 78 (36.3) |
| No | 137 (63.7) |
|
| |
| Using any aids to remember to take medication | |
| Yes | 65 (30.2) |
| No | 150 (69.8) |
Based on the BDI-II, 61 % (n=132) of the participants had minimal to no depressive symptoms. One-third of the participants experienced mild (n=37, 17.2%) or moderate (n=34, 15.8%) depressive symptoms, while less than 10 percent of participants (n=12, 5.6%) had severe depressive symptoms. On average, participants perceived that they had good social support (M=81.00; SD=22.22). Participants reported high medication-taking self-efficacy (M=138.80; SD=28.03) and moderate self-reported medication adherence (M=0.64; SD=0.48). Persons who perceived higher social support had fewer depressive symptoms. Perceived social support showed a significant positive relationship with medication-taking self-efficacy, but no significant relationship with self-reported medication adherence. The participants with fewer depressive symptoms showed a higher medication-taking self-efficacy to take antiretroviral therapy and greater self-reported medication adherence. Higher medication-taking self-efficacy was significantly associated with higher self-reported medication adherence in this study (see Table 2).
Table 2.
Descriptive statistics and correlations among the variables in the study
| Variables | 1. Social support | 2. Depressive symptoms | 3. Mediation-taking Self-efficacy beliefs | 4. Self-report medication adherence |
|---|---|---|---|---|
| 1 | - | −0.48* | 0.37* | 0.09 |
| 2 | - | −0.42* | −0.23* | |
| 3 | - | 0.44* | ||
|
| ||||
| Mean | 81.00 | 12.90 | 138.80 | 0.64 |
| SD | 22.22 | 9.59 | 28.03 | 0.48 |
|
| ||||
| Possible range | 0 – 120 | 0 – 63 | 17 – 170 | 0 –1 |
| Observed range | 11–118 | 0 – 47.25 | 52 – 170 | 0 –1 |
SD: Standard deviation
p< .001
Test of Mediation Hypotheses
Hypothesis 1: Medication-taking self-efficacy will mediate the negative relationship between depressive symptoms and self-reported medication adherence
The relationship between depressive symptoms and self-reported medication adherence was examined (see Figure 1). Participants with greater depressive symptoms showed a lower self-reported medication adherence (d; β= −0.23, Z= −2.53, p=.011). In addition, participants with greater depressive symptoms had lower medication-taking self-efficacy (b; β= −0.40, Z= −4.83, p<.001). Participants with higher self-efficacy had higher rates of self-reported medication adherence (e; β= 0.44, Z=7.16, p<.001). A significant negative prediction of self-reported medication adherence by depressive symptoms remained after adjusting for medication-taking self-efficacy (d′; β= −0.18); self-efficacy partially mediated the prediction of self-reported medication adherence by depressive symptoms, (the 95% CI of the indirect effect = [−.04, −.01]).
Hypothesis 2: Medication-taking self-efficacy will mediate the positive relationship between perceived social support and self-reported medication adherence
Perceived social support did not predict self-reported medication adherence (f; β= 0.08, Z=1.02, p=.308). Participants perceiving higher social support had higher medication-taking self-efficacy (c; β= 0.36, Z=5.83, p<.001). Participants with higher medication-taking self-efficacy had higher self-reported medication adherence (e; β= 0.50, Z= 8.45, p<.001). An indirect effect between perceived social support and self-reported medication adherence was identified (f′; β = 0.18, the 95% CI of the indirect effect= [.01,.03]). Although there was a significant indirect effect of perceived social support on self-reported mediation adherence, there was no significant direct effect. Therefore, medication self-efficacy did not act as a mediator between perceived social support and self-reported medication adherence as proposed in the hypothesis.
Hypothesis 3: Depressive symptoms will mediate the positive relationship between perceived social support and medication-taking self-efficacy
The mediating role of depressive symptoms between perceived social support and medication-taking self-efficacy was examined. When participants perceived higher perceived social support, they had greater medication-taking self-efficacy (c; β= .37, Z= 3.12, p=.002). Participants who perceived higher perceived social support reported fewer depressive symptoms (a; β= −.43, Z= −6.71, p<.001). Participants reporting fewer depressive symptoms had higher medication-taking self-efficacy (b; β= −.31, Z= −3.48, p<.001). A significant positive prediction of medication-taking self-efficacy by perceived social support remained after adjusting for depressive symptoms; however, there was a significant reduction in the prediction of medication-taking self-efficacy by perceived social support (c′; β = 0.13, the 95% CI of the indirect effect=[0.41,1.87]). Therefore, depressive symptoms partially mediated the prediction of self-efficacy by perceived social support.
Test of a comprehensive model with three hypotheses
The model fitting of a comprehensive model with the three hypotheses was tested. The initial conceptual model of this study shown in Figure 1 is a baseline diagram of the comprehensive model. As hypothesis 2, however, shows perceived social support did not significantly predict self-reported medication adherence (path “f” in Figure 1). Thus, a model which removed path “f” from the initial conceptual model was selected as a baseline model for this study (Model 1). Model 1 did not show good fit in the sample (see Table 3, Model 1). Based on the Wald test results, the second model (Model 2) that deleted a path between depressive symptoms and self-reported medication adherence [“d” in Figure 1] was tested. This model also did not meet the criteria for a “good” model. The LM test suggested adding an error covariance between affective and somatic elements under the construct of depressive symptoms on the Model 2. This model (Model 3) showed a good model fit (S-Bχ2 (24, N=215) = 69.06, p<.001; CFI=0.95; SRMR=0.057; see Table 3). Therefore, Model 3 was chosen as the parsimonious model to explain the mediation effects of depressive symptoms and medication-taking self-efficacy on self-reported medication adherence in PWHIV.
Table 3.
Changes in chi-square and fit indices of the final model that combines three hypotheses
| Model | S-B chi;2 | df | p-value | CFI | SRMR |
|---|---|---|---|---|---|
| Model 1 | 78.30 | 24 | <.001 | .94 | .063 |
| Model 2 | 78.74 | 25 | <.001 | .94 | .063 |
| Model 3 | 69.06 | 24 | <.001 | .95 | .057 |
Model 1: baseline model (deleting a path between perceived social support and self-report medication adherence (f) from the conceptual model)
Model 2: deleting a path between depressive symptoms and adherence (d) from Model 1
Model 3: model 2 added an error covariance between affective and somatic element of the depressive symptoms
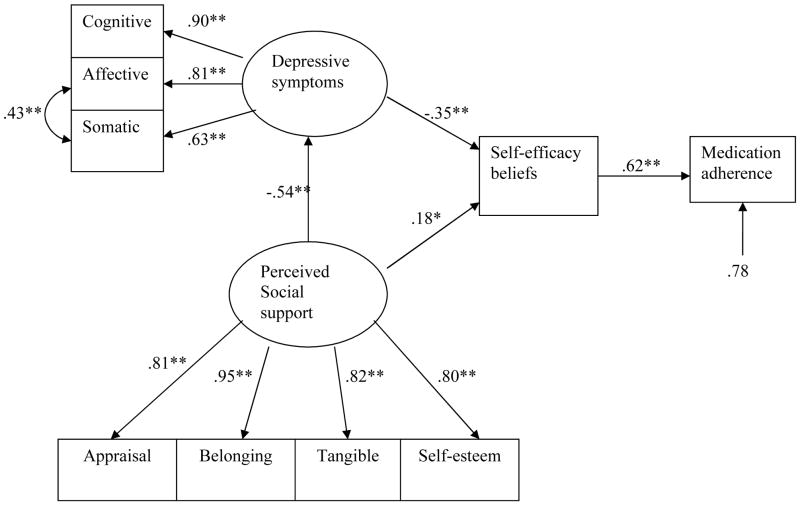
Medication-taking self-efficacy completely mediated the prediction of self-reported medication adherence by perceived social support and depressive symptoms. Depressive symptoms partially mediated the prediction of medication-taking self-efficacy by perceived social support. The cognitive element of depressive symptoms was the most significant factor to predict the medication taking self-efficacy beliefs in this study, although the affective and somatic elements also explained depressive symptoms (see Figure 2). Belonging was the strongest function explaining the person’s perceived social support. The total explained variance of self-reported medication adherence in persons with HIV was 21.4%.
Figure 2. Final model of this study.
* p<.01; **p<.001
4. Discussion
Depressive symptoms and perceived social support have been shown to be significant predictors of medication-taking self-efficacy and/or medication adherence in persons with HIV (Kalichman et al., 2003; Mizuno et al., 2003; Simoni et al., 2006). Growing interest exists regarding ways to include these variables in interventions aimed at improving medication adherence in PWHIV; however, only a few studies have identified a causal mechanism among selected psychosocial variables (Simoni et al., 2006; Simoni et al., 2002; Weaver et al., 2005). Furthermore, most of the existing studies examining the mediation effect of medication-taking self-efficacy in HAART regimen adherence tested a relatively simple model that included only one.
The findings of the current study may provide more insight into the development of the effective interventions because of the increased understanding of the diverse psychological factors affecting the health behavior outcome. Our model supported Simoni’s preliminary model which highlighted the role of social support in interventions to improve HAART regimen adherence (Simoni et al., 2006). Because of the social stigma, persons with HIV are likely to depression, anxiety and stress (Simoni et al., 2006). Adequate social support may help PWHIV overcome these psychological symptoms, and subsequently obtain optimal medication adherence rate.
Hypotheses 1 and 2 focusing on Bandura’s self-efficacy theory were confirmed (Bandura, 1986; Bandura, 2001). Self-efficacy beliefs are important factors when executing a health behavior such as medication adherence. In this study, these beliefs were affected by perceived social support and depressive symptoms as self-efficacy theory suggests. The identified role of self-efficacy beliefs to execute medication adherence, however, was two fold in this study; self-efficacy beliefs acted as a mediator in hypothesis 1, but not in hypothesis 2. Perceived social support indirectly affected medication adherence through self-efficacy in hypothesis 2.
Hypothesis 3, examining the mediating role of depressive symptoms between perceived social support and medication-taking self-efficacy was partially supported. That is, depressive symptoms can be reduced when there are efforts to enhance perceived social support. The belonging function of perceived social support was the strongest predictor; however, the other functions of perceived social support were also significant predictors of perceived social support. A possible intervention is the identification and development of supportive social networks and resources which are easily accessible and available. Supportive social networks which make persons available, who can spend time with participants, discuss their concerns regarding stigma, and engage them in some social activity, may be a good strategy for improving medication adherence in the HIV population. Therefore, understanding clients’ interest and concerns is necessary in order for health care providers to develop interventions that will provide persons with HIV with information about available social support networks and resource in the community. Additionally, the intervention will need to provide information regarding how to access social support networks.
In this study, the strongest predictor of depressive symptoms was the cognitive element. The finding provides a possible rationale for the use of a social support intervention. When a person perceives a supportive social network, cognitive depressive symptoms in an outpatient clinic participant may be decreased (Simoni et al., 2006). According to Schrimshaw (2003), unsupportive social support predicted a high level of non-clinical depressive symptoms, especially for women with HIV infection. Jia and colleagues (2004) found that depressive symptoms were a mediating variable between social support and the perceived quality of life among men with HIV. A correlation between the affective and somatic elements of the BDI was expected as persons frequently experience affective depressive symptoms when they are sick. Strategies to manage negative physiologic reactions and side effects also need to be included in an intervention of HAART regimen adherence.
Despite the important findings from this study, there are limitations suggesting implications for future research. First, the current study only examined the relationship between depressive symptoms and perceived social support in an outpatient clinic population of HIV patients. Although the BDI-II is an appropriate instrument to measure severity of depression in psychiatric patients and to screen potential depression in the general population (Beck et al., 1996), there is insufficient evidence to diagnose clinical depression in a community sample using a reported score. Thus, the following questions remain to be tested in future studies: 1) what is the relationship between depressive symptoms and the presence of a clinical diagnosis of depression, and 2) do different degrees of depressive symptoms support these study findings.
Second, the use of only baseline data in the analysis is a limitation. Although the findings of this study provide researchers with evidence to develop effective interventions for improving HIV-medication adherence through enhancing medication adherence self-efficacy, this study did not examine the intervention effect of self-efficacy beliefs. Future research is needed to examine the intervening effect for enhancing medication self-efficacy beliefs to identify effective strategies for enhancing the self-efficacy beliefs. Replicating this study using the same comprehensive model is needed using longitudinal data.
Third, other variables that might influence mediators or medication adherence need to be examined. Theoretically, physiologic factors can influence self-efficacy and health behavior (Bandura, 2001). In addition, a relationship between somatic variables and depressive symptoms may create a different model. For instance, participants may experience greater depressive symptoms when their physical health is poor. In that case, greater perceived social support may not reduce depressive symptoms and enhance self-efficacy beliefs. Although no previous studies suggested the need to adjust the effect of prescribed medication for psychological disorders, the use of the medications (e.g., drugs to treat depression), may be a moderating variable in the proposed model. A future study needs to examine mediating and moderating roles of depression simultaneously with how the severity of depressive symptoms (e.g, taking medication vs. no medication) affects the proposed model. As Weaver (2005) has suggested, the possible moderating effects of gender, ethnicity and risk factors for HIV also need to be examined in the same model.
Fourth, the reliability of a self-reported instrument to assess medication adherence is a limitation of this study. No gold standard exists to measure medication adherence in PWHIV; studies of HIV-medication adherence frequently use a self-report instrument (Fletcher et al., 2005; Yasuda et al., 2004). Using one self-report item to measure medication adherence may provide insufficient evidence when measuring this concept. The modified Morisky Self-report Medication Taking Scale includes only two items measuring actual behavior of taking medication in relation to a specific time: yesterday and the past two weeks. The tool has 7 additional items measuring general medication adherence habits and behavioral skills without a specific time frame. Thus, initially the two items with a specific time frame were chosen to measure the actual behavior of medication adherence and to create a latent variable. However, the correlation coefficient between the two items of actual behavior (r=.21) was relatively small and did not satisfy the condition for using structural equation modeling as moderate correlations are necessary among observed variables under the same construct (Kline, 1998). Furthermore, the item measuring yesterday’s medication adherence showed low variability; most participants (n=198, 92.1%) reported they took their medication yesterday. Thus, the researchers used the one item that asked about medication taking over the past two weeks to measure self-report medication adherence in the current study. Future studies need to test the proposed model with other adherence measures such as pill counts, pharmacy records, or electronic event monitoring.
Lastly, while we did have data on whether participants were taking medications for depression, we did not examine whether any of the participants had a history of or were currently diagnosed with psychiatric problems. Having this diagnostic information may have been helpful in regard to the scores reported on the BDI-II particularly for those who reported the use of medications for depression. Assessing both history of and current psychiatric health problems and whether subjects were prescribed medications need to be included in future studies in order to determine how they influence current depressive symptoms.
5. Conclusions
Testing for a mediation effect can provide researchers with an understanding of the intervening mechanism. Such research findings can enhance the body of knowledge beyond the examination of direct effects. Further, the accumulated knowledge can be used by researchers to enhance the development of intervention programs.
The findings of this study provide researchers with increased understanding of the mediating role of medication-taking self-efficacy beliefs between selected psychological variables and self-reported medication adherence in PWHIV. Furthermore, this study demonstrated the mediating role of depressive symptoms between perceived social support and medication-taking self-efficacy. These findings may be useful when designing treatment adherence interventions strategies for future research.
Acknowledgments
The authors acknowledge National Institute of Nursing Research at NIH for funding of this study (R01 NR04749 [ PI: J. A. Erlen]).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
EunSeok Cha, Instructor, Chung-Ang University, #506 Department of Nursing School of Medicine, 221 Heukseok dong Dongjakgu, Seoul, 156-756, South Korea.
Judith A. Erlen, Professor and PhD Program Coordinator, University of Pittsburgh School of Nursing, 440 Victoria Building, Pittsburgh PA, 15261, USA.
Kevin H. Kim, Assistant Professor, University of Pittsburgh School of Education, 5918 WWPH Building, Pittsburgh PA, 15260,USA.
Susan M. Sereika, Associate Professor and Director, Statistical Support Services, University of Pittsburgh School of Nursing and Graduate School of Public Health, 360 Victoria Building, Pittsburgh PA, 15261,USA.
Donna Caruthers, Assistant Professor, University of Pittsburgh School of Nursing, 440 Victoria Building, Pittsburgh PA, 15261,USA.
References
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bandura A. Social cognitive theory: An agentic perspective. Annual Review of Psychology. 2001;52:26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA. Beck Depression Inventory Manual. San Antorio, TX: The Psychological Corp; 1987. [Google Scholar]
- Beck AT, Steer RA, Ball R, Ranieri WF. Comparison of Beck depression inventories-IA and -II in Psychiatric outpatients. Journal of Personality Assessment. 1996;67:588–97. doi: 10.1207/s15327752jpa6703_13. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Wu EJC. EQS for Windows User’s Guide. 5. Encino, CA: Multivariate Software, Inc; 2002. [Google Scholar]
- Cha ES, Erlen JA, Kim Y. Psychometric evaluation of the HIV self-efficacy scale (HIV SES) Annals of Behavioral Medicine. 2004;27:S148. [Google Scholar]
- Cohen S, Mermelstein R, Kamarck T, Hoberman HM. Measuring the functional components of social support. In: Sarason IGSBR, editor. Social support: Theory, research, and application. Hague, Holland: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- Ferguson TF, Stewart KE, Funkhouser E, Tolson J, Westfall AO, Saag MS. Patient-perceived barriers to antiretroviral adherence: Association with race. AIDS Care. 2002;14:607–17. doi: 10.1080/0954012021000005434. [DOI] [PubMed] [Google Scholar]
- Fletcher CV, Testa MA, Brundage RC, Chesney MA, Haubrich R, Acosta EP, Martinez A, Jiang H, Gulick RM. Four measures of antiretroviral medication adherence and virologic response in AIDS clinical trials group study 359. Journal of Acquired Immune Deficiency Syndromes. 2005;40:301–06. doi: 10.1097/01.qai.0000180078.53321.6a. [DOI] [PubMed] [Google Scholar]
- Godin G, Cote J, Naccache H, Lambert LD, Trottier S. Prediction of adherence to antiretroviral therapy: a one-year longitudinal study. AIDS Care. 2005;17:493–504. doi: 10.1080/09540120412331291715. [DOI] [PubMed] [Google Scholar]
- Hsu LC, Vittinghoff E, Katz MH, Schwarcz SK. Predictors of use of highly active antiretroviral therapy (HAART) among persons with AIDS in San Francisco, 1996–1999. Journal of Acquired Immune Deficiency Syndromes. 2001;28:345–50. doi: 10.1097/00126334-200112010-00007. [DOI] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jia H, Uphold CR, Wu S, Reid K, Findley K, Duncan PW. Health-related quality of life among men with HIV infection: effects of social support, coping, and depression. AIDS Patient Care STDs. 2004;18:594–603. doi: 10.1089/apc.2004.18.594. [DOI] [PubMed] [Google Scholar]
- Johnson ME, Neal DB, Brems C, Fisher DG. Depression as measured by the Beck Depression Inventory-II among injecting drug users. Assessment. 2006;13:168–77. doi: 10.1177/1073191106286951. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. Journal of Behavioral Medicine. 2003;26:315–32. doi: 10.1023/a:1024252926930. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Sikkema KJ, Somlai A. Assessing persons with human immunodeficiency virus (HIV) infection using the Beck depression inventory: Disease processes and other potential confounds. Journal of Personality Assessment. 1995;64:86–100. doi: 10.1207/s15327752jpa6401_5. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: Guilford Press; 1998. [Google Scholar]
- Lewis SJ, Abell N. Development and evaluation of the adherence attitude inventory. Research on Social Work Practice. 2002;12:107–23. [Google Scholar]
- Malcolm SE, NG JJ, Rosen RK, Stone VE. An examination of HIV/AIDS patients who have excellent adherence to HAART. AIDS Care. 2003;15:251–61. doi: 10.1080/0954012031000068399. [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Dawson-Rose C, Parsons JT, SUDIS Team. Correlates of depressive symptoms among HIV-positive injection drug users: the role of social support. AIDS Care. 2003;15:689–98. doi: 10.1080/09540120310001595177. [DOI] [PubMed] [Google Scholar]
- Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Medical Care. 1986;24:67–74. doi: 10.1097/00005650-198601000-00007. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Johnson-Roberts K, Hoffmann D, Molina A, Lu MC. Barriers and successful strategies to antiretroviral adherence among HIV-infected monolingual Spanish-speaking patients. AIDS Care. 2003;15:217–30. doi: 10.1080/0954012031000068362. [DOI] [PubMed] [Google Scholar]
- Power C, Selnes OA, Grim JA, McArthur JC. HIV Dementia Scale: a rapid screening test. Journal of Acquired Immune Deficiency Syndromes and Human Retrovirology. 1995;8:273–78. doi: 10.1097/00042560-199503010-00008. [DOI] [PubMed] [Google Scholar]
- Power R, Koopman C, Volk J, Israelski DM, Stone L, Chesney MA, Spiegel D. Social support, substance use, and denial in relationship to antiretroviral treatment adherence among HIV-infected persons. AIDS and Patient Care & STDs. 2003;17:245–52. doi: 10.1089/108729103321655890. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, and Computers. 2004;36:717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Read T, Mijch A, Fairley CK. Adherence to antiretroviral therapy: are we doing enough? Intern Med J. 2003;33:254–56. doi: 10.1046/j.1445-5994.2003.00333.x. [DOI] [PubMed] [Google Scholar]
- Schrimshaw EW. Relationship-specific unsupportive social interactions and depressive symptoms among women living with HIV/AIDS: Direct and moderating effects. Journal of Behavioral Medicine. 2003;26:297–313. doi: 10.1023/a:1024200910092. [DOI] [PubMed] [Google Scholar]
- Shrout PE, Bolger N. Mediataion in experimental and nonexperimental studies: New procedures and recommendations. Psychological Methods. 2002;7:422–45. [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Huang B. A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychology. 2006;25:74–81. doi: 10.1037/0278-6133.25.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Lockhart D, Liebovitz D. Mediators of social support and antiretroviral adherence among an indigent population in New York City. AIDS Patient Care and STDs. 2002;16:431–39. doi: 10.1089/108729102760330272. [DOI] [PubMed] [Google Scholar]
- van Servellen G, Lombardi E. Supportive relationships and medication adherence in HIV-infected, low-income Latinos. Western Journal of Nursing Research. 2005;27:1023–39. doi: 10.1177/0193945905279446. [DOI] [PubMed] [Google Scholar]
- Weaver KE, Llabre MM, Duran RE, Antoni MH, Ironson G, Penedo FJ, Schneiderman N. A Stress and Coping Model of Medication Adherence and Viral Load in HIV-Positive Men and Women on Highly Active Antiretroviral Therapy (HAART) Health Psychology. 2005;24:385–92. doi: 10.1037/0278-6133.24.4.385. [DOI] [PubMed] [Google Scholar]
- Yasuda JM, Miller C, Currier JS, Forthal DN, Kemper CA, Beall GN, Tilles JG, Capparelli EV, McCutchan JA, Haubrich RH California Collaborative Treatment G. The correlation between plasma concentrations of protease inhibitors, medication adherence and virological outcome in HIV-infected patients. Antiviral Therapy. 2004;9:753–61. [PubMed] [Google Scholar]