Abstract
Background and aims. To introduce a special dissection technique named “Curettage and Aspiration Dissection Technique” (CADT) using a versatile instrument called Peng's Multifunction Operative Dissector (PMOD) for liver resection. PMOD is an electrosurgical pencil with an inline suction, bearing four functions: electric cutting, coagulation, aspiration and dissection, The above-mentioned functions can be achieved simultaneously or sequentially during liver resection. The purpose of this study was to evaluate this technique and the special electrosurgical device in hepatic surgery. Patients and methods. From June 2005 to December 2006, 70 consecutive patients with segmentectomy or major hepatectomy were performed with this dissection technique by the same surgeon. Peri-operative data and the technical aspect of this device and dissection technique for various types of liver resection were summarised. Results. Forty-nine of 70 cases with various degrees of cirrhosis. Median blood loss were 470 ml (100–2400 ml), the bleeding and mortality within one month postoperatively was zero. There were postoperative complications in 20 patients: bile leak occurred in five cases, nine cases with right pleural effusion and six with ascites. No relative complications with this method were found. Conclusion. The CADT and PMOD can achieve better dissection and hemostasis. It possible is a much more valuable alternative to other devices currently used for liver surgery.
Keywords: liver resection, PMOD, curettage and aspiration dissection technique, Peng's multifunction operative dissector
Introduction
Prolonged operating time and massive intraoperative hemorrhage are associated with higher mortality and morbidity in liver resection. But it seems to be a conflict between operative time and precise surgical anatomy. Decrease of hemorrhage and shorter operating time are related to high level of training, skill and improvement of surgical instrument. Classical surgical procedure such as cutting, coagulation, dissection and suction must be executed separately by operator and assistant. To reduce time on these procedure would be of great help for the operation.
For liver parenchyma transection, a variety of special instruments has been designed and used clinically such as cavitron ultrasonic surgical aspirator (CUSA), water-jet, ultrasonic scalpel, argon beam coagulation (ABC), etc for achieving above-mentioned objectives 1. Each of them has merits and demerits. For example, CUSA has the function of dissection but no coagulation function; these also apply to water-jet. In addition, the speed of parenchymal dissection is very slowly with CUSA, especially so when the liver is cirrhotic. Ultrasonic scalpel can be used to separate tissue and coagulate vessels, yet it doesn't have the function of isolating the vessels or ducts which should be preserved. ABC without the function of dissection and only be used for stopping bleeding on the raw surface 2,3.
In 1990, one of the authors (Penga SY) developed a versatile electrosurgical instrument called Peng's Multifunction Operative Dissector (PMOD, Hangzhou Shuyou Medical Instrument Co, Hangzhou, Zhejiang, PR China, FDA 510(K) Number K040780) for liver parenchymal transection. PMOD is used to scrape (curettage) on the liver incision line. Debris and oozing blood, if any, are sucked away synchronously, so as to expose the vessels and bile ducts in the parenchyma. The PMOD combine together four functions: suck, electro-coagulate, cut and dissect, and eliminates the necessity to change frequently surgical instruments, reducing the operating times and bleeding, improving the quality of surgery 4. Therefore this dissection technique is named “Curettage and Aspiration Dissection Technique” (CADT). Excellent results have been demonstrated with this technique in liver surgery. The aim of this study is to introduce the characteristics of this technique and how to perform in liver surgery.
Patients and methods
Patients
From June 2005 to December 2006, 70 consecutive patients with segmentectomy or major hepatectomy were performed with this dissection technique by the same surgeon. The terminology for liver anatomy and resections used in this report is the Brisbane 2000 terminology of the International Hepato-Pancreato-Biliary Association 5.
The ages ranged from 11–77 years (mean 53.8 years) in 51 male and 19 female patients, According to the type of resection, these patients were divided into three groups. The patients undergoing single segmentectomy from segment I to segment VIII are less in 20 cases; bisegmentectomy were performed in 17 cases; A variety of hemihepatectomy in 33 cases, including left hemihepatectomy in nine patients, right hemihepatectomy in 13 patients, right trisegmentectomy in three cases, and the other eight cases were performed non-anatomical resection. Inflow occlusion (Pringle's manoeuvre) was routinely used.
Peng's Multifunction Operative Dissector (PMOD) and Curretage and Aspiration Dissection Technique (CADT)
PMOD looks like an electrosurgical-pencil, but its structures are different. The main difference is that a metal pipe is passing through the pencil, while the body of the pipe is coated with insulated material and the tip of the pipe is made oblique forming a bevel end Figure 1A B. A removable blade is attached to the tip of the tube for electric cutting. This special design makes PMOD have the four different functions.
Figure 1. .
(A) The main body of PMOD is composed of dissection tip and metallic suction pipe which is coated with insulated material. Curettage, aspiration, electro-coagulation and dissection function can be performed simultaneously or in sequence. (B) The overall structure of PMOD, The pipe is connected to a vacuum apparatus through a tube. PMOD also has an electric wire to connect with a common electrosurgical generator.
The pipe is connected to a vacuum apparatus through a tube. PMOD also has an electric wire to connect with a common electrosurgical generator.
Both of the aspiration tube and wire are anchored on the operating tube by the right side of surgeon with a length of 60–80cm free, so the surgeon can manipulate PMOD conveniently.
By using the same way as holding a pen to hold the PMOD in hand.
By using thumb or index finger to control the button “on” or “off”, thetissue can be dissected with bevel edge of the tip, during curetting and dissecting, the tip is not electrified. Blood, fluid and oddment in the operative field can be aspirated continually to make the operating field clear and clean.
CADT is a manoeuvre that is composed of four principal surgical actions: curettage, aspiration, electro-coagulation and dissection by using PMOD, PMOD allows the operator to perform all operative manipulations including cutting, haemostasis, suction and dissections. These manipulations can be performed simultaneously or in sequence.
Liver resection
Intermittent inflow occlusion was routinely used, the time limit was 10 min each time with 2 min reperfusion. Total vascular exclusion was seldom necessary except when the tumor is closely adherent to the IVC or major hepatic veins. In some cases, the major hepatic vein right hepatic vein and/or common trunk of middle and left hepatic veins were dissected and pre-looped with tape to substitute IVC control 6.
The power setting of electrosurgical generator varies according to the tissue to be dissected or transected. For dissection and division of hepatic ligament, 40–60 HZ would be enough. For transection of liver parenchyma, the maximum power of 120 HZ can be used. Usually dissection is carried out along the transection plane, but when large vessels are encountered, curettage was proceeded in parenchyma paralleled along the vessel in deep cleavage plane by altering direction, to expose a short segment of the vessel in an effort to avoid injury so that the important vessels can be safely preserved with this technique and sudden, massive hemorrhage occurred rarely (Figure 2). Hepatic vein tributaries up to 3 mm in diameter can be coagulated, but the Glissonian tributaries should be ligated when the diameter is over 1 mm. Tension should be kept on both side of the tissue to be dissected to facilitate the transection process. Two PMODs can also be used at the same time separately by the operator and assistant to expedite the process of dissection and homeostasis.
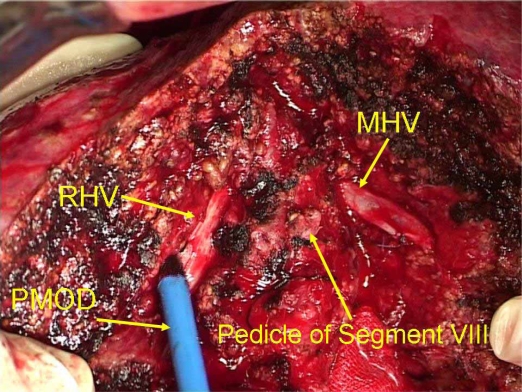
Figure 2. .
After the tumor of segment VIII was anatomical resected completely, the main trunk of right hepatic vein (RHV), the middle hepatic vein (MHV) and the hepatic pedicle of segment VIII were exposed on cut surface. These important vessels can be dissected clearly and safely with the use of PMOD.
After resection, the cut surface of liver was generally electro-coagulated with PMOD, bile leaks was examined and treated when identified. Drains were routinely placed and removed within one week unless bile leak occurred.
Results
The most common indications for resection were hepatocellular carcinoma in 55 cases and metastatic colorectal cancer in five cases, gallbladder carcinoma in two cases, hilar cholangiocarcinoma in three cases, hemangioma in five cases. In 49 of the 70 cases the livers were cirrhotic.
Median blood loss were 470 ml (100–2400 ml), The bleeding and mortality within one month postoperatively was zero. There were postoperative complications in 20 patients: bile leak occurred in five cases, nine cases with right pleural effusion and six with ascites.
Discussion
Intraoperative blood loss remains a major concern for liver resection because it is associated with a high rate of postoperative complications and survival. Over the years different technique have been developed to allow safer liver resection, liver parenchyma division can be performed with the scalpel, crushing the tissue with the finger or clamps, vibrating with ultrasonic dissectors, hydro-jet dissectors or stapling devices. These instruments have different function and effect during hepatectomy respectively, ultrasonic dissectors can dissect the vessel of parenchyma but no function of cutting and coagulation. In China, over 80% hepatocellular carcinoma (HCC) occurs in cirrhotic liver, a condition to impede the speed of liver transection using CUSA. Hepatic vein and portal vein is easy injured accidentally with finger fracture or clamping, particularly for the surgeons who are not familiar with the anatomy of the liver. In addition, surgeons have to change instrument frequently when using the above-mentioned instruments. In the early period of our practice we used to apply finger fracture, forceps crush and CUSA for liver transection, the results were unsatisfactory in cirrhosis patients. As a result we designed a versatile instrument PMOD, with which operations can be carried out without changing instruments frequently because PMOD can be used for dissecting, cutting, coagulating and aspirating, almost every basic operating element except suturing. The most outstanding feature is that all the vessels and ducts can be clearly dissected and exposed during transection of liver parenchyma. Therefore safety of operation is much enhanced. In 1994, we undertook a control trial to compare liver transection methods: Using CADT technique with PMOD versus using forceps crush technique. The results showed that the amount of blood loss with CADT was only half of that with forceps crush, the time for liver transection with CADT was 40% shorter than with the latter 7. With respect to stop bleeding, PMOD is much more effective than regular electrosurgical pencil due to the fact that bleeding point can be clearer seen and can be dried for the electro-coagulation to act owing to the suction function built-in. During transection, bleeders from small intrahepatic vessels can easily be sucked and coagulated by the operator himself.
For an ideal and safe liver transection, we proposed to observe the principle of three “I”, which is short for Identification, Isolation, Individually dealing with, 3 “I” principle means important intrahepatic vessels are identified first, then isolated for a short segment before dealt with individually, either preserved or cut and ligated. As a matter of fact, 3 “I” principle can be applied to a great variety of operations. Most of the time during operation, a surgeon would have to deal with different kinds of vessels or ducts. CADT would be of great help in this regard.
With “Curetage and Aspiration Dissection Technique”, the operative time, anesthesia time and amount of hemorrhage have been reduced significantly, and liver resection becomes a less risky surgical procedure. Particularly for difficult hepatectomies such as tumors that are very close to major hepatic veins or inferior vena cava, Moreover, transection of liver parenchyma using PMOD were quite rapid.
Recently, two new devices have been introduced for liver resection. These include a computer controlled bipolar vessel device marketed as Ligasure and a saline-linked radio frequency ablation device marketed as the 3.0 dissector-sealer Tissuelink, Ligasure can sealed the vessels and bile ducts effectively in normal parenchyma, but the device was much less effective on pathological vessels, such as those around cysts 8. Tissuelink can be used for ablation of the cut surface of the liver so that it has the capacity to extend resection margins as “precoagulation” device. However, veins and arteries can be injured and it is inadvisable to isolate veins and arteries with Tissuelink 9. With PMOD, when veins and arteries were encountered or tumor closed to the important vessels, liver parenchyma can be pushed parallelly along the vessel with the cautary tip without electrified. We have performed 168 cases of caudate lobe including isolated complete caudate lobectomy with this technique safely 10,11. During liver transection, the task of one assistant is holding a sucker to keep the operating field clear and clean while the operator is using CUSA or Ligasure. However, in the situation of using PMOD the surgeon can do the suction himself sparing the assistant to do other more important manipulations rather than simply holding suction.
In addition, this technique is also developed for laparoscopic hepatectomy and the results are good 12,13,14.
Conclusions
CADT using PMOD is a very useful technique for transection of liver parenchyma, not only operating time is shortened, the amount of bleeding is reduced resulting in enhancement of safety but also difficult operations become easy to perform. Moreover, PMOD looks simple but functionally is versatile and it is not expensive at all as it can fit in any kind of generator. Therefore it can be used in all kinds of operating room and hospital.
Acknowledgements and disclosures
This work was funded by grants from Zhejiang Province Natural Science Fund. China (Fund Number: 0306GJHZ).
References
- 1.Allen PJ, Jarnagin WR. Current status of hepatic resection. Adv Surg 2003;37:29–9. [PubMed] [Google Scholar]
- 2.Rau HG, Schardey HM, Buttler E, Reuter C, Cohnert TU, Schildberg FW. A comparison of different techniques for liver resection: blunt dissection, ultrasonic aspirator and jet-cutter. Eur J Surg Oncol. 1995;21:183–7. doi: 10.1016/s0748-7983(95)90435-2. [DOI] [PubMed] [Google Scholar]
- 3.Wolf RF, Xie H, Petty J, Teach JS, Prahl SA. Argon ion beam hemostasis with albumin after liver resection. Am J Surg. 2002;183:584–7. doi: 10.1016/s0002-9610(02)00844-9. [DOI] [PubMed] [Google Scholar]
- 4.Di Carlo I.Peng's Multifunctional Operational Dissector (PMOD) in Chirurgia Epatica, Edizioni Minerva Medica, 2007;34–5. [Google Scholar]
- 5.International Hepato-Pancreato-Biliary Association. Brisbane 2000 terminology of liver anatomy and resections. HPB 2000;2:333–9. [Google Scholar]
- 6.Peng SY, Li JT, Du JJ, Liu YB, Wang XB, Wang JW, Xu B, Li HJ, Fang HQ. The role and significance of looping round the major hepatic vein in difficult hepatectomies (in Chinese) Chin J Gen Surg. 2003;18:444–5. [Google Scholar]
- 7.Peng SY, Jiang XC, Li JD, Cai XJ, Peng CH, Mou YP, Su Y, Fan MM. Liver transection by Curettage and Aspiration – A new technique for hepatectomy (in Chinese) J Basic Clin Gen Surg. 1995;2:11–3. [Google Scholar]
- 8.Sakamoto Y, Yamamoto J, Kokudo N, Seki M, Kosuge T, Yamaguchi T, et al. Bloodless liver resection using the monopolar floating ball plus ligasure diathermy: preliminary results of 16 liver resections. World J Surg. 2004;28:166–72. doi: 10.1007/s00268-003-7167-5. [DOI] [PubMed] [Google Scholar]
- 9.Topp SA, McClurken M, Lipson D, Upadhya GA, Ritter JH, Linehan D, Strasberg SM. Saline-linked surface radiofrequency ablation: factors affecting steam popping and depth of injury in the pig liver. Ann Surg. 2004;239:518–27. doi: 10.1097/01.sla.0000118927.83650.a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Peng SY, Li JT, Mou YP, Liu YB, Wu YL, Fang HQ, Cao LP, Chen L, Cai XJ, Peng CH. Different approaches to caudate lobectomy with “curettage and aspiration” technique using a special instrument PMOD: a report of 76 cases. World J Gastroenterol. 2003;9:2169–73. doi: 10.3748/wjg.v9.i10.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Peng SY, Li JT, Liu YB, Cai XJ, Mou YP, Feng XD, Wang JW, Xu B, Qian HR, Hong de F, Wang XB, Fang HQ, Cao LP, Chen L, Peng CH, Liu FB, Xue JF. Surgical treatment of hepatocellular carcinoma originating from caudate lobe – A report of 39 cases. J Gastrointest Surg. 2006;10(3):371–8. doi: 10.1016/j.gassur.2005.09.026. [DOI] [PubMed] [Google Scholar]
- 12.Cai XJ, Liang L, Wang YF, Yu H, Zheng XY, Huang DY, Peng SY. Laparoscopic hepatectomy by curettage and aspiration: a new technique. Chinese Med J. 2007;120(20):1773–6. [PubMed] [Google Scholar]
- 13.Cai XJ, Yu H, Liang X, Wang YF, Zheng XY, Huang DY, Peng SY. Laparoscopic hepatectomy by curettage and aspiration-experiences of 62 cases. Surg Endosc Intervent Tech. 2006;20(10):1531–5. doi: 10.1007/s00464-005-0765-6. [DOI] [PubMed] [Google Scholar]
- 14.Ji ZL, Peng SY, Cai XJ. A laparoscopic multifunctional operative device in laparoscopic hepatectomy. Chirurgische Gastroenterologie. 2004;20(4):308–12. [Google Scholar]