Abstract
OBJECTIVE—Wolfram syndrome is an autosomal recessive neurodegenerative disorder characterized by diabetes insipidus, diabetes (nonautoimmune), optic atrophy, and deafness (a set of conditions referred to as DIDMOAD). The WFS1 gene is located on the short arm of chromosome 4. Wolfram syndrome prevalence is 1 in 770,000 live births, with a 1 in 354 carrier frequency.
RESEARCH DESIGN AND METHODS—We evaluated six Italian children from five unrelated families. Genetic analysis for Wolfram syndrome was performed by PCR amplification and direct sequencing.
RESULTS—Mutation screening revealed five distinct variants, one novel mutation (c.1346C>T; p.T449I) and four previously described, all located in exon 8.
CONCLUSIONS—Phenotype-genotype correlation is difficult, and the same mutation gives very different phenotypes. Severely inactivating mutations result in a more severe phenotype than mildly inactivating ones. Clinical follow-up showed the progressive syndrome's seriousness.
Wolfram syndrome includes nonautoimmune diabetes and optic atrophy within the first decade followed by diabetes insipidus and deafness (1). Additional characteristics are ureterohydronephrosis, neuropsychiatric and endocrinological impairment, and, seldomly, powdered cataract and retinopathy (2). Mortality is ∼65% before age 35 years, due to central respiratory and renal failure (1). The gene involved (WFS1) was identified in 1998 on chromosome 4p (3). WFS1 spans 33.4 kb of genomic DNA and includes eight exons: the first is noncoding, 2–7 are coding, and the 8th is 2.6 kb long (3). WFS1 mRNA encodes an 890–amino acid polypeptide with nine putative transmembrane domains and a 100-kd molecular mass. WFS1 mRNA is expressed in heart, brain, placenta, lung, and pancreas; WFS1 transcripts were detected in liver, skeletal muscle, and kidney. Wolframin protein is an endoglycosidase H-sensitive membrane glycoprotein that localizes in the endoplasmic reticulum. In the endoplasmic reticulum, it regulates membrane trafficking and protein processing and has a crucial role in β-cell death through the apoptotic pathway (4).
RESEARCH DESIGN AND METHODS
We evaluated six Italian patients (two male and four female) with Wolfram syndrome from five different families. We performed brain nuclear magnetic resonance (to assess posterior pituitary and brain structures) (5), endocrinologic evaluation, ultrasonography, and intravenous urography (to detect renal abnormalities) (6).
Genomic DNA for WFS1 gene mutation screening was obtained after written informed consent. The WFS1 gene coding region was analyzed by PCR amplification and direct sequencing using primers and methods previously described (7). Sequences were compared with human genomic and cDNA WSF1 sequences (GenBank accession no. AF084481), and changes in the nucleotides were checked against published polymorphisms and mutations. Each sequence alteration was confirmed by sequencing both DNA strands of two independent PCR products.
RESULTS
Mutation screening revealed a total of five distinct variants, including one novel mutation (c.1346C>T; p.T449I) and four previously described variants (c.1230_1233delCTCT, c.1362_1377del16, c.1328G>T, and IVS6 + 16G>A). Two patients (case 1, a male patient with a compound heterozygous mutation [S443I] + [IVS6 + 16G>A], and case 2, a female patient carrying a homozygous mutation c.1362_1377del16) have already been the subjects of publication by our group (8). All the mutations were in exon 8.
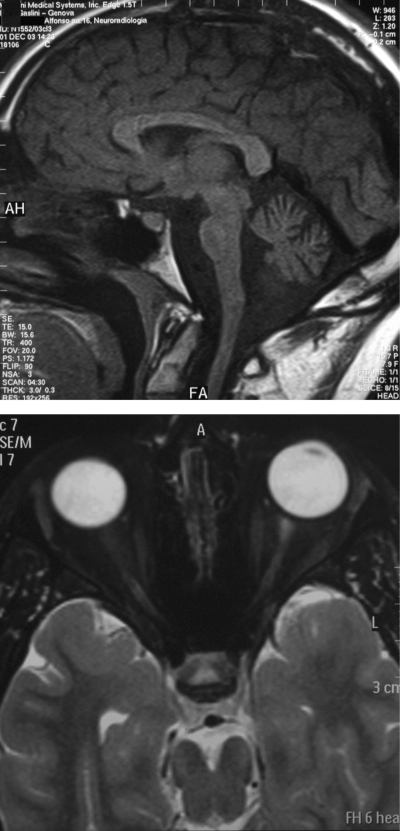
Case 3, a male patient with homozygous mutation at the nucleotide c.1362_1377del16, showed the most severe phenotype, and at age 11 years he experienced acute respiratory failure. Brain nuclear magnetic resonance revealed brain stem, cerebellum, medulla, and pons atrophy (Fig. 1A) and reduced high-signal intensity from the posterior pituitary and optic nerve (Fig. 1B). Urinary tract infections were followed by kidney insufficiency. Renal scintigraphy showed left-obstructive hydronephrosis at the pyelo-uretheral junction. Urodynamic study showed high bladder pressure and confirmed hydronephrosis. Atonic bladder with emptying problems was followed by radical cystectomy with ileal duct when the subject was 19 years old. Interestingly, the other patient carrying the same mutation did not show any respiratory involvement up to now. Her main clinical complication was less severe kidney insufficiency, and she did not otherwise require surgery. The other described male patient ([S443I] + [IVS6 + 16G>A]) showed a less severe phenotype characterized only by diabetes and optic atrophy and without diabetes insipidus or kidney damage. The female patient homozygous for mutation c.1230_1233delCTCT leading to V412fsX440, case 4, showed all the clinical features of the syndrome.
Figure 1.
Brain magnetic resonance of case 3. Upper panel: brain stem atrophy. Lower panel: optic nerve atrophy.
In family no. 5, a new mutation, c1346C>T (ACC>ATC codon change), leading to pT449I amino acid change, was detected; it was heterozygous in consanguineous parents. Cases 5 and 6 were sisters (mutation c.1346C>T; p.T449I), but they still possessed a different phenotype: the older had urethral involvement and severe anorexia; the younger had microalbuminuria but no neurological or urinary tract involvement.
CONCLUSIONS
Severe respiratory complications (the “severe phenotype”) (9) were observed in one boy. A severe respiratory involvement led to the diagnosis of Wolfram syndrome in an adult patient (10). Neurological dysfunctions are responsible for apneic and hypopneic spells during sleep.
Urinary tract involvement including hydrourether, detrursor-sphincter dyssynergia, and detrursor overactivity occurs in up to 90% of patients in adolescence or adulthood and might be due to neuronal degeneration (6). No correlation has been found between the bladder dysfunction and presence or duration of other manifestations, suggesting that bladder dysfunction may be a primary rather than a secondary manifestation of the syndrome (6).
Mutational studies in patients with Wolfram syndrome reported a wide spectrum of mutations distributed throughout the coding sequence of the WFS1 gene. WFS1 protein in vivo is organized as a tetramer that originates a membrane Ca2+ channel of the endoplasmic reticulum, and lack of function of WFS1 determines apoptotic input signaling (11). In spite of the great improvements in the study of the physiological role of WFS1, it is still difficult to establish a phenotype-genotype correlation (9). WFS1 expression was detected in both pancreatic β-cells and the limbic system of mice. Moreover, using immunohistochemical methods, strong WFS1 expression was found in the hippocampus and cerebellum of mice. Using a specific rat insulinoma cell line and fractionated mouse brain tissue, wolframin localization into the endoplasmic reticulum was confirmed.
The only predicting information that genetic analysis can give regards the difference between severely inactivating (such as premature stop codon from insertion or deletion) and mildly inactivating mutations (such as missense mutations). Patients homozygous for a missense mutation seem to have a better prognosis than patients carrying a severely inactivating mutation. Even in our study, although clinical symptoms are different, patients showing more severe features had a severely inactivating mutation (9).
All the mutations described are located in exon 8, corresponding to the transmembrane region and carboxy tail of wolframin protein (9). This is in agreement with other studies in Italian and worldwide populations. Phenotype-genotype correlation is difficult: the same mutation gives different phenotypes in both related and unrelated subjects. Severely inactivating mutations seem to give a more severe phenotype than mildly inactivating mutations.
Published ahead of print at http://care.diabetesjournals.org on 19 June 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Barrett TG, Bundey SE, Macleod AF: Neurodegeneration and diabetes: UK nationwide study of Wolfram (DIDMOAD) syndrome. Lancet 346:1458–1463, 1995 [DOI] [PubMed] [Google Scholar]
- 2.Medlej R, Wasson J, Baz P, Azar S, Salti I, Loiselet J, Permutt A, Halaby G: Diabetes mellitus and optic atrophy: a study of Wolfram syndrome in the Lebanese population. J Clin Endocrinol Metab 89:1656–1661, 2004 [DOI] [PubMed] [Google Scholar]
- 3.Inoue H, Tanizawa Y, Wasson J, Behn P, Kalidas K, Bernal-Mizrachi E, Mueckler M, Marshall H, Donis-Keller H, Crock P, Rogers D, Mikuni M, Kumashiro H, Higashi K, Sobue G, Oka Y, Permutt MA: A gene encoding a transmembrane protein in mutated patients with diabetes mellitus and optic atrophy (Wolfram syndrome). Nat Genet 20:143–148, 1998 [DOI] [PubMed] [Google Scholar]
- 4.Riggs AC, Bernal-Mizrachi E, Ohsugi M, Wasson J, Fatrai S, Welling C, Murray J, Schmidt RE, Herrera PL, Permutt MA: Mice conditionally lacking the Wolfram gene in pancreatic islet beta cells exhibit diabetes as a result of enhanced endoplasmic reticulum stress and apoptosis. Diabetologia 48:2313–2321, 2005 [DOI] [PubMed] [Google Scholar]
- 5.Pakdemirli E, Karabulut N, Bir LS, Sermez Y: Cranial magnetic resonance imaging of Wolfram (DIDMOAD) syndrome. Australas Radiol 49:189–191, 2005 [DOI] [PubMed] [Google Scholar]
- 6.Piccoli GB, Mezza E, Jeantet A, Segoloni JP: An uncommon genetic syndrome with acute renal failure in a 30-year-old diabetic patient. Nephrol Dial Transplant 18:206–208, 2003 [DOI] [PubMed] [Google Scholar]
- 7.Colosimo A, Guida V, Rigoli L, Di Bella C, De Luca A, Briuglia S, Stuppia L, Salpietro DC, Dallapiccola B: Molecular detection of novel WFS1 mutations in patients with Wolfram syndrome by a DHPLC-based assay. Hum Mutat 21:622–629, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Tessa A, Carbone I, Matteoli MC, Bruno C, Patrono C, Patera IP, De Luca F, Lorini R, Santorelli FM: Identification of Novel WFS1 Mutations in Italian Children With Wolfram Syndrome. Hum Mutat 7:348–349, 2001 [DOI] [PubMed] [Google Scholar]
- 9.Smith CJ, Crock PA, King BR, Meldrum CJ, Scott RJ: Phenotype-genotype correlations in a series of Wolfram syndrome families. Diabetes Care 27:2003–2009, 2004 [DOI] [PubMed] [Google Scholar]
- 10.Fabbri LP, Nucera M, Grippo A, Menicucci A, De Feo ML, Becchi C, Al Malyan M: Wolfram syndrome: how much could knowledge challenge the fate? A case report. Med Sci Monit 11:CS40–CS44, 2005 [PubMed] [Google Scholar]
- 11.Philbrook C, Fritz E, Weiher H: Expressional and functional studies of Wolframin, the gene function deficient in Wolfram syndrome, in mice and patient cells. Exper Gerontol 40:671–678, 2005 [DOI] [PubMed] [Google Scholar]