Abstract
OBJECTIVE—The purpose of this study was to test the hypothesis that changing utilization of lipid-lowering, antihypertensive, and oral hypoglycemic drugs may be associated with trends in all-cause mortality in men and women with type 2 diabetes.
RESEARCH DESIGN AND METHODS—This was a cohort study in 197 general practices in the U.K. General Practice Research Database including 48,579 subjects with type 2 diabetes first diagnosed between 1996 and 2006. Measures included all-cause mortality and prescription of hypoglycemic, lipid-lowering, and antihypertensive drugs.
RESULTS—From 1996 to 2006, incidence of type 2 diabetes increased and the mean age at diagnosis declined in women. Prescription of statins within 12 months of diagnosis increased (1996, women 4.9%, men 5.1%; 2005, women 63.5%, men 71.0%), as did drugs acting on the renin-angiotensin system (1996, women 19.4%, men 21.5%; 2005, women 45.5%, men 54.6%) and metformin (1996, women 19.1%, men 15.8%; 2005, women 45.5%, men 42.8%), whereas prescription of sulfonylureas declined. All-cause mortality in the first 24 months after diabetes diagnosis declined in men from 47.9 per 1,000 person-years for subjects with diabetes diagnosed in 1996 to 25.2 for subjects with diabetes diagnosed in 2006 and in women from 37.4 in 1996 to 27.6 in 2006. In a multiple regression model adjusting for age and comorbidity, prescription of statins before or after diagnosis, renin-angiotensin system drugs before or after diagnosis, and metformin after diagnosis were associated with lower mortality.
CONCLUSIONS—Widespread implementation of more effective prescribing to control lipids, blood glucose, and blood pressure may have contributed to recent declines in early mortality in men and women with type 2 diabetes.
The epidemiology of type 2 diabetes is changing. The prevalence of diagnosed diabetes has increased rapidly in national health survey data from a number of countries including the U.S. and the U.K. (1,2). Epidemiological studies also showed that the incidence of type 2 diabetes is increasing (3). This increasing frequency of type 2 diabetes has been associated with increased occurrence of diabetes at younger ages, with some studies suggesting a decline in the mean age at diagnosis of diabetes in the U.S. (4).
At the same time, evidence has accumulated for the potential effectiveness of cholesterol-lowering therapy with statin drugs (5,6) and antihypertensive therapy (7), especially with drugs acting on the renin-angiotensin system (RAS) (8), for reducing cardiovascular events and mortality in type 2 diabetes. When good blood glucose control is achieved, oral hypoglycemic therapy reduces diabetes-related end points (9). Therapy with metformin has been specifically associated with reduced all-cause mortality in diabetes (10). In the UK Prospective Diabetes Study, therapy with sulfonylurea drugs was not associated with increased mortality compared with insulin therapy (9), but several nonrandomized studies have associated sulfonylurea drugs with increased mortality compared with metformin (11,12).
The aim of the present study was to analyze the significance of these developments for the prognosis of patients with newly diagnosed type 2 diabetes. We aimed to evaluate the extent and time course of changes in use of statins, antihypertensive drugs, and oral hypoglycemic drugs among patients with type 2 diabetes and to determine whether changes in drug usage are associated with changes in early mortality in men and women with type 2 diabetes.
RESEARCH DESIGN AND METHODS
We analyzed data from the U.K. General Practice Research Database (GPRD), a large database including electronic patient records for ∼5% of U.K. family practices (13). In the U.K., there is population-based provision of primary care with 98% of the population being registered with a family practice. The quality of GPRD data has been evaluated in several studies (13).
The present longitudinal study included all 197 family practices, with a registered population of ∼1.63 million, that contributed data to GPRD continuously between 1995 and 2006. We selected the population aged ≥30 years because type 1 and type 2 diabetes are less readily distinguished at younger ages. Individuals with prevalent diabetes were identified from the electronic clinical record if they ever had the diagnosis of diabetes or were given a prescription for oral hypoglycemic drugs or insulin. The date of diagnosis was identified as the earlier of the first medical diagnosis for diabetes or the first medical prescription for hypoglycemic drugs, and only subjects with diabetes newly diagnosed between 1 January 1996 and 31 December 2006 were included. Of these, 93.6% were identified with diagnostic codes and only 6.4% were initially identified with therapy codes only. There were 399 of 22,997 (1.7%) women first diagnosed with codes associated with “diabetes in pregnancy,” but there was no increase in this proportion over the time of study. All subjects had a minimum period of 12 months of records before the diabetes diagnosis date. Subjects who were ever diagnosed with type 1 diabetes or who were given prescriptions for insulin within 6 months of diagnosis were excluded as cases of type 1 diabetes. Prevalent cases were excluded because both therapy and hazards vary with duration of diabetes.
Analysis
Age-specific incidence rates for type 2 diabetes were estimated using the number of incident cases as the numerator and the registered person-years at risk as the denominator. Age-standardized rates were estimated using the European Standard Population for reference. The mean age at diagnosis and the proportion of diagnoses that were at ages 30–44 were also estimated. Trends by study year were estimated by linear regression using means or proportions as observations.
The characteristics of subjects at diagnosis were evaluated including whether coronary heart disease (CHD) (13), stroke (13), or renal disease (including any mention of a diagnosis associated with the kidney) was ever diagnosed before the diagnosis of diabetes using appropriate medical codes (13). Drug prescriptions were analyzed by mapping drug codes to chapter subheadings in the British National Formulary (14). We analyzed whether statins or antihypertensive drugs were ever prescribed before diagnosis of diabetes, with drugs acting on the RAS as a separate class. Antihypertensive drugs included ACE inhibitors, adrenergic neuron inhibiting drugs, angiotensin II receptor blockers, β-blockers, calcium channel antagonists, centrally acting drugs, thiazide and potassium-sparing diuretics, and vasodilators. Oral hypoglycemic drugs were grouped into metformin and sulfonylurea drugs. To analyze drug utilization after the diagnosis of diabetes while taking into account both calendar time and the duration of the diabetic illness, subjects were grouped by year of diagnosis. Then for each cohort defined by year of diagnosis, prescriptions were analyzed by year after the diagnosis of diabetes.
Mortality from all causes was estimated using the death records within the GPRD. To compare mortality of patients with diabetes diagnosed in different years, only the first 2 years after diagnosis were considered. This was because duration of follow-up was longer for earlier years of study, but mortality varies with diabetes duration. To avoid confounding of year of diagnosis with diabetes duration, analyses were restricted to the first 2 years after diagnosis. Mortality rates were estimated per 1,000 person-years of follow-up for men and women with diabetes and were standardized to the sample distribution for 2001 as reference. To adjust for explanatory variables, Cox proportional hazards models were fitted with date of diabetes diagnosis as the start date and the earliest of the date of death or 24 months after diagnosis or the end of the patient's record as the end date. Explanatory variables were year of diagnosis, age, prevalent CHD, stroke and renal disease, use of statins, antihypertensive therapy, and RAS drugs before diagnosis and prescribing of metformin, sulfonylurea drugs, statins, antihypertensive drugs, or RAS drugs after diagnosis. Robust SEMs were estimated to allow for clustering by practice. Because drug treatment after diagnosis varied over time, utilization of each drug was also fitted separately as a time-dependent covariate, with adjustment for prediagnosis events. Estimates from the two models were compared.
RESULTS
In the registered population aged ≥30 years, there were 953,223 person-years in 1996, rising to 1,048,067 in 2006. The proportion of registered subjects aged 30–44 years was 35% in 1996 and 34% in 2006. The female-to-male sex ratio was 1.08 in 1996 and 1.05 in 2006. There were 29,068 prevalent cases of diagnosed diabetes in 1996 and 62,455 in 2006. There were 2,636 incident cases of type 2 diabetes in 1996 and 5,416 in 2006 with 48,579 subjects with newly diagnosed diabetes in total between 1996 and 2006.
Table 1 shows age-standardized type 2 diabetes incidence rates for men and women by study year. The incidence of new diagnoses of type 2 diabetes increased in women from 2.23 per 1,000 in 1996 to 4.37 per 1,000 in 2006. In men, the increase was from 3.00 per 1,000 in 1996 to 5.24 per 1,000 in 2006. The mean age at first diagnosis of diabetes decreased in women from 66.1 years in 1996 to 62.5 years in 2006, but there was no trend in men (Table 1). The proportion of incident diabetes diagnoses in the 30- to 44-year age-group increased in women from 7.5% in 1996 to 15.8% in 2006.
Table 1.
Trends in type 2 diabetes incidence, mean age at diagnosis of diabetes, and comorbidity and drug utilization at diagnosis by year of diagnosis
| Year of diagnosis | Diabetes incidence ≥30 years (rate per 1,000 person-years)*
|
Age (years) at first diabetes diagnosis†
|
Proportion (%) of all new diagnoses in those aged 30–44 years
|
Prevalent CHD at diagnosis
|
Prevalent stroke at diagnosis
|
Prevalent renal disease before diagnosis
|
Prescribed statins before diagnosis
|
Prescribed other hypertensives before diagnosis
|
Prescribed RAS before diagnosis
|
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | Women | Men | |
| 1996 | 2.23 ± 0.07 | 3.00 ± 0.08 | 66.1 ± 13.4 | 62.5 ± 12.2 | 7.5 | 7.9 | 17.2 | 19.6 | 6.1 | 5.4 | 3.7 | 5.1 | 1.9 | 2.2 | 58.9 | 44.0 | 13.2 | 13.9 |
| 1997 | 2.29 ± 0.07 | 3.07 ± 0.08 | 65.5 ± 13.8 | 62.3 ± 12.1 | 8.6 | 7.9 | 15.9 | 19.9 | 4.9 | 5.1 | 3.0 | 5.8 | 3.5 | 4.3 | 61.5 | 41.9 | 16.5 | 15.4 |
| 1998 | 2.36 ± 0.07 | 3.39 ± 0.08 | 65.3 ± 14.3 | 62.1 ± 12.5 | 9.4 | 9.5 | 16.4 | 21.0 | 4.2 | 4.6 | 3.1 | 6.0 | 5.0 | 6.4 | 60.8 | 44.8 | 17.8 | 17.3 |
| 1999 | 2.66 ± 0.07 | 3.66 ± 0.09 | 65.3 ± 14.2 | 62.5 ± 12.1 | 9.3 | 7.6 | 16.5 | 22.9 | 4.6 | 5.9 | 2.3 | 5.2 | 8.1 | 9.9 | 63.4 | 50.9 | 19.6 | 19.6 |
| 2000 | 3.50 ± 0.08 | 4.58 ± 0.10 | 64.6 ± 14.5 | 62.3 ± 12.1 | 10.9 | 7.9 | 17.8 | 22.1 | 5.2 | 4.7 | 3.2 | 6.0 | 10.5 | 13.6 | 64.0 | 50.8 | 21.7 | 20.9 |
| 2001 | 3.83 ± 0.09 | 5.24 ± 0.10 | 64.1 ± 14.3 | 62.1 ± 12.2 | 11.0 | 8.5 | 17.0 | 22.8 | 4.1 | 4.0 | 3.3 | 5.6 | 14.0 | 15.8 | 65.4 | 53.9 | 24.4 | 24.2 |
| 2002 | 4.31 ± 0.09 | 5.63 ± 0.11 | 63.6 ± 14.7 | 62.0 ± 12.2 | 12.8 | 8.8 | 16.2 | 23.8 | 4.0 | 4.6 | 3.2 | 5.5 | 14.8 | 20.8 | 66.8 | 56.5 | 27.4 | 26.9 |
| 2003 | 4.62 ± 0.09 | 5.65 ± 0.11 | 63.0 ± 14.6 | 62.0 ± 12.5 | 13.4 | 9.2 | 17.2 | 21.7 | 3.7 | 5.0 | 2.9 | 6.5 | 19.5 | 25.0 | 68.1 | 58.1 | 29.6 | 29.5 |
| 2004 | 4.99 ± 0.10 | 5.81 ± 0.11 | 63.3 ± 15.1 | 62.8 ± 12.5 | 13.6 | 8.1 | 16.9 | 23.3 | 4.6 | 5.4 | 3.0 | 6.2 | 24.5 | 30.1 | 69.2 | 61.2 | 30.7 | 33.0 |
| 2005 | 4.71 ± 0.09 | 5.54 ± 0.10 | 62.9 ± 15.6 | 62.0 ± 12.3 | 15.7 | 9.3 | 14.2 | 21.3 | 3.8 | 4.8 | 3.3 | 6.5 | 27.6 | 33.5 | 67.0 | 59.3 | 33.1 | 34.4 |
| 2006 | 4.37 ± 0.09 | 5.24 ± 0.10 | 62.5 ± 15.3 | 62.0 ± 12.4 | 15.8 | 9.2 | 14.0 | 19.9 | 3.8 | 4.2 | 3.9 | 6.9 | 31.5 | 36.8 | 65.6 | 59.7 | 34.4 | 36.3 |
| P value‡ | <0.001 | <0.001 | <0.001 | 0.330 | <0.001 | 0.097 | 0.089 | 0.414 | 0.011 | 0.271 | 0.508 | 0.005 | <0.001 | <0.001 | 0.001 | <0.001 | <0.001 | <0.001 |
Data are percentage of subjects in whom diabetes was diagnosed in year except where indicated.
Age standardized to European Standard Population. Data are means ± SEM.
Data are means ± SD.
Test for linear trend by year.
Table 1 also shows comorbidity and coprescribing in subjects with newly diagnosed type 2 diabetes by year of diagnosis. Approximately 16% of women and 22% of men had prevalent CHD at diagnosis, whereas ∼4% of women and 5% of men had prevalent stroke. There was weak evidence of a decreasing trend in prevalent CHD and stroke in women. The proportion of subjects for whom statins were prescribed before the date of diagnosis increased from 2% in both men and women in 1996 to 32% in women and 37% in men in 2006. The prescription of antihypertensive drugs before diagnosis increased over time, more in men, and the increase was especially marked for the prescription of RAS drugs.
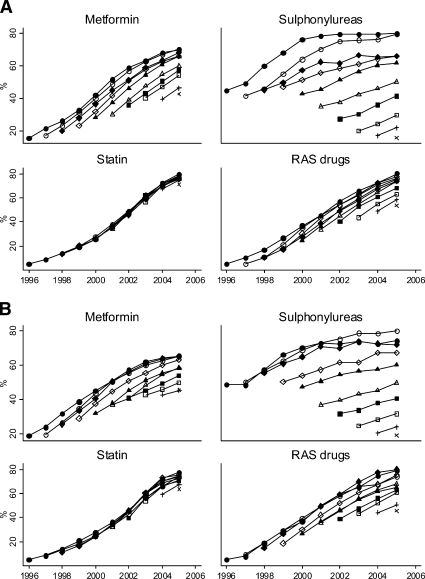
Figure 1 shows trends in drug utilization by patients with type 2 diabetes by year of diagnosis and duration of diabetes. Utilization of metformin, sulfonylurea drugs, and drugs acting on the RAS show a cohort effect, increasing as the duration of diabetes increases. However, utilization of metformin and RAS drugs increased for successive years of diagnosis, whereas utilization of sulfonylurea drugs declined. Utilization of statins only showed a period effect with increasing utilization over time independent of duration of diabetes. There were very large increases in prescribing of statins, metformin, and RAS drugs during the period. Prescription of statins within 12 months of diagnosis increased (1996, women 4.9%, men 5.1%; 2005, women 63.5%, men 71.0%) as did prescription of drugs acting on the RAS (1996, women 19.4%, men 21.5%; 2005, women 45.5%, men 54.6%) and metformin (1996, women 19.1%, men 15.8%; 2005, women 45.5%, men 42.8%), whereas prescription of sulfonylureas declined (1996, women 32.8%, men 34.3%; 2005, women 12.5%, men 14.1%). Utilization of insulin and other oral hypoglycemic drugs, including glitazones, increased during the period, but they were used by fewer than 10% of subjects within 2 years of diagnosis. Note that mortality analyses only included the first 2 years after diagnosis.
Figure 1.
Trends in drug utilization by patients with type 2 diabetes by year of diagnosis and duration of diabetes. Solid lines connect values for patients diagnosed in the same year and with data points representing increasing durations of diabetes. A: Men. B: Women.
Table 2 shows changes in all-cause mortality in men and women in the first 2 years after diagnosis of diabetes in subjects aged ≥30 years. In men, the relative decrease in mortality was 47% over the period, whereas in women, in whom absolute mortality was lower, the relative decline over the period was 26%.
Table 2.
Age-standardized rates for mortality within 2 years of diabetes diagnosis by year of diagnosis
| Year of diagnosis | Deaths (person-years)
|
Age-standardized mortality (per 1,000 person-years) within 24 months of diagnosis*
|
||
|---|---|---|---|---|
| Women | Men | Women | Men | |
| 1996 | 101 (2,387) | 127 (2,637) | 37.4 | 47.9 |
| 1997 | 107 (2,437) | 105 (2,749) | 40.7 | 37.7 |
| 1998 | 118 (2,558) | 148 (3,055) | 41.0 | 49.7 |
| 1999 | 134 (2,923) | 129 (3,413) | 40.7 | 37.6 |
| 2000 | 153 (3,838) | 151 (4,326) | 37.1 | 34.5 |
| 2001 | 166 (4,134) | 158 (5,009) | 39.9 | 31.5 |
| 2002 | 123 (4,792) | 176 (5,458) | 25.3 | 32.2 |
| 2003 | 147 (5,099) | 158 (5,595) | 30.7 | 28.1 |
| 2004 | 171 (5,675) | 167 (5,918) | 30.1 | 26.2 |
| 2005 | 118 (4,526) | 131 (4,780) | 25.9 | 27.2 |
| 2006* | 48 (1,751) | 50 (1,906) | 27.6 | 25.2 |
| P value† | 0.002 | <0.001 | ||
Rates were standardized to the sample distribution for 2001 for reference.
Two-year follow-up incomplete.
Test for linear trend.
In the proportional hazards model (Table 3), higher mortality was associated with older age and prevalent CHD, stroke, or renal disease. Prescription of statin drugs before or after diabetes diagnosis, prescription of drugs acting on the RAS before or after diagnosis, and prescription of metformin after diagnosis were associated with lower mortality and accounted for the association of year of diagnosis with mortality. After adjustment, increasing year of diagnosis was positively associated with mortality, but the significance of this finding is unclear. Hazard ratios (HRs) were generally similar for men and women, but HRs associated with prevalent CHD and stroke appeared to be higher for men, whereas the HR associated with prevalent renal disease was slightly higher in women. Fitting drug classes prescribed after diagnosis separately as time dependent covariates generally led to a similar interpretation.
Table 3.
Variables associated with mortality in first 2 years after diabetes diagnosis for men and women
| Women: HR (95% CI) | P value | Men: HR (95% CI) | P value | |
|---|---|---|---|---|
| Year of diagnosis (per year) | 1.04 (1.02–1.06) | <0.001 | 1.02 (1.00–1.04) | 0.113 |
| Age (per year) | 1.073 (1.067–1.078) | <0.001 | 1.071 (1.066–1.076) | <0.001 |
| Prevalent CHD at diagnosis | 1.15 (1.00–1.32) | 0.044 | 1.25 (1.10–1.43) | 0.001 |
| Prevalent stroke at diagnosis | 1.38 (1.13–1.69) | 0.002 | 1.71 (1.48–2.00) | <0.001 |
| Prevalent renal diseases at diagnosis | 1.58 (1.25–1.99) | <0.001 | 1.19 (0.98–1.44) | 0.071 |
| Statin use before diagnosis | 0.52 (0.43–0.63) | <0.001 | 0.56 (0.48–0.65) | <0.001 |
| Statins prescribed after diagnosis* | 0.29 (0.24–0.35) | <0.001 | 0.34 (0.29–0.40) | <0.001 |
| RAS drugs before diagnosis | 0.85 (0.75–0.96) | 0.007 | 0.90 (0.78–1.05) | 0.171 |
| RAS drugs prescribed after diagnosis* | 0.45 (0.37–0.55) | <0.001 | 0.56 (0.47–0.66) | <0.001 |
| Other antihypertensive treatment before diagnosis | 0.91 (0.80–1.04) | 0.158 | 1.18 (1.03–1.34) | 0.016 |
| Other antihypertensive prescribed after diagnosis* | 0.83 (0.62–1.10) | 0.206 | 0.86 (0.68–1.09) | 0.218 |
| Metformin prescribed after diagnosis* | 0.70 (0.60–0.80) | <0.001 | 0.61 (0.54–0.68) | <0.001 |
| Sulfonylurea drugs prescribed after diagnosis* | 1.44 (1.27–1.64) | <0.001 | 1.60 (1.43–1.78) | <0.001 |
| Insulin prescribed after diagnosis* | 1.20 (0.68–2.10) | 0.527 | 1.48 (0.92–2.36) | 0.103 |
HRs were adjusted for each of the variables shown.
Within 2 years of diagnosis.
CONCLUSIONS
Over the past 10 years there has been a substantial reduction in early mortality of type 2 diabetic patients within the first 2 years after diagnosis. Variables that may explain this decline in mortality include a decrease in the age at diagnosis in women and a slight fall in the proportion of women who have cardiovascular disease including CHD and stroke at diagnosis. Even allowing for case mix, there is evidence that a rapid increase in the proportion of men and women with newly diagnosed diabetes already taking statin drugs may be associated with lower mortality. Changing patterns of drug utilization after diagnosis of diabetes, including increased use of statins and metformin and decreased use of sulfonylurea drugs, may also be associated with lower mortality. These observations must be interpreted with caution as confounding by indication is generally important in nonrandomized studies, and the effects may be difficult to anticipate. The role of unmeasured risk factors such as cigarette smoking must also be considered. Earlier diagnosis may be contributing to increasing prevalence and could also contribute to declining mortality in clinical diabetes consistent with lead-time bias. This effect might be important for early mortality, whereas changes in drug utilization after diagnosis may be more relevant for later mortality after the first 2 years. Nevertheless, these analyses provide suggestive evidence that widespread implementation of preventive medical care both before and after the time of diagnosis may be contributing to the improving prognosis of type 2 diabetes. Trends in drug utilization were generally similar in men and women, but the decline in mortality was greater in men in whom absolute mortality rates were higher.
Comparison with other studies
The present observations must be set in the context of long-term declining trends in risk factors, such as smoking (15), as well as declining cardiovascular mortality in the general population (16). A number of studies have evaluated trends in all-cause mortality, cardiovascular mortality, and incident cardiovascular events in type 2 diabetes (17–22). Reports from Dundee, Scotland, from 1993 to 2004 (17) and Ontario, Canada, from 1992 to 2000 (18) show declining all-cause mortality in diabetic populations. These findings are consistent with a report from Rochester, Minnesota, which showed that between 1970 and 1994 mortality declined in diabetic subjects, although this decline was smaller than the mortality decrease observed in the nondiabetic population (19). Data from Ontario (17) and from the Framingham study (20) also demonstrate declining incidence of new cardiovascular events. However, there is evidence that trends may differ for men and women. Data from the U.S. National Health and Nutrition Examination Survey show that mortality of diabetic men declined between 1971 and 2000 (21,22). In women with diabetes, mortality initially increased (21) and then later showed no decline up to 2000 (22). Our results up to 2006 suggest that mortality in female as well as male diabetic patients is now declining. All-cause mortality in the general population has declined during this period, and further research is required to evaluate trends in relative mortality in patients with type 2 diabetes. It would also be desirable to evaluate cause-specific mortality. Analysis of GPRD data allows us to link individual patient survival data to information concerning comorbidity and prescribing. Results from these analyses show that across the diabetic population there have been major changes in drug utilization during this period, and these changes are associated with differences in mortality risk. In particular, utilization of statins either before or after diabetes diagnosis and use of metformin rather than sulfonylurea drugs after diagnosis may be associated with lower mortality risk.
Strengths and limitations
The validity of GPRD data has been demonstrated in several studies. In particular, Shah and Martinez (23) reported that mortality rates estimated from GPRD data were comparable to those observed in the U.K. general population. Mulnier et al. (24) reported a mortality rate for individuals with prevalent cases of diabetes in GPRD of 60.2 per 1,000 patient-years, which is higher than the rate we reported for individuals with incident cases of diabetes with short durations. The validity of clinical event data in GPRD has been shown to be good (13). However, causes of death were not readily available for analysis and cause-specific mortality was not estimated. Clinical information for measures including smoking, blood pressure, cholesterol, and A1C is included in the GPRD, but there were secular trends in recording in the present period that would complicate interpretation. Classification of drug prescribing was based on one or more prescriptions, but interpretation did not differ if two or more prescriptions were used. Drug combinations were not explicitly modeled.
Although overall data for mortality can be viewed with confidence, in this nonrandomized study, associations identified may be explained by unmeasured or misclassified confounders. When unmeasured and imprecisely measured confounding is present, associations may be incorrectly ascribed to more precisely measured exposures such as drug utilization. We caution that the results should not be used to estimate the benefits or harms of particular therapies. Rather, the present results suggest that findings from randomized clinical trials may hold in the general population and contribute to improving survival trends. Combinations of these interventions may be particularly beneficial (25).
In summary, mortality of men and women with newly diagnosed type 2 diabetes has declined between 1996 and 2006. Widespread use of statins before and after diagnosis and use of metformin rather than sulfonylurea drugs after diagnosis may be associated with improving mortality trends.
Published ahead of print at http://care.diabetesjournals.org on 28 May 2008.
This study is based in part on data from the Full Feature General Practice Research Database (GPRD) obtained under license from the U.K. Medicines and Healthcare Products Regulatory Agency (MHRA). However, the interpretation and conclusions contained in this study are those of the authors alone. Access to the GPRD database was funded through the Medical Research Council's license agreement with MHRA.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C Section 1734 solely to indicate this fact.
References
- 1.Centers for Disease Control, Division of Diabetes Translation: Diabetes data and trends [article online], 2007. Available from http://apps.nccd.cdc.gov/DDTSTRS/default.aspx. Accessed 10 January 2008
- 2.Sproston K, Primatesta P: Health Survey for England 2003. Volume 2. Risk Factors for Cardiovascular Disease. London, The Stationery Office, 2004
- 3.Burke JP, Williams K, Gaskill SP, Hazuda HP, Haffner SM, Stern MP: Rapid rise in the incidence of type 2 diabetes from 1987 to 1996: results from the San Antonio Heart Study. Arch Intern Med 159:1450–1456, 1999 [DOI] [PubMed] [Google Scholar]
- 4.Koopman RJ, Mainous AG III, Diaz VA, Geesey ME: Changes in age at diagnosis of type 2 diabetes mellitus in the United States, 1988 to 2000. Ann Fam Med 3:60–63, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trial. Lancet 360:7–22, 2002 [DOI] [PubMed] [Google Scholar]
- 6.Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH, CARDS Investigators: Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomized placebo-controlled trial. Lancet 364:685–696, 2004 [DOI] [PubMed] [Google Scholar]
- 7.UK Prospective Diabetes Study Group: Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. UK Prospective Diabetes Study Group. BMJ 317:720–726, 1998 [PMC free article] [PubMed] [Google Scholar]
- 8.Heart Outcomes Prevention Evaluation (HOPE) Study Investigators: Effects of ramipril on cardiovascular and microvascular outcomes in people with diabetes mellitus: results of the HOPE study and MICRO-HOPE substudy. Lancet 355:253–259, 2000 [PubMed] [Google Scholar]
- 9.UK Prospective Diabetes Study Group: Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853, 1998 [PubMed] [Google Scholar]
- 10.UK Prospective Diabetes Study Group: Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes (UKPDS 34). Lancet 352:854–865, 1998 [PubMed] [Google Scholar]
- 11.Evans J, Ogston S, Emslie-Smith A, Morris A: Risk of mortality and adverse cardiovascular outcomes in type 2 diabetes: a comparison of patients treated with sulfonylureas and metformin. Diabetologia 49:930–936, 2006 [DOI] [PubMed] [Google Scholar]
- 12.Johnson JA, Simpson SH, Toth EL, Majumdar SR: Reduced cardiovascular morbidity and mortality associated with metformin use in subjects with type 2 diabetes. Diabet Med 22:497–502, 2005 [DOI] [PubMed] [Google Scholar]
- 13.National Statistics: Key Health Statistics from General Practice 1998. Series MB6 No 2. London, National Statistics, 2000
- 14.British Medical Association and Royal Pharmaceutical Society of Great Britain: British National Formulary. No. 44. London, British Medical Association and Royal Pharmaceutical Society of Great Britain, 2002
- 15.Goddard E: General Household Survey 2006: Smoking and Drinking among Adults, 2006. Newport, U.K.: Office for National Statistics, 2008
- 16.Rautio A, Lundberg V, Messner T, Nasic S, Stegmayr B, Eliasson M: Favourable trends in the incidence and outcome of myocardial infarction in nondiabetic, but not in diabetic, subjects: findings from the MONICA myocardial infarction registry in northern Sweden in 1989–2000. J Intern Med 258:369–377, 2005 [DOI] [PubMed] [Google Scholar]
- 17.Evans J, Barnett K, Ogston S, Morris A: Increasing prevalence of type 2 diabetes in a Scottish population: effect of increasing incidence or decreasing mortality? Diabetologia 50:729–732, 2007 [DOI] [PubMed] [Google Scholar]
- 18.Booth GL, Kapral MK, Fung K, Tu JV: Recent trends in cardiovascular complications among men and women with and without diabetes. Diabetes Care 29:32–37, 2006 [DOI] [PubMed] [Google Scholar]
- 19.Thomas RJ, Palumbo PJ, Melton LJ III, Roger VL, Ransom J, O'Brien PC, Leibson CL: Trends in the mortality burden associated with diabetes mellitus: a population-based study in Rochester, Minn, 1970–1994. Arch Intern Med 163:445–451, 2003 [DOI] [PubMed] [Google Scholar]
- 20.Fox CS, Coady S, Sorlie PD, Levy D, Meigs JB, D'Agostino RB Sr, Wilson PW, Savage PJ: Trends in cardiovascular complications of diabetes. JAMA 292:2495–2499, 2004 [DOI] [PubMed] [Google Scholar]
- 21.Gu K, Cowie CC, Harris MI: Diabetes and decline in heart disease mortality in US adults. JAMA 281:1291–1297, 1999 [DOI] [PubMed] [Google Scholar]
- 22.Gregg EW, Gu Q, Cheng YJ, Venkat Narayan KM, Cowie CC: Mortality trends in men and women with diabetes, 1971 to 2000. Ann Intern Med 147:149–155, 2007 [DOI] [PubMed] [Google Scholar]
- 23.Shah AD, Martinez C: A comparison of the cause of death recorded in GPRD with national mortality statistics in England and Wales. Pharmacoepidemiol Drug Saf 13:S2–S3, 2004 [Google Scholar]
- 24.Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA: Mortality in people with type 2 diabetes in the UK. Diabet Med 23:516–521, 2006 [DOI] [PubMed] [Google Scholar]
- 25.Gaede P, Lund-Andersen H, Parving HH, Pedersen O: Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 358:580–591, 2008 [DOI] [PubMed] [Google Scholar]