Abstract
Background and purpose:
Chronic inflammatory conditions, such as granulomas, are associated with angiogenesis. Mast cells represent the main cell type orchestrating angiogenesis, through the release of their granule content. Therefore, compounds able to modulate mast cell behaviour may be considered as a new pharmacological approach to treat angiogenesis-dependent events. Here, we tested the effect of selective cannabinoid (CB) receptor agonists in a model of angiogenesis-dependent granuloma formation induced by λ-carrageenin in rats.
Experimental approach:
Granulomas were induced by λ-carrageenin-soaked sponges implanted subcutaneously on the back of male Wistar rats. After 96 h, implants were removed and granuloma formation was measured (wet weight); angiogenesis was evaluated by histological analysis and by the measurement of haemoglobin content. Mast cells in the granulomas were evaluated histologically and by RT-PCR and immunoblotting analysis for mast cell-derived proteins (rat mast cell protease-5 (rMCP-5) and nerve growth factor). Selective CB1 and CB2 receptor agonists, ACEA and JWH-015 (0.001–0.1 mg mL−1), were given locally only once, at the time of implantation.
Key results:
The CB1 and CB2 receptor agonists decreased the weight and vascularization of granulomas after 96 h. This treatment also reduced mast cell number and activation in granulomatous tissue. Specifically, these compounds prevented the transcription and expression of rMCP-5, a protein involved in sprouting and advance of new blood vessels.
Conclusion and implications:
Modulation of mast cell function by cannabinoids reduced granuloma formation and associated angiogenesis. Therefore cannabinoid-related drugs may be useful in the management of granulomatous diseases accompanied by angiogenesis.
Keywords: cannabinoids, chronic inflammation, granuloma formation, angiogenesis, mast cells
Introduction
Angiogenesis, the process leading to new vessel formation from the pre-existing vessels, is involved both in physiological and pathological conditions, such as rheumatoid arthritis, diabetic retinopathy and tumour growth. During chronic inflammation, angiogenesis occurs for the maintenance of tissue perfusion and to allow the increase in cellular trafficking necessary for chronicity (Colville-Nash et al., 1995).
Several experimental models, both in vitro and in vivo, have been used to characterize the mechanisms involved in new blood vessel formation and associated cell trafficking, to develop drugs and strategies to control or prevent the pathological consequences. The subcutaneous implantation of λ-carrageenin-soaked sponges on the back of rats induces a chronic response, characterized by granuloma formation and including an intense angiogenesis and infiltration of inflammatory cells (Lage and Andrade, 2000). Granulomatous tissue is histologically well-characterized by the presence of infiltrating macrophages, epithelioid and giant cells, activated mast cells (MCs), surrounded by a lymphocyte mantle and proliferating fibroblasts (Forehand and Johnston, 1994). Among the cells participating in granuloma formation, connective tissue type MCs, especially present in the skin, importantly contribute to the development of chronic inflammation. MCs, which have been shown to accumulate near sites of new capillary sprouting, have been implicated in angiogenesis; in fact they produce, store and release several mediators, both vasoactive amines (Metcalfe et al., 1997) and enzymes to degrade the connective tissue matrix, thus providing space for neovascular sprouts (Kähäri and Saarialho-Kere, 1997; Tozzi et al., 1998).
Among the mediators in MCs, the chymases, a family of serine proteases exclusively expressed in connective tissue MCs, represent interesting molecules exhibiting both pro-inflammatory and pro-angiogenic activities (Coussens et al., 1999). In humans and dogs, only α-chymases are present (Takai et al., 1997), whereas mice and rats have several chymase isoenzymes that belong to the α-chymase family (mouse mast cell protease-5 and rat mast cell protease-5 (rMCP-5)) and the β-chymase family (mouse MCP-1,2,4 and rMCP-1, 2, 4) (Reynolds et al., 1990; Lutzelschwab et al., 1997).
Recently, cannabinoids have been described as a novel class of antiangiogenic compounds, as they inhibit migration and survival of vascular endothelial cells (Blázquez et al., 2004). Moreover, administration of cannabinoids to glioma-bearing mice decreases the activity and the expression of matrix metalloproteinase-2, a proteolytic enzyme that allows tissue breakdown and remodelling during angiogenesis trans-activation (Hart, 2004).
Most of the effects of the cannabinoids are mediated by the activation of specific G protein-coupled receptors that are normally bound by a family of endogenous ligands—the endocannabinoids (Bisogno et al., 2005). Two different receptors for CB compounds (Alexander et al., 2008) have been characterized and cloned from mammalian tissues: the CB1 receptors, mostly expressed in the nervous system and responsible for CB psycho-activity (Pertwee, 1999), and the CB2 receptors, mostly expressed in the immune system and unrelated to CB psycho-activity (Matias et al., 2002). However, the expression of both CB1 and CB2 receptors on cells from the immune system has also been extensively documented (Croxford and Yamamura, 2005). In the present context, MCs express both CB1 and CB2 receptors, which exhibit differential roles during IgE-dependent responses (Samson et al., 2003). The endocannabinoid 2-arachydonoyl glycerol, which preferentially binds to CB2 receptors, decreases the immunological activation of guinea pig MCs (Vannacci et al., 2004).
Although the effects of cannabinoids in angiogenesis-dependent pathologies, especially that associated with several tumour types (Blazquez et al., 2003; Casanova et al., 2003) are well known (Kogan et al. 2006, De Filippis et al. 2007), their role in MC-dependent angiogenesis has never been studied. The aim of our study was, therefore, to investigate the effect of synthetic CB agonists as a new class of antiangiogenic agents, focusing on their ability to control MC function and their release of pro-angiogenic factors, in a model of granuloma formation in rats.
Methods
Animals
All animal procedures and experiments were in accordance with European Community Council Directive 86/609/EEC and efforts were made to minimize animal suffering and to reduce the number of animals used. Experiments using animals were done with the permission of the national authorities (Ministero della Salute Prot. 5/05 to Professor Teresa Iuvone). Male Wistar rats (Harlan, Italy), weighing 220–250 g, were used in all experiments. Animals were provided with food and water ad libitum. The light cycle was automatically controlled (on 07 h 00 min; off 19 h 00 min) and the room temperature thermostatically regulated to 22±1 °C with 60±5% humidity. Prior to the experiments, animals were housed in these conditions for 3–4 days to become acclimatized.
Sponge implantation
Sponges were implanted as previously described by De Filippis et al. (2007). Briefly, two polyether sponges (0.5 × 1.5 × 2.0 cm) weighing 0.035±0.002 g were implanted subcutaneously on the back of rats (n=12–18 for each group) under general anaesthesia. Sponges and surgical instruments were sterilized by autoclaving for 20 min at 120 °C. λ-carrageenin (1% w v−1) (Sigma, St Louise, MI, USA) was dissolved in pyrogen-free saline (500 mg in 0.5 mL per implant), in presence or absence of CB agonists and injected into each sponge; saline (0.5 mL per implant) was used as control. Ninety-six hours after sponge implantation, rats were killed by inhaling CO2.
Treatments
The non-selective CB1/CB2 full agonist WIN 55,212-2, a CB1 selective agonist, ACEA, or a CB2 selective agonist, JWH-015, were given only once, at the time of sponge implantation, together with the λ-carrageenin. In some experiments, ketotifen fumarate (0.1 mg mL−1; equivalent to 50 μg per implant), a mast cell stabilizer, was given similarly only at implantation, as a positive control to prevent mast cell degranulation. Three different concentrations of ACEA and JWH-015 (0.001, 0.01 and 0.1 mg mL−1; equivalent to 0.5, 5 and 50 μg per implant) were tested.
Collection of tissue, weight evaluation and homogenization
After death, implants and the adherent granulomas were excised from the back of the rats. The granulomatous tissue, that is, the newly formed tissue encapsulating the sponge, was then dissected from the sponge and weighed always by the same person who was unaware of the treatments. This tissue was then immediately frozen in liquid nitrogen and stored in sterile and RNAse free vials at −80 °C until used.
For homogenization, tissue was suspended in ice-cold hypotonic lysis buffer (20 mM HEPES, 100 mM MgCl2, 0.4 M NaCl, 0.5 mM phenylmethylsulphonylfluoride, 15 μg mL−1 soybean trypsin inhibitor, 3 μg mL−1 pepstatin A, 2 μg mL−1 leupeptin, 40 μM benzamidine, 1 mM dithiothreitol, 1% Nonidet P40, 20% glycerol) in a ratio of 0.4 mL per 100 mg of tissue and homogenized at the highest setting for 2–5 min in Polytron PT300 tissue homogenizer. Protein concentration was determined using the Bio-Rad protein assay kit.
Preparation of cytosolic fraction
After homogenization, the cytosolic fraction was obtained by centrifugation for 1 min at 13 000 g. The nuclear pellet was resuspended in 60 μL of high salt extraction buffer (20 mM HEPES pH 7.9, 420 mM NaCl, 1.5 mM MgCl2, 0.2 mM EDTA, 25% v v−1 glycerol, 0.5 mM phenylmethylsulphonylfluoride, 1.5 μg mL−1 soybean trypsin inhibitor, 7 μg mL−1 pepstatin A, 5 μg mL−1 leupeptin, 0.1 mM benzamidine, 0.5 mM dithiothreitol) and incubated with shaking at 4 °C for 30 min. Protein concentration in cytosolic fractions was determined by the Bio-Rad protein assay kit.
Evaluation of angiogenesis
Angiogenesis was evaluated both by histological investigations (Histology of granulomatous tissue) and by the measurement of haemoglobin (Hb) content in the granulomatous tissue. For the evaluation of Hb content, the granulomatous tissue was homogenized on ice with the Polytron PT300 tissue homogenizer in 1 M PBS (4 mL g−1 wet weight) as previously described (De Filippis et al., 2007). Briefly, after centrifugation at 2500 g for 20 min at 4 °C, the supernatant was further centrifuged at 5000 g for 30 min and Hb concentration in the supernatant was determined spectrophotometrically at 450 nm by using the Hb assay kit (Sigma Diagnostic, St Louise, MI, USA). The Hb content was expressed as mg Hb g−1 wet weight.
Western blot analysis
Western blotting analysis for r-MPC-5, nerve growth factor (NGF) and tubulin proteins was performed on the total protein fraction of homogenates of granulomatous tissue. Total proteins were mixed with gel loading buffer (50 mM Tris/10% SDS/10% glycerol 2-mercaptoethanol/2 mg bromophenol in a final volume of 1 mL) in a ratio of 1:1 and boiled for 3 min. Equivalent amounts (50 μg) of each sample were analysed by electrophoresis through a 12% discontinuous polyacrylamide minigel. Proteins were transferred onto nitrocellulose membrane, according to the manufacturer's instructions (Bio-Rad, Segrate, Milano, Italy). The membranes were saturated by incubation at 4 °C overnight with 10% non-fat dry milk in 1 M PBS and then incubated with the appropriate antiserum: anti-mouse chymase antiserum (1:250 v:v, NeoMarker, Fremont, CA, USA), anti-mouse NGF (1:250 v:v, Sigma-Aldrich, St Louise, MI, USA), anti-mouse tubulin (1:1000 v:v, Santa Cruz, Santa Cruz, CA, USA) for 2 h at room temperature. The membranes were washed three times with 1% Triton X-100 in PBS 1 M and then incubated with anti-mouse immunoglobulins coupled to peroxidase (Dako, Glostrup, Denmark) (1:2000 v:v). The immune complexes were developed using enhanced chemiluminescence detection reagents (Amersham, Freiburg, Germany), according to the manufacturer's instructions and exposed to Kodak X-Omat film. The protein bands on X-ray film were scanned and densitometrically analysed with a GS-700 imaging densitometer.
mRNA analysis
The r-MPC5 mRNA level in granulomatous tissue was determined by using the semi-quantitative RT-PCR method. Total RNA was extracted from tissue samples by using an ultrapure TRIzol reagent (GibcoBRL, Carlsbad, CA, USA) as directed by the manufacturer. RNA (5 μg) was then reverse-transcribed in 20 μL with 200 U of Superscript II RNase H-Reverse Transcriptase (Invitrogen, Carlsbad, CA, USA) in the presence of random hexamers (5 μM), 20 U of RNasin (Promega, Milano, Italy), dNTPs (10 mM), for 1 h at 42 °C. PCR was performed on 2 μL of the reverse transcription reaction mixture in a final volume of 50 μL with 2.5 U of Taq polymerase (Roche, Milano, Italy) and 5 μM of the appropriate primers as follows: rMCP-5 5′-TCCTGCAAACACTTCACCAG-3′ (forward primer) and 5′-CGAGATCCAGAGTTAATTCT-3′ (reverse primer); β-actin 5′-GGCACCACACCTTCTACA-3′ (forward primer) and 5′-CAGGAGGAGCAATGATCT-3′ (reverse primer). To obtain linear amplification curves, the cDNA mixtures were subjected to 10, 15 and 20 cycles for the control β-actin and 20, 25 and 30 cycles for all other genes under the following conditions: denaturating at 95 °C for 1 min, annealing at 52 or 56 °C for 1 min for chymase respectively, and extension at 72 °C for 1 min. The final extension step was performed at 72 °C for 10 min. Aliquots (15 μL) of PCR products were electrophoretically fractionated through 1% agarose gel containing the fluorescent Vistra green dye (Amersham Pharmacia Biotech, Freiburg, Germany) (Mullane et al., 1985). Labelling intensity of the PCR product, which is linear to the amount of DNA, was quantified using the Molecular Imager FX and Quantity One software (Bio-Rad).
Histology of granulomatous tissue
After excision of the implant, the granulomatous tissue around the sponge was removed and fixed in 10% formalin. Thin (0.5 μm) paraffin sections were prepared and stained with toluidine blue according to Iuvone et al. (1999) and then processed for light microscopy examination. Mast cells were counted in five randomly selected sections using a × 100 objective lens, differentiating between deep blue (un-degranulated) and light blue (degranulated) MCs. In some experiments, paraffin wax sections were cut at 4–6 μm and stained with haematoxylin and eosin for the evaluation of blood vessels. The same person counted the blood vessels in different fields on at least three different stained sections of the same group, but from different experiments.
β-Hexosaminidase analysis
Degranulation of MCs in granulomatous tissues was measured by the release of the granular enzyme β−hexosaminidase, using a method first described by Hernandez-Hansen et al. (2004). Granulomatous tissue was placed in 24-well culture plates and cultured in Dulbecco's modified Eagle's medium supplemented with 5% foetal bovine serum, 2 mM glutamine, 100 U mL−1 penicillin, 100 μg mL−1 streptomycin at 37 °C in 5% CO2/95% air for 24 h according to Coëffier et al. (2002).
Aliquots (50 μL) of tissue culture medium were then collected from each well and transferred into a 96-well plate. The substrate, p-nitrophenyl N-acetyl-β-D-glucosaminide (50 μL of a 2 mM solution diluted in 0.2 M citrate buffer, pH 4.5), was added to each well. The samples were then incubated with the substrate for 2 h at 37 °C. All incubations were carried out at this temperature because the reactions are sensitive to temperature changes. Medium and chemicals were also kept at 37 °C throughout the experiment to avoid any temperature changes. After 2 h, reactions were terminated by adding 150 μL of 1 M Tris-buffer pH 9.0. The absorbance was measured in a microplate reader at 405 nm. The β-hexosaminidase content was also determined in parallel wells where the cultured tissue was homogenized in PBS. Mast cell degranulation was expressed as percentage of β-hexosaminidase release, calculated as the ratio between β-hexosaminidase released into the supernatant and the total β-hexosaminidase content released from the homogenate.
Data analysis
Results were expressed as the mean±s.e.m. of n animals where each value is the average of responses in duplicate sites. Statistical comparisons were made by one way-ANOVA followed by Bonferroni's test for multiple comparisons. A P-value of less than 0.05 was considered to be significant.
Drugs
The non-selective CB1/CB2 full agonist WIN 55 212−2, (Ki=62,3 and 3,3 nM at human cloned CB1 and CB2 receptors respectively), the potent and the highly selective CB1 receptor agonist ACEA, (Ki=1,4 nM for CB1 displays >1400-fold selectivity over CB2 receptors) and the selective CB2 receptor agonist JWH-015 (Ki values are 13,8 and 383 nM as measured at human cloned CB2 and CB1 receptors expressed in CHO cells) were purchased from Tocris, Bristol, UK and were dissolved in ethanol. A volume of 100 μL of ethanol (0.01% v:v) did not affect the response under study. All other materials unless otherwise stated were purchased from Sigma Aldrich, Gallarate (Mi), Italy. Drug and molecular target nomenclature follows the Guide to Receptors and Channels (Alexander et al., 2008).
Results
Effect of the selective CB1 receptor agonist ACEA and selective CB2 receptor agonist JWH-015, on λ-carrageenin-induced granuloma formation and related angiogenesis
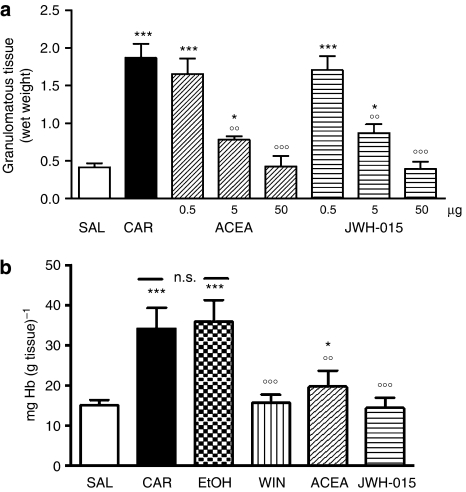
The selective CB1 and CB2 CB receptor agonists, ACEA and JWH-015, applied locally in the sponge at the time of implantation, decreased λ-carrageenin-induced granuloma formation in rats after 96 h of implantation (Figure 1a) This reduction was dose-dependent and approximately equal for the two agonists over the concentration range used (0.001–0.1 mg mL−1; 0.5–50 μg).
Figure 1.
Effect of the selective CB1 receptor agonist ACEA and the selective CB2 receptor agonist JWH-015 on λ-carrageenin (CAR)-induced granuloma. (a) ACEA (0.5, 5, 50 μg per implant) and JWH-015 (0.5, 5, 50 μg), significantly and in a concentration-dependent manner reduced granulomatous tissue formation, evaluated as wet weight at 96 h after implantation. (b) Local administration of ACEA (50 μg) or JWH-015 (50 μg) or the non-selective CB1/CB2 receptor agonist, WIN 55,212-2 (WIN; 50 μg), significantly reduced angiogenesis, evaluated as haemoglobin (Hb) content of the granuloma. No effects were observed in the group treated with vehicle (10% ethanol;EtOH). Results are expressed as mean±s.e.m. of three separate experiments. *P<0.05, ***P<0.001 vs saline; °°P<0.01, °°°P<0.001 vs λ-carrageenin alone.
The selective agonists, ACEA and JWH-015, at their highest dose (0.1 mg mL−1; 50 μg), as well the non-selective CB1/CB2 receptor agonist, WIN 55 212-2 (0.1 mg mL−1: 50 μg), significantly decreased neovascularization in the granulomatous tissue, measured as Hb content, by 55, 47 and 58%, relative to the values obtained with λ-carrageenin alone. The vehicle (10% ethanol) had no effect on either the weight of the granulomatous tissue or on its vascularization (Figures 1a and b).
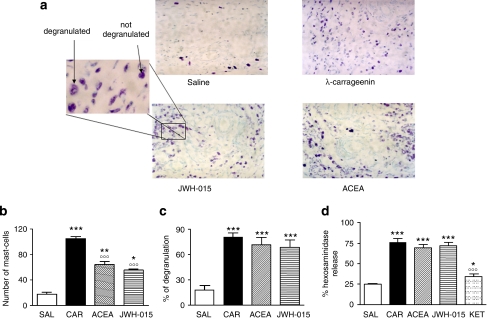
Effect of ACEA and JWH-015 on λ-carrageenin induced-mast cell activation in granulomatous tissue
Histological analysis of granulomatous tissue showed that ACEA (50 μg) and JWH-015 (50 μg) reduced the total number of MCs, by about 50% with respect to λ-carrageenin alone (Figure 2a; summarized in Figure 2b), but did not change the proportion of degranulated MCs induced by λ-carrageenin (Figure 2c). In addition, λ-carrageenin also increased β-hexosaminidase release (as marker of degranulation) in the granulomas, whereas the treatment with CB agonists did not affect this process (Figure 2d). Ketotifen (50 μg), a well known MC membrane stabilizer, used as positive control, reduced hexosaminidase release in the carrageenin-soaked sponge by 60% (Figure 2d).
Figure 2.
Effect of the selective CB1 receptor agonist ACEA (50 μg) and the selective CB2 receptor agonist JWH-015 (50 μg) on λ-carrageenin (CAR)-induced mast cell activation. In panel (a) is shown a representative histological analysis of mast cells present in granulomatous tissue. Mast cells were evaluated in paraffin sections stained with 0.05% (w v−1) toluidine blue and counterstained with 0.1% (w v−1) nuclear fast red (magnification × 100). The square panel is an enlargement showing the differences between not degranulated (deep blue) and degranulated (light blue) mast cells. In panel (b) is shown the total number of mast cells; in panel (c) the percentage of mast cell degranulation (the ratio between not degranulated and degranulated mast cells) is shown; in panel (d) is shown the percentage of the β−hexosaminidase release, as a specific marker of mast cell degranulation. Ketotifen (KET; 50 μg) was used as a positive control. Results are expressed as mean±s.e.m. of three separate experiments. *P<0.05, **P<0.01, ***P<0.001 vs saline; °°°P<0.001 vs λ-carrageenin alone.
Effect of ACEA and JWH-015 on levels of mRNA for rMCP-5
We have previously demonstrated that the amount of rMCP-5, the most abundantly expressed chymase in the skin (Wintroub et al., 1984) with pro-angiogenic effects, was increased in the granulomatous tissue by λ-carrageenin treatment (Russo et al., 2005). As we have shown that cannabinoids are able to reduce angiogenesis, we wondered if the formation of new vessels was associated with a modulation of rMCP-5 gene expression. To this purpose, total RNA extracted from the granulomatous tissue 96 h after sponge implants was subjected to semi-quantitative RT-PCR by using specific primers for rMCP-5. We also amplified the same preparation with oligonucleotides designed against β-actin mRNA as control of cDNA amount. As shown in Figure 3, levels of rMCP-5 mRNA were markedly higher in the granulomatous tissue of λ-carrageenin-soaked sponges. After treatment with ACEA (50 μg) or JWH-015 (50 μg), this induced increase was reduced by about 50% by either agonist (Figure 3b).
Figure 3.
Effects of the selective CB1 receptor agonist ACEA and the CB2 receptor agonist JWH-015 on rMCP-5 transcription and expression. (a) Representative Vistra green-stained agarose gel of RT-PCR products corresponding to rMCP-5 mRNA in sponges injected with saline solution (SAL) or with λ-carrageenin (CAR) or λ-carrageenin in the presence of ACEA (50 μg) or JWH-0.15 (50 μg). β-actin, a housekeeping gene, was used as a control. The gel shown corresponds to the products from 35 cycles of amplification for rMCP-5 and 15 cycles for β-actin. (b) Summary of values from three independent experiments expressed as percent, after normalization to β-actin mRNA level. Results are expressed as mean±s.e.m. of three separate experiments. *P<0.05, ***P<0.001 vs saline.; °°°P<0.001 vs λ-carrageenin alone.
Effect of ACEA and JWH-015 on λ-carrageenin- induced expression of rMCP-5 and NGF
Not only the transcription but also the expression of rMCP-5 protein in granulomatous tissue was affected by λ-carrageenin treatment, as shown by immunoblotting and relative densitometric analysis. The antibody used for rMCP-5 was raised in mice and recognized rat chymase. Either ACEA or JWH-015 significantly reduced rMCP-5 protein expression by about 50%, compared with that after λ-carrageenin alone (Figure 4a). We also evaluated another specific MC-derived protein, NGF. NGF protein expression was increased in λ-carrageenin-treated sponges as shown by western blot and relative densitometric analysis. The same dose of ACEA or JWH-015 (50 μg) reduced the expression of this marker protein by 53 and 51%, respectively, compared with that in sponges treated with λ-carrageenin alone (Figure 4b).
Figure 4.
Effects of the CB1 receptor agonist ACEA (50 μg) and the CB2 receptor agonist JWH-015 (50 μg) on expression of proteins secreted by mast cells. In (A) rMCP-5 and (B) NGF protein expression is shown by a representative western blot (a) and relative densitometric analysis (b). Tubulin expression is shown as a control. Data are expressed as mean±s.e.mean of three separate experiments. *P<0.05, **P<0.01, ***P<0.001 vs saline; □□P<0.01, □□□P<0.001 vs λ-carrageenin (CAR) alone.
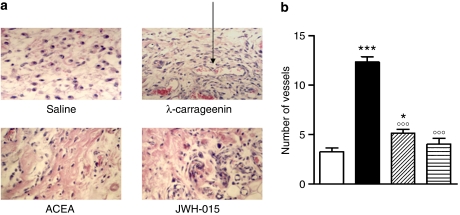
Effect of ACEA and JWH-015 on vessel numbers in granulomatous tissue
Histological analysis performed on haematoxylin–eosin stained sections of granulomas showed that λ-carrageenin treatment markedly increased the number of vessels in the tissue, compared with saline-treated sponges. ACEA or JWH-015 (50 μg) significantly reduced, by 59 and 68% respectively, the numbers of blood vessels, in comparison to those in sections from sponges treated with λ-carrageenin alone (Figure 5).
Figure 5.
Effect of the CB1 receptor agonist ACEA (50 μg) and the CB2 receptor agonist JWH-015 (50 μg) on angiogenesis in granulomatous tissue. Angiogenesis was evaluated by histological analysis and vessel number. Panel (a) shows a representative histological analysis of granulomatous tissue stained with hematoxylin and eosin. Fields are representative of three separate experiments. Original magnification × 100. Panel (b) shows the number of blood vessels in granulomatous tissue. Results are expressed as mean±s.e.m. of three separate experiments. *P<0.05, ***P<0.001 vs saline; °°°P<0.001 vs λ-carrageenin (CAR) alone.
Discussion
Angiogenesis occurs both in physiological processes, such as wound healing (Trabucchi et al., 1988) and placental development (Augustin et al., 1995) and in many pathological conditions, including solid tumours (Folkman, 1995), diabetic retinopathy (Mohamed et al., 2007), rheumatoid arthritis (Malone et al., 1987) and other inflammatory disorders (Hunt et al., 1984; Toda et al., 2000). The importance of MCs in orchestrating the processes of angiogenesis is now well recognized, as these cells are in close proximity to blood vessels and release a plethora of pro-angiogenic mediators. In the light of these findings, in the present study we investigated the effect of cannabinoids in preventing MC-dependent angiogenesis during granuloma formation.
Our results show that selective CB1 and CB2 receptor full agonists, respectively ACEA and JWH-015, given into the sponge at the time of implantation, were able to control MC function, resulting in a decreased growth of the granuloma (wet weight) and decreased angiogenesis within the granuloma. These results are in accordance with previous results from Facci et al. (1995) and our own recent data (Iuvone et al., 2007), indicating that cannabinoids are able to control MC activation through a mechanism which is mediated, at least in part, by either CB1 or CB2 receptor activation. In the present study, we did not counteract antiangiogenic effects of ACEA and JWH-015 by selective antagonism of CB1 and CB2 receptors, and we therefore cannot definitively exclude non-CB receptor-mediated effects, especially for JWH-015 which exhibits other activities unrelated to CB2 receptors (Velez-Pardo and Del Rio, 2006). On the other hand, it is well known that cannabinoids control MC behaviour, mainly through a CB2 receptor-dependent mechanism (for a review see De Filippis et al. 2008).
Here, for the first time, we showed that both the selective agonists, ACEA and JWH-015, reduced λ-carrageenin-induced increase of MC numbers in granulomatous tissue, without affecting, in our conditions, the extent of MC degranulation. In our experimental conditions, the effects of cannabinoids on MC function were linked to the inhibition of MC transcriptional machinery, as confirmed by RT-PCR for rMCP-5. After treatment with ACEA and JWH-015, we observed a significant downregulation (about 50%) of rMCP-5 gene expression at transcriptional and, at translational levels. We focused our study on rMCP-5 protein because it is the only protein stored and/or newly synthesized exclusively by connective tissue MCs and for this reason it could be considered as an index of MC function. Our data highlighted that cannabinoids reduce not only the transcription but also the expression of rMCP-5 protein in granulomatous tissue. This enzyme, rMCP-5, belongs to the chymase family and shares their functions in the angiogenetic process. Chymases act as extracellular matrix degrading enzymes, either by themselves or by the activation of metalloproteinases (Johnson et al., 1998), facilitating in this way the advance of blood vessels. Particularly, we have previously demonstrated that, by blocking rMCP-5 with an antisense oligonucleotide, specific for this chymase, it was possible to prevent angiogenesis during granuloma formation (Russo et al., 2005).
The evidence that cannabinoids affect MC was further strengthened by the ability of ACEA and JWH-015 to reduce, following λ-carrageenin treatment, the expression of NGF, another important mediator synthesized and released by MC. In the experiments presented here, we were not able to investigate, in more detail, the possibility that the decrease in rMCP-5 and NGF levels was related to the decline in total MC number. Our results suggest that cannabinoids, by controlling MC function, may prevent, at least in part, granuloma-associated angiogenesis. Here, we have shown that selective CB1 and CB2 agonists significantly reduced new vessel formation, both by histological analysis and by the measurement of the Hb content in the tissue. Moreover these results are compatible with our previous work demonstrating pro-angiogenic effects of CB1 and CB2 receptor antagonists, in the same model (De Filippis et al., 2007).
In conclusion, all the data reported here indicate that ACEA and JWH-015 exhibit antiangiogenic properties, as they were able to decrease neovascularization in the granulomas, correlated with a reduction in MC number and in MC granule-derived mediators (rMCP-5 and NGF), without affecting the degranulation responses (hexosaminidase release). From our results, we would propose a mechanism for the antiangiogenic effects of cannabinoids in granulomas, which could include the effects on NF-κB activation, previously demonstrated by us (De Filippis et al., 2007), recognizing for the first time MCs as an important cellular target of CB effects in our model.
Abbreviations
- ACEA
arachidonyl-2′-chloroethylamide
- Hb
haemoglobin
- JWH-015
2-methyl-1-propyl-1H-indol-3-yl)-1-naphthalenylmethanone
- MC
mast cell
- NGF
nerve growth factor
- rMCP-5
rat mast cell protease-5
- WIN 55,212-2, (R)-(+)-[2,3-dihydro-5-methyl-3-(4-morpholinylmethyl) pyrrolo[1,2,3-de]-1
4-benzoxazin-6-yl] -1-naphthalenylmethanone mesylate
Conflict of interest
The authors state no conflict of interest.
References
- Alexander SPH, Mathie A, Peters JA.Guide to receptors and channels (GRAC) Br J Pharmacol 2008153Suppl 2S1–S209.3rd edn [DOI] [PMC free article] [PubMed] [Google Scholar]
- Augustin HG, Braun K, Telemenakis I, Modlich U, Kuhn W. Ovarian angiogenesis. Phenotypic characterization of endothelial cells in a physiological model of blood vessel growth and regression. Am J Pathol. 1995;147:339–351. [PMC free article] [PubMed] [Google Scholar]
- Bisogno T, Ligresti A, Di Marzo V. The endocannabinoid signalling system: biochemical aspects. Pharmacol Biochem Behav. 2005;81:224–238. doi: 10.1016/j.pbb.2005.01.027. [DOI] [PubMed] [Google Scholar]
- Blazquez C, Casanova ML, Planas A, Del Pulgar TG, Villanueva C, Fernandez-Acenero MJ, et al. Inhibition of tumor angiogenesis by cannabinoids. FASEB J. 2003;17:529–531. doi: 10.1096/fj.02-0795fje. [DOI] [PubMed] [Google Scholar]
- Blázquez C, González-Feria L, Alvarez L, Haro A, Casanova ML, Guzmán M. Cannabinoids inhibit the vascular endothelial growth factor pathway in gliomas. Cancer Res. 2004;64:5617–5623. doi: 10.1158/0008-5472.CAN-03-3927. [DOI] [PubMed] [Google Scholar]
- Casanova ML, Blazquez C, Martinez-Palacio J, Villanueva C, Fernandez-Acenero MJ, Huffman JW, et al. Inhibition of skin tumor growth and angiogenesis in vivo by activation of cannabinoid receptors. J Clin Invest. 2003;111:43–50. doi: 10.1172/JCI16116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coëffier M, Le Pessot F, Leplingard A, Marion R, Lerebours E, Ducrotté P, et al. Acute enteral glutamine infusion enhances heme oxygenase-1 expression in human duodenal mucosa. J Nutr. 2002;132:2570–2573. doi: 10.1093/jn/132.9.2570. [DOI] [PubMed] [Google Scholar]
- Colville-Nash PR, Alam CA, Appleton I, Brown JR, Seed MP, Willoughby DA. The pharmacological modulation of angiogenesis in chronic granulomatous inflammation. J Pharmacol Exp Ther. 1995;274:1463–1472. [PubMed] [Google Scholar]
- Coussens LM, Raymond WW, Bergers G, Laig-Webster M, Behrendtsen O, Werb Z, et al. Inflammatory mast cells up-regulate angiogenesis during squamous epithelial carcinogenesis. Genes Dev. 1999;13:1382–1397. doi: 10.1101/gad.13.11.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croxford JL, Yamamura T. Cannabinoids and the immune system: potential for the treatment of inflammatory diseases. J Neuroimmunol. 2005;166:3–18. doi: 10.1016/j.jneuroim.2005.04.023. [DOI] [PubMed] [Google Scholar]
- De Filippis D, Russo A, De Stefano D, Maiuri MC, Esposito G, Cinelli MP, et al. Local administration of WIN 55,212-2 reduces chronic granuloma-associated angiogenesis in rat by inhibiting NF-kappa B activation. J Mol Med. 2007;85:635–645. doi: 10.1007/s00109-007-0188-z. [DOI] [PubMed] [Google Scholar]
- De Filippis D, D'Amico A, Iuvone T. Cannabimimetic control of mast cell mediator release: new perspective in chronic inflammation. J Neurol Endocrinol. 2008;80:20–25. doi: 10.1111/j.1365-2826.2008.01674.x. [DOI] [PubMed] [Google Scholar]
- Facci L, Dal Toso R, Romanello S, Buriani A, Skaper SD, Leon A. Mast cells express a peripheral cannabinoid receptor with differential sensitivity to anandamide and palmitoylethanolamide. Proc Natl Acad Sci USA. 1995;92:3376–3380. doi: 10.1073/pnas.92.8.3376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folkman J.Angiogenesis in cancer vascular, rheumatoid and other disease Nat Med 1995127–31.Review [DOI] [PubMed] [Google Scholar]
- Forehand JR, Johnston RB., Jr Chronic granulomatous disease: newly defined molecular abnormalities explain disease variability and normal phagocyte physiology. Curr Opin Pediatr. 1994;6:668–675. [PubMed] [Google Scholar]
- Hernandez-Hansen V, Smith AJ, Surviladze Z, Chigaev A, Mazel T, Kalesnikoff J, et al. Dysregulated FcepsilonRI signaling and altered Fyn and SHIP activities in Lyn-deficient mast cells. J Immunol. 2004;173:100–112. doi: 10.4049/jimmunol.173.1.100. [DOI] [PubMed] [Google Scholar]
- Hart IR. Role of integrins in tumor invasion and metastasis. Exp Dermatol. 2004;13:663. doi: 10.1111/j.0906-6705.2004.0250g.x. [DOI] [PubMed] [Google Scholar]
- Hunt TK, Knighton DR, Thakral KK, Goodson WH, III, Andrews WS. Studies on inflammation and wound healing: angiogenesis and collagen synthesis stimulated in vivo by resident and activated wound macrophages. Surgery. 1984;96:48–54. [PubMed] [Google Scholar]
- Iuvone T, Den Bossche RV, D'Acquisto F, Carnuccio R, Herman AG. Evidence that mast cell degranulation, histamine and tumour necrosis factor alpha release occur in LPS-induced plasma leakage in rat skin. Br J Pharmacol. 1999;128:700–704. doi: 10.1038/sj.bjp.0702828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iuvone T, De Filippis D, Di Spiezio Sardo A, D'Amico A, Simonetti S, Insabato L, et al. Selective CB2 up-regulation in women affected by endometrial inflammation. J Cell Mol Med. 2007;12:661–670. doi: 10.1111/j.1582-4934.2007.00085.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JL, Jackson CL, Angelini GD, George SJ. Activation of matrix-degrading metalloproteinases by mast cell proteases in atherosclerotic plaques. Arterioscler Thromb Vasc Biol. 1998;18:1707–1715. doi: 10.1161/01.atv.18.11.1707. [DOI] [PubMed] [Google Scholar]
- Kähäri VM, Saarialho-Kere U.Matrix metalloproteinases in skin Exp Dermatol 19976199–213.Review [DOI] [PubMed] [Google Scholar]
- Kogan NM, Blázquez C, Alvarez L, Gallily R, Schlesinger M, Guzmán M, et al. A cannabinoid quinone inhibits angiogenesis by targeting vascular endothelial cells. Mol Pharmacol. 2006;70:51–59. doi: 10.1124/mol.105.021089. [DOI] [PubMed] [Google Scholar]
- Lage AP, Andrade SP. Assessment of angiogenesis and tumor growth in conscious mice by a fluorimetric method. Microvasc Res. 2000;59:278–285. doi: 10.1006/mvre.1999.2217. [DOI] [PubMed] [Google Scholar]
- Lutzelschwab C, Pejler G, Aveskogh M, Hellman L. Secretory granule proteases in rat mast cells Cloning of 10 different serine proteases and a carboxypeptidase A from various rat mast cell populations. J Exp Med. 1997;185:13–29. doi: 10.1084/jem.185.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone JM, Jr, Gershenson DM, Carrasco CH, Charansangavej C, Copeland LJ, Larson DM, et al. Intrahepatic infusional therapy for metastatic ovarian carcinoma. Cancer. 1987;59:1866–1869. doi: 10.1002/1097-0142(19870601)59:11<1866::aid-cncr2820591104>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Matias I, Pochard P, Orlando P, Salzet M, Pestel J, Di Marzo V. Presence and regulation of the endocannabinoid system in human dendritic cells. Eur J Biochem. 2002;269:3771–3778. doi: 10.1046/j.1432-1033.2002.03078.x. [DOI] [PubMed] [Google Scholar]
- Metcalfe DD, Baram D, Mekori YA.Mast cells Physiol Rev 1997771033–1079.Review [DOI] [PubMed] [Google Scholar]
- Mohamed Q, Gillies MC, Wong TY.Management of diabetic retinopathy: a systematic review JAMA 2007298902–916.Review [DOI] [PubMed] [Google Scholar]
- Mullane KM, Kraemer R, Smith B. Myeloperoxidase activity as a quantitative assessment of neutrophil infiltration into ischemic myocardium. J Pharmacol Methods. 1985;14:157–167. doi: 10.1016/0160-5402(85)90029-4. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. Evidence for the presence of CB1 cannabinoid receptors on peripheral neurones and for the existence of neuronal non-CB1 cannabinoid receptors. Life Sci. 1999;65:597–605. doi: 10.1016/s0024-3205(99)00282-9. [DOI] [PubMed] [Google Scholar]
- Reynolds DS, Stevens RL, Lane WS, Carr MH, Austen KF, Serafin WE. Different mouse mast cell populations express various combinations of at least six distinct mast cell serine proteases. Proc Natl Acad Sci USA. 1990;87:3230–3234. doi: 10.1073/pnas.87.8.3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo A, Russo G, Peticca M, Pietropaolo C, Di Rosa M, Iuvone T. Inhibition of granuloma-associated angiogenesis by controlling mast cell mediator release: role of mast cell protease-5. Br J Pharmacol. 2005;145:24–33. doi: 10.1038/sj.bjp.0706112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samson MT, Small-Howard A, Shimoda LM, Koblan-Huberson M, Stokes AJ, Turner HJ. Differential roles of CB1 and CB2 cannabinoid receptors in mast cells. Immunol. 2003;170:4953–4962. doi: 10.4049/jimmunol.170.10.4953. [DOI] [PubMed] [Google Scholar]
- Takai S, Shiota N, Kobayashi S, Matsumura E, Miyazaki M. Induction of chymase that forms angiotensin II in the monkey atherosclerotic aorta. FEBS Lett. 1997;412:86–90. doi: 10.1016/s0014-5793(97)00752-7. [DOI] [PubMed] [Google Scholar]
- Toda S, Tokuda Y, Koike N, Yonemitsu N, Watanabe K, Koike K, et al. Growth factor-expressing mast cells accumulate at the thyroid tissue-regenerative site of subacute thyroiditis. Thyroid. 2000;10:381–386. doi: 10.1089/thy.2000.10.381. [DOI] [PubMed] [Google Scholar]
- Tozzi CA, Thakker-Varia S, Yu SY, Bannett RF, Peng BW, Poiani GJ, et al. Mast cell collagenase correlates with regression of pulmonary vascular remodeling in the rat. Am J Respir Cell Mol Biol. 1998;18:497–510. doi: 10.1165/ajrcmb.18.4.2536. [DOI] [PubMed] [Google Scholar]
- Trabucchi E, Radaelli E, Marazzi M, Foschi D, Musazzi M, Veronesi AM, et al. The role of mast cells in wound healing Int J Tissue React 198810367–372.Review [PubMed] [Google Scholar]
- Vannacci A, Giannini L, Passani MB, Di Felice A, Pierpaoli S, Zagli G, et al. The endocannabinoid 2-arachidonylglycerol decreases the immunological activation of Guinea pig mast cells: involvement of nitric oxide and eicosanoids. J Pharmacol Exp Ther. 2004;311:256–264. doi: 10.1124/jpet.104.068635. [DOI] [PubMed] [Google Scholar]
- Velez-Pardo C, Del Rio MJ. Avoidance of Abeta[(25-35)]/(H(2)O(2)) -induced apoptosis in lymphocytes by the cannabinoid agonists CP55,940 and JWH-015 via receptor-independent and PI3K-dependent mechanisms: role of NF-kappaB and p53. Med Chem. 2006;2:471–479. doi: 10.2174/157340606778250171. [DOI] [PubMed] [Google Scholar]
- Wintroub BU, Schechter NB, Lazarus GS, Kaempfer CE, Schwartz LB. Angiotensin I conversion by human and rat chymotryptic proteinases. J Invest Dermatol. 1984;83:336–339. doi: 10.1111/1523-1747.ep12264144. [DOI] [PubMed] [Google Scholar]