Abstract
OBJECTIVE—Hypoglycemia commonly occurs in intensively-treated diabetic patients. Repeated hypoglycemia blunts counterregulatory responses, thereby increasing the risk for further hypoglycemic events. Currently, physiologic approaches to augment counterregulatory responses to hypoglycemia have not been established. Therefore, the specific aim of this study was to test the hypothesis that 6 weeks’ administration of the selective serotonin reuptake inhibitor (SSRI) fluoxetine would amplify autonomic nervous system (ANS) and neuroendocrine counterregulatory mechanisms during hypoglycemia.
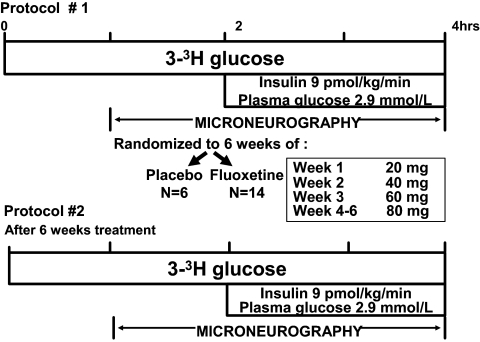
RESEARCH DESIGN AND METHODS—A total of 20 healthy (10 male and 10 female) subjects participated in an initial single-step hyperinsulinemic (9 pmol · kg−1 · min−1)-hypoglycemic (means ± SE 2.9 ± 0.1 mmol/l) clamp study and were then randomized to receive 6 weeks’ administration of fluoxetine (n = 14) or identical placebo (n = 6) in a double-blind fashion. After 6 weeks, subjects returned for a second hypoglycemic clamp. Glucose kinetics were determined by three-tritiated glucose, and muscle sympathetic nerve activity (MSNA) was measured by microneurography.
RESULTS—Despite identical hypoglycemia (2.9 ± 0.1 mmol/l) and insulinemia during all clamp studies, key ANS (epinephrine, norepinephrine, and MSNA but not symptoms), neuroendocrine (cortisol), and metabolic (endogenous glucose production, glycogenolysis, and lipolysis) responses were increased (P < 0.01) following fluoxetine.
CONCLUSIONS—This study demonstrated that 6 weeks’ administration of the SSRI fluoxetine can amplify a wide spectrum of ANS and metabolic counterregulatory responses during hypoglycemia in healthy individuals. These data further suggest that serotonergic transmission may be an important mechanism in modulating sympathetic nervous system drive during hypoglycemia in healthy individuals.
Several reports have indicated that fluoxetine could have metabolic effects and influence carbohydrate metabolism (1–3). In fact, there have been three case studies reporting the occurrence of hypoglycemia related to the use of selective serotonin reuptake inhibitors (SSRIs) in depressed patients with and without diabetes (4–6). However, although SSRIs are potent inhibitors of neuronal serotonin uptake, they also have the ability to block norepinephrine transport (7). This could increase sympathetic outflow activity (2,8). Baudrie and Chaouloff (9) have previously reported an increased hyperglycemic response to 2-deoxy-d-glycose in conscious rats following serotononergic receptor antagonists, implying increased counterregulation in these animals.
A subsequent study by Perry and Fuller (2) demonstrated that systemic injection of the SSRI fluoxetine in rats resulted in threefold increases of hypothalamic norepinephrine release, thereby providing a mechanistic basis for SSRIs to modulate sympathetic nervous system activity. A later study by Bymaster et al. (3) examined the specificity of five different SSRIs (fluoxetine, citalopram, fluvoxamine, paroxetine, and sertraline) to acutely increase the extracellular concentration of serotonin and norepinephrine in rat forebrains. The study demonstrated that among the SSRIs examined, only fluoxetine increased extracellular concentrations of both norepinephrine and serotonin in the rat brains and suggested that fluoxetine may have differential effects compared with other SSRIs.
Thus, previous information from depressed humans and physiologic data from healthy rats have provided conflicting data concerning possible effects of SSRIs on counterregulatory mechanisms. In addition, despite the widespread clinical use of SSRIs, there have been no clinical studies evaluating the effects of prolonged administration of these agents on counterregulatory responses during clamped hyperinsulinemic hypoglycemia. In the present study, fluoxetine was chosen based on the drug's frequent use in clinical practice and data demonstrating physiologic effects on both serotonergic and norepinephrine transport in rats. The hypoglycemic clamp technique was used to quantify autonomic nervous system (ANS), neuroendocrine, and metabolic counterregulatory mechanisms prospectively before and after 6 weeks’ administration of fluoxetine in healthy nondepressed individuals.
RESEARCH DESIGN AND METHODS
A total of 20 healthy volunteers (10 male and 10 female) of mean ± SE age 29 ± 2 years (range 20–44) with a BMI of 24 ± 3 kg/m2 and A1C of 5.3 ± 0.1% (normal range 4–6.5%) were studied. The Zung Self-Rating Depression Scale (10,11) was completed by each subject to rule out symptoms of clinical depression. None had a history of epilepsy or any major psychiatric illness. None were taking any psychotropic medication. Each subject had normal blood count, plasma electrolytes, and liver and renal function. Three subjects had a family history of diabetes. All gave written informed consent. Hypoglycemia (2.9 mmol/l) and euglycemia (∼5.0 mmol/l) studies were approved by the Vanderbilt University Human Subjects Institutional Review Board.
Experimental design.
The subjects (n = 20) participated in two separate hypoglycemia studies separated by at least 6 weeks (Fig. 1). Subjects received the study medication (n = 14; 7 male and 7 female) or placebo (n = 6; 3 male and 3 female) in a randomized, double-blind fashion after completion of their first clamp study.
FIG. 1.
Schematic diagram of experimental protocol.
The subjects were asked to avoid any exercise and consume their usual weight-maintaining diet for 3 days before each study. Each subject was admitted to the Vanderbilt General Clinical Research Center on the evening before an experiment. All subjects were studied after an overnight 10-h fast.
On the morning of each study, two intravenous cannulae were inserted under 1% lidocaine local anesthesia. One cannula was placed in a retrograde fashion into a vein on the back of the hand. This hand was placed in a heated box (55–60°C) so that arterialized blood could be obtained (12). The other cannula was placed in a large vein in the contralateral arm so that 20% glucose could be infused via a variable rate volumetric infusion pump (Imed, -San Diego, CA).
Hypoglycemia experiments.
After insertion of venous cannulae, at 0 min, a primed (18 μCi) continuous infusion (0.18 μCi/min) of high-performance liquid chromatography (HPLC) purified [3-3H] glucose (11.5 mCi · mmol−1 · l−1; Perkin Elmer Life Sciences, Boston, MA) was started. At time 120 min, a primed constant (9.0 pmol · kg−1 · min−1) infusion of insulin (Eli Lilly, Indianapolis, IN) was started and continued until 240 min. The rate of fall of glucose was controlled (0.06 mmol/min) and the glucose nadir (2.9 mmol/l) was achieved using a modification of the glucose clamp technique (13,14). Potassium chloride (20 mmol/l) was infused during the clamp to reduce insulin-induced hypokalemia. A second identical hyperinsulinemic-hypoglycemic clamp was performed after receiving 6 weeks ’ administration of study medication.
Study medication.
Following the initial clamp study, volunteers were given either fluoxetine or placebo for 6 weeks. The fluoxetine dose was as follows: 20 mg/day during week 1, 40 mg/day during week 2, 60 mg/day during week 3, and 80 mg/day during weeks 4–6. Volunteers were blinded as to the treatment group to which they were assigned. Stratified block randomization was performed by the Vanderbilt University Investigational Pharmacy. The subjects were stratified according to sex because sex is known to affect counterregulatory responses (15). Randomization was performed within each sex, and blocks of two were used to ensure an equal number of male and female subjects in the placebo and fluoxetine treatment groups. The study was powered at n = 14 for the fluoxetine group. When we reached this total, it became obvious that there were clear statistical differences between the groups, and it was not necessary to study additional placebo subjects. The placebo group was used primarily as a time control to demonstrate that counterregulatory responses to hypoglycemia in our normal subjects had not changed during the 6-week study period or that involvement in the experimental protocol did not influence physiologic responses to hypoglycemia.
During the 6-week treatment period, volunteers came to the Vanderbilt General Clinical Research Center once a week for monitoring of compliance and adverse events. Compliance was determined via a pill count and a blood draw to measure serum fluoxetine levels. One subject in the placebo group withdrew from the study because of perceived side effects of the treatment. After taking either placebo or fluoxetine for 6 weeks, subjects underwent another single-day hypoglycemic clamp study as previously described. Upon completion of this second 1-day study, subjects were tapered off the study medication (placebo or fluoxetine). Those randomized to fluoxetine received 40 mg/day for 1 week and 20 mg/day for a second week. Once subjects finished the medication, they were unblinded to the medication they had taken.
Direct measurement of muscle sympathetic nerve activity.
Muscle sympathetic nerve activity (MSNA) was recorded from the peroneal nerve at the level of the fibular head and popliteal fossa (16,17). The approximate location of this nerve was determined by transdermal electrical stimulation to produce painless muscle contraction of the foot. Following this, a reference stainless steel microelectrode with a shaft diameter of 200 μm was placed subcutaneously. A similar tungsten electrode, with an uninsulated tip, was inserted into the nerve and used for recording of MSNA.
Nerve activity was recorded on a PC-based Windaq data acquisition system at 1,000 H2Z channel−1 (DATAQ Instruments, Akron, OH). We analyzed 5-min Windaq files with a MatLab GUIDE interface (to adjust for an individual's 1.3-s nerve burst delay from a 1-removed R-R interval, automatically detected by pulse synchronicity, a 2:1 signal-to-noise ratio, and wave-form shape). Further criteria for acceptable MSNA recordings were the following: 1) electrical stimulation produced muscle twitches but not paresthesia, 2) nerve activity increased during phase II of the Valsalva maneuver (hypotensive phase) and was suppressed during phase IV (blood pressure overshoot), and 3) nerve activity increased in response to held expiration.
Tracer calculations.
Rates of glucose appearance (Ra), endogenous glucose production (EGP), and glucose utilization were calculated according to the methods of Wall et al. (18). EGP was calculated by determining the total Ra (comprising both EGP and any exogenous glucose infused to maintain the desired hypoglycemia) and subtracting it from the amount of exogenous glucose infused. It is now recognized that this approach is not fully quantitative because underestimates of total Ra and rate of glucose disposal (Rd) can be obtained. The use of a highly purified tracer and taking measurements under steady-state conditions (i.e., constant specific activity) in the presence of low glucose flux eliminate most, if not all, of the problems. In addition, to maintain a constant specific activity, isotope delivery was increased commensurate with increases in exogenous glucose infusion. During these studies, only glucose flux results from the steady-state basal and the final 30-min periods of the hypoglycemic clamps are reported.
Analytical methods.
Plasma glucose concentrations were measured in triplicate using the glucose oxidase method with a glucose analyzer (Beckman, Fullerton, CA). Glucagon and insulin were measured as previously described (19,20) with an interassay coefficients of variation (CVs) of 12 and 9%, respectively. Catecholamines were determined by HPLC (21) with an interassay CV of 12% for epinephrine and 8% for norepinephrine. Cortisol was assayed using the Clinical Assays Gamma Coat Radioimmunoassay kit with an interassay CV of 6%. Growth hormone and pancreatic polypeptide levels were determined by radioimmunoassay (22,23) with CVs of 8.6 and 8.0%, respectively. Lactate, glycerol, alanine, and β-hydroxybutyrate were measured in deproteinized whole blood using the method of Lloyd et al. (24). Nonesterified fatty acids (NEFAs) were measured using the WAKO kit adopted for use on a centrifugal analyzer (25). A1C was determined in whole blood using the Variant II A1C cation-exchange HPLC kit system (26). Fluoxetine and norfluoxetine were determined by gas chromatography with electron-capture detection based on a modification described by Torok-Both et al. (27).
Blood was drawn for hormones and intermediary metabolites twice during the control period and every 15 min during the experimental period. Cardiovascular parameters (pulse, systolic blood pressure, diastolic blood pressure, and mean arterial pressure) were measured noninvasively by a Dinamap (Critikon, Tampa, FL) every 10 min throughout each study.
Hypoglycemic symptoms were quantified using a previously validated questionnaire using the model of Deary et al. (28). Each individual was asked to rate his/her experience of the symptoms twice during the control period and every 15 min during experimental periods.
Statistical analysis.
Data are expressed as means ± SE and were analyzed using standard, parametric, and one- and two-way ANOVA and with repeated measures where appropriate (SigmaStat; SPSS Science, Chicago, IL). Tukey's post hoc analysis was used to delineate statistical significance across time within each group and for each group compared with the control group. A P value of <0.05 was accepted as statistically significant. Baseline hypoglycemic clamp data represent an average of time points (110 and 120 min), and the final 30-min data from each clamp represent an average of three measurements at 210, 225, and 240 min.
Materials.
HPLC-purified [3-3H] glucose (New England Nuclear, Boston, MA) was used as the glucose tracer (11.5 mCi · mmol−1 · l−1). Human regular insulin was purchased from Eli Lilly (Indianapolis, IN).
RESULTS
Glucose, insulin, and fluoxetine levels.
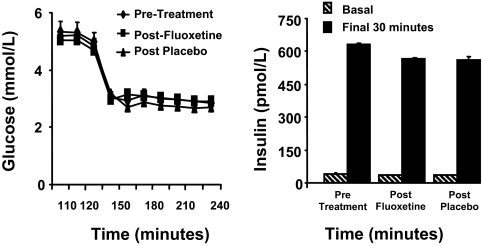
Basal plasma glucose levels were 5.3 ± 0.2 mmol/l during the prefluoxetine study and 5.1 ± 0.06 mmol/l during the postfluoxetine study. Weight was unchanged during both the 6-week fluoxetine (71.1 ± 3.3 to 70.0 ± 3.2 kg) and placebo (74.5 ± 6.1 to 74.8 ± 5.4 kg) studies. Plasma glucose levels reached steady state by 30 min, and identical hypoglycemia was maintained with plasma glucose levels of 2.9 + 0.05 mmol/l during clamp procedures for all study groups (Fig. 2). Basal and steady-state insulin levels for both fluoxetine and placebo groups were similar during both pretreatment (43 ± 6 and 631 ± 30 pmol/l, respectively) and postfluoxetine and -placebo (37 ± 6 and 567 ± 30 pmol/l; 35 ± 12 and 559 ± 78 pmol/l, respectively) clamp studies (Fig. 2). Mean fluoxetine and norfluoxetine levels at the end of the study were 336.7 ± 61 and 230 ± 41 ng/ml, respectively, in the SSRI group and were undetectable in the placebo group.
FIG. 2.
Plasma glucose and insulin concentrations (means ± SE) during hypoglycemic clamp studies in 20 (10 male and 10 female) nondiabetic patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo.
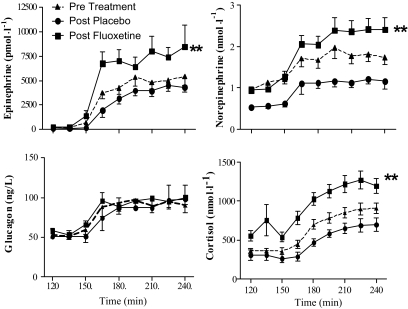
Neuroendocrine counterregulatory hormones.
Epinephrine responses were significantly higher (8,187 ± 1,365 pmol/l; P < 0.001) during the final 30 min of hypoglycemia postfluoxetine compared with those pretreatment (5,065 ± 797 pmol/l) and following placebo (4,366 ± 508 pmol/l). Epinephrine responses were similar (4,366 ± 508 vs. 5,065 ± 797 pmol/l) during the final 30 min postplacebo compared with those associated with pretreatment hypoglycemic clamps (Fig. 3).
FIG. 3.
Plasma epinephrine and norepinephrine levels (means ± SE) during hyperinsulinemic-hypoglycemic (2.9 ± 0.1 mmol/l) clamp studies in 20 (10 male and 10 female) patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo. Plasma epinephrine and norepinephrine levels were significantly increased (P < 0.01) following fluoxetine compared with pretreatment and placebo values. Plasma glucagon and cortisol levels (means ± SE) during hyperinsulinemic-hypoglycemic (2.9 ± 0.1 mmol/l) clamp studies in 20 (10 male and 10 female) patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo. Plasma cortisol levels are significantly increased (P < 0.01) following fluoxetine administration.
Norepinephrine responses were significantly higher (2.4 ± 0.2 nmol/l) during the final 30 min of postfluoxetine as compared with those measured during the pretreatment (1.8 ± 0.2 nmol/l) and placebo (1.2 ± 0.1 nmol/l) (P < 0.01) hypoglycemic clamps. Norepinephrine responses during hypoglycemia following placebo were similar to pretreatment values and significantly reduced compared with those of the fluoxetine group (Fig. 3).
Basal cortisol levels were significantly increased (P < 0.05) in the fluoxetine group (552 ± 55 nmol/l) compared with those in the pretreatment and placebo groups (359 ± 27 and 304 ± 55 nmol/l, respectively). Plasma cortisol responses were also significantly higher (1,242 ± 110 and 883 ± 55 nmol/l; P < 0.01) during the final 30 min of postfluoxetine versus pretreatment and following placebo (678 ± 79 nmol/l). However, no significant differences occurred in the placebo group (Fig. 3).
Peak pancreatic polypeptide levels during hypoglycemia increased to 214 ± 54 nmol/lafter fluoxetine administration compared with pretreatment values (149 ± 22 nmol/l) (P < 0.06). Pancreatic polypeptide levels during the final 30 min of hypoglycemia postfluoxetine were significantly increased compared with postplacebo values (165 ± 19 vs. 122 ± 17 nmol/l, respectively; P < 0.01).
Glucagon responses were similar during hypoglycemia in all groups (postfluoxetine or postplacebo) (Fig. 3). Fluoxetine had no effect on growth hormone responses during hypoglycemia. Growth hormone increased from 2 ± 1 to 28 ± 6 ng/l pretreatment, 2 ± 1 to 29 ± 7 ng/l posttreatment, and 2.5 ± 1 to 21 ± 7 ng/l during placebo.
Glucose kinetics.
Glucose specific activity (disintegrations per minute per milligram) was in a steady state during the basal period and the final 30 min of all hyperinsulinemic-hypoglycemic clamps (Table 1). During the final 30 min of hypoglycemia, exogenous glucose infusion rates were significantly less in the fluoxetine group (posttreatment 1.1 ± 0.5 μmol · kg−1 · min−1 vs. both prefluoxetine 3.1 ± 1.1 and postplacebo 5.5 ± 1.7 μmol · kg−1 · min−1; P < 0.01). For the placebo group, exogenous glucose infusion rates were not significantly changed (pretreatment 3.3 ± 1.1 vs. postplacebo 5.5 ± 1.7 μmol · kg−1 · min−1). The EGP response in postfluoxetine (14 ± 1.1 μmol · kg−1 · min−1) was significantly increased (P < 0.01) compared with both pretreatment (10.3 ± 1.1) and postplacebo (9 ± 1.1 μmol · kg−1 · min−1) levels. The EGP in the postplacebo group was similar to that pretreatment 9 ± 1.1 vs. 10.3 ± 1.1 μmol · kg−1 · min−1. The Rd during the final 30 min of hypoglycemia was not significantly changed as a result of receiving 6 weeks ’ administration of fluoxetine (Fig. 4).
TABLE 1.
Glucose specific activity (dpm/mmol) during the basal period and the final 30 min of all hyperinsulinemic-hypoglycemic clamps in nondiabetic individuals before and after 6 weeks of fluoxetine treatment or placebo
| −20 min | −10 min | 0 min | 90 min | 105 min | 120 min | |
|---|---|---|---|---|---|---|
| Pretreatment | 432 ± 21 | 428 ± 22 | 417 ± 18 | 257 ± 18 | 254 ± 17 | 254 ± 16 |
| Postfluoxetine | 443 ± 20 | 452 ± 20 | 437 ± 21 | 279 ± 23 | 286 ± 27 | 277 ± 24 |
| Postplacebo | 408 ± 36 | 415 ± 38 | 401 ± 38 | 234 ± 22 | 219 ± 18 | 216 ± 16 |
Data are means ± SD.
FIG. 4.
Glucose kinetics during the basal period and the final 30 min of hyperinsulinemic-hypoglycemic (2.9 ± 0.1 mmol/l) clamp studies in 20 (10 male and 10 female) patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo. EGP was increased and glucose infusion rates were reduced (P < 0.01) following fluoxetine administration. Data are means ± SE.
 , basal. ▪, final 30 min.
, basal. ▪, final 30 min.
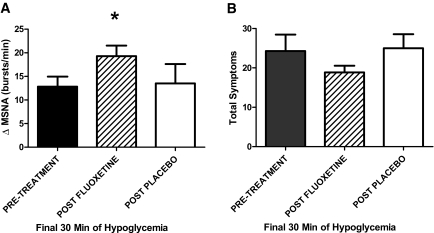
MSNA.
MSNA increased by a significantly greater amount (P < 0.05) during hypoglycemia in the postfluoxetine group (19 ± 3 bursts/min) compared with both pretreatment (13 ± 3 bursts/min) and postplacebo (14 ± 3 bursts/min) groups. There were no differences in the postplacebo versus pretreatment groups (14 ± 3 vs. 13 ± 3 bursts/min, respectively).
Intermediary metabolism.
Baseline glycerol, lactate, β-hydroxybutyrate, NEFA, and alanine levels were similar among the groups (Table 2). The increase in glycerol during hypoglycemia (19 ± 4 μmol/l) was significantly greater (P < 0.05) following fluoxetine compared with pretreatment (12 ± 3 μmol/l) or postplacebo (10 ± 2 μmol/l values. There was no difference in the increase of glycerol during hypoglycemia in the placebo group.
TABLE 2.
Plasma glycerol, lactate, ß-hydroxybutyrate, NEFA, and alanine levels during the basal period and the final 30 min of hyperinsulinemic-hypoglycemic clamp studies in nondiabetic individualsbefore and after 6 weeks of fluoxetine treatment or placebo
| Basal period | Final 30 min | |
|---|---|---|
| Glycerol (mmol/l) | ||
| Pretreatment | 50 ± 3 | 62 ± 6 |
| Postfluoxetine | 64 ± 9 | 82 ± 11* |
| Postplacebo | 90 ± 21 | 100 ± 23 |
| Lactate (mmol/l) | ||
| Pretreatment | 0.5 ± 0.07 | 1.3 ± 0.08 |
| Postfluoxetine | 0.6 ± 0.09 | 1.8 ± 0.2* |
| Postplacebo | 0.5 ± 0.13 | 1.1 ± 0.09 |
| ß-Hydroxybutyrate (μmol/l) | ||
| Pretreatment | 0.03 ± 0.01 | 0.015 ± 0.01 |
| Postfluoxetine | 0.06 ± 0.02 | 0.027 ± 0.01* |
| Postplacebo | 0.095 ± 0.04 | 0.017 ± 0.01 |
| NEFA (μmol/l) | ||
| Pretreatment | 390 ± 53 | 114 ± 13 |
| Postfluoxetine | 332 ± 45 | 141 ± 22 |
| Postplacebo | 308 ± 87 | 95 ± 20 |
| Alanine (μmol/l) | ||
| Pretreatment | 0.22 ± 0.03 | 0.21 ± 0.01 |
| Postfluoxetine | 0.24 ± 0.02 | 0.24 ± 0.02 |
| Postplacebo | 0.26 ± 0.05 | 0.24 ± 0.03 |
Data are means ± SE.
A significantly increased response during the final 30 min of hypoglycemia following 6 weeks of fluoxetine administration (*P < 0.05).
Blood lactate was significantly increased during the final 30 min of hypoglycemia in the postfluoxetine group versus pretreatment and placebo groups (1.8 ± 0.2 vs. 1.3 ± 0.08 and 1.1 ± 0.1 mmol/l, respectively; P < 0.05). No significant changes occurred in the control group (postplacebo 1.1 ± 0.09 vs. pretreatment 1.3 ± 0.08 mmol/l).
β-Hydroxybutyrate levels were also significantly higher in the postfluoxetine group versus pretreatment and placebo groups (0.27 ± 0.01 vs. 0.015 ± 0.01 and 0.017 ± 0.01mmol/l, respectively; P < 0.05). No differences occurred in the pre- and postplacebo group (0.015 ± 0.01 vs. 0.017 ± 0.01 mmol/l, respectively). There was a trend for a greater reduction in NEFA levels during pretreatment (276 ± 40 as compared with postfluoxetine 192 ± 25; P = 0.069).
Cardiovascular parameters.
Basal heart rate and blood pressure were not different after 6 weeks’ administration of fluoxetine. Heart rate was significantly higher during the final 30 min of postfluoxetine compared with that in the pretreatment and placebo groups (79 ± 6 vs. 69 ± 3 and 70 ± 5 bpm, respectively; P < 0.05). No significant differences in heart rate were noted for the control group (70 ± 5 postplacebo vs. 69 ± 3 bpm pretreatment). Systolic blood pressure was also significantly increased during hypoglycemia in the postfluoxetine group versus the pretreatment and placebo groups (129 ± 6 vs. 121 ± 5 and 118 ± 6 mmHg, respectively; P < 0.05). There were no differences in the increase of systolic blood pressure in the placebo group (118 ± 6 vs. 121 ± 5 mmHg). No significant changes in diastolic blood pressure occurred in the experimental or placebo groups (Table 3).
TABLE 3.
Cardiovascular responses during hyperinsulinemic-hypoglycemic clamp studies in nondiabetic individuals before and after 6 weeks of fluoxetine or placebo
| Basal period | Final 30 min | |
|---|---|---|
| Heart rate (beats/min) | ||
| Pretreatment | 62 ± 3 | 69 ± 3 |
| Postfluoxetine | 62 ± 4 | 79 ± 6* |
| Postplacebo | 59 ± 4 | 70 ± 5 |
| Systolic blood pressure (mmHg) | ||
| Pretreatment | 116 ± 3 | 121 ± 5 |
| Postfluoxetine | 115 ± 4 | 129 ± 6* |
| Postplacebo | 111 ± 6 | 118 ± 6 |
| Diastolic blood pressure (mmHg) | ||
| Pretreatment | 67 ± 2 | 61 ± 2 |
| Postfluoxetine | 69 ± 2 | 65 ± 2 |
| Postplacebo | 63 ± 2 | 59 ± 4 |
Data are means ± SE.
Significantly increased response during the final 30 min of hypoglycemia following 6 weeks of fluoxetine administration (*P < 0.05).
Symptom response.
There were no differences in total symptom scores in the fluoxetine group compared with either the pretreatment or control groups (autonomic symptoms 10 ± 2 pretreatment vs. 8 ± 1 posttreatment; neuroglycopenic scores 14 ± 3 pretreatment and 11 ± 1 posttreatment). Symptoms increased similarly in the postplacebo control group compared with those in the pretreatment clamp study (Fig. 5).
FIG. 5.
A: ΔMSNA during the final 30 min of hyperinsulinemic-hypoglycemic (2.9 ± 0.1 mmol/l) clamp studies in 20 (10 male and 10 female) patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo. ΔMSNA levels were significantly increased (P < 0.05) following 6 weeks’ fluoxetine administration. B: Total symptom scores during the final 30 min of hypoglycemic clamp studies in 20 (10 male and 10 female) patients before and after 6 weeks of fluoxetine administration (SSRI) or placebo. Data are means ± SE.
DISCUSSION
This study investigated hypoglycemic counterregulatory responses following 6 weeks’ chronic administration of fluoxetine in nondiabetic, nondepressed individuals. We determined that plasma concentrations of key neuroendocrine ANS and metabolic counterregulatory responses were increased during the final 30 min of clamped moderate hypoglycemia following high-dose fluoxetine administration. Key counterregulatory mechanisms (ANS, hypothalamic pituitary adrenal, EGP, glycogenolysis, and lipolysis) were significantly amplified following fluoxetine.
Six weeks’ administration of fluoxetine at a stepped dose to 80 mg/day resulted in a substantial increase in most, but not all, ANS responses to hypoglycemia. Plasma epinephrine, norepinephrine, pancreatic polypeptide, and MSNA levels were increased by 25–50% following fluoxetine. ANS drive was increased during hypoglycemia but not during basal conditions. This indicates that the SSRI did not produce a chronic overstimulation of the sympathetic nervous system, particularly evidenced by no increase in basal heart rate, systolic blood pressure, norepinephrine, or MSNA levels. The fluoxetine-increased sympathetic nervous system drive during hypoglycemia therefore appears to be due to an amplification of usual physiologic responses rather than modulation of basal homeostatic mechanisms. Sympatho-adrenal, sympathetic neural, and MSNA response were all amplified following fluoxetine. This was distinct to fluoxetine's effects on plasma cortisol, where there was an increase in both basal levels and responses of the hormone during hypoglycemia. The increased sympathetic nervous system drive resulted in significant amplification of metabolic homeostatic mechanisms during hypoglycemia. Of note, glucose kinetics were profoundly influenced by fluoxetine administration. In particular, EGP was strikingly elevated by fluoxetine. During prolonged hypoglycemia, the ability to defend against a reduced glucose level depends on the balance of increasing glucose production and limiting glucose utilization. Typically, during hypoglycemia that occurs in patients with type 1 diabetes, it is the restriction of glucose uptake that is the major homeostatic mechanism, as there is little or no EGP in these individuals. Fluoxetine administration resulted in a small reduction in glucose uptake but a significant amplification of EGP. This latter response may have been as a result of the combination of the elevated basal cortisol and amplified catecholamines during hypoglycemia (29). Key metabolic counterregulatory mechanisms such as lipolysis (increased glycerol responses), glycogenolysis (increased lactate), and ketogenesis were all elevated by the amplified sympathetic nervous system response caused by fluoxetine. The major regulation of glucose kinetics during hypoglycemia in long-standing type 1 diabetic and insulin-deficient type 2 diabetic patients revolves around a functioning sympathetic nervous system. Glucagon responses to hypoglycemia in type 1 diabetes are typically lost after only 5 years’ duration and are also significantly reduced in long-standing type 2 diabetes (30). Thus, the sympathetic nervous system and epinephrine become the principle defense against a falling plasma glucose level. In the present study, epinephrine responses were increased by chronic fluoxetine therapy, whereas the placebo control had no effect on responses of the catecholamine during hypoglycemia. Norepinephrine and MSNA responses during hypoglycemia were also similarly increased following fluoxetine, thus indicating a widespread amplification of the sympathetic neural and sympatho-adrenal responses. Of particular note, however, were the intriguing findings regarding the lack of an increase in autonomic symptoms despite very large increases in sympathetic nervous system activity following fluoxetine.
The origin of hypoglycemic symptoms during hypoglycemia is complex. Previous studies demonstrated scenarios whereby discordant responses between autonomic symptoms and catecholamine responses can exist during hypoglycemia (17,31–33). Generally, studies have determined that autonomic symptoms can be preserved despite reduced activity in other branches of the sympathetic nervous system. For example, DeRosa et al. (31) demonstrated that symptom responses are preserved in adrenalectomized subjects who have no measurable epinephrine levels during hypoglycemia. Additionally, Aftab-Guy et al. (34,35) demonstrated that high levels of plasma epinephrine mimicking values observed during moderate hypoglycemia only produce minor increases in hypoglycemic symptoms. These studies are examples from a large body of work demonstrating that hypoglycemic symptoms are generated primarily from central ANS drive and end-organ responses. There are also data indicating that hypoglycemic symptoms can be influenced independently by other components of the ANS during hypoglycemia. Dagogo-Jack et al. (32) demonstrated that hypoglycemic symptoms can increase before adrenomedullary or sympathetic neural responses in patients with hypoglycemia-associated autonomic failure (32). Sandoval et al. (33) and Davis et al. (17) also demonstrated that hypoglycemic symptoms are preserved relative to blunting of other ANS responses following antecedent stress. Thus, previous studies seem to indicate that hypoglycemic symptoms are resultant of central ANS drive and are preserved high in the hierarchy of ANS responses to hypoglycemia. Our finding, therefore, of a relatively reduced symptom response (∼20%) following fluoxetine in the context of a generalized increased (∼50–60%) ANS drive (MSNA, epinephrine, norepinephrine, and pancreatic polypeptide) is interesting and unexpected. This may indicate a role for serotonergic pathways in the generation of symptoms during hypoglycemia in healthy man.
The neural mechanisms responsible for fluoxetine's effects on amplifying counterregulatory responses to hypoglycemia are not evident from this study. Numerous studies have demonstrated interactions between serotonergic (both 5-HT1A and 5-HT3) and catecholamine neurotransmission pathways in multiple areas of the brain (8). These include forebrain (thalamus and hypothalamus) and hindbrain nuclei that are known to play important roles in regulating ANS responses during hypoglycemia. Carvalho et al. (36) demonstrated that third-ventricle injections of fluoxetine in wistar rats resulted in hyperglycemia without accompanying hyperinsulinemia. Pretreatment with a selective corticotropin-releasing hormone (CRH) antagonist prevented the increase in hyperglycemia. These data support a role for fluoxetine in increasing CRH levels, which can modulate metabolism via increases in sympathetic nervous system outflow (i.e., hyperglycemia independent of hyperinsulinemia that was suppressed by elevated sympathetic nervous system activity [32]). An earlier study by Chaouloff et al. (37) also demonstrated a role in central serotonergic receptors in the regulation of adrenal catecholamine release. Subsequently, Durand et al. (38) reported that repeated fluoxetine administration can result in increased adrenal weight and amplified corticosteroid responses to stress in certain strains of conscious rats . Thus, the above studies document a role for the interaction of central serotonegic receptors and 1) hypothalamo-pituitary-adrenal axis and 2) sympathetic outflow in rats that may provide a mechanistic basis for the novel findings of the present study in humans. It should be noted that fluoxetine had little or no effect on amplifying glucagon responses during hypoglycemia. This has some relevance, as glucagon is an important component of the normal counterregulatory response to falling plasma glucose and there are data demonstrating that ANS can regulate glucagon release during hypoglycemia (39).
The present study has provided a proof of principle in evaluating the integrated physiologic effects of the SSRI fluoxetine on counterregulatory responses during hypoglycemia. Despite the findings of significant amplification of ANS and metabolic counterregulatory responses following fluoxetine, we should note some particular aspects of the study design. The dose of fluoxetine used in this study was increased to 80 mg over a 6-week period and is larger than often used in clinical practice. Despite this, the drug was well tolerated, with ∼33% of subjects reporting a transient reduction of appetite and mild nausea; however, body weight was unchanged from start to end of the study. One other subject receiving fluoxetine experienced some sexual dysfunction, and one subject on placebo reported vivid dreams. Side effects had abated by the final 2 weeks of fluoxetine administration. Additionally, the healthy volunteers recruited into this study were screened to have no depression or depressive symptoms. Furthermore, fluoxetine had no effects on amplifying hypoglycemic symptoms during hypoglycemia.
In summary, this study demonstrated that 6 weeks’ administration of fluoxetine can profoundly increase key autonomic nervous system (epinephrine, norepinephrine, pancreatic polypeptide, and MSNA), metabolic (EGP, lipolysis, and glycogenolysis), and cardiovascular counterregulatory responses during clamped moderate (2.9 mmol/l) hypoglycemia. This study also demonstrates the importance of serotonergic mechanisms in regulating ANS and hypothalamo-pituitary-adrenal physiologic responses during hypoglycemia in healthy people. In conclusion, these results have provided novel findings demonstrating that serotonergic transmission may be an important mechanism in modulating ANS drive during hypoglycemia in healthy people.
Acknowledgments
Support for this study was provided by grants from the National Insitutes of Health (R01-DK-069803, MO1-RR-000095, P01-HL-056693 and P60-DK-020593).
The authors thank Eric Allen, Susan Hajizadeh, Nathan Jones, and Mary Garmon for expert technical assistance and acknowledge the superb care provided by the staff of the Vanderbilt General Clinical Research Center.
Published ahead of print at http://diabetes.diabetesjournals.org on 20 June 2008.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Perry KW, Fuller RW: Effect of fluoxetine on serotonin and dopamine concentration in microdialysis fluid from rat striatum. Life Sci 50 :1683 –1690,1992 [DOI] [PubMed] [Google Scholar]
- 2.Perry KW, Fuller RW: Fluoxetine increases norepinephrine release in rat hypothalamus as measured by tissue levels of MHPG-SO4 and microdialysis in conscious rats. J Neural Transm 104 :953 –966,1997 [DOI] [PubMed] [Google Scholar]
- 3.Bymaster FP, Zhang W, Carter PA, Shaw J, Chernet E, Phebus L, Wong DT, Perry KW: Fluoxetine, but not other selective serotonin uptake inhibitors, increases norepinephrine and dopamine extrecellular levels in prefrontal cortex. Psychopharmacology (Berl) 160 :353 –361,2002 [DOI] [PubMed] [Google Scholar]
- 4.Deeg MA, Lipkin EW: Hypoglycemia associated with the use of fluoxetine. West J Med 164 :262 –263,1996 [PMC free article] [PubMed] [Google Scholar]
- 5.Sawka AM, Burgart V, Zimmerman D: Loss of hypoglycemia awareness in an adolescent with type 1 diabetes mellitus during treatment with fluoxetine hydrochloride. J Pediatr 136 :394 –396,2000 [DOI] [PubMed] [Google Scholar]
- 6.Sawka AM, Burgart V, Zimmerman D: Loss of awareness of hypoglycemia temporally associated with selective serotonin reuptake inhibitors. Diabetes Care 24 :1845 –1846,2001 [DOI] [PubMed] [Google Scholar]
- 7.Chaouloff F, Gunn SH, Young JB: Influence of 5-HT1 and 5 HT2 Receptor antagonists on insulin-induced adrenomedullary catecholamine release. Neuroendocrinology 54 :639 –645,1991 [DOI] [PubMed] [Google Scholar]
- 8.Blardi P, de Lalla A, Auteri A, Iapichino S, Dell'Erba A, Castrogiovanni P: Plasma catecholamine levels after fluox treatment in depressive patients. Neuropsychobiology 51 :72 –76,2005 [DOI] [PubMed] [Google Scholar]
- 9.Baudrie V, Chaouloff F: Mechanisms involved in the hyperglycemic effect of the 5-HT1c/5 HT2 receptor agonist, DOI. Eur J Pharmacol 213 :41 –46,1992 [DOI] [PubMed] [Google Scholar]
- 10.Zung WW, Richards CB, Short MJ: Self-rating depression scale in an outpatient clinic: further validation of the SDS. Arch Gen Psychiatry 13 :508 –515,1965 [DOI] [PubMed] [Google Scholar]
- 11.Carroll BJ, Fielding JM, Blashki TG: Depression rating scales: a critical review. Arch Gen Psychiatry 28 :361 –366,1973 [DOI] [PubMed] [Google Scholar]
- 12.Abumrad NN, Rabin D, Diamond MC, Lacy WW: Use of a heated superficial hand vein as an alternative site for measurement of amino acid concentration and for the study of glucose and alanine kinetics in man. Metabolism 30 :936 –940,1981 [DOI] [PubMed] [Google Scholar]
- 13.DeFronzo RA, Tobin K, Andres R: Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol 237 :E216 –E223,1979 [DOI] [PubMed] [Google Scholar]
- 14.Amiel SA, Tambolane WV, Simonson DC, Sherwin R: Defective glucose counterregulation after strict control of insulin-dependent diabetes mellitus. N Engl J Med 316 :1376 –1383,1987 [DOI] [PubMed] [Google Scholar]
- 15.Davis SN, Shavers C, Costa F: Differential gender responses to hypoglycemia are due to alterations in CNS drive and not glycemic thresholds. Am J Physiol Endocrinol Metab 279 :E1054 –E1063,2000 [DOI] [PubMed] [Google Scholar]
- 16.Wallin B, Sundiot G, Eriksson B, Domniak P, Grobecker H, Lindblad L: Plasma noradrenaline correlates by sympathetic muscle nerve activity in normotensive man. Acta Physiol Scand 11 :69 –73,1981 [DOI] [PubMed] [Google Scholar]
- 17.Davis SN, Mann S, Galassetti P, Neil RA, Ertl AC, Tate D, Costa F: Effects of differing durations of antecedent hypoglycemia on counterregulatory responses to subsequent hypoglycemia in normal humans. Diabetes 49 :1897 –1903,2000 [DOI] [PubMed] [Google Scholar]
- 18.Wall JS, Steele R, Debodo RD, Altszuler N: Effect of insulin on utilization and production of circulating glucose. Am J Physiol 189 :43 –50,1957 [DOI] [PubMed] [Google Scholar]
- 19.Aguilar-Parada E, Eisentraut AM, Unger RH: Pancreatic glucagon secretion in normal and diabetic subjects. Am J Med Sci 257 :415 –419,1969 [DOI] [PubMed] [Google Scholar]
- 20.Wide L, Porath J: Radioimmunoassay of proteins with the uses of sephadex-coupled antibodies. Biochim Biophys Acta 130 :257 –260,1966 [Google Scholar]
- 21.Causon R, Caruthers M, Rodnight R: Assay of plasma catecholamines by liquid chromatography with electrochemical detection. Anal Biochem 116 :223 –226,1982 [DOI] [PubMed] [Google Scholar]
- 22.Hunter W, Greenwood F: Preparation of [131I]-labeled human growth hormone of high specific activity. Nature 194 :495 –496,1962 [DOI] [PubMed] [Google Scholar]
- 23.Hagopian W, Lever E, Cen D, Emmonoud D, Polonsky K, Pugh W, Moosa A, Jaspan J: Predominance of renal and absence of hepatic metabolism of pancreatic polypeptide in the dog. Am J Physiol 245 :171 –177,1983 [DOI] [PubMed] [Google Scholar]
- 24.Lloyd B, Burrin J, Smythe P, Alberti KGMM: Enzymatic fluorometric continuous flow assays for blood glucose, lactate, pyruvate, alanine, glycerol and 2-hydroxybutyrate. Clin Chem 24 :1724 –1729,1978 [PubMed] [Google Scholar]
- 25.Ho RJ: Radiochemical assay of long chain fatty acids using 63NI as tracer. Anal Biochem 26 :105 –113,1970 [DOI] [PubMed] [Google Scholar]
- 26.Higgins TN, Blackney GB, Dayton J: Analytical evaluation of the Bio-Rad Variant II automated HBA1c Analyzer. Clin Biochem 34 :361 –365,2001 [DOI] [PubMed] [Google Scholar]
- 27.Torok-Both GA, Baker GB, Coutts RT, McKenna KF, Aspeslet LJ: Simultaneous determination of fluoxetine and norfluoxetine enantiomers in biological samples by gas chromatography with electron capture detection. J Chromatogr Biomed Applic 579 :99 –106,1992 [DOI] [PubMed] [Google Scholar]
- 28.Deary L, Hepburn D, Macleod K, Frier BM: Partitioning the symptoms of hypoglycemia using multi-sample confirmatory factor analysis. Diabetologia 36 :771 –770,1993 [DOI] [PubMed] [Google Scholar]
- 29.Gautier C, el Tayeb K, Vranic M, Lickley H: Glucoregulatory role of cortisol and epinephrine interaction studied in adrenal ectomized dogs. Am J Physiol 250 :E343 –E401,1986 [DOI] [PubMed] [Google Scholar]
- 30.Briscoe VJ, Davis SN: Hypoglycemia in type 1 and type 2 diabetes: physiology, pathophysiology and management. Clinical Diabetes 24 :115 –121,2006 [Google Scholar]
- 31.DeRosa MA, Cryer PE: Hypoglycemia and the sympathoadrenal system: neurogenic symptoms are largely the result of sympathetic neural, rather than adrenomedullary, activation. Am J Physiol Endocrinol Metab 287 :E32 –E41,2004 [DOI] [PubMed] [Google Scholar]
- 32.Dagogo-Jack S, Rattarasarn C, Cryer PE: Reversal of hypoglycemia unawareness, but not defective glucose counterregulation, in IDDM. Diabetes 43 :1426 –1434,1994 [DOI] [PubMed] [Google Scholar]
- 33.Sandoval D, Aftab-Guy D, Richardson A, Ertl AC, Davis SN: Acute, same day effects of antecedent exercise on counterregulatory responses to subsequent hypoglycemia in type 1 DM. Am J Physiol-Endocrinology and Metabolism 6 :E1331 –E1338,2006 [DOI] [PubMed] [Google Scholar]
- 34.Aftab-Guy D, Sandoval D, Richardson A, Tate D, Davis SN: Differing physiologic effects of epinephrine in type 1 diabetics and healthy subjects. Am J Physiol-Endocrinol Metab 288 :E178 –E186,2005 [DOI] [PubMed] [Google Scholar]
- 35.Aftab-Guy D, Sandoval D, Richardson A, Tate D, Davis SN: Effects of glycemic control on target organ responses to epinephrine in type 1 diabetes. Am J Physiol-Endocrinol Metab 289 :E258 –E265,2005 [DOI] [PubMed] [Google Scholar]
- 36.Carvalho F, Barros D, Silva J, Rezende, E., Soares, M, Fregoneze, J, De Castro e Silva, E: Hyperglycemia induced by acute central fluoxetine administration: role of the central CRH system and 5-HT3 receptors. Neuropeptides 38 :98 –105,2004 [DOI] [PubMed] [Google Scholar]
- 37.Chaouloff F, Gunn SH, Young JB: Central 5-hydroxytryptamine2 receptors are involved in the adrenal catecholamine-releasing and hyperglycemic effects of the 5-hydroxytryptamine indirect agonist D-fenfluramine in the conscious rat. J Pharmacol Exp Ther 260 :1008 –1016,1992 [PubMed] [Google Scholar]
- 38.Durand M, Berton O, Aguerre S, Endo L, Combourieu I, Mormede P, Chaouloff F: Effects of repeated fluoxetine on anxiety-related behaviours, central serotonergic systems, and the corticotropic axis in SHR and WKY rats. Neuropharmacology 38 :893 –907,1999 [DOI] [PubMed] [Google Scholar]
- 39.Taborsky GJ Jr, Ahren B, Mundinger TO, Mei Q, Havel PJ: Autonomic mechanism and defects in the glucagon response to insulin induced hypoglycemia. Diabetes Nutr Metab 15 :318 –322,2000 [PubMed] [Google Scholar]