Abstract
Undercutting decompression is a common surgical procedure for the therapy of lumbar spinal canal stenosis. Segmental instability, due to segmental degeneration or iatrogenic decompression is a typical problem that is clinically addressed by fusion, or more recently by semi-rigid stabilization devices. The objective of this experimental biomechanical study was to investigate the influence of spinal decompression alone, as well as in conjunction with two semi-rigid stabilizing implants (Wallis, Dynesys®) on the range of motion (ROM) of lumbar spine segments. A total of 21 fresh-frozen human lumbar spine motion segments were obtained. Range of motion and neutral zone (NZ) were measured in flexion-extension (FE), lateral bending (LAT) and axial rotation (ROT) for each motion segment under four conditions: (1) with all stabilizing structures intact (PHY), (2) after bilateral undercutting decompression (UDC), (3) after additional implantation of Wallis (UDC-W) and (4) after removal of Wallis and subsequent implantation of Dynesys® (UDC-D). Measurements were performed using a sensor-guided industrial robot in a pure-moment-loading mode. Range of motion was defined as the angle covered between loadings of −5 and +5 Nm during the last of three applied motion cycles. Untreated physiologic segments showed the following mean ROM: FE 6.6°, LAT 7.4°, ROT 3.9°. After decompression, a significant increase of ROM was observed: 26% FE, 6% LAT, 12% ROT. After additional implantation of a semi-rigid device, a decrease in ROM compared to the situation after decompression alone was observed with a reduction of 66 and 75% in FE, 6 and 70% in LAT, and 5 and 22% in ROT being observed for the Wallis and Dynesys®, respectively. When the flexion and extension contribution to ROM was separated, the Wallis implant restricted extension by 69% and flexion by 62%, the Dynesys® by 73 and 75%, respectively. Compared to the intact status, instrumentation following decompression led to a ROM reduction of 58 and 68% in FE, 1 and 68% in LAT, −6 and 13% in ROT, 61 and 65% in extension and 54 and 70% in flexion for Wallis and Dynesys®. The effect of the implants on NZ corresponded to that on ROM. In conclusion, implantation of the Wallis and Dynesys® devices following decompression leads to a restriction of ROM in all motion planes investigated. Flexion–extension is most affected by both implants. The Dynesys® implant leads to an additional strong restriction in lateral bending. Rotation is only mildly affected by both implants. Wallis and Dynesys® restrict not only isolated extension, but also flexion. These biomechanical results support the hypothesis that postoperatively, the semi-rigid implants provide a primary stabilizing function directly. Whether they can improve the clinical outcome must still be verified in prospective clinical investigations.
Keywords: Range of motion, Lumbar spine, Decompression, Dynesys®, Wallis
Introduction
Undercutting decompression is a standard procedure in the therapy of lumbar spinal stenosis [3, 4, 13, 21, 25]. Accompanying segmental instability may occur, which is caused either by degenerative segmental disease involving the intervertebral disc, the zygapophysial joints and ligaments, or as a consequence of the surgical decompression itself [7, 8, 15, 17]. Intervertebral fusion is the gold standard for the treatment of segment instability [9]. Nevertheless, several disadvantages and side effects of fusion, i.e., adjacent segment degeneration, and potential complications have motivated the development of a new family of dynamic implants. A number of semi-rigid implant designs, all applied via a posterior approach, have been developed to improve segmental stability, unload posterior elements and restrict painful motion while otherwise enabling movement. Among these new implants are the interspinous Wallis implant (Abbott Spine, Bordeaux, France) [5, 27–30, 35], and the Dynesys® implant (Zimmer GmbH, Winterthur, Switzerland) [12, 18, 20, 22–24, 26, 31]. Both devices belong to the group of dynamic systems, which functionally bridge the gap between an unstabilized decompression on the one hand, and rigid fusion procedures following decompression on the other. The methods differ in their mode of operation and as such also in the surgical technique required for implantation.
The Wallis implant is a floating system, consisting of an interspinous spacer (made of polyetheretherketone = PEEK), which does not require the insertion of pedicle screws. The implant is augmented by two woven dacron ribbons, which are wrapped around the spinous processes and fixed under tension. The interspinous block is intended to limit extension as well as flexion and rotation, keep the spinal canal and neuroforamina open and unload the posterior disc and zygapophysial joints [28]. The Dynesys® implant is a bilateral device consisting of titanium pedicle screws and hollow polycarbonate urethane (PCU) spacers containing tensioned cords made of polyethylene terephthalate (PET). The indications for the use of both implants are similar. They are intended to stabilize a lumbar segment following spinal canal decompression.
Review of the literature shows multiple investigations and studies on Dynesys® but only very few on Wallis. To the authors’ knowledge there is no literature available, which directly compares both implants in a biomechanical in vitro study.
The aim of this study was thus to analyze the effect of these implants, as well as of undercutting decompression, on the range of motion (ROM) and neutral zone (NZ) of human lumbar segments in an in vitro setting. The working hypothesis was that the implants provide a stabilizing function on the lumbar spine motion segments. An experimental cadaver study was designed in which motion segments were investigated under pure moment loadings.
Materials and methods
A total of 11 human lumbar non-fixated spines were obtained (7 female, 4 male; mean age 77 years, range: 65–87 years) from the Institute of Anatomy of the University of Münster, Germany and frozen in triple sealed bags at −20°C until being thawed at 6°C before testing. The specimens were visually inspected for abnormalities. Structural integrity of the specimens was verified by means of multidetector spiral computed tomography (MDCT). Images were obtained using a 16-MDCT system (Somatom Sensation 16, Siemens Medical Solutions, Forchheim, Germany) using standard parameters for spine CT: detector configuration of 16 × 1.5 mm, 120 kV, CareDose ref. mAs 300, pitch 0.75. No fractures, neoplasms or signs of severe systemic diseases were observed in any of the tested specimens.
After thawing, a total of 21 lumbar motion segments were dissected (6× L1/L2; 5× L2/L3; 5× L3/L4; 5× L4/L5). Muscle tissue was dissected away from the specimens while maintaining all stabilizing ligaments (anterior and posterior longitudinal ligament, yellow ligament, inter- and supraspinous ligament), the intervertebral disc and the zygapophysial joints including their capsules. In order to fix the specimens firmly in the testing apparatus, the cranial and caudal endplates including a third of the cranial and caudal vertebral body were embedded in a two-component polyurethane casting resin (UREOL FC 53, Vantico GmbH, Wehr, Germany) such that segmental motion was not restricted in any way.
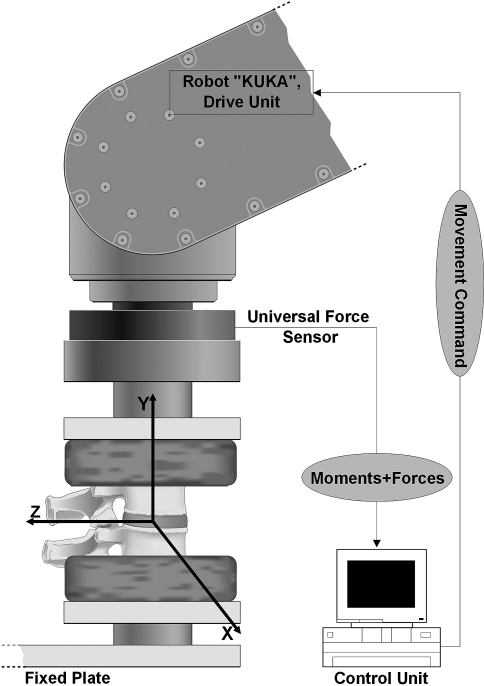
Testing of the specimens was performed in a validated technique [14] (Fig. 1), in which pure moments were applied to the motion segment by means of a sensor-guided robot. The testing device consisted of an industrial robot (KUKA, GmbH, Augsburg, Germany) equipped with a six-component force-moment sensor (IpeA, GmbH, Berlin, Germany). The robot was programmed to operate in displacement-control (angular speed 2.5°/min, moment limit 5 Nm) about the primary testing axis, while simultaneously closed-loop load- or movement-controlled about the remaining 5° of freedom, respectively (two remaining moments regulated to 0 Nm, and three force axes regulated to 0 N).
Fig. 1.
Sensor-guided robot KUKA (KUKA Roboter GmbH, Augsburg, Germany) applying pure moments on a lumbar motion segment
Three loading and unloading cycles to 5 Nm were applied in pure flexion–extension, lateral bending and axial rotation, respectively. Range of motion was defined as the covered angle between a loading of −5 and +5 Nm during the last of three motion cycles. This was in accordance with the recommended testing criteria for spinal implants; the first two cycles were used as preconditioning cycles and the third cycle was used for data analysis [37].
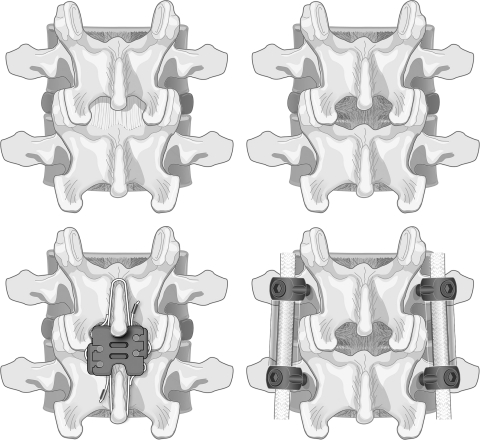
Range of motion was measured a total of four times for each motion segment, once each in the physiological state (PHY), after undercutting decompression (UDC), after additional implantation of the Wallis (UDC-W), and finally after implantation of the Dynesys® (UDC-D) (Fig. 2).
Fig. 2.
Different treatment conditions of a lumbar motion segment tested (view from posterior). Top left: physiologic with all stabilizing ligaments intact; top right: following bilateral undercutting decompression; bottom left: after additional implantation of Wallis; bottom right: after additional implantation of Dynesys®
The first condition (PHY) was performed with the specimens prepared as described above. Subsequently, bilateral posterior undercutting decompression of the spinal canal was performed by transection of the supra- and interspinous ligaments as well as the yellow ligaments. Three milimeter of the cranial and caudal lamina were resected. Medial parts of the zygapophysial joints were resected until a “normal anatomy” was restored. This included resection of hyerptrophic parts of the joints. The joint space was not opened and the stabilizing joint capsules were kept intact. The stability of the articular processes was strictly maintained.
After decompression was performed and ROM measured, an interspinous spacer (Wallis, size 10) was implanted using the established surgical techniques. The spacer was placed anteriorly between the spinous processes and secured with the two dacron ligaments that were wrapped around the spinous processes under tension. The specimen was tested again according to the above-mentioned protocol.
The Wallis implant was subsequently removed and the Dynesys® implant (6.4 × 45 mm pedicle screws) inserted using the manufacturer’s recommended operative procedure and instrumentation. The stiffness of the Dynesys® spacers (PCU), which are normally subjected to body temperature in the patient, varies with temperature. Since the experiments were carried out at room temperature, spacers were used reproducing the in vivo stiffness of the implanted original device at body temperature [22]. Biomechanical testing was again performed according to the same protocol. The specimens were kept moist during testing by applying isotonic physiologic saline solution.
In addition to ROM, the neutral zone (NZ) and neutral position of the motion segments were computed. The NZ was defined as the range of displacement, where force-free motion occurs [34]. It is a common parameter used to describe segmental instability [17]. The neutral position was defined as the middle (bisector) of the end-points of the NZ, and used as a reference point for discerning the flexion and extension components of ROM [17]. Testing each specimen in the intact state, after decompression, following stabilization with an interspinous spacer and finally after Dynesys® instrumentation, allowed each specimen to act as its own control resulting in a repeated measures study design. Statistical analysis was performed using SPSS 13.0 (SPSS Inc., Chicago, IL, USA). Explorative testing for a normal distribution using the Kolmogorov–Smirnow test revealed that a non-parametric analysis should be performed, on which the Friedman and the Wilcoxon tests were used for comparison of the repeated measures of dependent variables for the comparison of the surgical status. The Kruskal–Wallis test was used for comparison of ROM from independent samples, i.e., different motion segment levels. Pearson’s correlation analysis was applied to study the effect of Dynesys® spacer height on ROM restriction. P-values of significance tests are to be interpreted in an explorative way and are regarded significant in case P < 0.05. No adjustment for multiple testing was conducted.
Results
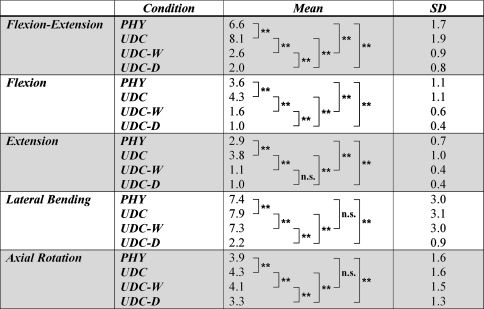
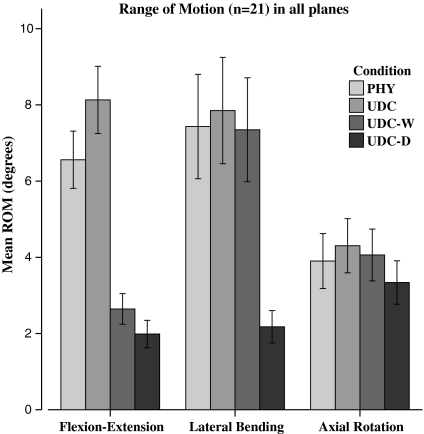
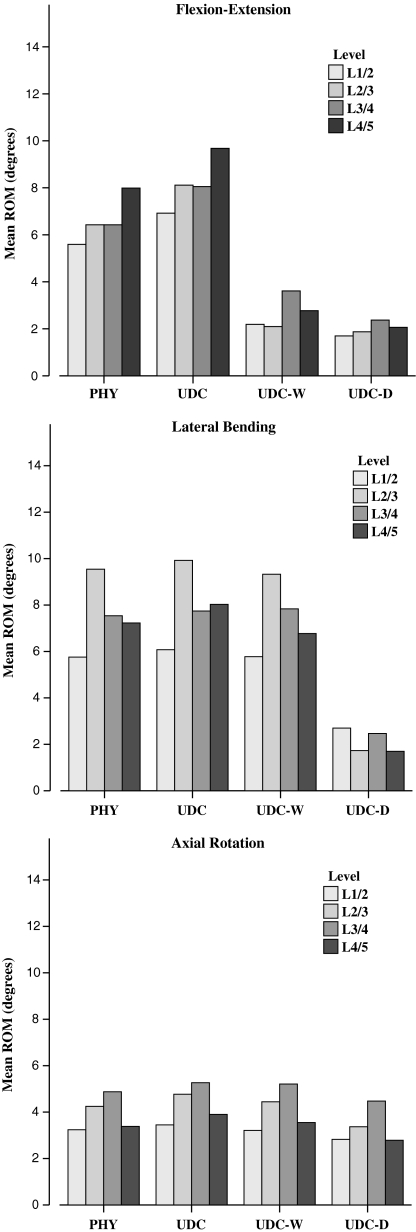
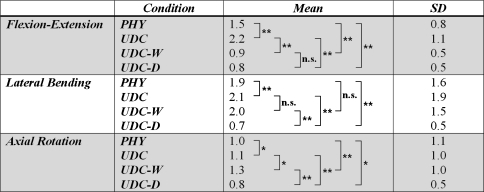
The physiologic motion segment ROM was observed to be 6.6° ± 1.7° in flexion–extension, 7.4° ± 3.0° in lateral bending and 3.9° ± 1.6° in axial rotation for all 21 segments (Table 1). After decompression, a significant increase (P < 0.001) in ROM of 26% in flexion–extension, 6% in lateral bending and 12% in axial rotation was observed (Table 1; Fig. 3).
Table 1.
Mean ROM (in degrees) of all specimens (n = 21) under the four investigated treatment conditions
ROM for lateral bending and axial rotation include displacement to the left and right side
Statistical significances were calculated using Wilcoxon test (* P ≤ 0.05; ** P ≤ 0.01)
SD standard deviation, PHY segments with all stabilizing structures intact, UDC after bilateral undercutting decompression, UDC-W after additional implantation of Wallis, UDC-D after removal of Wallis and subsequent implantation of Dynesys®
Fig. 3.
Mean ROM (in degrees) of all 21 segments including 95% confidence interval. PHY segments with all stabilizing structures intact, UDC after bilateral undercutting decompression, UDC-W after additional implantation of Wallis, UDC-D after removal of Wallis and subsequent implantation of Dynesys®. ROM for lateral bending and axial rotation include displacement to the left and right side
Additional implantation of a semi-rigid device led to a reduction in ROM compared to the situation after decompression alone: 66% (Wallis) and 75% (Dynesys®) (each P < 0.001) in flexion–extension, 6% (Wallis) (P = 0.003) and 70% (Dynesys®) (P < 0.001) in lateral bending, 5% (Wallis) (P = 0.002) and 22% (Dynesys®) (P < 0.001) in axial rotation (Table 1; Fig. 3). The Wallis and Dynesys® implants differed significantly in the amount of reduction of ROM, with the Dynesys® implant creating a more stable situation in all three planes of motion (flexion–extension P = 0.001, lateral bending P < 0.001, axial rotation P < 0.001).
On observing flexion and extension separately, it was indicated that decompression led to a highly significant ROM increase of both flexion (P < 0.001) and extension (P < 0.001). Implantation of the Wallis and Dynesys® implants resulted in a highly significant stabilization of extension (P < 0.001) as well as of flexion (P < 0.001) compared to the decompressed status (Table 1).
Compared to the intact status, instrumentation following decompression led to a ROM reduction of 58% (Wallis) and 68% (Dynesys®) (each P < 0.001) in flexion–extension, 1% (Wallis) (P = 0.526) and 68% (Dynesys®) (P < 0.001) in lateral bending, −6% (Wallis) (P = 0.063) and 13% (Dynesys®) (P < 0.001) in axial rotation, 61% (Wallis) and 65% (Dynesys®) (each P < 0.001) in extension, 54% (Wallis) and 70% (Dynesys®) in flexion (each P < 0.001).
On comparing the effect of Wallis and Dynesys®, no significant difference was found in the restriction of extension (P = 0.170), whereas restriction of flexion was more pronounced with the Dynesys® compared to the Wallis implant (P < 0.001) (Table 1). The mean Dynesys® spacer height on the right side was 26.1 mm (SD 4.7 mm) and on the left side 26.3 mm (SD 4.8 mm). No significant effect of spacer height on ROM reduction was found in all planes.
Statistical analysis (Kruskal–Wallis test) did not identify a rational significant effect of segmental level on ROM in the various motion planes investigated. However, a tendency towards slight differences could be observed (Fig. 4). Especially, the relative stabilizing effect of Wallis and Dynesys® on the different motions compared to the decompressed status without any additional instrumentation was not dependent on the segmental level.
Fig. 4.
Mean ROM (in degrees) of specimens grouped according to segmental level in the four investigated conditions in flexion–extension, lateral bending and axial rotation
The data showed that decompression led to a significant increase of the NZ in all planes investigated (Table 2). Additional implantation of Wallis led to a significant decrease of the NZ only in flexion–extension. The Dynesys® implant significantly reduced the NZ in all planes compared to the status after decompression, more in flexion–extension and lateral bending than in axial rotation. When comparing the effect of both implants, it was found that they did not differ in their effect on the NZ in flexion–extension, whereas differences were observed in lateral bending, and small differences in rotation. The Dynesys® implant was observed to cause a significantly greater restriction of the NZ than the Wallis implant.
Table 2.
Neutral zone (in degrees)
Wilcoxon test (* P ≤ 0.05; ** P ≤ 0.01) was applied to determine statistical differences
SD standard deviation
Discussion
Lumbar spinal stenosis is probably the most common contemporary ailment leading to spine surgery [1, 6, 9]. For years, surgeons had the option of either performing an isolated decompression or to decompress with an accompanying fusion. In the last several years, non-rigid, dynamic implants have been developed functionally bridging the wide gap between isolated decompression and decompression with fusion. Two general principles of device implantation have emerged: interspinous spacers and pedicle screw-based implants [5].
The first group contains implants that are fixed between the interspinous processes without the need for pedicle screw insertion: X STOP (St. Francis Medical Technologies, Alameda, CA, USA), Coflex (Paradigm Spine, New York, NY, USA), Diam (Medtronic, Memphis, TN, USA) and Wallis. Whereas several studies have been published investigating X STOP [2, 7, 16, 32, 38, 40, 41], only few data have been published studying Wallis [27–30, 35].
The second group of implants includes pedicle screw-based systems such as Dynesys®, TOPS (total posterior-element system) (Impliant Ltd., Ramat Poleg, Israel) and Cosmic (Ulrich medical, Ulm, Germany) [36]. Dynesys® is the most intensively studied implant in this context with several clinical and biomechanical studies having been published to date [12, 20, 24, 26, 31].
The present study investigated the effect of decompression and additional dynamic stabilization on the ROM of human lumbar segments in an in vitro setting. We observed that decompression led to a significant increase of ROM in all planes. This indicates that a certain amount of iatrogenic instability due to decompression is normal. Additional implantation of Wallis and Dynesys® led to a significant restriction of ROM in all planes, with flexion–extension being mostly strongly affected. Dynesys® led to an additional strong restriction of lateral bending. Rotation was only mildly affected by both implants. Furthermore, the Wallis and Dynesys® implants not only restricted extension, but also flexion.
Our physiologic ROM and neutral zones correlated well with values reported in the literature [8, 19, 39]. This agreement with published values, in addition to our own validation study [14], indicates that our testing method and setup were reliable.
Fuchs et al. [7] observed a significant increase of ROM in L3/4 following bilateral total facetectomy during flexion and axial rotation and a trend towards an increase of ROM during extension and lateral bending. Our results also indicated significant increases of ROM in all planes. When comparing these results, it should be considered that our decompression procedure was not directly comparable to that of Fuchs et al. since we chose a bilateral decompression, resecting only medial superficial parts of the articular processes and preserving the integrity of the joint’s space and thus the joint’s stability.
We observed that additional implantation of the Wallis implant led to a ROM reduction in all planes. In lateral bending and rotation, a status similar to the physiologic status was achieved, significant reductions in flexion–extension in sum as well as isolated flexion and extension were observed.
Tsai et al. [33] found a significant reduction of ROM in flexion–extension in L4/5 segments on comparing decompressed segments with decompressed segments additionally instrumented with Coflex. However, they did not differentiate between isolated flexion and extension. This group found a significant ROM reduction in axial rotation on comparing decompressed segments and decompressed segments with Coflex. These results are similar to ours. With regard to lateral bending, they found a trend towards an increase of ROM induced by Coflex insertion compared to the decompressed status. Tsai et al. [33] interpreted this fact as “not particularly relevant” stating that the implant “should not influence lateral bending”. However, Fuchs et al. [7] described a similar effect of X STOP following surgical decompression, reporting an increase of lateral bending ROM in L3/4 segments, on comparing decompressed segments with decompressed segments that were additionally instrumented with X STOP. Our results of all 21 segments show that Wallis obviously does not lead to this effect. Wallis induces a mild but significant reduction of lateral bending ROM compared to the decompressed status resulting in a ROM similar to the physiologic status. Distraction forces induced by Wallis might be similar to those by Coflex and X STOP, but fixation with the dacron ribbons causes the stabilizing effect. Another contributing factor for the differences in lateral bending restriction between our study and the studies by Fuchs et al. and Tsai et al. [7, 33] might be differences in facet joint resection: Fuchs et al. described a bilateral total facetectomy, Tsai et al. resected 50% of the inferior bony facet bilaterally in addition to the facet capsules. Our technique of decompression seems to be comparable to the technique by Tsai et al. For this reason, we think that the main reason for these ROM differences between Coflex and Wallis is the fixation by ribbon.
It has been reported that X STOP significantly reduces zygapophysial joint loading during extension and significantly unloads the intervertebral disc in the neutral and extended position [32, 38]. A similar effect on the disc and the joints can be assumed after implantation of other interspinous blockers such as Wallis. X STOP has been reported to decrease flexion and extension ROM following decompression or also without additional decompression, which correlates well with our results [7, 16]. The reports of the effect of X STOP on isolated flexion are contradictory in the literature. We also doubt the restricting effect on flexion because of the weakening of the posterior ligaments by device implantation without a compensating stabilization mechanism such as the ribbon of the Wallis implant. Whereas Lindsey et al. and Fuchs et al. [7, 16] found a significant reduction of flexion, Wilke et al. [35] described only marginal effects on flexion. Our results confirm a significant restricting effect of Wallis on isolated flexion and extension. Fuchs et al. [7] did not observe a significant effect of X STOP following decompression on axial rotation ROM. Our results show a partly significant but very mild ROM restriction in rotation induced by Wallis. In this point, our results generally correspond to the currently published X STOP data. The results of our study are in general similar to the results by Fuchs et al., in that we observe major stabilizing effects of Wallis and X STOP in the sagittal plane, but less in the frontal and axial plane. A difference between both studies is the fact that Fuchs et al. used a superimposed 700 N compressive load and applied ±7.5 Nm bending moments instead of ±5 Nm without preload as in our setting.
Our results showed that Dynesys® led to a significant ROM restriction in all planes compared to the decompressed status as well as compared to the decompressed status stabilized with Wallis. Only in isolated extension, the Dynesys® and Wallis implants do not differ significantly. Nevertheless, segments instrumented with Dynesys® allow minor motions, which in our opinion justifies this implant being referred to as “semi-rigid” or “dynamic”. Dynesys® led to a predominant restriction of flexion–extension, isolated flexion, isolated extension and lateral bending. Rotation was also significantly reduced, but only to a lesser extent. This may be explained by the construct of spacers and cords allowing the cords to move and especially rotate within the spacers. The construct is not an angularly locked design in contrast to an instrumented fusion with rods and screws. These results of our study correlate well to data in the literature [18]. Whereas Niosi et al. could find an effect of Dynesys® spacer height on ROM, we could not confirm this effect. Our findings might be explained by the standardized tensioning in all segments independent of the spacer height.
A study of the ROM of the different native lumbar segmental levels did not show statistically significant differences. However, we found tendencies that correlate well with the literature [39]. The relative amount of motion restriction induced by both implants does not differ significantly between the tested segmental levels. This is relevant to clinical practice.
The results studying the effects of the different surgical conditions on NZ indicate that decompression leads to a significant increase of the NZ in all planes of motion investigated. This seems logical when keeping in mind that decompression leads to a slight instability. Additional implantation of Wallis or Dynesys® leads to a reduction of the NZ in flexion–extension. Concerning lateral bending, Wallis does not lead to a significant change of the NZ, whereas Dynesys® significantly reduces it. With regard to axial rotation, both implants only led to minor changes of the NZ. The effects on NZ in all planes correspond well to the effects on ROM. Our findings concerning effects of decompression and additional Dynesys® instrumentation on NZ correspond excellently to the reported data of Niosi et al. [18].
This study was performed with pure moments without additional preload. Although this might not represent ideally the physiologic condition, it follows internationally accepted recommendations and guidelines [10, 11, 22, 36, 37]. Niosi et al. [18] compared ROM with and without a preload of 600 N. With a follower preload they found the same trends in ROM as seen without preload, but typically differences between the test conditions were smaller. This effect was described in the same quantity in all three planes and since the motion with Dynesys® was already small, differences became less pronounced using preload. So to better focus on slight differences between two implants, such as Dynesys® and Wallis in our study, it was chosen to perform the study without preload.
In this study, each segment was tested with ±5 Nm. The authors are well aware that other authors recommended testing amplitudes of ±7.5 Nm or 6–10 Nm in the lumbar spine [11, 37]. However, Wilke et al. [37] recommended reducing the load by one-half when testing osteoporotic specimens. The increased mean age of our specimens (77 years) implying an age-dependent vulnerability, even though no apparent osteoporosis was found, as well as the fact that each specimen was tested 4 × 3 × 3 times consecutively (four different conditions, each condition in three planes, each plane in three consecutive testing cycles) were reasons to choose a lower loading amplitude of ±5 Nm in order to maintain the integrity of the specimens until the end of the last measurement. In addition, typical lumbar load-displacement curves only show small increments of ROM above 5 Nm. Major differences mostly occur at lower moments.
The aim of our study was to focus on the operated segment rather than on adjacent segments. Therefore, it was chosen to study single motion segments. In case of samples consisting of three segments including cranial and caudal adjacent levels, investigation would have required a considerably more complex testing setup with kinematic measurements on three motion segments.
The results of the present study should be interpreted in the context of the knowledge that ROM changes induced by segmental degeneration differs in the motion planes affected. Fujiwara et al. [8] thus found that axial rotation was most affected by disc degeneration, leading to an increase of ROM during initial and intermediate degeneration. As segmental degenerative instability predominantly affects axial rotation, it could be hypothesized that dynamic semi-rigid implants should primarily aim to stabilize axial rotation. Our results show that neither the Wallis nor Dynesys® implants fulfill this criterion.
Conclusion
Undercutting decompression leads to a significant segmental instability in all planes. Implantation of Wallis and Dynesys® after decompression leads to a significant restriction of segmental ROM. Wallis limits only the flexion–extension plane; Dynesys® limits both flexion–extension and lateral bending. Axial rotation is minimally restricted by both implants. The observed effects on the NZ correspond well with the effects on ROM.
The results of this study suggest that these two implants can bridge the gap between decompression alone without any stabilizing implant and instrumented fusion limiting also axial rotation. Although both, the Wallis and Dynesys®, are non-rigid implants, they differ in the amount and plane of restriction and may thus be applied for different clinical or biomechanical situations. The biomechanical results of this study support the hypothesis that the semi-rigid implants provide a primary stabilizing function. Whether they can improve clinical outcome must still be verified in prospective clinical investigations.
References
- 1.Aalto TJ, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, Kroger H, Andrade J, Jimenez R, Tapaninaho A, Turunen V, Savolainen S, Airaksinen O. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine. 2006;31:E648–E663. doi: 10.1097/01.brs.0000231727.88477.da. [DOI] [PubMed] [Google Scholar]
- 2.Anderson PA, Tribus CB, Kitchel SH. Treatment of neurogenic claudication by interspinous decompression: application of the X STOP device in patients with lumbar degenerative spondylolisthesis. J Neurosurg Spine. 2006;4:463–471. doi: 10.3171/spi.2006.4.6.463. [DOI] [PubMed] [Google Scholar]
- 3.Benini A. [Lumbar spinal stenosis. An overview 50 years following initial description] Orthopade. 1993;22:257–266. [PubMed] [Google Scholar]
- 4.Benini A. [Stenosis of the lumbar spinal canal. Pathophysiology, clinical aspects and therapy] Orthopade. 1997;26:503–514. doi: 10.1007/s132-1997-8286-3. [DOI] [PubMed] [Google Scholar]
- 5.Christie SD, Song JK, Fessler RG. Dynamic interspinous process technology. Spine. 2005;30:S73–S78. doi: 10.1097/01.brs.0000174532.58468.6c. [DOI] [PubMed] [Google Scholar]
- 6.Ciol MA, Deyo RA, Howell E, Kreif S. An assessment of surgery for spinal stenosis: time trends, geographic variations, complications, and reoperations. J Am Geriatr Soc. 1996;44:285–290. doi: 10.1111/j.1532-5415.1996.tb00915.x. [DOI] [PubMed] [Google Scholar]
- 7.Fuchs PD, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The use of an interspinous implant in conjunction with a graded facetectomy procedure. Spine. 2005;30:1266–1272. doi: 10.1097/01.brs.0000164152.32734.d2. [DOI] [PubMed] [Google Scholar]
- 8.Fujiwara A, Lim TH, An HS, Tanaka N, Jeon CH, Andersson GB, Haughton VM. The effect of disc degeneration and facet joint osteoarthritis on the segmental flexibility of the lumbar spine. Spine. 2000;25:3036–3044. doi: 10.1097/00007632-200012010-00011. [DOI] [PubMed] [Google Scholar]
- 9.Gibson JN, Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane review. Spine. 2005;30:2312–2320. doi: 10.1097/01.brs.0000182315.88558.9c. [DOI] [PubMed] [Google Scholar]
- 10.Goel VK, Panjabi MM. A new standard guide for the testing of spinal implant constructs, Part I: Guide for the multidirectional instability evaluation of the construct. ASTM (draft version) 1992;6:1–9. [Google Scholar]
- 11.Goel VK, Panjabi MM, Patwardhan AG, Dooris AP, Serhan H. Test protocols for evaluation of spinal implants. J Bone Joint Surg Am. 2006;88(Suppl 2):103–109. doi: 10.2106/JBJS.E.01363. [DOI] [PubMed] [Google Scholar]
- 12.Grob D, Benini A, Junge A, Mannion AF. Clinical experience with the Dynesys semirigid fixation system for the lumbar spine: surgical and patient-oriented outcome in 50 cases after an average of 2 years. Spine. 2005;30:324–331. doi: 10.1097/01.brs.0000152584.46266.25. [DOI] [PubMed] [Google Scholar]
- 13.Gunzburg R, Szpalski M. The conservative surgical treatment of lumbar spinal stenosis in the elderly. Eur Spine J. 2003;12(Suppl 2):S176–S180. doi: 10.1007/s00586-003-0611-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hurschler C, Pott L, Gossé F, Wirth CJ (2005) Sensor-guided robotic spine motion-segment biomechanical testing: Validation against the pure moment apparatus. Transactions of the 51st annual meeting of the Orthopaedic Research Society, vol. 30, Washington DC
- 15.Knaub MA, Won DS, McGuire R, Herkowitz HN. Lumbar spinal stenosis: indications for arthrodesis and spinal instrumentation. Instr Course Lect. 2005;54:313–319. [PubMed] [Google Scholar]
- 16.Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28:2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 17.Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine. 1994;19:1371–1380. doi: 10.1097/00007632-199406000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Niosi CA, Zhu QA, Wilson DC, Keynan O, Wilson DR, Oxland TR. Biomechanical characterization of the three-dimensional kinematic behaviour of the Dynesys dynamic stabilization system: an in vitro study. Eur Spine J. 2006;15:913–922. doi: 10.1007/s00586-005-0948-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Panjabi MM, Oxland TR, Yamamoto I, Crisco JJ. Mechanical behavior of the human lumbar and lumbosacral spine as shown by three-dimensional load-displacement curves. J Bone Joint Surg Am. 1994;76:413–424. doi: 10.2106/00004623-199403000-00012. [DOI] [PubMed] [Google Scholar]
- 20.Putzier M, Schneider SV, Funk J, Perka C. [Application of a dynamic pedicle screw system (DYNESYS) for lumbar segmental degenerations: comparison of clinical and radiological results for different indications] Z Orthop Ihre Grenzgeb. 2004;142:166–173. doi: 10.1055/s-2004-818781. [DOI] [PubMed] [Google Scholar]
- 21.Rompe JD, Eysel P, Zollner J, Nafe B, Heine J. Degenerative lumbar spinal stenosis. Long-term results after undercutting decompression compared with decompressive laminectomy alone or with instrumented fusion. Neurosurg Rev. 1999;22:102–106. doi: 10.1007/s101430050040. [DOI] [PubMed] [Google Scholar]
- 22.Schmoelz W, Huber JF, Nydegger T, Claes L, Wilke HJ. Influence of a dynamic stabilisation system on load bearing of a bridged disc: an in vitro study of intradiscal pressure. Eur Spine J. 2006;15:1276–1285. doi: 10.1007/s00586-005-0032-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schmoelz W, Huber JF, Nydegger T, Dipl I, Claes L, Wilke HJ. Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech. 2003;16:418–423. doi: 10.1097/00024720-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Schnake KJ, Schaeren S, Jeanneret B. Dynamic stabilization in addition to decompression for lumbar spinal stenosis with degenerative spondylolisthesis. Spine. 2006;31:442–449. doi: 10.1097/01.brs.0000200092.49001.6e. [DOI] [PubMed] [Google Scholar]
- 25.Schulte TL, Bullmann V, Lerner T, Schneider M, Marquardt B, Liljenqvist U, Pietila TA, Hackenberg L. Lumbar spinal stenosis. Orthopade. 2006;35:675–692. doi: 10.1007/s00132-006-0971-5. [DOI] [PubMed] [Google Scholar]
- 26.Schwarzenbach O, Berlemann U, Stoll TM, Dubois G. Posterior dynamic stabilization systems: DYNESYS. Orthop Clin North Am. 2005;36:363–372. doi: 10.1016/j.ocl.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Senegas J. La ligamentoplastie intervertebrale, alternative a l’arthrodese dans le traitement des instabilities degeneratives. Acta Orthop Belg. 1991;57(Suppl. 1):221–226. [PubMed] [Google Scholar]
- 28.Senegas J. Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J. 2002;11(Suppl 2):S164–S169. doi: 10.1007/s00586-002-0423-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Senegas J, Etchevers JP, Baulny D, Grenier F. Widening of the lumbar vertebral canal as an alternative to laminectomy in the treatment of lumbar stenosis. Fr J Orthop Surg. 1988;2:93–99. [PubMed] [Google Scholar]
- 30.Senegas J, Vital JM, Pointillart V, Mangione P (2007) Long-term actuarial survivorship analysis of an interspinous stabilization system. Eur Spine J, Apr 11 (Epub ahead of print) [DOI] [PMC free article] [PubMed]
- 31.Stoll TM, Dubois G, Schwarzenbach O. The dynamic neutralization system for the spine: a multi-center study of a novel non-fusion system. Eur Spine J. 2002;11(Suppl 2):S170–S178. doi: 10.1007/s00586-002-0438-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003;28:26–32. doi: 10.1097/00007632-200301010-00008. [DOI] [PubMed] [Google Scholar]
- 33.Tsai KJ, Murakami H, Lowery GL, Hutton WC. A biomechanical evaluation of an interspinous device (Coflex) used to stabilize the lumbar spine. J Surg Orthop Adv. 2006;15:167–172. [PubMed] [Google Scholar]
- 34.White AA, Panjabi MM. Clinical biomechanics of the spine. 2nd ed. Philadelphia: Lippincott; 1990. [Google Scholar]
- 35.Wilke HJ, Drumm J, Häussler K, Claes L. Segmental stability and intradiscal pressure achieved with different interspinous implants. Eur Spine J. 2006;15:1561–1632. doi: 10.1007/s00586-006-0215-8. [DOI] [Google Scholar]
- 36.Wilke HJ, Schmidt H, Werner K, Schmolz W, Drumm J. Biomechanical evaluation of a new total posterior-element replacement system. Spine. 2006;31:2790–2796. doi: 10.1097/01.brs.0000245872.45554.c0. [DOI] [PubMed] [Google Scholar]
- 37.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7:148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wiseman CM, Lindsey DP, Fredrick AD, Yerby SA. The effect of an interspinous process implant on facet loading during extension. Spine. 2005;30:903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 39.Yamamoto I, Panjabi MM, Crisco T, Oxland T. Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine. 1989;14:1256–1260. doi: 10.1097/00007632-198911000-00020. [DOI] [PubMed] [Google Scholar]
- 40.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio S, Cauthen JC, Ozuna RM. A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J. 2004;13:22–31. doi: 10.1007/s00586-003-0581-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Zucherman JF, Hsu KY, Hartjen CA, Mehalic TF, Implicito DA, Martin MJ, Johnson DR, 2nd, Skidmore GA, Vessa PP, Dwyer JW, Puccio ST, Cauthen JC, Ozuna RM. A multicenter, prospective, randomized trial evaluating the X STOP interspinous process decompression system for the treatment of neurogenic intermittent claudication: two-year follow-up results. Spine. 2005;30:1351–1358. doi: 10.1097/01.brs.0000166618.42749.d1. [DOI] [PubMed] [Google Scholar]