Abstract
Interspinous implants are used to treat lumbar spinal stenosis or facet joint arthritis. The aims of implanting interspinous devices are to unload the facet joints, restore foraminal height and provide stability especially in extension but still allow motion. The aim of this in vitro study was to compare four different interspinous implants––Colfex, Wallis, Diam and X-Stop––in terms of their three-dimensional flexibility and the intradiscal pressure. Twenty-four human lumbar spine specimens were divided into four equal groups and tested with pure moments in flexion/extension, lateral bending and axial rotation: (1) intact, (2) defect, (3) after implantation. Range of motion and the intradiscal pressure were determined.In each implant-group the defect caused an increase in range of motion by about 8% in lateral bending to 18% in axial rotation. Implantation had similar effects with all four implants. In extension, Coflex, Wallis, Diam, and X-Stop all overcompensated the instability caused by the defect and allowed about 50% of the range of motion of the intact state. In contrast, in flexion, lateral bending and axial rotation the values of the range of motion stayed about the values of the defect state. Similarly the intradiscal pressure after implantation was similar to that of the intact specimens in flexion, lateral bending and axial rotation but much smaller during extension. All tested interspinous implants had a similar effect on the flexibility: they strongly stabilized and reduced the intradiscal pressure in extension, but had almost no effect in flexion, lateral bending and axial rotation.
Keywords: Lumbar spine, Interspinous implant, Biomechanics, Flexibility, Intradiscal pressure
Introduction
Many different surgical treatments for degenerative lumbar spinal stenosis exist. The most commonly used therapy is a decompressive surgery. The success of this therapy reported in the literature varies from moderate to excellent results, depending on the point of interest for example pain reduction or neurological deficit [1, 10, 12]. One of the problems associated with decompression surgery is the creation of an instability as a consequence of the degeneration of the disc, the facetectomy or a combination of both [3]. Therefore different methods of restabilization have been developed for example rigid stabilization systems with pedicle screw fixation [18]. However rigid systems are accused to increase the loads acting on the adjacent segments, which may lead to accelerated degeneration. To prevent such overloading dynamic stabilization systems have been established [9].
Interspinous implants are used for motion-preserving stabilization of primarily posterior lumbar spinal pathologies like spinal stenosis or facet joint arthritis [8]. The aims are to unload the facet joints, to restore foraminal height and to provide sufficient stability especially in extension but still allow motion in the treated segment.
This technology is still in an early stage of development and the indications are not yet clearly defined because scientific evidence is lacking [2, 13]. Yet, there are already several interspinous implants on the market today. Their design strongly varies and they are made of different materials. However, whether these differences influence their biomechanical behavior is still unknown.
The purpose of this biomechanical in vitro study was to investigate the segmental stability and intradiscal pressure achieved with the following four interspinous implants: Coflex, Wallis, Diam, and X-Stop.
Materials and methods
Implants
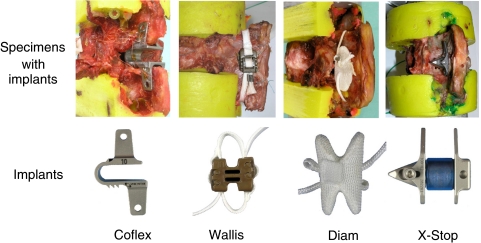
Four different interspinous implants were tested in the present study (Fig. 1).
Fig. 1.
Implants tested in this study; in the upper line implants placed in the specimen for better illustration
The Coflex implant (Paradigm Spine, Wurmlingen, Germany) is a “U” shaped interspinous spacer made of titanium. The interspinous and supraspinous ligament have been resected during implantation in this test. Then, its four lateral wings are crimped to the spinous processes to secure the implant in place.
The Diam implant (Medtronic Sofamor Danek, Paris, France) is a silicone interspinous spacer. It is covered with a polyethylene coat. The two ligatures secure it in place. For this implant, only the interspinous space has to be prepared while the supraspinous ligament can be left intact.
The Wallis implant (Abbott Laboratories, Bordeaux, France) is an interspinous spacer, which is composed of polyetheretherketone. Similarly to the Coflex implant, both, the interspinous and supraspinous ligament have to be resected. The implant is secured in place with two ligatures. They are wrapped around the two adjacent spinous processes. After implantation the supraspinous ligament is refixed in place with stitches.
The X-Stop implant (St Francis Medical Technologies, Alameda, USA) is an oval titanium interspinous implant, which is similary to the Coflex secured in place with two lateral wings. However, these wings are not crimped to the spinous processes. In order to be able to implant the X-Stop, only the interspinous ligament has to be pierced.
Specimens and preparation
For this study, 24 fresh frozen human lumbar spine specimens (12 × L2–L3 and 12 × L4–L5) were used. The specimens were freshly dissected and frozen at −20°C until testing. Lateral and postero-anterior X-rays were taken prior testing and the degree of disc degeneration was estimated [15]. As far as possible, specimens with severe degeneration were then excluded from testing.
Before testing the specimens were thawed overnight at 4°C and prepared at room temperature. All soft tissue was removed, leaving the discs, ligaments and joint capsules intact. Then, the upper half of the cranial vertebra and the lower half of the caudal vertebra were embedded in polymethylmethacrylate (PMMA, Technovit 3040, Heraeus Kulzer, Wehrheim, Germany) ensuring that the middle disc was aligned horizontally. Before the embedding process several screws were fixed in the upper and lower vertebra in order to improve the fixation between vertebra and PMMA. Flanges were fixed to the cranial and caudal PMMA blocks to mount the specimens in a spine tester.
The specimens where divided into four similar groups. Removal of the interspinous ligament (ISL) and/or supraspinous ligament (SSL) was not necessary for all implants, therefore different specimens were used and the implants have not been tested in the same specimens. To make the results of the different implant groups comparable, each group consisted of the same number L2/L3 and L4/L5 segments and was matched according to their age. In the Coflex group the average age was 55 years, in the Wallis group 54, in the Diam group 52 and in the X-Stop group 53 years.
Test procedure
Before testing an intradiscal pressure (IDP) transducer (FMSPEZ50, MIPM GmbH, Mammendorf, Germany) was implanted into the nucleus of the disc, the position was checked by X-rays in lateral and postero-anterior direction. The flexibility tests were conducted in a spine tester (Fig. 2). First the specimens were tested in the intact state, then the test was repeated after creating the defect and again after implantation. The defect consisted of a bilateral hemifacetectomy (the lower two third of the inferior articular process has been resected) with a resection of both flaval ligaments. This defect was the same in all four implant-groups. All implantations were carried out according to the instructions provided by the manufactures as described above.
Fig. 2.
Specimen with intradiscal pressure transducer mounted in the spine tester
As recommended for spinal implant testing, pure moments of ±7.5 Nm were applied without preload in lateral bending right/left, flexion/extension and axial rotation left/right [16]. The motor speed was 0.5°/s in every loading direction. The three-dimensional rotational movements of the segment were recorded using rotary variable displacement transducers (P2701A502, Novotechnik, Ostfildern, Germany; resolution 0.1°), which are integrated into the spine tester. During loading the specimens were allowed to move unconstrained in the five uncontrolled degrees of freedom. The bending moments, which were applied, and the resulting rotations of the specimens were recorded continuously. Two loading cycles were applied for preconditioning, the third cycle was used for evaluation.
Data analysis
From the third loading cycle, Range of motion (ROM) was determined. Range of motion was defined as the deformation at + and −7.5 Nm. Surgical procedures can cause the treated segment to become tilted. In the present study the creation of the defect and the implantation of the implants again caused such a tilting in the sagittal plane which was also evaluated. The tilt was determined from the offset of the neutral position (0 Nm) between the intact (0°) and the new neutral position after the surgical manipulation.
The intradiscal pressure was plotted against the bending moment, which was applied. Since such measurements of the intradiscal pressure are only possible in non- or only mildly-degenerated discs (grade 0 or in maximum grade 1) they could only be evaluated exemplarily in this study.
Statistical evaluation
Since only six specimens were tested in each group, a normal distribution of the data could not be assumed. Therefore, median values with ranges are reported and the statistical tests used were all non-parametric.
The four implant groups did not show any significant differences in the intact state and none in the defect state (P > 0.05, Kruskal–Wallis test). Therefore they were lumped together to evaluate the effect of the defect on ROM. For this purpose, Wilcoxon signed rank tests were applied. Further Wilcoxon signed rank tests were used for comparisons between the intact and implanted conditions, however, within each implant group separately. The intact condition was used as a reference instead of the defect state, since the aim was to evaluate whether the implants have any effect on the flexibility of the intact specimens. Yet, in a descriptive way, the defect and implanted states were still compared to each other.
Wilcoxon rank sum tests were used to determine statistical differences of the ROM between the four implant groups in the intact state, with the defect and after implantation as well as the differences between the four groups concerning the segmental tilt caused by implantation. Since this study was explorative, the P values were not corrected for multiple comparisons.
Results
In the intact state all four groups showed similar ROM (P > 0.05) data and therefore create a good baseline for the following comparisons (Figs. 3, 4, 5). This was also the case for the defect condition. Therefore, the four groups were put together to evaluate the effect of the defect on the ROM. However, after implantation, each group was evaluated separately.
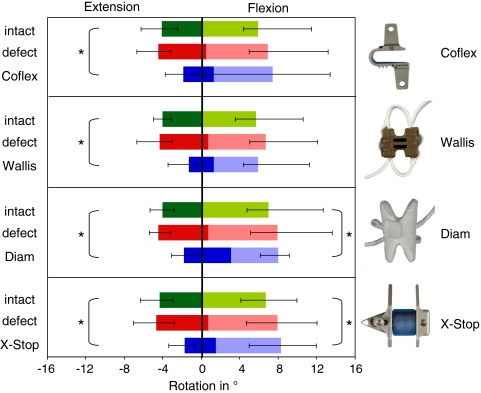
Fig. 3.
Range of motion (ROM) in flexion and extension for the intact, the defect condition and after implantation. Values are median with minimum and maximum.*P < 0.05 for comparisons between implanted and intact condition in each of the four groups (Wilcoxon signed rank test). The border between the light and the darkbars represents the median segmental tilt caused by defect (red) and by implantation (blue)
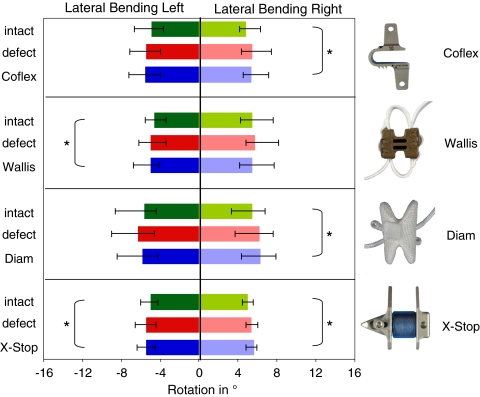
Fig. 4.
Range of motion (ROM) in lateral bending for the intact, the defect condition and after implantation. Values are median with minimum and maximum. *P < 0.05 for comparisons between implanted and intact condition in each of the four groups (Wilcoxon signed rank test)
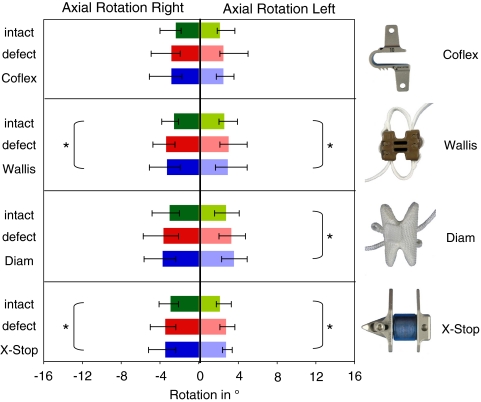
Fig. 5.
Range of motion (ROM) in axial rotation for the intact, the defect condition and after implantation. Values are median with minimum and maximum. *P < 0.05 for comparisons between implanted and intact condition in each of the four groups (Wilcoxon signed rank test)
Segmental tilt
Creation of the standardized defect caused a slightly kyphotic deformation of the specimens. This kyphosis ranged between 0.5° and 0.7° in median (Fig. 3) compared to the intact state (0°). Again all four groups behaved very similar. After implantation, however, this segmental tilt became different between the four implant-groups. While implantation of the Diam caused an increasing kyphosis, implantation of the Wallis or X-Stop had almost no effect on the kyphosis caused by the defect (P < 0.05 between Diam and Wallis and Diam and X-Stop). This also applies to the Coflex, however, in this group the range of the single values was larger. In the Coflex group one specimen went into lordosis in all other implant groups all specimens went into kyphosis after implantation.
Range of motion
In general, the defect caused an increase in ROM compared to the intact condition in all loading directions. This resulted in a ROM, which was similar in all four groups (P > 0.05). Implantation of the Coflex, Wallis, Diam and X-Stop could not compensate this destabilizing effect in none of the three loading directions, except for extension.
In flexion/extension, the defect had a destabilizing effect (P < 0.05), yet the increase of the ROM was in median only about 10% in extension and about 14% in flexion (Fig. 3). In extension if referred to the neutral position of the intact condition all implants had a stabilizing effect (P < 0.05, Wilcoxon signed rank test). They all allowed in median no more than 50% of the range of motion in the intact state (Fig. 3). In this loading direction there were no differences between the four implant groups (P > 0.05, Wilcoxon rank sum test). The behavior of all implants in flexion if referred to the neutral position of the intact condition was also similar. The implants Coflex, Diam and X-Stop allowed more flexion than in the intact state but about the same as or little more than with the defect, while the Wallis implant tended to restabilize the specimens to the values of the intact specimens. In the Coflex group there was a large range of the single values which indicates that crimping probably sometimes provides a good anchorage to the spinous processes but sometimes also loosens. If referred to the neutral position of the implanted state, the Diam showed the largest amount of extension.
In lateral bending, the increase of the ROM caused by the defect was only about 10% (P ≤ 0.05) (Fig. 4). Generally, the implants Coflex, Wallis, Diam and X-Stop allowed slightly more motion compared to the intact state (Fig. 5). Compared to the defect, however the four implants had neither a stabilizing nor a destabilizing effect. There was no strongly difference between the four implant-groups (P > 0.05, Wilcoxon rank sum test).
In axial rotation the defect caused a larger increase of the range of motion than in flexion/extension and lateral bending. In this loading direction an increase by about 20% was found (P < 0.05) (Fig. 5). Generally, the implants were not able to compensate this destabilization. Compared to intact, the ROM strongly increased only with the Wallis and the X-Stop and to one side also with the Diam (P < 0.05, Wilcoxon signed rank test (Fig. 5). Nevertheless, the four implant groups did not differ strongly from each other (P > 0.05, Wilcoxon rank sum test).
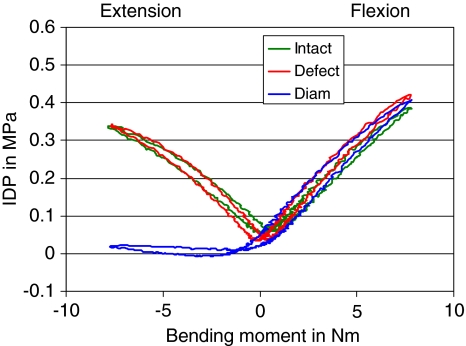
Intradiscal pressure
In all four implant groups, the intradiscal pressure was strongly released in extension (Fig. 6). In all other loading directions flexion, lateral bending and axial rotation, none of the implants caused a significant change in the intradiscal pressure.
Fig. 6.
Intradiscal pressure (IDP) in flexion and extension for the intact condition the defect condition and after implantation. Exemplary curve for Diam-Implant
Discussion
In the present study, the primary stabilizing effect of four interspinous implants for the lumbar spine was investigated and the intradiscal pressure of the motion segment was measured in in vitro flexibility tests. It was shown, that all implants had very similar effects despite of their very different designs. There was a stabilizing effect and a decrease of the intradiscal pressure in extension for all implants, while flexion, lateral bending and axial rotation was almost unaffected by implantation.
For this study L2–L3 and L4–L5 segments were used. Besides the segments L5-S1 and L3–L4 these are most commonly affected by degenerative diseases and, thus, are susceptible for being treated with an interspinous implant. The applied defect, a bilateral hemifacetectomy, with a resection of both flaval ligaments is a clinically ISL relevant defect, which can be used for decompression. Yet, in clinical practice the defects created for decompression may sometimes also be smaller. Nonetheless, for this study a big defect was chosen to get clearer differences between the four implants. One of the four implants tested in this study––the X-Stop––is intended to be clinically used only without decompression.
For the flexibility tests pure bending moments of ±7.5 Nm without preload were applied as recommended for lumbar spine in vitro testing [16]. Furthermore, it could be shown that this load is almost physiological if the anterior column of the spine is intact [7]. During loading the specimens were allowed to move unconstrained in the five uncontrolled degrees of freedom.
As expected all four interspinous implants had the best stabilizing effect in extension. Less stability was achieved in flexion. Even though the four implant groups did not significantly differ in ROM, the Wallis tended to results in the most stable condition in flexion. In this implant group, the ROM of the intact specimen was restored, i.e. the destabilizing effect of the defect was reversed. Further stabilization was not achieved probably since the fixation of the two ligatures around the spinous processes and the interspinous blocker is not strong enough. The Diam, although also fixed to the spinous processes using ligatures had no restabilizing effect. Thus, the type of fixation is probably less efficient. In the Coflex group, there was a great range of the ROM noticed in flexion. This could be explained by the crimping of the wings to the spinous process. In some cases crimping of the wings caused a connection between implant and spinous process strong enough to resist flexion movements, in other cases this connection immediately loosened. This emphasizes the need to use specific forceps meanwhile supplied by the distributers of the Coflex. Independently to the used implant the ROM in axial rotation and lateral bending were similar.
Only a few reports of in vitro flexibility tests of interspinous implants are available in the literature for comparison. Most data about the biomechanical behavior of interspinous implants were gathered using the X-Stop [7, 11, 17]. Lindsey et al. [7] could show for example, that the ROM in flexion-extension was significantly reduced at the instrumented level, whereas there was no significant effect for the other directions. Compared with our observations Lindsey et al. could show that the sagittal angle was affected by implantation, the specimens were in a more flexed, i.e. kyphotic position. Therefore, interpretation of the absolute ROM is difficult. Unfortunately, in vitro stability tests only reflect the acute postoperative stability. Biological effects can therefore not be predicted.
Hydrostatic pressure can only be found in healthy non- (or mildly-) degenerated intervertebral discs [5, 14]. In more severely degenerated discs this hydrostatic pressure turns into a non-hydrostatic pressure, which varies within one and the same nucleus pulposus depending on the position of the transducer. The recorded values therefore no more represent the overall intradiscal pressure but rather a kind of local non-hydrostatic pressure, which cannot properly be interpreted. Unfortunately, intervertebral disc degeneration has a high prevalence in the population. Most of the specimens tested in this study were already more than only mildly degenerated and, thus, no more suitable for reliable intradiscal pressure measurements. Nevertheless, in each implant group, at least one segment could be evaluated. Parallel to this reported one we performed a similar study with calf spines, where we tested only non-degenerated discs[6]. They showed the same behavior as described here. We could show that the pressure decreased in extension with all implants. This is also in agreement with a study by Swanson et al. [11] using the X-Stop, who measured the intradiscal pressure at the instrumented and the adjacent levels with the same study design as Lindsey et al. [7]. They could show, that there was a strong decrease of the IDP in the instrumented segment during extension without significant effect at the adjacent levels. This is resulting from the restricted extension, which probably lead to a smaller bulging of the posterior annulus and thus to less narrowing of the spinal canal. Physiological loading of the disc therefore seems to be the most advantageous condition, which is the case after implantation of all tested interspinous implants in all load directions except for extension [4].
Overall, it can be concluded from this study that the interspinous implants Coflex, Wallis, Diam and X-Stop had a similar effect on the flexibility of the treated segments despite of their various designs: referred to the neutral position of the intact segments, they significantly stabilized and unloaded the disc in extension, but had little effect on range of motion and intradiscal pressure in flexion, lateral bending and axial rotation. Other parameters such as center of rotation, facet joint loading or the dynamic effect of the implants (e.g from the spring design of the Coflex) will be the purpose of further studies.
Acknowledgments
The authors gratefully acknowledge Paradigm Spine for financial support.
References
- 1.Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleas F. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10-year study. Spine. 2000;25(11):1424–1435. doi: 10.1097/00007632-200006010-00016. [DOI] [PubMed] [Google Scholar]
- 2.Christie SD, Song JK, Fessler RG. Dynamic interspinous process technology. Spine. 2005;30(16 Suppl):S73–S78. doi: 10.1097/01.brs.0000174532.58468.6c. [DOI] [PubMed] [Google Scholar]
- 3.Fujiwara A, Tamai K, An HS, Kurihashi T, Lim TH, Yoshida H, Saotome K. The relationship between disc degeneration, facet joint osteoarthritis, and stability of the degenerative lumbar spine. J Spinal Disord. 2000;13(5):444–500. doi: 10.1097/00002517-200010000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Guehring T, Unglaub F, Lorenz H, Omlor G, Wilke HJ, Kroeber MW. Intradiscal pressure measurements in normal discs, compressed discs and compressed discs treated with axial posterior disc distraction: an experimental study on the rabbit lumbar spine model. Eur Spine J. 2006;15(5):597–604. doi: 10.1007/s00586-005-0953-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Höjer S, Krantz M, Ekström L, Kaigle A, Holm S. A microstructure based fiberoptic pressure sensor for measurements in lumbar intervertebral discs. Proc SPIE (in revision) 1999;3570:115–122. doi: 10.1117/12.336921. [DOI] [Google Scholar]
- 6.Kettler A, Liakos L, Haegele B, Wilke HJ. Are the spines of calf, pig and sheep suitable models for pre-clinical implant tests? Eur Spine J. 2007;16(12):2186–2192. doi: 10.1007/s00586-007-0485-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindsey DP, Swanson KE, Fuchs P, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on the kinematics of the instrumented and adjacent levels in the lumbar spine. Spine. 2003;28(19):2192–2197. doi: 10.1097/01.BRS.0000084877.88192.8E. [DOI] [PubMed] [Google Scholar]
- 8.Minns RJ, Walsh WK. Preliminary design and experimental studies of a novel soft implant for correcting sagittal plane instability in the lumbar spine. Spine. 1997;22(16):1819–1825. doi: 10.1097/00007632-199708150-00004. [DOI] [PubMed] [Google Scholar]
- 9.Schmoelz W, Huber JF, Nydegger T, Dipl I, Claes L, Wilke HJ. Dynamic stabilization of the lumbar spine and its effects on adjacent segments: an in vitro experiment. J Spinal Disord Tech. 2003;16(4):418–423. doi: 10.1097/00024720-200308000-00015. [DOI] [PubMed] [Google Scholar]
- 10.Simotas AC, Dorey FJ, Hansraj KK, Cammisa F., Jr Nonoperative treatment for lumbar spinal stenosis. Clinical and outcome results and a 3-year survivorship analysis. Spine. 2000;25(2):197–203. doi: 10.1097/00007632-200001150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Swanson KE, Lindsey DP, Hsu KY, Zucherman JF, Yerby SA. The effects of an interspinous implant on intervertebral disc pressures. Spine. 2003;28(1):26–32. doi: 10.1097/00007632-200301010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Turner JA, Ersek M, Herron L, Deyo R. Surgery for lumbar spinal stenosis. Attempted meta-analysis of the literature. Spine. 1992;17(1):1–8. doi: 10.1097/00007632-199201000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Whitesides TE., Jr The effect of an interspinous implant on intervertebral disc pressures. Spine. 2003;28(16):1906–1907. doi: 10.1097/01.BRS.0000084662.02029.B2. [DOI] [PubMed] [Google Scholar]
- 14.Wilke HJ, Wenger K, Claes L. Testing criteria for spinal implants: recommendations for the standardization of in vitro stability testing of spinal implants. Eur Spine J. 1998;7(2):148–154. doi: 10.1007/s005860050045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wilke HJ, Neef P, Caimi M, Hoogland T, Claes LE. New in vivo measurements of pressures in the intervertebral disc in daily life. Spine. 1999;24(8):755–762. doi: 10.1097/00007632-199904150-00005. [DOI] [PubMed] [Google Scholar]
- 16.Wilke HJ, Rohlmann F, Neidlinger-Wilke C, Werner K, Claes L, Kettler A. Validity and interobserver agreement of a new radiographic grading system for intervertebral disc degeneration: part I. Lumbar spine. Eur Spine J. 2006;15(6):720–730. doi: 10.1007/s00586-005-1029-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wiseman CM, Lindsey DP, Fredrick AD, Yerby SA. The effect of an interspinous process implant on facet loading during extension. Spine. 2005;30(8):903–907. doi: 10.1097/01.brs.0000158876.51771.f8. [DOI] [PubMed] [Google Scholar]
- 18.Zindrick MR, Wiltse LL, Widell EH, Thomas JC, Holland WR, Field BT, Spencer CW. A biomechanical study of intrapeduncular screw fixation in the lumbosacral spine. Clin Orthop. 1986;203:99–112. [PubMed] [Google Scholar]