Abstract
The Weight Control Smoking Scale (WCSS), originally developed as part of a Reasons for Smoking Scale, includes 3 items (smoke to avoid weight gain; smoke to control appetite; less hungry when smoking). Although widely used, it has not previously been subjected to psychometric analysis. To fill this gap, we analyzed data from 1,512 smokers. WCSS score correlated significantly and positively with the Dieting and Bingeing Severity Scale, self-efficacy about relapse if post-cessation weight gain occurred, increased appetite/weight gain as a withdrawal symptom, and the Three Factor Eating Questionnaire subscales, and negatively with Body Satisfaction. Cronbach’s alpha was .834. Female participants scored significantly higher than males. When only Black and White smokers were included, a significant interaction emerged such that White women scored higher than any other category. In a subsample of 50 smokers who completed the questionnaire twice, test-retest correlations were significant for all items and for the scale as a whole. Overall, our results suggest that the WCSS is a reliable and valid instrument that lends itself to use as a screening tool.
Keywords: appetite, postcessation weight gain; smoking, withdrawal symptoms
1. Introduction
Smoking suppresses appetite and body weight (Klesges, Meyers, Klesges, & La Vasque, 1989), and smoking cessation is commonly associated with weight gain—in some instances, substantial weight gain (Williamson, Madans, Anda, Kleinman, Giovino, & Byers, 1991). Many smokers, especially women, endorse the use of smoking as a weight-management tool and dieting strategy (Klesges & Klesges, 1988). Considerable evidence has been amassed showing that such concerns constitute a barrier to successful quitting (Klesges & Klesges, 1988; Sorensen, Goldberg, Ockene, Klar, Tannenbaum, & Lemeshow, 1992), and even to making an attempt to quit smoking (Weekley, Klesges, & Relyea, 1992; Namenek & Pomerleau, 2000). Women with disordered eating patterns (e.g., clinical or subclinical binge eating disorder or bulimia) are over-represented among smokers (Anzengruber et al., 2006; Pomerleau & Krahn, 1993) and are especially likely to report strong concerns about postcessation weight gain (Pomerleau, Zucker, & Stewart, 2001). (See Saules, Tate, and Pomerleau [in press] for a detailed review of this topic.) These facts underscore the need for a standard, psychometrically sound measure of weight control smoking that can be easily administered in both research and clinical settings to identify smokers who are resistant to smoking cessation treatment because of weight concerns and to serve as a marker of maladaptive eating behavior in this population.
The Weight Control Smoking Scale (WCSS; Pomerleau, Ehrlich, Tate, Flessland, & Pomerleau, 1993) was originally developed to supplement a version of the self-report Smoking Motivation Scale developed by Russell and colleagues (Russell, Peto, & Patel, 1974) and modified to include 3 items per subscale (Tate, Pomerleau, & Pomerleau, 1994). The scale specifically focuses on smoking-related concerns about weight and appetite, which may be more relevant to smoking-cessation outcomes than weight concerns in general (Jeffery, Hennrikus, Lando, Murray, Liu, 2000).
Although the WCSS has been extensively used by the authors and their colleagues (e.g., Pomerleau, 1996; Pomerleau & Kurth, 1996; Pomerleau, Namenek Brouwer, & Jones, 2000, Namenek Brouwer & Pomerleau, 2000; Pomerleau, Zucker & Stewart, 2001, Pomerleau, Zucker, Namenek Brouwer, Pomerleau, & Stewart, 2001; Zucker, Harrell, Miner-Rubino, Stewart, Pomerleau, & Boyd, 2001), it has not previously been subjected to psychometric analysis. To fill this gap, we assembled a database of daily smokers who completed this scale as part of the baseline battery for laboratory experiments and clinical trials. Test-retest reliability was studied in a subsample of smokers who had taken the test on more than one occasion.
2. Method
2.1 Participants
Participants were regular daily smokers recruited from the local community to participate in laboratory investigations of smoking and nicotine dependence and of the genetics of smoking, and in clinical trials of smoking cessation medications. Data collected in studies focused on weight concerns were excluded in order to obtain an approximation of a random sample with respect to key variables. Consent for the collection of data via a standard baseline assessment battery was obtained, and individuals who did not qualify for subsequent participation in a laboratory study or clinical trial were paid for completing this battery. The resulting sample included 1,512 smokers. A subsample of 50 individuals who participated in more than one study not focused on weight concerns and had therefore taken the test twice was also assembled.
2.2. Study instruments
The Weight Control Smoking Scale (WCSS; Pomerleau et al., 1993) consists of 3 items: 1) ”I smoke to keep from gaining weight”; 2) ”Smoking helps me control my appetite”; 3) ”I don’t get so hungry when I smoke.” Response options are 0 (not at all), 1 (a little), 2 (quite a bit), and 3 (very much so), yielding a total score ranging from 0 to 9. The three items were embedded in the modified Smoking Motivation Scale (Russell et al., 1974; Tate et al., 1994):
The following instruments were also administered: the Fagerstrom Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker, & Fagerström, 1991), rated on a scale of 0 to 10; the Dieting and Bingeing Severity Scale (DBSS; Kurth, Krahn, Nairn, & Drewnowski, 1995); and the Three Factor Eating Questionnaire (TFEQ; subscales Cognitive Restraint, Disinhibition, and Hunger; Stunkard & Messick, 1985).
Three single-item measures were also used. Body satisfaction (taken from the DBSS) was queried as follows: “I am satisfied with the shape of my body”, rated on a scale of 1 (never) to 5 (always). Self-efficacy about relapse if post-cessation weight gain occurred (taken from the Nicotine Research Laboratory’s baseline smoking history) was evaluated as follows: “How concerned are you that you might relapse to smoking because of gaining weight after you quit?”, rated on a scale of 1 (not at all) to 3 (very). Increased appetite/weight gain as a withdrawal symptom (also taken from the Nicotine Research Laboratory’s baseline smoking history) was assessed as follows: “Please rate the extent to which you experienced [increased appetite/weight gain] because you were unable to smoke cigarettes due to either restrictions on smoking or because you were trying to quit”, rated on a scale of 1 (not at all) to 4 (severe).
Smoking history and demographics were collected via standard assessments in use by the Nicotine Research Laboratory.
2.3 Data analysis
Internal consistency was calculated using Cronbach’s alpha. External validity was calculated by conducting pairwise correlations of scale scores with the DBSS, TFEQ, body satisfaction, self-efficacy about maintaining abstinence in the face of weight gain, and increased appetite/weight gain during previous periods of abstinence. Face validity based on expected sex and race differences were analyzed using t-tests and ANOVA. Test-retest reliability was computed by correlating scores on two different test administrations in a subset of the sample.
3. Results
3.1 Sample characteristics
The sample was 56% female and 80% White. Mean age ± SD was 35.3 ± 12.0. Mean smoking rate was 20.7 ± 9.8 and mean FTND score was 4.9 ± 2.4.
3.2 Measures of validity and reliability
Cronbach’s alpha (N=1,512) was .834.
Correlations of the WCSS with measures related to appetite, eating, weight, and weight-control smoking are shown in Table 1.
Table 1.
Pearson Correlation Coefficients of WCSS (N=216) with measures of disordered eating, body satisfaction, self-efficacy about maintaining abstinence in the face of weight gain, and appetite/weight gain as a withdrawal symptom. Because data for these variables were not available for all cases, sample size for each correlation is indicated.
| Dieting and Bingeing Severity Scale (Kurth et al., 1995) | r = .352, p < .001 (n=760) |
| Three Factor Eating Questionnaire (Stunkard & Messick, 1985): Cognitive Restraint | r = .348, p < .001 (n=717) |
| Three Factor Eating Questionnaire (Stunkard & Messick, 1985): Disinhibition | r = .267, p < .001 (n=735) |
| Three Factor Eating Questionnaire (Stunkard & Messick, 1985): Hunger | r = .128, p < .01 (n=730) |
| Body Satisfaction | r = −.244, p < .001 (n=761) |
| [Lack of] Self-efficacy About Relapse | r = .552, p < .001 (n=984) |
| Increased Appetite/Weight Gain as a Withdrawal Symptom | r = .533, p < .001 (n=482) |
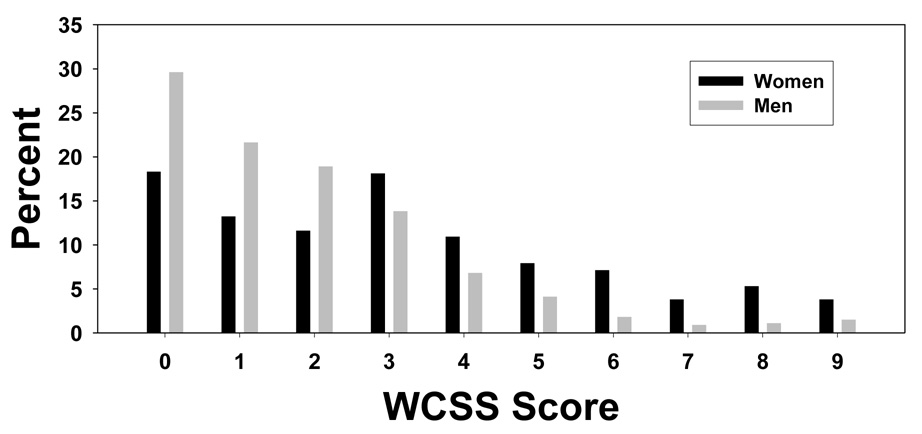
Women scored significantly higher than men on the WCSS (3.19 ±.09 vs. 1.87 ±.08; t = −11.37; p<.001). As seen in Figure 1, distributions for both sexes were skewed to the left.
Figure 1.
Distribution of scores for male and female smokers (N=1,512).
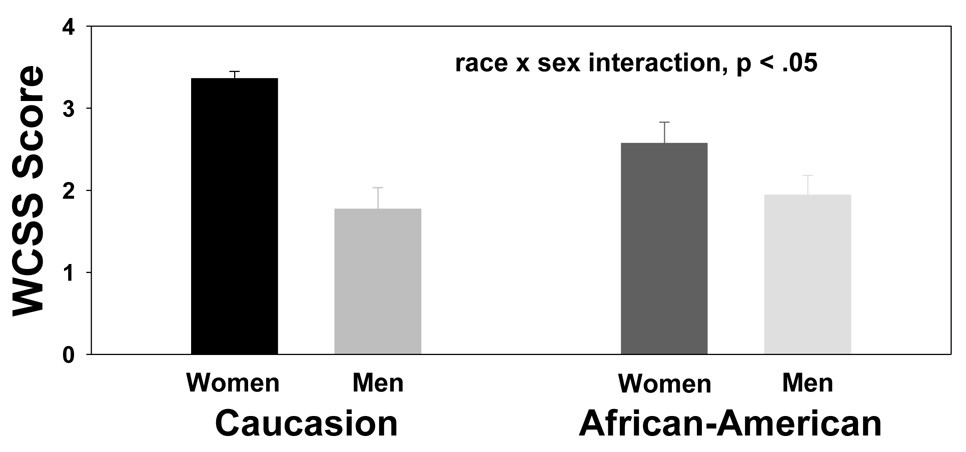
Race differences were tested including only cases self-identifying as either White/Caucasian (n=1,083) or Black/African American (n=170). Sex (women vs. men) was also included as a grouping variable. Results are shown in Figure 2. Although significant race differences were not detected, an interaction effect emerged such that White women scored higher than any other category.
Figure 2.
Race differences, including only White/Caucasian and Black/African American smokers (N=1,253).
The subsample of 50 who completed the scale on two occasions was significantly older (38.5 ±9.6; p<.05), and included a higher proportion of women (72% p<.05) than did the remainder of the sample, but it did not differ on WCSS, number of cigarettes per day, or FTND scores. Controlling for time between administrations (mean ± SD; 2.7 ± 1.9 years), correlations between times 1 and 2 were r=+.742 for the entire scale (p<.01), and r=+.777, r=+.701, and r=+.478 (all p<.01) for items 1, 2, and 3 respectively.
4. Discussion
Scores on the WCSS correlated significantly and positively with measures of self-efficacy about relapse if post-cessation weight gain occurred, increased appetite/weight gain as a withdrawal symptom, disordered eating patterns, and restrained and disinhibited eating, and negatively with body satisfaction. The instrument performed well on measures of internal consistency and test-retest reliability. Strengths of our study include the large sample and the diversity of participants, who were drawn from a variety of studies on smoking and nicotine dependence rather than solely from smoking cessation trials.
Nearly a quarter of the men scored zero, and mean scores for men were significantly lower than those for women. To accommodate these pronounced sex differences, a possible classification scheme would be to categorize men scoring ≥3 and women scoring ≥5—putting them in the top 30% for their sex—as weight control smokers. Note, however, that such a strategy results in many men with scores that would be regarded as normative for women being classified as weight control smokers, and that such men endorse a lower level of “use” of nicotine as a weight management tool than women classified as weight-control smokers. Men with scores truly comparable to women weight control smokers—i.e., ≥5 on the WCSS—constitute only 9.3% of men and must therefore be regarded as an exceptional subset of the smoking population. Before adopting a different cut-point for men, therefore, further research should be carried out to determine whether such a procedure is justified based on differences in outcome (e.g., ability to quit, amount of postcessation weight gain, etc.).
An interesting interaction emerged such that White women appear to be a particularly vulnerable population, consistent with a documented emphasis on slimness in this population (Pomerleau, Zucker, Namenek Brouwer, et al., 2001). While thinness is less a value among African American women, however, it has been shown that they too do not want to be on the “wrong” side of their ideal weight (Pomerleau, Zucker, Namenek Brouwer, et al., 2001). Items tapping into specific issues related to appearance, and testing in more diverse samples, might be helpful in clarifying race and ethnic differences in weight control smoking.
Some caveats are in order. 1) Since the items were embedded in a larger questionnaire, we cannot assess the extent to which the context in which they were administered might have influenced scores. 2) Because the scale consists of only three items, with limited ability to tease apart the related but distinct dimensions of weight concerns, appetite, and body shape, conclusions regarding the reliability, validity, and utility of the scale need to be interpreted with caution. 3) Use of psychometrically-sound measures of body image, body dissatisfaction, and self-efficacy about maintaining abstinence in the face of weight gain instead of unvalidated single items would increase confidence in our findings. 4) Mean smoking rate and degree of dependence in our sample were relatively high; testing in samples including non-daily smokers and a larger representation of less-dependent smokers would improve generalizability. 5) Correlations of the WCSS with variables used to establish external validity were in some instances modest and must therefore be interpreted with caution.
Overall, our findings suggest that the WCSS is a reliable and valid instrument for identifying a broad range of weight-concerned smokers. Being brief, it lends itself to use as a screening tool in both clinical and research settings. Further research will be needed to confirm its predictive value by systematically relating scores to successful quitting and relapse in clinical trials, as well as eating and weight gain; and to determine whether various groups of smokers (e.g., different ethnicities, obese and non-obese, men and women) differ with respect to scale factor structure, internal consistency, relationships to validity criteria, and item mean scores. If the instrument lives up to its promise, it can be used to develop and test more effective methods of enhancing motivation to quit in weight-concerned smokers. Those who are receptive can be referred to behavioral or pharmacological interventions shown to be particularly effective in promoting cessation in such individuals (e.g., Clark, Hays, Vickers, Patten, Croghan, Berg, et al., 2005; Perkins, Marcus, Levine, D'Amico, Miller, Broge, et al., 2001) and/or in managing post-cessation weight gain (e.g., Hays, Hurt, Rigotti, Niaura, Gonzales, Durcan et al., 2001).
Acknowledgments
A preliminary version of this report was presented at the 13th Annual Meeting of the Society for Research on Nicotine and Tobacco in Austin, TX, February, 2007. Preparation of the manuscript was supported in part by Grant HL52981.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anzengruber D, Klump KL, Thornton L, Brandt H, Crawford S, Fichter MM, et al. Smoking in eating disorders. Eating Behaviors. 2006;7:291–299. doi: 10.1016/j.eatbeh.2006.06.005. [DOI] [PubMed] [Google Scholar]
- Clark MM, Hays JT, Vickers KS, Patten CA, Croghan IT, Berg E, et al. Body image treatment for weight concerned smokers: A pilot study. Addictive Behaviors. 2005;30(6):1236–1240. doi: 10.1016/j.addbeh.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Hays JT, Hurt RD, Rigotti NA, Niaura R, Gonzales D, Durcan MJ, et al. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation: A randomized, controlled trial. Annals of Internal Medicine. 2001;135(6):423–433. doi: 10.7326/0003-4819-135-6-200109180-00011. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Hennrikus DJ, Lando HA, Murray DM, Liu JW. Reconciling conflicting findings regarding postcessation weight concerns and success in smoking cessation. Health Psychology. 2000;19(3):242–246. doi: 10.1037//0278-6133.19.3.242. [DOI] [PubMed] [Google Scholar]
- Klesges RC, Meyers AW, Klesges LM, La Vasque ME. Smoking, body weight, and their effects on smoking behavior: a comprehensive review of the literature. Psychological Bulletin. 1989;106:204–230. doi: 10.1037/0033-2909.106.2.204. [DOI] [PubMed] [Google Scholar]
- Kurth CL, Krahn DD, Nairn K, Drewnowski A. The severity of dieting and bingeing behaviors in college women: interview validation of survey data. Journal of Psychiatric Research. 1995;29(3):211–225. doi: 10.1016/0022-3956(95)00002-m. [DOI] [PubMed] [Google Scholar]
- Namenek Brouwer RJ, Pomerleau CS. “Pre-quit attrition” among weight-concerned women smokers. Eating Behaviors. 2000;1:145–151. doi: 10.1016/s1471-0153(00)00014-3. [DOI] [PubMed] [Google Scholar]
- Perkins K, Marcus M, Levine M, D'Amico D, Miller A, Broge M, et al. Cognitive-behavioral therapy to reduce weight concerns improves smoking cessation outcome in weight-concerned women. Journal of Consulting and Clinical Psychology. 2001;69(4):604–613. [PubMed] [Google Scholar]
- Pomerleau CS. Smoking and nicotine replacement treatment issues specific to women (invited article) American Journal of Health Behavior. 1996;20:291–299. [Google Scholar]
- Pomerleau CS, Ehrlich E, Tate JC, Marks JL, Flessland KA, Pomerleau OF. The female weight-control smoker: A profile. Journal of Substance Abuse. 1993;5:391–400. doi: 10.1016/0899-3289(93)90007-x. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Krahn D. Smoking and eating disorders: A connection? Journal of Addictive Diseases. 1993;12:169. [Google Scholar]
- Pomerleau CS, Kurth CL. Willingness of female smokers to tolerate postcessation weight gain. Journal of Substance Abuse. 1996;8:371–378. doi: 10.1016/s0899-3289(96)90215-1. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Namenek Brouwer RJ, Jones LT. Weight concerns in women smokers during pregnancy and postpartum. Addictive Behaviors. 2000;25:759–767. doi: 10.1016/s0306-4603(00)00086-1. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Zucker AN, Namenek Brouwer RJ, Pomerleau OF, Stewart AJ. Race differences in weight concerns among women smokers: Results from two independent samples. Addictive Behaviors. 2001;26:651–663. doi: 10.1016/s0306-4603(00)00148-9. [DOI] [PubMed] [Google Scholar]
- Pomerleau CS, Zucker AN, Stewart AJ. Characterizing concerns about postcessation weight gain: Results from a national survey of women smokers. Nicotine & Tobacco Research. 2001;3:55–64. doi: 10.1080/14622200020032105. [DOI] [PubMed] [Google Scholar]
- Russell MAH, Peto J, Patel V. The classification of smoking by factorial structure of motives. Journal of the Royal Statistics Society. 1974;37:313–346. [Google Scholar]
- Saules KK, Tate JC, Pomerleau CS. Weight control smoking in women. In: Columbus F, editor. Smoking and Women’s Health Research. Hauppauge, NY: Nova Science Publishers, Inc.; (in press). [Google Scholar]
- Sorensen G, Goldberg R, Ockene J, Klar J, Tannenbaum T, Lemeshow S. Heavy smoking among a sample of employed women. American Journal of Preventive Medicine. 1992;8:207–214. [PubMed] [Google Scholar]
- Stunkard AJ, Messick S. The Three-Factor Eating Questionnaire to measure dietary restraint, disinhibition and hunger. Journal of Psychosomatic Research. 1985;29:71–83. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Tate JC, Pomerleau CS, Pomerleau OF. Pharmacological and non-pharmacological smoking motives: a replication and extension. Addiction. 1994;89:321–330. doi: 10.1111/j.1360-0443.1994.tb00899.x. [DOI] [PubMed] [Google Scholar]
- Weekley CK, Klesges RC, Relyea G. Smoking as a weight-control strategy and its relationship to smoking status. Addictive Behaviors. 1992;17:259–271. doi: 10.1016/0306-4603(92)90031-p. [DOI] [PubMed] [Google Scholar]
- Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. New England Journal of Medicine. 1991;324:739–745. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- Zucker AN, Harrell ZA, Miner-Rubino K, Stewart AJ, Pomerleau CS, Boyd CJ. Smoking in college women: The role of thinness pressures, media exposure, and critical consciousness. Psychology of Women Quarterly. 2001;25:233–241. [Google Scholar]