Abstract
Background and objectives: The diagnosis of hypertension among hemodialysis patients by predialysis or postdialysis blood pressure (BP) recordings is imprecise and biased and has poor test-retest reliability. The use of intradialytic BP measurements to diagnose hypertension is unknown.
Design, setting, participants, & measurements: A diagnostic-test study was done with interdialytic ambulatory BP as reference standard. Index BP recordings tested were: predialysis (method 1), postdialysis (method 2), intradialytic (method 3), intradialytic including predialyis and postdialysis (method 4), and the average of predialysis and postdialysis (method 5). Each index BP was recorded over six consecutive dialysis treatments.
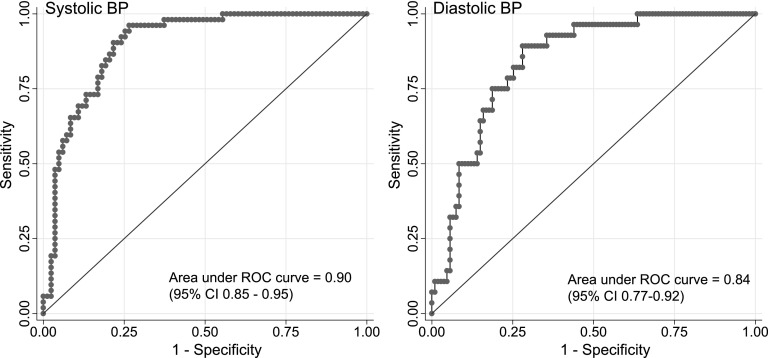
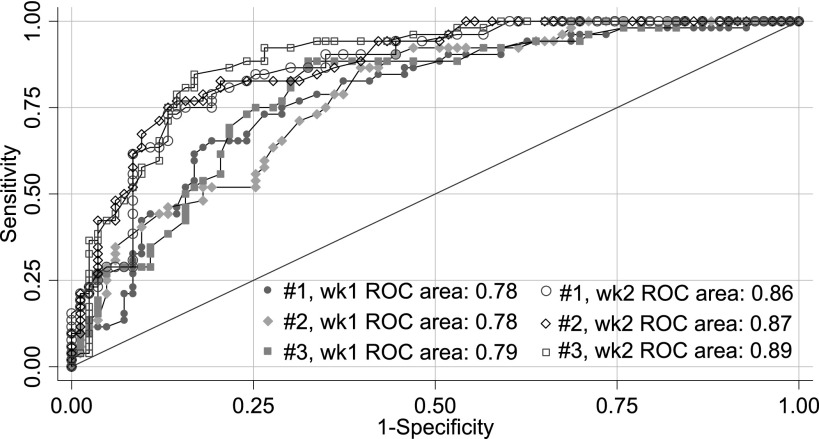
Results: There were differences among index BP measurements in reproducibility, bias, precision, and accuracy. Method 4 was the most reproducible (intraclass correlation coefficient = 0.70 for systolic and diastolic BP). All 5 measurement methods overestimated 44-h ambulatory systolic BP. Methods 2, 3, or 4 overestimated ambulatory systolic BP by only a small amount. Method 4 was the most precise and accurate. For diagnosis of hypertension, BP cut-point by method 4 of 135/75 mmHg, had a sensitivity of 90.4% and specificity of 75.9% for systolic BP (area under ROC curve 0.90). Median cut-off systolic BP of 140 mmHg from a single dialysis provides approximately 80% sensitivity and 80% specificity in diagnosing systolic hypertension; a median cut-off diastolic BP of 80 mmHg provides approximately 75% sensitivity and 75% specificity in diagnosing diastolic hypertension.
Conclusions: Consideration of intradialytic BP measurements together with predialysis and postdialysis BP measurements improves the reproducibility, bias, precision, and accuracy of BP measurement compared with predialysis or postdialysis measurements.
The diagnostic and prognostic significance of hypertension among hemodialysis patients continues to be debated (1,2). Whereas many have suggested that blood pressure (BP) recordings are of little value in managing cardiovascular risk (3,4), others have argued that BP control is important (2,5,6). The accurate measurement of arterial pressure is the essential first step in managing this cardiovascular risk factor, yet the diagnosis of hypertension in hemodialysis patients continues to be a vexing problem (7,8).
Although home BP monitoring is a superior tool to diagnose hypertension, typically BP measurements obtained just before and after dialysis are used to diagnose and treat hypertension in hemodialysis patients (8,9). However, predialysis and postdialysis BP measurements are generally inaccurate estimates of ambulatory BP measurements (10). In the dialysis unit, BP measurements are obtained every 30 min during dialysis, primarily to ensure the hemodynamic stability of patients during treatment. But the BP measurements so obtained are usually ignored when making a diagnosis of hypertension. The utility of intradialytic BP measurements in diagnosing hypertension among hemodialysis patients therefore remains unknown.
The purpose of our study was to evaluate the usefulness of intradialytic BP in diagnosing hypertension among hemodialysis patients. We measured the utility of intradialytic BP by comparing the dialysis-to-dialysis reproducibility and comparing the bias, precision, and accuracy of intradialytic BP measurements to the reference standard of interdialytic ambulatory BP recordings. Finally, we constructed receiver-operating characteristic (ROC) curves to determine clinically useful cut-points and to assess the diagnostic performance of intradialytic BP recordings.
Materials and Methods
Study Cohort
Between September 2003 and February 2005, we recruited 150 patients from four dialysis units staffed by the nephrology faculty of Indiana University, Indianapolis, IN. The performance of predialysis and postdialysis BP measurements has previously been reported (9). The Institutional Review Board of Indiana University and the Research and Development Committee of the VA Medical Center approved this study, and all patients gave their written informed consent.
Intradialytic BP
Over a 2-week period, BP measurements obtained during dialysis were recorded by dialysis technicians or nurses using the oscillometric BP monitor equipped with dialysis machines. Dialysis machines used were Fresenius H 2008, Fresenius K 2008, Cobe Centry III, and Cobe Plus (Fresenius, Waltham, MA; Cobe Laboratories, Lakewood, CO) and were maintained per the protocol of the respective dialysis units. To reflect clinical practice, no technique was specified for measurement of these BP measurements. Typically, measurements were made every 30 min. These measurements were entered into a relational database. Accuracy of data entry into the database was verified by at least two people.
Ambulatory BP Monitoring
Ambulatory BP monitoring was performed after the mid-week hemodialysis session for 44 h. Ambulatory BP measurements were recorded every 20 min during the day (6 a.m. to 10 p.m.) and every 30 min during the night (10 p.m. to 6 a.m.) using a Spacelab 90207 ABP monitor (SpaceLabs Medical, Redmond, WA) in the nonaccess arm, as done previously (11). Recordings began immediately after hemodialysis and terminated immediately before the subsequent dialysis. Accuracy of ambulatory BP recordings was confirmed against auscultated BP at baseline. Data were analyzed using ABP Report Management System software, version 1.03.05 (SpaceLabs Medical). Those patients who had <16 recordings on ambulatory BP were excluded from analysis (n = 15) (12). At least 25 ambulatory recordings were available from each patient.
Index and Reference BP
The following methods were used to define summary measures for various BP recordings:
Method 1. Predialysis: Systolic BP obtained before dialysis for six treatments were averaged. Diastolic BP measurements obtained before dialysis were averaged separately over these six treatments.
Method 2. Postdialysis: Systolic BP obtained after dialysis for six treatments were averaged. Separately, diastolic BP measurements obtained after dialysis were averaged over these six treatments.
Method 3. Intradialytic BP: Systolic BP obtained during a single treatment was averaged. Subsequently, these averages from a single hemodialysis treatment were averaged over 6 treatments to yield a single intradialytic systolic BP. Diastolic BP averages were analogously calculated.
Method 4. Intradialytic BP including predialysis and postdialysis BP: These were done as for intradialytic BP except that predialysis and postdialysis BP measurements were also included before averaging the measurements.
Method 5. Predialysis and postdialysis BP: Systolic BP obtained before and after dialysis was averaged. These averages were then averaged to yield the mean predialysis and postdialysis BP over 6 treatments.
Method 6. Ambulatory BP average: Hourly averages of ambulatory BP were averaged to yield the overall ambulatory BP as the reference BP.
Statistical Analysis
Measurement of Reproducibility.
We calculated for each of the 6 dialysis treatments the following BP measurements: predialysis (method 1), postdialysis (method 2), average intradialytic (method 3), average of all dialysis unit BP measurements (intradialytic + predialysis + postdialysis) (method 4), and the average of predialysis and postdialysis BP measurements (method 5). We first fitted a mixed-effects model with full maximum likelihood estimates where subject was the random variable and systolic BP was a fixed effect (13). Specifically, we fitted the following model yij = β̂ + ζj + ɛij, where yij is the systolic BP for the jth individual (j = 1,…,N) with ith measurement occasion (i = 1,…,6), ζj is random intercept for the jth individual (i.e., the individuals deviation from the overall mean), β̂ is the estimated population mean systolic BP, and ɛij is the error for the jth individual at the ith measurement occasion. ɛij was assumed to distribute normally and independently with a mean of zero and constant variance across individuals. This model provided the SD between subjects and within subjects. Intraclass correlation coefficient was calculated as the between subject variance as a fraction of total variance (between and within subjects). Intraclass correlation coefficient can vary from 0 to 1, and a larger fraction represents greater dialysis-to-dialysis reproducibility.
Next, the statistical significance of the reproducibility was tested by examining the residual variation in BP within individuals from one dialysis to next. We constructed two mixed models. In the first model, systolic BP measured by an index method was used as a fixed effect and subject as the random effect. Specifically, the following model was fitted yij = β̂ + ζj + ɛij, where yij is the systolic BP for the jth individual (j = 1,…, N) on the ith measurement occasion (j = 1,…, 6), ζj is random intercept for the jth individual, and ɛij is the error for the jth individual at the ith measurement occasion. The second model contained systolic BP measured by a specified method as a fixed effect as well as two nested random effects; one random effect was for subjects and another for the measurement method nested within subjects. This three-level model can be written as yijk = β̂ + ζjk + ζk + ɛijk where ζjk is the random intercept for method j and subject k and ζk is the random intercept for subject k. The likelihood ratio test was used to compare the two nested models.
Measurement of Bias.
Average BP measurements were computed by methods 1 through 5. The average ambulatory BP was subtracted from each of these five averaged BP measurements, respectively. Bias was defined as the mean difference in BP from each method compared with ambulatory. The 95% confidence interval for bias was also computed. If the 95% confidence interval included zero, the method was regarded as unbiased. A fixed effects full maximum likelihood estimates model was used to determine the significance of differences in bias between different methods.
Measurement of Precision.
Precision was defined as the variance of the difference between ambulatory and index BP. A mixed-effects model was fitted to test a model testing the differences in BP measurements with fixed effects only and another with method of measurement as a random effect by the likelihood ratio test. The significance of differences among precision of BP recordings with various methods was determined by the likelihood ratio test.
Measurement of Accuracy.
Accuracy was measured as the square root of the sum of the variance and squared bias. This is the definition of the (square) root of the mean square error.
Measurement of Diagnostic Test Performance.
We calculated the area under the curve of ROC curves and their 95% confidence intervals for the model that was most precise, accurate, and reproducible (14). Ambulatory BP of ≥135 mmHg was used to classify patients with systolic hypertension. Ambulatory diastolic BP of ≥85 mmHg was used to classify patients with diastolic hypertension. The best cut-point BP was calculated based on the Youden Index (15). The Youden Index, a measure of overall diagnostic effectiveness, is the maximum vertical distance or difference between the ROC curve and the diagonal or chance line; it occurs at the cut-point that optimizes the BP's differentiating ability when equal weight is given to sensitivity and specificity. Youden Index was calculated as sensitivity + specificity − 1. The higher the index, the better the classification at the cutoff point.
Regression Analysis.
We performed several regression analyses with predialysis, postdialysis, and averaged intradialytic BP measurements and their combinations used to predict the averaged interdialytic ambulatory BP measurements. The nested models were compared with F tests for the goodness-of-model fit.
Sensitivity Analysis.
We asked the question whether method 4 BP could be used during a single mid-week dialysis treatment as a diagnostic test. At the bedside, median BP measurements are easier to calculate, compared with mean BP. Therefore, we reasoned that median BP measurements may provide diagnostically comparable information compared with mean BP measurements obtained by method 4 over six dialysis treatments. Therefore, we calculated the median BP at each of the 6 dialysis treatments and compared the diagnostic performance of these BP measurements (16).
All analyses were performed using Stata 10.0 (Stata, College Station, TX). P values are two sided and significance set at 0.05.
Results
We collected 8620 BP measurements recorded in the dialysis unit among 150 patients over 6 dialysis treatments. Of the estimated 900 dialysis treatments, 25 (2.7%) were missing either because of patient absence or withdrawal of consent.
The clinical characteristics of the patients are shown in Table 1. The population was predominantly black. All patients were dialyzed three times weekly and were prescribed a dialysis time of about 4 h, blood flow rate of approximately 400 ml/min, and dialysate flow rate of approximately 800 ml/min. Comparison of patients who did not have ambulatory BP recording with those who had these recordings did not reveal any significant differences.
Table 1.
Clinical characteristics of the study population
| Clinical Characteristic | All Patients | With 44-h Ambulatory BP | Missing 44-h Ambulatory BP | P |
|---|---|---|---|---|
| N | 150 | 135 | 15 | |
| Age (yr) (mean ± SD) | 55.8 ± 13.5 | 56.3 ± 13.0 | 51.6 ± 17.3 | 0.21 |
| Men | 94 (63%) | 88 (65%) | 6 (40%) | 0.06 |
| Race | 0.72 | |||
| white | 13 (9%) | 11 (8%) | 2 (13%) | |
| black | 135 (90%) | 122 (90%) | 13 (87%) | |
| other | 2 (1%) | 2 (1%) | 0 (0%) | |
| Predialysis weight (kg) (mean ± SD) | 81.8 ± 19.5 | 81.7 ± 19.8 | 82.6 ± 17.8 | 0.87 |
| Postdialysis weight (kg) (mean ± SD) | 79.1 ± 19.0 | 79.0 ± 19.2 | 79.8 ± 17.4 | 0.88 |
| Body mass index (kg/m2) (mean ± SD) | 26.7 ± 6.1 | 26.8 ± 6.2 | 25.9 ± 6.1 | 0.67 |
| Hemodialysis (yr) (mean ± SD) | 4.0 ± 3.0 | 4.0 ± 3.0 | 4.1 ± 2.9 | 0.85 |
| Etiology of end-stage renal disease | 0.85 | |||
| diabetes mellitus | 47 (31%) | 43 (32%) | 4 (27%) | |
| hypertension | 83 (55%) | 75 (56%) | 8 (53%) | |
| glomerulonephritis | 9 (6%) | 8 (6%) | 1 (7%) | |
| obstruction | 1 (1%) | 1 (1%) | 0 (0%) | |
| other | 10 (7%) | 8 (6%) | 2 (13%) | |
| Urea reduction ratio (%) (mean ± SD) | 73.0 ± 7.6 | 73.0 ± 7.5 | 73.4 ± 8.3 | 0.85 |
| Albumin (g/dl) (mean ± SD) | 3.8 ± 0.4 | 3.8 ± 0.4 | 3.8 ± 0.4 | 0.97 |
| Hemoglobin (g/dl) (mean ± SD) | 12.4 ± 1.5 | 12.5 ± 1.5 | 11.9 ± 1.3 | 0.13 |
| No. receiving antihypertensive drugs | 124 (83%) | 112 (83%) | 12 (80%) | 0.77 |
| No. of antihypertensives in users (mean ± SD) | 2.3 ± 1.2 | 2.3 ± 1.2 | 1.9 ± 1.1 | 0.28 |
| Nature of antihypertensive agent | ||||
| dihydropyridine calcium channel blockers | 49 (33%) | 45 (33%) | 4 (27%) | 0.60 |
| non-dihydropyridine calcium-channel blockers | 6 (4%) | 6 (4%) | 0 (0%) | 0.41 |
| β-blockers | 94 (63%) | 85 (63%) | 9 (60%) | 0.82 |
| α-blockers | 8 (5%) | 7 (5%) | 1 (7%) | 0.81 |
| centrally acting agents | 27 (18%) | 25 (19%) | 2 (13%) | 0.62 |
| vasodilators | 20 (13%) | 19 (14%) | 1 (7%) | 0.42 |
| ACE inhibitors | 57 (38%) | 52 (39%) | 5 (33%) | 0.70 |
| angiotension receptor blockers | 22 (15%) | 21 (16%) | 1 (7%) | 0.36 |
| 44-h ambulatory BP (mmHg) (mean ± SD) | NA | 130 ± 22.8/73.6 ± 14.2 | NA |
BP, blood pressure; ACE, angiotensin converting enzyme; NA, not applicable.
Reproducibility
Table 2 shows the reproducibility of the BP measurements from dialysis to dialysis.
Table 2.
Reproducibility of dialysis unit BP measurements
| Method No.Timing | Systolic BP (mmHg) |
Diastolic BP (mmHg) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Systolic BP | SD Between Patients | SD Within Patients | ICC | Mean Diastolic BP | SD Between Patients | SD Within Patients | ICC | ||
| 1 | Pre-HD | 146.6 | 20.7 | 17.2 | 0.59 | 80.0 | 12.3 | 11.0 | 0.56 |
| 2 | Post-HD | 133.1 | 19.6 | 15.5 | 0.62 | 73.1 | 10.6 | 10.4 | 0.51 |
| 3 | Intradialytic | 135.0 | 18.7 | 13.0 | 0.67 | 74.4 | 11.2 | 7.7 | 0.68 |
| 4 | Intradialytic + pre-HD + post-HD | 136.0 | 18.5 | 12.2 | 0.70 | 74.8 | 11.1 | 7.3 | 0.70 |
| 5 | Pre-HD + post-HD | 140.0 | 18.7 | 13.4 | 0.66 | 76.6 | 11.1 | 8.5 | 0.63 |
BP, blood pressure; HD, hemodialysis; ICC, intraclass correlation coefficient.
Systolic BP.
When all 5 measurement methods were considered together, the measurement method accounted for a significant source of variability (P < 0.0001). Between-subject SD was 18.8 mmHg, between-method SD was 4.0 mmHg, and dialysis-to-dialysis SD was 14.4 mmHg.
The reproducibility of predialysis BP or postdialysis BP was lower compared with method 4 (P < 0.0001 and P < 0.01, respectively). Predialysis BP measurements were less reproducible (P < 0.0001) compared with postdialysis BP measurements. The intraclass correlation coefficient for method 4 was the highest.
Diastolic BP.
For diastolic BP measurements, the measurement method did not account for a significant source of variability (P = 0.35). Between-subject SD was 11.3 mmHg, between-method SD was 0.6 mmHg, and dialysis-to-dialysis SD was 9.0 mmHg. Although predialysis BP was less reproducible than method 4 (P < 0.01), no differences in reproducibility could be demonstrated between any of the other methods compared with method 4. Again, the intraclass correlation coefficient for method 4 was the highest.
Bias, Precision, and Accuracy
Table 3 shows the mean difference of the BP measurements compared with the reference standard of 44-h ambulatory BP monitoring (bias), 95% confidence intervals of these differences, the standard differences of differences (precision), and accuracy.
Table 3.
Bias, precision, and accuracy of dialysis unit BP measurements
| Method No.Timing | 44 h-Systolic Ambulatory BP − Systolic BP (mmHg) |
44 h-Diastolic Ambulatory BP − Diastolic BP (mmHg) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Difference Systolic BP | 95% CI of Difference | SD of Difference | Accuracy | Mean Difference Diastolic BP | 95% CI of Difference | SD of Difference | Accuracy | ||
| 1 | Pre-HD | −16.9 | −19.9, −13.8 | 17.8 | 24.5 | −6.2 | 8.0, −4.4 | 10.7 | 12.4 |
| 2 | Post-HD | −4.0 | −6.9, −1.1 | 17.2 | 17.7 | 0.1 | −1.7, 1.9 | 10.6 | 10.6 |
| 3 | Intradialytic | −5.4 | −8.0, −2.8 | 15.2 | 16.1 | −0.9 | −2.6, 0.8 | 10.0 | 10.0 |
| 4 | Intradialytic + pre-HD + post-HD | −6.4 | −8.9, −3.9 | 14.7 | 16.0 | −1.3 | −3.0, 0.3 | 9.7 | 9.8 |
| 5 | Pre-HD + post-HD | −10.6 | −13.1, −8.0 | 15.0 | 18.4 | −3.1 | −4.7, −1.4 | 9.7 | 10.2 |
BP, blood pressure; HD, hemodialysis.
Systolic BP.
All 5 measurement methods overestimated 44-h ambulatory systolic BP. Measurement methods were significantly different from each other (P < 0.0001). On average, postdialysis overestimated systolic BP by 4 mmHg and predialysis BP by 16.9 mmHg. Methods 2, 3, or 4 were similar in bias, but more accurate than method 1 or 5.
When measurement methods were considered together, the measurement method accounted for a significant source of variability (P < 0.0001). Between-subject SD was 14.6 mmHg and between-method SD was 4.1 mmHg. The smallest SD was seen for method 4, making it the most precise.
Consideration of intradialytic systolic BP measurements (model 3 and 4) improved accuracy of estimation of ambulatory systolic BP. Method 4 was also the most accurate.
Diastolic BP.
Only 2 measurement methods (method 1 and 5) overestimated 44-h diastolic ambulatory BP. Measurement methods were significantly different from each other (P < 0.0001). Method 1 was the most biased and significantly more biased compared with all other methods. Method 5 was the next most biased and significantly more biased compared with methods 1 (P < 0.01) and 2 (P < 0.01), but not method 3 (P = 0.06) or method 4 (P = 0.12). Methods 2, 3, and 4 were similar in bias.
The measurement method accounted for a significant source of variability (P = 0.03). Between-subject SD was 9.3 mmHg and between-method SD was 1.0 mmHg. Again, the smallest SD was seen for method 4, one where all BP measurements were used in the calculation. Thus, method 4 was the most precise and also the most accurate.
Diagnostic Performance of Median BP
Figure 1 shows the ROC curves for method 4, with 44-h ambulatory BP as the reference standard. The area under ROC curve for systolic BP was 0.90 (95% CI, 0.85 to 0.95). The area under ROC curve for diastolic BP was 0.84 (95% CI, 0.77 to 0.92). Table 4 shows the sensitivities, specificities, positive likelihood ratio, and negative likelihood ratio for a range of systolic and diastolic BP cut-points.
Figure 1.
Receiver operating-characteristic curves for averaged BP by dialysis treatment over 6 consecutive dialyses.
Table 4.
Diagnostic performance of dialysis unit BP measurements by method 4
| Systolic BP (mmHg) |
Diastolic BP (mmHg) |
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cut-point | Sensitivity | Specificity | LR+ | LR− | Cut-point | Sensitivity | Specificity | LR+ | LR− | ||||||||
| ≥ 125 | 98.1 | 45.8 | 1.81 | 0.04 | ≥ 70 | 96.4 | 43.0 | 1.69 | 0.08 | ||||||||
| ≥ 130 | 96.2 | 63.9 | 2.66 | 0.06 | ≥ 75 | 92.9 | 63.6 | 2.55 | 0.11 | ||||||||
| ≥ 135 | 90.4 | 75.9 | 3.75 | 0.13 | ≥ 80 | 75.0 | 79.4 | 3.65 | 0.31 | ||||||||
| ≥ 140 | 84.6 | 80.7 | 4.39 | 0.19 | ≥ 85 | 50.0 | 88.8 | 4.46 | 0.56 | ||||||||
| ≥ 145 | 73.1 | 86.8 | 5.51 | 0.31 | ≥ 90 | 32.1 | 94.4 | 5.73 | 0.72 | ||||||||
| ≥ 150 | 55.8 | 94.0 | 9.26 | 0.47 | ≥ 95 | 10.7 | 98.1 | 5.73 | 0.91 | ||||||||
| AUC (95% CI) | 0.90 (0.85–0.95) | 0.84 (0.77–0.92) | |||||||||||||||
BP, blood pressure; LR+, likelihood ratio for positive test result; LR−, likelihood ratio for negative test result; AUC, area under receiver operating characteristic curve; CI, confidence interval.
Systolic BP.
The optimal Youden Index of 0.69 was obtained for a cut-point systolic BP of 132.5 mmHg. At this cut-point, the sensitivity for diagnosing hypertension was 96.2%, specificity was 73.5%, positive likelihood ratio was 3.63, negative likelihood ratio 0.05, and 82.2% of patients were correctly classified. At a cut-point BP of 135 mmHg, the Youden Index was 0.66 and 81.5% of the patients were correctly classified. At a cut-point BP of 140 mmHg, the Youden Index was 0.65 and 82.2% of the patients were correctly classified.
Diastolic BP.
The optimal Youden Index of 0.61 was obtained for a cut-point diastolic BP of 76.8 mmHg. At this cut-point, the sensitivity for diagnosing hypertension was 89.3%, specificity was 72.0%, positive likelihood ratio was 3.18, negative likelihood ratio 0.15, and 75.6% of patients were correctly classified. At a cut-point BP of 75 mmHg, the Youden Index was 0.56 and 69.6% of the patients were correctly classified.
Figure 2 shows the ROC curves for method 4, for each of the 6 dialysis treatments. The area under ROC curves were significantly different from each other for systolic BP (χ2 = 14.6, P = 0.01), but not for diastolic BP (χ2 = 10.1, P = 0.07). In general, the dialysis treatments in the second week had higher area under ROC curves compared with the first week.
Figure 2.
Receiver operating-characteristic (ROC) curves for median systolic BP by dialysis treatment. ROC curves for each dialysis treatment are shown. Filled symbols represent the first week of dialysis; open symbols represent the second week of dialysis. The second week of dialysis had area under ROC curves that were larger than that of the first week.
Systolic BP.
Table 5 shows that area under ROC curves were similar for median systolic BP whether the dialysis was first, second, or third in the week. However, the optimal cut-off BP at the Youden Index progressively decreased from 147 mmHg for the first dialysis, 140 mmHg for the second dialysis, and 137 mmHg the third dialysis of the week. Nonetheless, the sensitivities and specificities for the various cut-off BP measurements remained similar regardless of the day of the week.
Table 5.
Diagnostic performance of single dialysis unit systolic BP measurement at median
| Systolic BP Cut-point (mmHg) | Median Systolic BP (mmHg): First Dialysis |
Median Systolic BP (mmHg): Second Dialysis |
Median Systolic BP (mmHg): Third Dialysis |
||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | LR+ | LR− | Sensitivity | Specificity | LR+ | LR− | Sensitivity | Specificity | LR+ | LR− | ||||||||||
| ≥ 125 | 96.2 | 43.4 | 1.70 | 0.09 | 94.2 | 56.6 | 2.17 | 0.10 | 94.2 | 56.6 | 2.17 | 0.10 | |||||||||
| ≥ 130 | 90.4 | 60.2 | 2.27 | 0.16 | 82.7 | 68.7 | 2.64 | 0.25 | 92.3 | 69.9 | 3.06 | 0.11 | |||||||||
| ≥ 135 | 86.5 | 69.9 | 2.87 | 0.19 | 82.7 | 75.9 | 3.43 | 0.23 | 86.5 | 78.3 | 3.99 | 0.17 | |||||||||
| ≥ 140 | 80.8 | 78.3 | 3.72 | 0.25 | 78.9 | 81.9 | 4.36 | 0.26 | 80.8 | 84.3 | 5.16 | 0.23 | |||||||||
| ≥ 145 | 75.0 | 84.3 | 4.79 | 0.30 | 76.9 | 84.3 | 4.91 | 0.27 | 71.2 | 86.8 | 5.37 | 0.33 | |||||||||
| ≥ 150 | 63.5 | 88.0 | 5.27 | 0.42 | 63.5 | 90.4 | 6.58 | 0.40 | 51.9 | 91.6 | 6.16 | 0.53 | |||||||||
| AUC (95% CI) | 0.86 (0.80–0.92) | 0.87 (0.82–0.93) | 0.89 (0.83–0.94) | ||||||||||||||||||
| Youden Index | 0.60 | 0.61 | 0.68 | ||||||||||||||||||
| BP cut-point at Youden Index | 147.0 | 140.0 | 136.0 | ||||||||||||||||||
| % correct classification at Youden Index | 81.5% | 80.7% | 83.7% | ||||||||||||||||||
BP, blood pressure; LR+, likelihood ratio for positive test result; LR−, likelihood ratio for negative test result; AUC, area under receiver operating characteristic curve; CI, confidence interval.
Diastolic BP.
Table 6 shows that area under ROC curves were similar for median diastolic BP measurements regardless of the dialysis day. The optimal cut-off BP at the Youden Index was identical at 78 mmHg regardless of the dialysis day. Also, the sensitivities and specificities for the various cut-off BP measurements remained similar regardless of the day of the week.
Table 6.
Diagnostic performance of single dialysis unit diastolic BP measurement at median
| Diastolic BP Cut-point (mmHg) | Median Diastolic BP (mmHg): First Dialysis |
Median Diastolic BP (mmHg): Second Dialysis |
Median Diastolic BP (mmHg): Third Dialysis |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sensitivity | Specificity | LR+ | LR− | Sensitivity | Specificity | LR+ | LR− | Sensitivity | Specificity | LR+ | LR− | |
| ≥ 70 | 96.4 | 43.0 | 1.69 | 0.08 | 85.7 | 44.9 | 1.55 | 0.32 | 100.0 | 54.2 | 2.18 | 0.00 |
| ≥ 75 | 85.7 | 57.9 | 2.04 | 0.25 | 82.1 | 60.8 | 2.09 | 0.29 | 89.3 | 68.2 | 2.81 | 0.16 |
| ≥ 80 | 78.6 | 72.0 | 2.80 | 0.30 | 75.0 | 71.0 | 2.59 | 0.35 | 75.0 | 83.2 | 4.46 | 0.30 |
| ≥ 85 | 60.7 | 80.4 | 3.09 | 0.49 | 42.9 | 84.1 | 2.70 | 0.68 | 60.7 | 88.8 | 5.41 | 0.44 |
| ≥ 90 | 39.3 | 87.9 | 3.23 | 0.69 | 35.7 | 88.8 | 3.19 | 0.72 | 32.1 | 93.5 | 4.91 | 0.72 |
| ≥ 95 | 25.0 | 94.4 | 4.46 | 0.79 | 32.1 | 91.6 | 3.82 | 0.74 | 14.3 | 95.3 | 3.06 | 0.90 |
| AUC (95% CI) | 0.81 (0.73–0.89) | 0.78 (0.68–0.87) | 0.87 (0.81–0.93) | |||||||||
| Youden Index | 0.53 | 0.51 | 0.65 | |||||||||
| BP cut-point at Youden Index | 78.0 | 78.0 | 78.0 | |||||||||
| % correct classification at Youden Index | 71.1% | 71.9% | 80.7% | |||||||||
BP, blood pressure; LR+, likelihood ratio for positive test result; LR−, likelihood ratio for negative test result; AUC, area under receiver operating characteristic curve; CI, confidence interval.
Regression Analysis
Results of the multiple regression analyses to predict interdialytic ambulatory BP are shown in Table 7. The lowest prediction error, and consequently the highest coefficient of determination, was seen when predialytic, postdialytic, and intradialytic BP measurements were present in the model. The combined dialysis unit BP measurements (model 7) had the best model fit.
Table 7.
Multivariate relationships between dialysis unit BP and ambulatory BP
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | |
|---|---|---|---|---|---|---|---|
| Systolic BP β coefficients | |||||||
| pre-HD | 0.709 | 0.410 | 0.212 | 0.246 | |||
| post-HD | 0.745 | 0.464 | 0.190 | 0.239 | |||
| intradialytic | 0.872 | 0.677 | 0.693 | 0.421 | |||
| constant | 25.9 | 30.2 | 12.0 | 7.7 | 7.2 | 10.7 | 4.9 |
| r2 | 0.471 | 0.489 | 0.570 | 0.577 | 0.583 | 0.577 | 0.595 |
| RMSE | 16.62 | 16.35 | 15.00 | 14.93 | 14.82 | 14.92 | 14.66 |
| P value: model 7 versus model in column | <0.001 | <0.001 | <0.05 | <0.05 | 0.051 | <0.05 | NA |
| Diastolic BP β coefficients | |||||||
| pre-HD | 0.768 | 0.460 | 0.324 | 0.314 | |||
| post-HD | 0.840 | 0.447 | 0.238 | 0.216 | |||
| intradialytic | 0.875 | 0.574 | 0.667 | 0.394 | |||
| constant | 12.3 | 11.9 | 8.4 | 4.1 | 5.0 | 6.4 | 3.3 |
| r2 | 0.481 | 0.464 | 0.520 | 0.535 | 0.544 | 0.528 | 0.550 |
| RMSE | 10.27 | 10.44 | 9.88 | 9.76 | 9.67 | 9.84 | 9.64 |
| P value: model 7 versus model in column | <0.001 | <0.001 | <0.05 | <0.05 | 0.174 | <0.05 | NA |
BP, blood pressure; HD, hemodialysis; RMSE, root mean squared error; NA, not applicable.
Discussion
The major finding of our study is that the averaged BP over several treatments improves the reproducibility, precision, bias, and accuracy of BP measurements in hemodialysis patients. However, averaging many BP readings in a single treatment is resource intensive. Median BP is easier to calculate compared with mean BP. Therefore, we asked the question whether the median BP from one dialysis treatment assists in making a diagnosis of hypertension. The results show that the diagnostic performance of median BP measurements was similar to that of mean BP measurements. Using a median cut-off systolic BP of 140 mmHg provides approximately 80% sensitivity and 80% specificity in diagnosing interdialytic systolic hypertension; a median cut-off diastolic BP of 80 mmHg provides approximately 75% sensitivity 75% specificity in diagnosing interdialytic diastolic hypertension.
Although numerous studies compare the relationship of predialysis and postdialysis BP measurements with ambulatory BP, there are no studies reported to our knowledge to assess the relationship between intradialytic BP and interdialytic recordings (10). Mitra et al. measured BP in hemodialysis patients at arrival to the dialysis unit, after 10 min of rest in a quiet room, and at other time points in relationship to dialysis (17). The authors reported that the BP on arrival to the hemodialysis unit was >20/10 mmHg higher than that in the previous 6 h recorded by ambulatory BP in 15 of 36 (41%) patients. This suggests that BP taken in the dialysis unit without adequate rest in a quiet room can substantially elevate BP; in the 41% of the patients who experienced this increase in BP, the average increment was 25/13 mmHg. Even after resting for 10 min, BP was elevated in 19% of the patients, suggesting true white coat effect or true increase in BP as a result of volume expansion or uremic toxin accumulation. BP measured 20 min after dialysis agreed best with interdialytic ambulatory BP. Our data support the work of Peixoto et al. who reported poor reproducibility of predialysis and postdialysis BP recordings compared with ambulatory BP (18).
Why were intradialytic BP measurements superior estimates of interdialytic ambulatory BP recording? Ambulatory BP recording is an accurate estimate of the arterial pressure and shares a stronger relationship with all-cause mortality compared with BP measurements obtained in the dialysis unit (19). BP increases over the interdialytic period most likely because of accumulation of volume and uremic toxins (20–23). Recent studies using ambulatory BP monitoring estimate that systolic BP increases by 1 mmHg every 4 h and diastolic BP increases by 1 mmHg every 8 h (24). The BP decrease during dialysis countervails the interdialytic increase in BP. Thus, a reciprocal relationship exists between interdialytic increase in BP and intradialytic fall in BP. Because averaging many interdialytic BP measurements over a range of volume states provides an accurate estimate of arterial pressure, we speculate that averaging many intradialytic recordings over a range of volume states during dialysis provided a better relationship with interdialyic ambulatory BP recordings. However, it is unlikely that obtaining greater number of measurements is the sole reason for the superior performance of intradialytic BP measurements to predict interdialytic hypertension. We found that the median BP of a single dialysis treatment had better diagnostic ability than the average of six predialysis or six postdialysis BP measurements alone. We have also reported previously that the greater number of recordings is not the reason why ambulatory BP recordings are superior correlates of left ventricular hypertrophy or mortality outcomes (25). Thus, intradialytic recordings may be ecologically more valid measures of the true barometric load experienced by the arterial tree of the hemodialysis patient.
A limitation of our study is that the majority of the participants were black. Although race should not influence the measurement of BP, whether these data are applicable to nonblacks requires further studies. We did not measure the reproducibility of ambulatory BP. But this was not a purpose of this study. A strength of our study is the large number of intradialytic BP measurements that were prospectively collected and validated for accurate data entry before analysis. The simultaneous measurement of interdialytic ambulatory BP allowed the assessment of bias and precision.
An unintended consequence of this report would be to abandon home BP monitoring for the assessment of hypertension in hemodialysis patients. However, it would be premature to discontinue home BP monitoring; home BP is associated with left ventricular hypertrophy (26) and mortality in hemodialysis patients (19), relationships that are yet to established for intradialytic BP recordings. Nonetheless, BP measurements obtained during dialysis appear to contain a larger amount of diagnostic information than what is apparent in predialysis and postdialysis BP measurements alone. Our study shows that the consideration of intradialytic BP recordings together with predialysis and postdialysis BP measurements improves the reproducibility, bias, and precision of BP measurement. Median cut-off systolic BP of 140 mmHg from a single dialysis, obtained every 30 min, provides approximately 80% sensitivity and 80% specificity in diagnosing systolic hypertension; a median cut-off diastolic BP of 80 mmHg provides approximately 75% sensitivity and 75% specificity in diagnosing diastolic hypertension. These thresholds may improve the reproducibility, bias, and precision of hypertension management in hemodialysis patients.
Disclosures
None.
Acknowledgments
Supported by Grant 5RO1-NIDDK062030–05 from National Institutes of Health. The authors thank Jennifer E. Bills and Carla Petersen for data entry, the dialysis staff at Dialysis Clinics, Inc, Clarian Health for assistance, the Roudebush VA Medical Center, and the faculty of the Division of Nephrology who gratefully allowed us to the study their patients.
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Lacson E Jr, Lazarus JM: The association between blood pressure and mortality in ESRD: not different from the general population? Semin Dial 20 :510 –517,2007 [DOI] [PubMed] [Google Scholar]
- 2.Foley RN, Agarwal R: Hypertension is harmful to dialysis patients and should be controlled. Semin Dial 20 :518 –522,2007 [DOI] [PubMed] [Google Scholar]
- 3.Kalantar-Zadeh K, Kilpatrick RD, McAllister CJ, Greenland S, Kopple JD: Reverse epidemiology of hypertension and cardiovascular death in the hemodialysis population: the 58th annual fall conference and scientific sessions. Hypertension 45 :811 –817,2005 [DOI] [PubMed] [Google Scholar]
- 4.Li Z, Lacson E Jr, Lowrie EG, Ofsthun NJ, Kuhlmann MK, Lazarus JM, Levin NW: The epidemiology of systolic blood pressure and death risk in hemodialysis patients. Am J Kidney Dis 48 :606 –615,2006 [DOI] [PubMed] [Google Scholar]
- 5.Agarwal R: Hypertension and survival in chronic hemodialysis patients: past lessons and future opportunities. Kidney Int 67 :1 –13,2005 [DOI] [PubMed] [Google Scholar]
- 6.Agarwal R: Exploring the paradoxical relationship of hypertension with mortality in chronic hemodialysis. Hemodialysis Int 8 :207 –213,2004 [DOI] [PubMed] [Google Scholar]
- 7.Agarwal R: Assessment of blood pressure in hemodialysis patients. Semin Dial 15 :299 –304,2002 [DOI] [PubMed] [Google Scholar]
- 8.Lazar AE, Smith MC, Rahman M: Blood pressure measurement in hemodialysis patients. Semin Dial 17 :250 –254,2004 [DOI] [PubMed] [Google Scholar]
- 9.Agarwal R, Andersen MJ, Bishu K, Saha C: Home blood pressure monitoring improves the diagnosis of hypertension in hemodialysis patients. Kidney Int 69 :900 –906,2006 [DOI] [PubMed] [Google Scholar]
- 10.Agarwal R, Peixoto AJ, Santos SF, Zoccali C: Pre and post dialysis blood pressures are imprecise estimates of interdialytic ambulatory blood pressure. Clin J Am Soc Nephrol 1 :389 –398,2006 [DOI] [PubMed] [Google Scholar]
- 11.Agarwal R: Supervised atenolol therapy in the management of hemodialysis hypertension. Kidney Int 55 :1528 –1535,1999 [DOI] [PubMed] [Google Scholar]
- 12.O'Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P: European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 21 :821 –848,2003 [DOI] [PubMed] [Google Scholar]
- 13.Rabe-Hesketh S, Skrondal A: Multilevel and Longitudinal Modeling Using Stata. College Station, Texas, Stata Press,2005
- 14.Thompson ML, Zucchini W: On the statistical analysis of ROC curves. Stat Med 8 :1277 –1290,1989 [DOI] [PubMed] [Google Scholar]
- 15.Youden WJ: Index for rating diagnostic tests. Cancer 3 :32 –35,1950 [DOI] [PubMed] [Google Scholar]
- 16.DeLong ER, DeLong DM, Clarke-Pearson DL: Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44 :837 –845,1988 [PubMed] [Google Scholar]
- 17.Mitra S, Chandna SM, Farrington K: What is hypertension in chronic haemodialysis? The role of interdialytic blood pressure monitoring. Nephrol Dial Transplant 14 :2915 –2921,1999 [DOI] [PubMed] [Google Scholar]
- 18.Peixoto AJ, Santos SF, Mendes RB, Crowley ST, Maldonado R, Orias M, Mansoor GA, White WB: Reproducibility of ambulatory blood pressure monitoring in hemodialysis patients. Am J Kidney Dis 36 :983 –990,2000 [DOI] [PubMed] [Google Scholar]
- 19.Alborzi P, Patel N, Agarwal R: Home blood pressures are of greater prognostic value than hemodialysis unit recordings. Clin J Am Soc Nephrol 2 :1228 –1234,2007 [DOI] [PubMed] [Google Scholar]
- 20.Lins RL, Elseviers M, Rogiers P, Van Hoeyweghen RJ, De Raedt H, Zachee P, Daelemans RA: Importance of volume factors in dialysis related hypertension. Clin Nephrol 48 :29 –33,1997 [PubMed] [Google Scholar]
- 21.Dionisio P, Valenti M, Bergia R, Caramello E, Stramignoni E, Berto IM, Pellerey M, Bajardi P: Influence of the hydration state on blood pressure values in a group of patients on regular maintenance hemodialysis. Blood Purif 15 :25 –33,1997 [DOI] [PubMed] [Google Scholar]
- 22.Sherman RA, Daniel A, Cody RP: The effect of interdialytic weight gain on predialysis blood pressure. Artif Organs 17 :770 –774,1993 [DOI] [PubMed] [Google Scholar]
- 23.Inrig JK, Patel UD, Gillespie BS, Hasselblad V, Himmelfarb J, Reddan D, Lindsay RM, Winchester JF, Stivelman J, Toto R, Szczech LA: Relationship between interdialytic weight gain and blood pressure among prevalent hemodialysis patients. Am J Kidney Dis 50 :108 –118,2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelley K, Light RP, Agarwal R: Trended cosinor change model for analyzing hemodynamic rhythm patterns in hemodialysis patients. Hypertension 50 :143 –150,2007 [DOI] [PubMed] [Google Scholar]
- 25.Agarwal R, Andersen MJ, Light RP: Location not quantity of blood pressure measurements predicts mortality in hemodialysis patients. Am J Nephrol 28 :210 –217,2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Agarwal R, Brim NJ, Mahenthiran J, Andersen MJ, Saha C: Out-of-hemodialysis-unit blood pressure is a superior determinant of left ventricular hypertrophy. Hypertension 47 :62 –68,2006 [DOI] [PubMed] [Google Scholar]