Abstract
Background and objectives: It is unknown whether adherence to recommended medications after myocardial infarction (MI) differs by kidney function.
Design, setting, participants, & measurements: This was a retrospective cohort study of older patients who were discharged after MI in two Eastern states between 1995 and 2004. Patients were categorized as having ESRD, having chronic kidney disease (CKD), and being free from diagnosed CKD. Use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers (ACEI/ARB), β blockers (BB), and statins was assessed within 30 d after discharge. Good adherence was defined as proportion of days covered >80% during the first year after discharge.
Results: Compared with patients with no CKD, patients with CKD had 22% lower adjusted use of ACEI/ARB but similar rates of BB and statin use. Patients with ESRD experienced 43% lower ACEI/ARB and 17% lower statin use. Only 64% (BB), 57% (statins), and 54% (ACEI/ARB) of patients had good 1-yr adherence. Adherence was similar between patients with CKD and with no CKD for all study drugs. Fewer patients with ESRD had good adherence to BB.
Conclusions: With the exception of lower ACEI/ARB use in patients with CKD, we found no differences between patients with CKD and with no CKD in their use of and adherence to these cardiovascular medications after MI. Patients with ESRD experienced lower use of ACEI/ARB and statins and lower adherence to BB regimens. Postulated differences in medication use after MI across levels of kidney function are unlikely to explain the observed differences in long-term outcomes.
In 2000, more than 26 million individuals in the United States had chronic kidney disease (CKD), with more than 16 million individuals having an estimated GFR (eGFR) of <60 ml/min per 1.73 m2 (1). In addition, more than 485,000 patients had ESRD and were undergoing dialysis treatment or lived with a functioning kidney transplant at the end of 2005 (2). In recent years, kidney function has been recognized as a major cardiovascular risk factor. Patients with reduced kidney function are more likely to experience a myocardial infarction (MI) (3). Kidney function is further independently associated with short-term and long-term mortality after MI (4–6).
It has been hypothesized that the relative underuse of certain cardiovascular medications in patients with kidney disease may, at least in part, be responsible for the increased mortality after MI in patients with reduced kidney function. Indeed, previous studies demonstrated that use of such medications as aspirin, β receptor blockers (BB), 3-hydroxy-3-methyl-glutaryl-CoA inhibitors (statins), and angiotensin-converting enzyme inhibitors (ACEI) or angiotensin-receptor blockers (ARB) was lower in patients with more reduced kidney function and particularly low in patients with ESRD (7–9).
Little attention has been paid to the possibility that patients with reduced kidney function may also exhibit lower adherence to these long-term therapies, once initiated. We conducted this study with the intention to evaluate whether the use and adherence to these recommended medications differed by kidney function in older survivors of an MI. We also tested whether secular trends over a decade in the use and adherence to these medications differed by kidney function.
Materials and Methods
Study Population and Follow-up
For this study, we used medical claims data for the years 1994 through 2004 from the New Jersey Pharmaceutical Assistance for the Aged and Disabled program and the Pennsylvania Pharmaceutical Assistance Contract for the Elderly program. These means-tested programs provide comprehensive prescription drug coverage for eligible elderly patients in New Jersey and Pennsylvania. Neither program had any restrictions or prior-authorization programs in place for any of the study drugs. The claims data from each drug-benefit program were merged with Medicare Part A and B claims for these patients. We identified all patients who were aged ≥65 yr and were hospitalized for at least 3 d but no longer than 180 d and discharged alive with a primary diagnosis of acute MI (International Classification of Diseases, Ninth Revision code 410.x). This algorithm for identifying episodes of MI had a positive predictive value of 94% in a previous validation study using our data (10). To provide a uniform ascertainment window for postdischarge drug use, we further required eligible patients to survive at least 30 d after discharge from their MI hospitalization.
Main Variable
The study variable of interest, kidney disease, was composed of three mutually exclusive categories: ESRD, CKD, and absence of diagnosed CKD. ESRD that required maintenance dialysis was ascertained from dialysis-specific procedure codes before the index admission. Presence of CKD without the need for renal replacement therapy was ascertained from the presence of at least one of a large number of diagnosis codes indicating kidney disease within 1 yr before MI admission (11). We previously showed that a very similar algorithm of identifying patients with eGFR <60 ml/min per 1.73 m2 had a positive predictive value of 92% in a subset of patients in this study (12). All other patients were categorized as not having (diagnosed) CKD and constituted the reference group for all analyses.
Other Patient Characteristics
From enrollment files, we defined each patient's age on the date of admission for the index hospitalization, gender, and race (white, nonwhite). From 12 mo of claims preceding the index hospitalization, we ascertained several comorbid conditions (coronary artery disease, congestive heart failure, cerebrovascular disease, peripheral vascular disease, hypertension, diabetes, malignancy, chronic obstructive pulmonary disease, depression, dementia, and other mental disease). Previous health care use was defined in terms of total hospital days, number of physician visits, and number of different medications recorded in the previous year. We also defined presence of cardiovascular procedures during the index hospitalization (coronary artery bypass graft surgery, angiography, and coronary intervention: percutaneous transluminal coronary angioplasty or stent insertion) and each patient's length of stay.
Outcomes
The use of BB, statins, and ACEI/ARB was assessed within 30 d after discharge from MI (any use versus no use). Among patients who filled a first prescription within 30 d of discharge, we calculated the proportion of days covered (PDC) for each study class, a widely used measure of adherence to long-term medications. Its numerator includes the number of pills supplied divided by the daily frequency in which these were prescribed to be taken. Overlapping supplies at the filling of subsequent prescriptions were prorated. The denominator consists of the total follow-up time minus the sum of all days spent in a hospital, where medications are usually provided for the patient (13–15). Patients were censored at death, admission to a nursing home, or end of the study period. We then identified patients whose PDC was ≥80 d, a measure of good adherence to long-term medications (13,15,16). Adherence was studied for the first year after discharge and limited to patients who had their MI between 1995 and 2003, to ensure availability of at least 1 yr of follow-up data after their index MI for all patients. Use of and adherence to the study medications were assessed using National Drug Code numbers of all filled prescriptions.
Statistical Analyses
Patient characteristics were tabulated as stratum-specific means (± SD) and counts (proportions) for the three kidney disease strata. Differences across these three categories were compared using ordinal tests for trend. Associations between kidney disease and the study outcomes were analyzed using modified Poisson regression models (17), which allowed direct estimation of risk ratios (RR) and the corresponding 95% confidence intervals (CI). We present results from (1) unadjusted analyses; (2) models that adjusted for demographics, comorbidities, in-hospital procedures, and discharge year; and (3) models that additionally included indicators of past health care use. To assess the trend in the use and adherence over time after adjusting for changes in the patients’ characteristics, we used the aforementioned multivariate models. We also tested interactions between kidney disease status and calendar year of discharge to evaluate any differences in secular trends by kidney disease status. We used the SAS for Windows software (release 8.2; SAS Institute, Cary, NC) for all statistical analyses. The study was approved by the institutional review board of Brigham and Women's Hospital, and all patient identifiers were removed before the analyses to protect patients’ privacy.
Results
We identified 21,484 patients who experienced an MI between 1995 and 2004, were discharged alive, and survived >30 d after discharge. Of those, 436 (2%) were identified as having ESRD and undergoing long-term dialysis, 3645 (17%) were categorized as having CKD, and 17,403 (81%) had no previous diagnosis of CKD. Most patient characteristics varied across strata of kidney disease (Table 1). More advanced kidney disease was associated with younger age, female gender, and nonwhite race. Average length of stay was longer for patients with advanced kidney disease, who also had a substantially greater burden of comorbid disease and history of greater use of health care services. Notably, use of BB, statins, and ACEI/ARB before the index hospitalization was greater in patients with more advanced kidney impairment.
Table 1.
Characteristics of study patients by level of kidney functiona
| Characteristic | No Diagnosed CKD(n = 17,403) | CKD(n = 3645) | ESRD(n = 436) | Pb |
|---|---|---|---|---|
| Demographics | ||||
| age (yr; mean ± SD) | 79.8 ± 6.9 | 79.6 ± 6.9 | 76.3 ± 6.3 | <0.001 |
| gender male versus female (n [%]) | 4505 (25.9) | 1218 (33.4) | 169 (38.8) | <0.001 |
| Race (n [%]) | ||||
| white | 16,148 (92.8) | 3256 (89.3) | 357 (81.9) | |
| nonwhite | 1255 (7.2) | 389 (10.7) | 79 (18.1) | <0.001 |
| Characteristics of index hospitalization | ||||
| length of stay (d; mean ± SD) | 9.4 ± 6.3 | 11.8 ± 8.8 | 15.9 ± 14.8 | <0.001 |
| angiography (n [%]) | 7776 (44.7) | 1452 (39.8) | 186 (42.7) | <0.001 |
| coronary intervention (PTCA or stent; n [%]) | 3687 (21.2) | 629 (17.3) | 80 (18.4) | <0.001 |
| CABG (n [%]) | 1327 (7.6) | 296 (8.1) | 32 (7.3) | 0.500 |
| Comorbid conditions | ||||
| Previous diagnosis of (n [%]) | ||||
| coronary artery disease | 10,530 (60.5) | 2523 (69.2) | 319 (73.2) | <0.001 |
| congestive heart failure | 10,742 (61.7) | 2943 (80.7) | 394 (90.4) | <0.001 |
| cerebrovascular disease | 5255 (30.2) | 1369 (37.6) | 178 (40.8) | <0.001 |
| peripheral artery disease | 4115 (23.7) | 1241 (34.1) | 184 (42.2) | <0.001 |
| hypertension | 12,551 (72.1) | 2916 (80.0) | 355 (81.4) | <0.001 |
| diabetes mellitus | 7409 (42.6) | 2199 (60.3) | 310 (71.1) | <0.001 |
| malignancy | 3407 (19.6) | 863 (23.7) | 91 (20.9) | <0.001 |
| COPD | 6614 (38.0) | 1631 (44.8) | 155 (35.6) | <0.001 |
| depression | 2655 (15.3) | 543 (14.9) | 57 (13.1) | 0.250 |
| dementia | 1618 (9.3) | 355 (9.7) | 31 (7.1) | 0.820 |
| other mental disease | 1696 (9.8) | 406 (11.1) | 62 (14.2) | <0.001 |
| Charlson Comorbidity Index (mean ± SD) | 2.3 ± 1.9 | 3.8 ± 2.4 | 5.3 ± 2.5 | <0.001 |
| Previous health care use (mean ± SD) | ||||
| hospital days (previous year) | 3.1 ± 7.5 | 6.6 ± 12.1 | 10.5 ± 15.6 | <0.001 |
| no. of physician visits (previous year) | 9.7 ± 6.8 | 11.7 ± 8.6 | 11.3 ± 10.4 | <0.001 |
| no. of different drugs (previous year) | 9.8 ± 5.6 | 12.4 ± 6.4 | 14.1 ± 6.8 | <0.001 |
| Previous use of (n [%]) | ||||
| β blockers | 5496 (31.6) | 1471 (40.4) | 207 (47.5) | <0.001 |
| ACEI/ARB | 6171 (35.5) | 1796 (49.3) | 198 (45.4) | <0.001 |
| statins | 3941 (22.7) | 1095 (30.0) | 151 (34.6) | <0.001 |
ACE, angiotensin-converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass graft; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; PTCA, percutaneous transluminal coronary angioplasty.
P value for trend across categories of kidney function (no diagnosed CKD > CKD > ESRD).
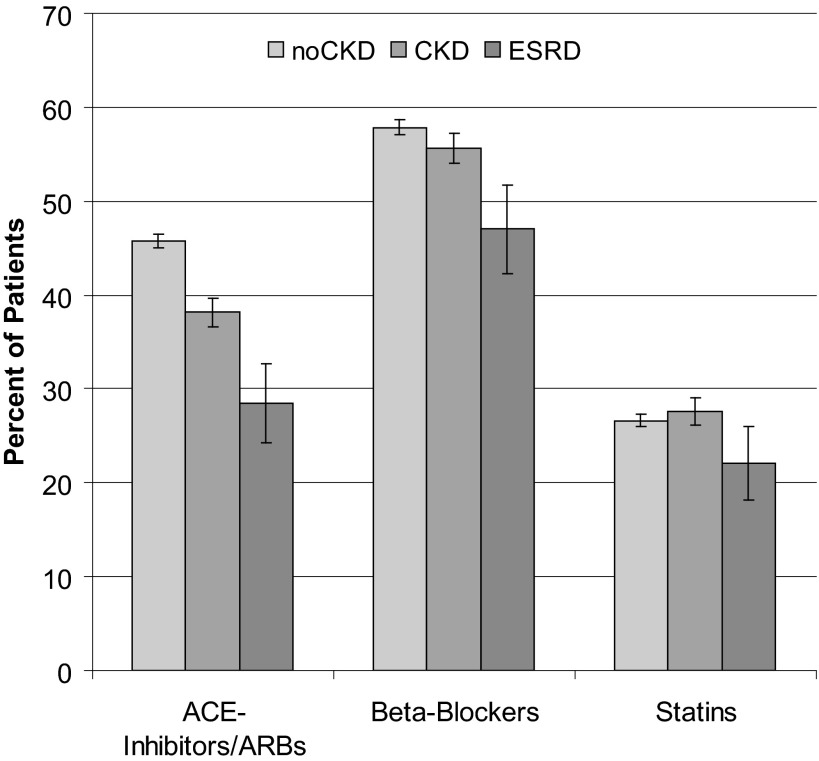
Within 30 d after discharge, 12,304 (57.3%) patients filled a prescription for a BB, 5735 (26.7%) for a statin, and 9469 (44.1%) for an ACEI or ARB. Figure 1 displays the proportion of patients who received each study drug, by category of kidney function. The unadjusted and adjusted relative rates of medication use for each class are listed in Table 2. Compared with patients without diagnosed CKD, those with CKD had similar rates of BB and statin use but 22% lower use of ACEI/ARB (RR 0.78; 95% CI 0.75 to 0.82) after multivariate adjustment. Patients who had ESRD and were on dialysis had even lower ACEI/ARB use (RR 0.57; 95% CI 0.49 to 0.66) as well as lower use of statins (RR 0.83; 95% CI 0.70 to 0.99). Use of BB was significantly lower in patients with ESRD in crude analysis, but, after adjustment, this association was no longer significant.
Figure 1.
Use of recommended medications within 30 d after discharge for myocardial infarction (MI), by level of kidney function. The outcome was any filled prescription of the study drug within 30 d after discharge from hospitalization for MI. Shown are proportions and corresponding 95% confidence intervals (CI). ACE, angiotensin-converting enzyme; ARB, angiotensin II receptor blocker; CKD, chronic kidney disease; noCKD, patient free from diagnosed CKD.
Table 2.
Kidney function and recommended medication use after discharge for MIa
| Parameter | Statins (RR [95%]) | β Blockers (RR [95%]) | ACEI/ARB (RR [95%]) |
|---|---|---|---|
| Unadjusted | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.04 (0.98 to 1.10) | 0.96 (0.93 to 0.99) | 0.83 (0.80 to 0.87) |
| ESRD | 0.83 (0.69 to 0.99) | 0.81 (0.74 to 0.90) | 0.62 (0.54 to 0.72) |
| Model with comorbidities and in-hospital procedures | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.01 (0.95 to 1.06) | 1.00 (0.97 to 1.04) | 0.77 (0.74 to 0.81) |
| ESRD | 0.79 (0.67 to 0.94) | 0.88 (0.80 to 0.97) | 0.55 (0.47 to 0.64) |
| Model with above plus health service measures | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.02 (0.96 to 1.08) | 1.00 (0.96 to 1.03) | 0.78 (0.75 to 0.82) |
| ESRD | 0.83 (0.70 to 0.99) | 0.94 (0.86 to 1.04) | 0.57 (0.49 to 0.66) |
The outcome was any filled prescription of the study drug within 30 d after discharge from hospitalization for myocardial infarction (MI). All models controlled for calendar year. Model with comorbidities and in-hospital procedures included demographics, characteristics of the index hospitalization, and all comorbid conditions. The health service measures that were additionally included in the last model were number of hospital days, number of physician visits, and number of different prescription drugs used in the year before the index admission. CI, confidence interval; RR, relative risk.
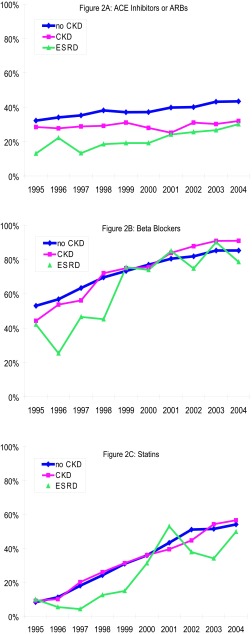
Overall, use of all study drugs increased over time: Adjusted BB use increased by 6% (95% CI 5.6 to 6.4%), statin use by 21% per year (95% CI 20 to 22%), and ACEI/ARB use by 3% per year. Figure 2 shows the adjusted rates of study drug use over time. Interaction terms between calendar year and CKD (P < 0.001) and ESRD (P = 0.006) were significant for the outcome of BB use after MI, indicating that use of BB increased disproportionately in both patients with CKD and patients with ESRD compared with patients who were fee from diagnosed CKD. The interaction between calendar year and CKD was also significant for the outcome of ACEI/ARB use (P = 0.005) but indicated a relative decline in ACEI/ARB use in patients with CKD compared with patients without diagnosed CKD.
Figure 2.
Temporal trends in medication use after MI, by level of kidney function. Medication use within 30 d after discharge from hospitalization for MI. (A) ACE inhibitors or ARB. (B) β Blockers. (C) Statins.
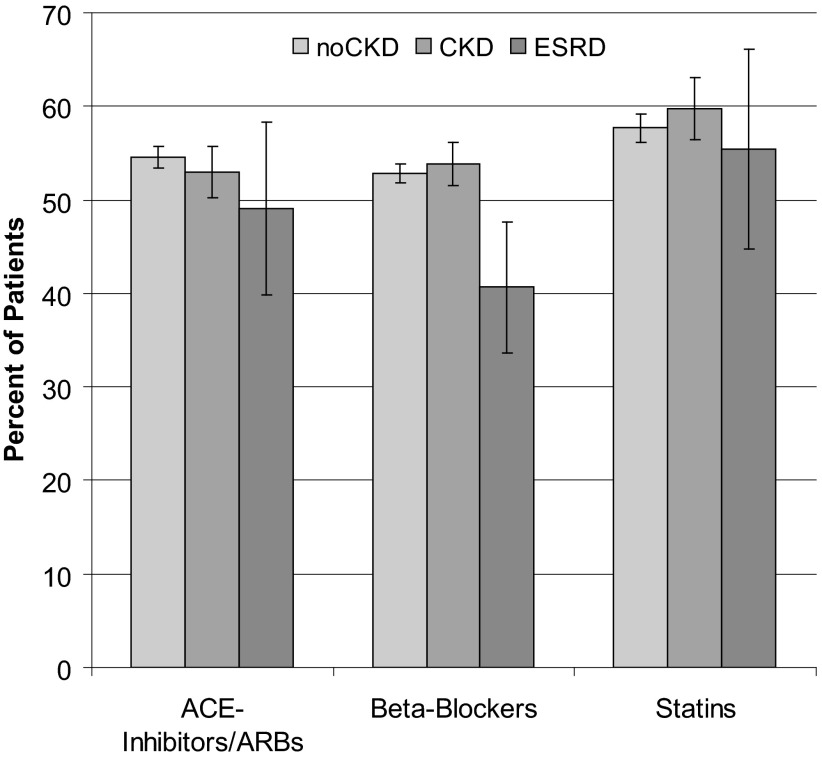
As stated already, we excluded from all analyses of medication adherence patients who experienced their index MI in 2004 to ensure data availability and potential follow-up of >1 yr. Overall adherence to the study drugs during the year after discharge was suboptimal, with only 63.7% (BB), 56.8% (statins), and 53.5% (ACEI/ARB) of patients reaching a PDC ≥80%, an indicator of good adherence to long-term medications. Figure 3 shows the proportion of patients who were classified as having good adherence to each medication class, once again by category of kidney function. Compliance with BB was not different between the no CKD and the CKD groups (Table 3) but was 23% lower among patients who were on dialysis (95% CI 9 to 35%). After multivariate adjustment, 20% fewer patients with ESRD were persistent with their BB regimen compared with patients with no diagnosed CKD (95% CI 5 to 33%). Adherence patterns for statin or ACEI/ARB treatment did not differ between patients without CKD and those with CKD or ESRD in univariate or adjusted analyses.
Figure 3.
Proportion of patients with good adherence to recommended medications in the year after discharge for MI. The outcome was percentage of days covered ≥80% for each study drug during the first year after discharge from hospitalization for MI, among those who filled a prescription for the study drug with 30 d of discharge. Shown are proportions and corresponding 95% CI.
Table 3.
Adherence to initiated drug regimen during the year after MI admission, by level of kidney functiona
| Parameter | Statins (RR [95%]) | β Blockers (RR [95%]) | ACEI/ARB (RR [95%]) |
|---|---|---|---|
| Unadjusted | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.03 (0.97 to 1.10) | 1.02 (0.97 to 1.07) | 0.97 (0.92 to 1.03) |
| ESRD | 0.96 (0.79 to 1.17) | 0.77 (0.65 to 0.92) | 0.90 (0.74 to 1.09) |
| Model with comorbidities and in-hospital procedures | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.04 (0.97 to 1.11) | 1.03 (0.98 to 1.08) | 0.96 (0.91 to 1.02) |
| ESRD | 0.99 (0.82 to 1.21) | 0.79 (0.67 to 0.94) | 0.90 (0.74 to 1.09) |
| Model with above plus health service measures | |||
| no diagnosed CKD | 1.00 (Referent) | 1.00 (Referent) | 1.00 (Referent) |
| CKD | 1.04 (0.97 to 1.11) | 1.03 (0.98 to 1.08) | 0.96 (0.91 to 1.02) |
| ESRD | 0.99 (0.81 to 1.21) | 0.80 (0.67 to 0.95) | 0.90 (0.74 to 1.09) |
The outcome was percentage of days covered ≥80% for each study drug during the first year after discharge from hospitalization for MI, among those who filled a prescription for the study drug with 30 d of discharge. All models controlled for calendar year. Model with comorbidities and in-hospital procedures included demographics, characteristics of the index hospitalization, and comorbid conditions. The health service measures that were additionally included in the last model were number of hospital days, number of physician visits, and number of different prescription drugs used in the year before the index admission.
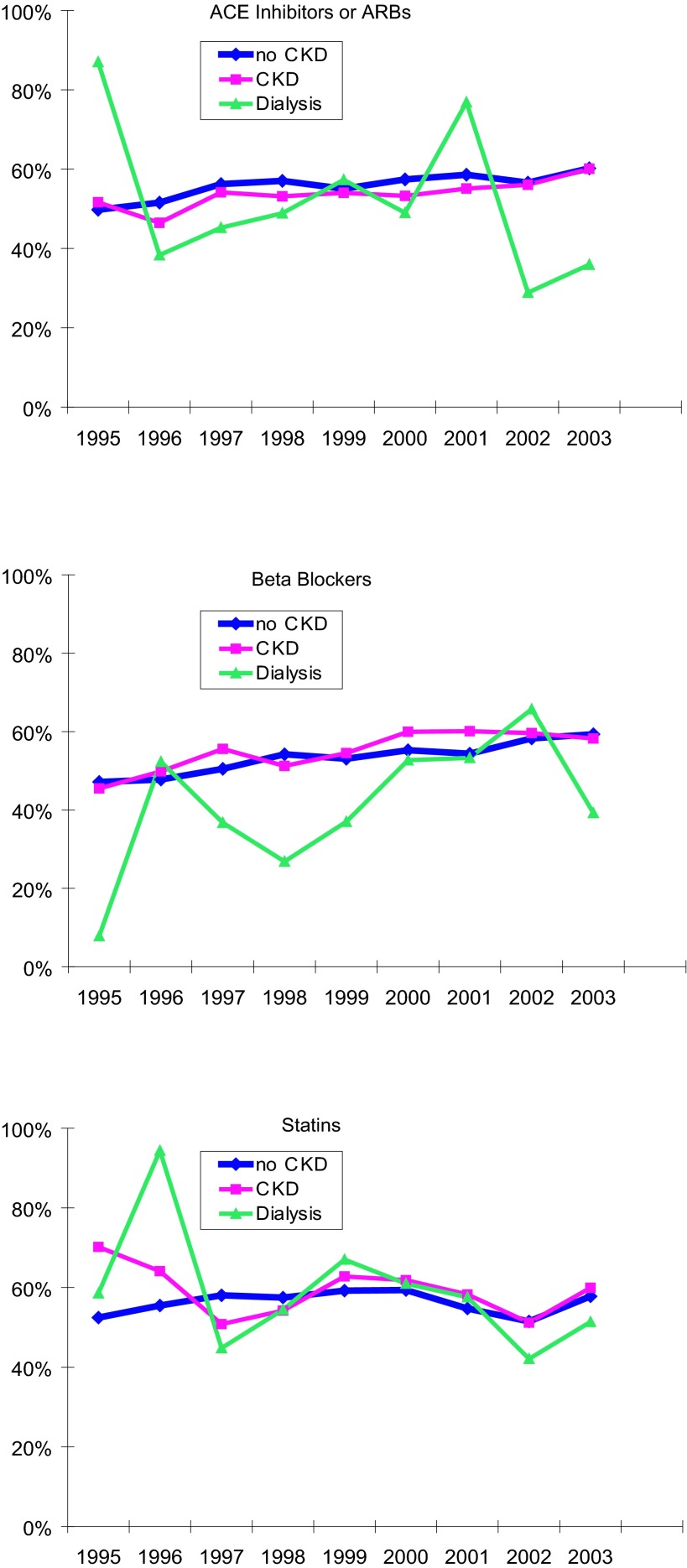
Adherence to statins did not improve over time (RR 1.01; 95% CI 0.98 to 1.01), but the proportion of patients with PDC ≥80% increased by 3% (95% CI 2 to 4%) for BB and by 2% (95% CI 1 to 3%) for ACEI/ARB therapy annually. Figure 4 shows the adjusted rates of good adherence to each study drug over time, by kidney disease status. Interaction tests between kidney disease status and calendar year were NS, indicating that these temporal trends pertained to all patients regardless of their kidney disease status.
Figure 4.
Temporal trends in good adherence to recommended medications in the year after discharge for MI. Proportion of patients with good adherence as indicated by a proportion of days covered >80% during the year after discharge from hospitalization for MI. (A) ACE inhibitors or ARB. (B) β Blockers. (C) Statins.
Discussion
In a large cohort of patients who survived an MI between 1995 and 2004, we found suboptimal use of several medication classes within 30 d of discharge. Only 57% of patients received a BB, 27% filled a prescription for a statin, and 44% received an ACEI or ARB. For all drug classes, however, use improved considerably over the decade of observation. Compared with patients without any diagnosed CKD, patients who had ESRD and were on dialysis had significantly lower uses of these drugs. Patients with CKD also had lower use of ACEI or ARB, but rates of statin and BB use did not differ from those without diagnosed CKD. Adherence to these medications was similarly suboptimal, with only 64% (BB), 57% (statins), and 54% (ACEI/ARB) of patients obtaining sufficient medication from the pharmacy to be covered for at least 80% of their noninstitutionalized days (i.e., while not being admitted at a hospital or nursing home). Kidney disease status was not a determinant of 1-yr adherence with these study drugs with the exception that patients who had ESRD and were on dialysis had lower adherence to initiated BB therapy compared with patients with CKD and with no CKD. Whereas overall adherence with BB and ACEI or ARB improved slightly over time, statin adherence did not. These temporal trends did not differ by kidney disease status.
This study has certain limitations. Retrospective in nature, it draws from information available in administrative claims databases. We did not include low-dosage aspirin use in our analyses, because it was available over the counter at a cost below the copayment required by the pharmaceutical benefits programs. Thus, patients may have obtained aspirin over the counter, which would not generate a claim to the benefits program and therefore lead to underascertainment of aspirin use. Absence of laboratory measures made it necessary to ascertain kidney disease or function using diagnosis codes that were submitted with billing claims from health care encounters. Although we previously demonstrated that patients with a diagnosis of CKD have reliably reduced kidney function (12), the group of patients with no apparent kidney disease may include a proportion of patients who have reduced kidney function but did not receive a diagnosis of it. The consequence of such misclassification is a bias toward the null. The large sample size of our cohort, however, would still enable us to detect significance even if the observed estimate of association were deflated. Thus, we are confident that relevant differences in drug use and adherence by presence versus absence of diagnosed CKD are indeed absent. Furthermore, medications recorded in our database reflect episodes of filled prescriptions. We cannot distinguish whether the patient did not receive a prescription or chose not to fill one that he or she received. Similarly, we do not know whether a patient actually took the medications that he or she obtained at the pharmacy. Finally, we cannot determine any reasons for discontinuation of any give drug, whether true nonadherence or indicated and ordered discontinuation on medical grounds.
Few studies have investigated use of recommended medications after MI in patients with CKD or ESRD, and even fewer have drawn comparisons across levels of kidney function. Berger et al. (8) found lower use of aspirin, BB, and ACEI in dialysis patients compared with patients without ESRD in the Collaborative Cardiovascular Project, a nationwide observational study of US Medicare beneficiaries who experienced an MI in 1994 through 1995. Shlipak et al. (4), using the same data set but categorizing patients by their admission serum creatinine, found a monotonic decline of aspirin and BB use across categories of kidney function, whereas ACEI use seemed similar across groups of kidney function. McCullough et al. (18) confirmed this observation using several years of data (1990 through 1998) from a large Midwestern tertiary center and found that aspirin and BB were less likely to be used by patients with lower estimated creatinine clearance, with long-term dialysis patients experiencing the lowest use. Finally, Anavekar et al. (6) confirmed this observation of lower use of aspirin and BB by declining eGFR in a large, prospective, randomized trial of valsartan in patients who had experienced an MI. Although they did not observe any differences in ACEI use after MI, they did find lower use of statins in patients with lower kidney function (6). These studies have in common that medication use was ascertained during the initial MI hospitalization. It is unclear from these observations, however, whether lower use of these medications persisted after discharge. A single study of elderly Medicare beneficiaries in Pennsylvania confirmed that crude associations between kidney function and outpatient use after discharge from MI existed for ACEI/ARB, BB, and statin use. After adjustment for other factors, however, only the association with ACEI/ARB use remained significant (7). In this study, ACEI/ARB use was lower in patients with eGFR <30 ml/min per 1.73 m2, which persisted after multivariate adjustment (7). This study confirms this observation in a substantially larger data set: No difference in BB and statin use existed between patients with and without CKD, whereas ACEI/ARB were used less in patients with diagnosed CKD. By contrast, patients with ESRD experienced significantly lower use of all studied cardiovascular drugs compared with patients who were free from diagnosed CKD. The relative underuse of ACEI/ARB in patients with diagnosed CKD is striking, because these are exactly the ones who might benefit the most from these drugs, through both their cardiovascular and their renoprotective effects. We can only speculate that this underuse might be related to providers’ fears of adverse events such as hyperkalemia or sudden increases in serum creatinine, particularly because these patients both are older and have diagnosed CKD.
This study is novel in that it is the first one to evaluate putative differences across categories of kidney function in long-term adherence to initiated cardiovascular medications. We had hypothesized that not only initiation or continuation of key therapeutic regimens after hospital discharge from MI but also adherence to these medications would be lower in patients with more advanced kidney disease. This hypothesis was supported by other observations that greater comorbidity and complexity of medical regimens reduced compliance with proven medications (19). Indeed, as shown in Table 1, the number of different drugs used before MI admission increased with category of kidney disease in our study sample. Thus, it came as a surprise to us that rates of good adherence to the three medication classes studied did not differ between patients with CKD and those without diagnosed CKD. The only significant difference was that patients with ESRD had lower adherence to their BB regimen but were no different in their long-term use of initiated therapies of ACEI/ARB and statins. To our knowledge, this study is the first to evaluate patients’ adherence to recommended medications by level of kidney function.
The findings from this study and those of others have important implications. It seems that initiation of recommended therapy during hospitalization and its translation into immediate outpatient use after discharge are the preferred targets of intervention. Only if practitioners initiate recommended therapies during hospitalization and patients actually receive prescriptions for recommended medications and fill them after discharge does the subsequent question of long-term adherence come into play. Because neither primary adjusted filling rates of prescribed drugs after discharge nor adjusted adherence to initiated medication regimens differed between patients with CKD and those without diagnosed CKD, other mechanisms are likely responsible for the observed adjusted morbidity and mortality difference between patients with better versus more reduced kidney function. Improving medication use after MI may improve outcomes in the population overall but not necessarily serve to close the mortality gap across categories of kidney function. Furthermore, there is only limited evidence supporting that extrapolation of trials data from the general population to patients with CKD or even ESRD is a valid approach. Because most studies that have informed our practice have excluded patients with ESRD or advanced CKD and a mere 7% of cardiovascular trials reviewed had even reported kidney function (20), it seems that establishing high-level evidence in the CKD and ESRD populations is a top public health priority (21). High-quality randomized trials of sufficient statistical power designed on the basis of realistic event rates and meaningful risk reductions need to be conducted specifically in the CKD population.
Conclusions
Initiation of and adherence to recommended cardiovascular medications may not differ between patients with versus without CKD after taking into account differences in patient characteristics. Other factors are likely responsible for the observed gradient in cardiovascular risk by kidney function. Detection of potentially modifiable factors that are specific to advanced kidney disease and the development of candidate therapies and proof of their efficacy to reduce cardiovascular risk in kidney disease should be a top priority for the investment of private and public funds, especially given the high and increasing prevalence of kidney disease.
Disclosures
None.
Acknowledgments
This work was supported by an American Heart Association Scientist Development grant (0535232N) and a Norman S. Coplon Extramural Research Program Award from Satellite Research to W.C.W.
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298 :2038 –2047,2007 [DOI] [PubMed] [Google Scholar]
- 2.Collins AJ, Foley R, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Xue J, Fan Q, Guo H, Li Q, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Weinhandl E, Zaun D, Zhang R, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L: Excerpts from the United States Renal Data System 2007 Annual Data Report. Am J Kidney Dis 51 :S1 –S320,2008 [DOI] [PubMed] [Google Scholar]
- 3.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY: Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351 :1296 –1305,2004 [DOI] [PubMed] [Google Scholar]
- 4.Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McClellan MB: Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med 137 :555 –562,2002 [DOI] [PubMed] [Google Scholar]
- 5.Wright RS, Reeder GS, Herzog CA, Albright RC, Williams BA, Dvorak DL, Miller WL, Murphy JG, Kopecky SL, Jaffe AS: Acute myocardial infarction and renal dysfunction: A high-risk combination. Ann Intern Med 137 :563 –570,2002 [DOI] [PubMed] [Google Scholar]
- 6.Anavekar NS, McMurray JJ, Velazquez EJ, Solomon SD, Kober L, Rouleau JL, White HD, Nordlander R, Maggioni A, Dickstein K, Zelenkofske S, Leimberger JD, Califf RM, Pfeffer MA: Relation between renal dysfunction and cardiovascular outcomes after myocardial infarction. N Engl J Med 351 :1285 –1295,2004 [DOI] [PubMed] [Google Scholar]
- 7.Winkelmayer WC, Charytan DM, Brookhart MA, Levin R, Solomon DH, Avorn J: Kidney function and use of recommended medications after myocardial infarction in elderly patients. Clin J Am Soc Nephrol 1 :796 –801,2006 [DOI] [PubMed] [Google Scholar]
- 8.Berger AK, Duval S, Krumholz HM: Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol 42 :201 –208,2003 [DOI] [PubMed] [Google Scholar]
- 9.Winkelmayer WC, Charytan DM, Levin R, Avorn J: Poor short-term survival and low use of cardiovascular medications in elderly dialysis patients after acute myocardial infarction. Am J Kidney Dis 47 :301 –308,2006 [DOI] [PubMed] [Google Scholar]
- 10.Kiyota Y, Schneeweiss S, Glynn RJ, Cannuscio CC, Avorn J, Solomon DH: Accuracy of Medicare claims-based diagnosis of acute myocardial infarction: Estimating positive predictive value on the basis of review of hospital records. Am Heart J 148 :99 –104,2004 [DOI] [PubMed] [Google Scholar]
- 11.Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ: Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol 16 :489 –495,2005 [DOI] [PubMed] [Google Scholar]
- 12.Winkelmayer WC, Schneeweiss S, Mogun H, Patrick AR, Avorn J, Solomon DH: Identification of individuals with CKD from Medicare claims data: A validation study. Am J Kidney Dis 46 :225 –232,2005 [DOI] [PubMed] [Google Scholar]
- 13.Benner JS, Glynn RJ, Mogun H, Neumann PJ, Weinstein MC, Avorn J: Long-term persistence in use of statin therapy in elderly patients. JAMA 288 :455 –461,2002 [DOI] [PubMed] [Google Scholar]
- 14.Steiner JF, Prochazka AV: The assessment of refill compliance using pharmacy records: Methods, validity, and applications. J Clin Epidemiol 50 :105 –116,1997 [DOI] [PubMed] [Google Scholar]
- 15.Chapman RH, Benner JS, Petrilla AA, Tierce JC, Collins SR, Battleman DS, Schwartz JS: Predictors of adherence with antihypertensive and lipid-lowering therapy. Arch Intern Med 165 :1147 –1152,2005 [DOI] [PubMed] [Google Scholar]
- 16.Rasmussen JN, Chong A, Alter DA: Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 297 :177 –186,2007 [DOI] [PubMed] [Google Scholar]
- 17.Zou G: A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159 :702 –706,2004 [DOI] [PubMed] [Google Scholar]
- 18.McCullough PA, Sandberg KR, Borzak S, Hudson MP, Garg M, Manley HJ: Benefits of aspirin and beta-blockade after myocardial infarction in patients with chronic kidney disease. Am Heart J 144 :226 –232,2002 [DOI] [PubMed] [Google Scholar]
- 19.Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Brookhart MA: Compliance with osteoporosis medications. Arch Intern Med 165 :2414 –2419,2005 [DOI] [PubMed] [Google Scholar]
- 20.Charytan D, Kuntz RE: The exclusion of patients with chronic kidney disease from clinical trials in coronary artery disease. Kidney Int 70 :2021 –2030,2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Himmelfarb J: Chronic kidney disease and the public health: Gaps in evidence from interventional trials. JAMA 297 :2630 –2633,2007 [DOI] [PubMed] [Google Scholar]