Abstract
This study is designed based on the retrospective analysis of patients treated in the Neurosurgical Department of two major hospitals and review of the literature. The aim of this study is to evaluate the efficacy of surgery and address controversial issues in the treatment of symptomatic lumbar intraspinal synovial cysts. Spinal juxtafacet cysts (synovial and ganglion cysts) are a rare cause of low back and radicular leg pain. Although the relevant reports in the international literature are increasing, the controversy about conservative versus surgical treatment and the need for concomitant fusion still exists. Data from seven patients (age range 58–69 years, mean age 61 years) with low back and radicular leg pain due to a lumbar facet joint cyst were retrospectively analyzed. Demographic data, cyst level, presence of concomitant local pathology, treatment and results of treatment were recorded. A follow-up of at least 6 months (range 6–48 months) was conducted and results were noted. All patients had back pain, while five also experienced unilateral radicular leg pain and one had bilateral leg pain. One patient had neurogenic claudication. MRI identified the cyst and highlighted underlying pathology in all cases. All patients underwent surgical cyst excision. No fusion was performed. Post-operatively, all patients showed a total resolution of symptoms with sustained benefit at final evaluation. Review of the literature revealed a trend towards surgery, as this is correlated to a more favorable outcome compared with conservative treatment. Fusion should be performed on a case-by-case basis only. Surgery is a safe and effective treatment choice in this increasingly appearing ailment. A prospective, randomized trial should clarify issues under debate.
Keywords: Intraspinal cyst, Synovial cyst, Surgical treatment, Fusion
Introduction
Intraspinal synovial cysts are reported with increasing frequency in the literature but continue to be an uncommon cause of radicular pain [25]. The use of newer imaging modalities such as CT and MRI has allowed the accurate preoperative diagnosis of this entity that could once be identified only during surgery [20, 45]. This enables accurate preoperative planning and avoidance of therapeutic pitfalls. We report the clinical presentation, management and outcome of seven patients with lumbar intraspinal synovial cysts and review the literature, focusing on issues that remain under debate. We also performed a thorough review of the literature regarding all reported juxtafacet cysts treated surgically over a period of 15 years, from 1991 to 2006. We identified the relevant published studies and cases by searching the Medline and the reference lists of related articles and performed a systematic review and assessment of the full texts of all articles selected; only articles written in English were reviewed. Our research yielded a total of 499 patients. We report on the demographics, symptoms, complications, treatment and outcome from this data and focus on the issues that are still controversial.
Materials and methods
Between 2000 and 2006, seven patients (four women and three men) were diagnosed and treated for lumbar spine synovial cysts by the Neurosurgical Department of two major hospitals in Greece. All patients were evaluated pre-operatively with lumbar MRI in a standardized fashion, including a scout view followed by T1- and T2-weighted axial, sagittal and coronal images. Information regarding duration and type of symptoms (back and/or radicular pain, neurogenic claudication), findings on neurological examination and surgical outcome were recorded. All patients underwent microscope-assisted surgical removal of the cysts. In three cases this was performed through a hemi-laminectomy, in three through a foraminotomy while one patient required a two-level laminectomy. Spinal fusion was not performed in any of the patients.
The follow-up period ranged from 6 months to 4 years (mean: 28 months). All patients were initially evaluated within the first 2 months post-surgery and again at 6 and 12 months, with the exception of one patient (case 1) who was lost during follow-up following his 6-month post-operative assessment. During the preparation of this manuscript, all but one patient were evaluated by the primary author either as outpatients or by telephonic follow-up.
Results were rated based on a three-scale questionnaire scoring system: “excellent” outcome meant total symptoms resolution without development of new symptoms or signs; “good” would stand for marked improvement (more than 75% as described subjectively by the patient), with occasional pain and/or occasional need for pain medication and “fair/poor” meant either improvement with frequent need for pain medication, no improvement or even pain worsening. Even though this scale could have been more detailed, it was fashioned in this way in order to allow the unification of results reported in the case series reviewed and enabling the extraction of statistical data.
Results
Median age at the time of surgery was 61 years (range 58–69 years). All patients were suffering from back pain. Median duration of symptoms prior to surgery was 14.8 months (range 1–48 months). Symptoms and signs are presented in Table 1. Symptoms were unresponsive to conservative treatment, which included bed rest and administration of non-steroidal anti-inflammatory drugs. One patient complained of bilateral L5 radicular pain, and MRI demonstrated a left synovial cyst and a herniated nucleus pulposus compressing the right L5 nerve root. Imaging demonstrated osteoarthritic changes in the facet joints in all patients and degenerative disc disease in two. Finally, one patient (case 2) had central canal stenosis along with bony and ligamentus overgrowth and significant development of local osteophytes.
Table 1.
Demographic data, symptoms, signs and treatment in seven patients with intraspinal synovial cysts
| Case | Age | Sex | Symptom duration (months) | Symptom | Level | Local pathology | Neurologic deficit | Treatment | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Back pain | Sciatica | Motor | Sensory | Reflex | |||||||
| 1 | 51 | F | 6 | 2 | Radicular pain L5 right | L4/L5 | – | – | – | – | FT |
| 2 | 64 | M | 48 | 6 | Neurogenic claudication | L3/L4 | LS | L4 | Diffuse | Yes | 2-level LT |
| 3 | 59 | M | 12 | 8 | Radicular pain L5 Right | L4/L5 | – | – | – | Hemi-LT | |
| 4 | 69 | F | 18 | 12 | Radicular pain L5 left | L4/L5 | DDD | – | – | – | FT |
| 5 | 60 | F | 1 | 2 | Radicular pain l5 Left + right | L4/L5 | HNP | L5 | L5 | – | Hemi-LT |
| 6 | 64 | M | 12 | 6 | Radicular pain L5 left | L4/L5 | – | L5 | – | – | Hemi-LT |
| 7 | 58 | F | 6 | 5 | Radicular pain L5 right | L4/L5 | – | – | – | – | FT |
LS lumbar stenosis, DDD degenerative disc disease, HNP herniated nucleus pulposus, FT foraminotomy, LT laminectomy
All patients were surgically treated with cyst excision. In two patients (cases 3 and 6) excision was performed through a hemi-laminectomy, one patient (case 5) underwent hemi-laminectomy, discectomy and cyst excision, while three patients (cases 1, 4 and 7) underwent cyst excision through foraminotomy. In the patient suffering from spinal claudication (case 2), the presence of significant central canal stenosis along with bony and ligamentus overgrowth and osteophytes led to a decision for a two-level decompressive laminectomy along with cyst excision. No perioperative complications were noted. At 2 months post-operative follow-up, four out of seven patients reported a complete resolution of symptoms while 3 patients were significantly better and became excellent 1 and 6 months later (cases 4, 5 and case 2 respectively). At 12 months follow-up, six out of the seven patients were evaluated with dynamic flexion–extension radiographs of the lumbar spine for signs of post-operative spondylolisthesis and possible need for fusion. No signs of instability were noted. The clinical outcome was evaluated as “excellent” in all cases.
Discussion
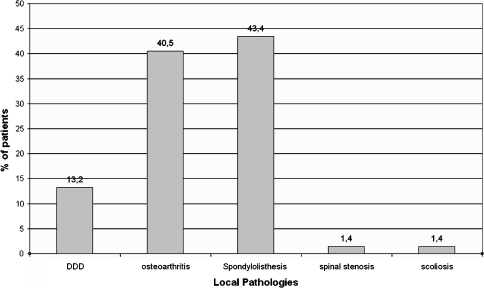
The term lumbar intraspinal synovial cysts (LISC) refers to cysts that arise from the zygapophyseal joint capsule of the lumbar spine. They are included in the term “juxtafacet cyst” which also encompasses ganglion cysts and was introduced by Kao et al. in 1974 [21]. The differentiation between these two entities is only of histological value, as they share the same characteristics with respect to clinical presentation, treatment and outcome and most likely represent different endpoints of the same degenerating process [12, 37]. Degeneration will cause protrusion of the synovial membrane through defects of the joint capsule. This herniation causes the formation of a para-articular cavity filled with synovial fluid [14]. The aetiopathogenesis of synovial cysts remains a matter of debate [4]. The fact that most synovial cysts arise at the L4/5 level, the single-most mobile level of the vertebral column, along with the frequent association with spondylolisthesis, favors instability as a pivotal factor in their aetiopathogenesis [42]. Nonetheless, it is clear that their formation comes as part of the degenerative spinal disease as a whole. In that context, spinal instability and spinal trauma play a major role [16]. Trauma, although not so strongly incriminated by some authors [21, 26, 31, 35] undoubtedly exercises a cumulative effect in spinal degeneration. Yarde et al. [47] reported the presence of hemosidirin in six out of eight patients with LISCs, of whom only one had a clear history of trauma. The fact that repetitive minor injuries may go unnoticed and not come up in the patient’s medical history, along with the fact that these injuries usually happen more at the mobile parts of the spine, suggests that the pathogenetic roles of instability and trauma are intertwined. The definite association with osteoarthritis (40.5%) and spondylolisthesis (43.4%) and the reported relationship with disc degeneration (13.2%) only highlight the major role of segmental spinal instability in the pathogenesis of spinal synovial cysts [10, 21, 26, 31, 34, 35, 44, 47] (Fig. 1).
Fig. 1.
Coinciding pathology in 499 patients with spinal synovial cysts
The prevalence of lumbar facet joint synovial cysts is unknown, and it is highly possible that there is no uniform distribution in all populations. Doyle and Merrilees reported their frequency to be as high as 10% in patients having low back pain or radiculopathy [10]. Sachdev et al. [40] reported 31 periarticular cysts as incidental findings in a series of 1,400 lumbar laminotomies (2.2%). In another study, Lemish et al. identified 10 LISCs in a total of 1,000 lumbar CT scans. This prevalence of 1% is rather underestimated, given the relatively low sensitivity of CT scanning compared with MRI [14, 43].
Juxtafacet cysts are ailments of the older population, with the higher prevalence being in the seventh decade of life [42]. In our study, the mean age was 61 years while it was 64 in the cases reviewed. Obviously, their association with degenerative spine disease is responsible for that age distribution. A female predominance has been reported, and our literature review found this preponderance to be marginal, as the number of female patients was only slightly larger to that of male [256 female (51.2%) vs. 243 male (48.8%)] [18, 26, 39, 42].
The majority of spinal synovial cysts in our case series occurred at the L4/5 level, which corresponds well with data from other studies. The predilection for this particular level, (62% L4/5 occurrence in the literature reviewed), is in favor of instability playing a major role [31]. Other less common vertebral segments include L5–S1 and L3/4 (18 and 17%, respectively, in a total of 297 patients.) Cysts in the cervical spine are uncommon. When they do appear, like their lumbar counterparts, it is in the most mobile segments of the cervical spine, usually C5–C6 or C7–T1, the level where a mobile segment is attached to a non-mobile [13, 26]. Those involving the thoracic spine are even more rare [6, 9, 15, 21]. It is highly likely that the stability of the rather motionless thoracic spine prevents the formation of synovial cysts [11]. In that context, the observed sacral sparing is nothing but expectable [16].
The clinical presentation of any intraspinal cyst depends on its size, site and relationship with adjacent structures. It may be asymptomatic, but it frequently presents with radicular pain, neurogenic claudication or cauda equina syndrome [16, 38, 47]. Back pain is also a common complaint among these patients and usually precedes root compression symptoms, as was noted in our series as well. Associated neurologic deficits from root compression commonly coexist. Myelopathy can occur in cysts located in the cervical/thoracic spine or at least above the L1/L2 level. From the literature reviewed, out of 499 cases, 258 (52.5%) had back pain, 303 (61.7%) and 116 (23.6%) had painful radiculopathy and neurogenic claudication, respectively, 183 (37.2%) had motor deficits, 187 (38%) had sensory loss and 175 (35.2%) demonstrated reflex disturbances. Radicular pain with acute onset may be associated with intracystic hemorrage and can be a result of both acute cyst distention or compression of a nervous element [32, 36]. Symptoms may simulate a herniated nucleus pulposus, lumbar stenosis or facet joint syndrome, all of which are more common [2, 13, 28].
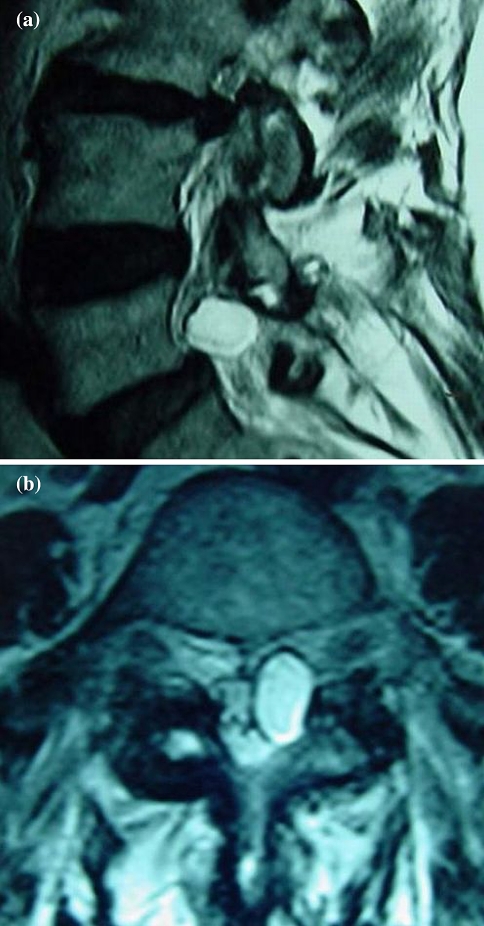
Undoubtedly, MRI is the modality of choice for the diagnosis of juxtafacet cysts [1, 7, 24, 27–29, 41, 46]. It has a 90% sensitivity compared to 70% of CT scanning [14, 20]. In our cases reported, all diagnoses were achieved preoperatively by lumbar spine MRI (Fig. 2a, b). A typical synovial cyst appears with low-intensity signal in T1-weighted images and a high-intensity signal in T2-weighted sequences [31]. However, this signal can vary depending on the proteinaceous concentration of the fluid or even the presence of blood [30]. In the past, CT myelography has also been used in the diagnosis of synovial cysts but is now only used when MR imaging is not available or cannot be performed (metallic prosthesis etc.).
Fig. 2.
T2-weighted sagittal (a) and axial (b) MR scan of a spinal synovial cyst located at the L4–L5 level (case 1)
The optimal treatment remains a matter of debate. Even though there have been reports of synovial cysts resolving spontaneously, they will usually require treatment [30]. This can be either conservative or surgical. Conservative treatment consists of bed rest, analgesics and anti-inflammatory drugs, physical therapy, bracing, transcutaneous electrical stimulation, epidural or intra-articular steroid injections and cyst aspiration. Although conservative treatment has been proposed in certain reports, the results are rather disappointing, especially in series follow-up over 6 months [17, 30, 41, 42]. In a large European study including 77 patients, failure rates with conservative treatment reached 60% at 6 months, and finally patients that initially received conservative treatment had to undergo surgery because of absence of sustained benefit [31]. In a retrospective analysis of data collected from 30 non-surgically treated patients, only 10 (33%) had an excellent or good outcome 6 months after treatment while 47% of these patients finally had to undergo surgery [34]. In another literature review, Shah and Lutz [42] identified 139 patients treated conservatively, out of which 47% finally received surgical treatment due to absence of sustained benefit. Similarly, Hsu et al. had a success rate of 55% with conservative therapy, while in another series of treatment by corticosteroid injection the long-term success rate did not exceed 57% [3, 5, 45]. Furthermore, most authors reporting results of conservative treatment have rather short follow-up periods [24, 30]. Therefore, surgical treatment can be recommended as soon as simple conservative methods (bed rest, physiotherapy, analgesics) fail to control the symptoms or as soon as neurologic deficits develop. Older and high-risk patients may benefit from cyst aspiration or steroid injection. On the other hand, surgery seems to be associated with high rates of a favorable outcome. In the literature reviewed, the overall “excellent” outcomes were as high as 75%, 14% scored a “good” outcome while 11% of the cases had a “fair/poor” result. Taken together, 83% of the cases reviewed (382 out of 413 patients) had an excellent or good result. These rates are significantly higher compared with those reported from a series of conservatively treated patients and are collected from reports with a follow-up period of at least 6 months.
The surgical technique to be used remains a matter of debate and varies depending on the cyst size, its adhesion to the dura and the presence of concomitant local pathologies. Metellus et al. advocate performing medial facetectomy along with hemilaminectomy, suggesting that this technique helps prevent recurrence [31]. Not all authors agree with this technique, for the fear of producing spinal instability, but in a large retrospective analysis by Lyons et al. [27], no correlation between the extent of laminectomy and/or facetectomy and the development of symptomatic spondylolisthesis was identified. Trummer et al. found no statistically significant difference between the type of surgical approach and the final outcome [45]. The procedure of choice should be the one that the surgeon believes will best enable complete resection of the cyst and treatment of any coinciding disease in the safest way possible, because excising the cyst seems to be the single-most important factor for a favorable outcome. Thus, the surgical approach should be tailored to the individual patient. Partial hemilaminectomy with medial facetectomy is usually sufficient. Microsurgical procedures are preferred in small cysts, as they allow a satisfactory outcome with minimal surgical trauma whilst enabling early patient mobilization [22]. Larger cysts are more likely to be adherent to the dura, and in these cases a more extensive procedure may be appropriate. However, persistence to achieve gross-total resection of the cyst risking neural damage is not justified, especially if the nerve root is adequately decompressed.
Controversy exists as to the need of concomitant fusion as a first-line treatment. In a retrospective analysis of 39 surgically treated cases, Khan et al. concluded that patients who underwent spinal fusion along with laminectomy tended to have better rates of excellent or good outcomes compared with those who had had decompression surgery alone (80% vs. 70%) [22]. On the contrary, several other reports including a total of 54 patients, 18 of whom had concomitant fusion, show no difference in outcome between the two groups [14, 21, 39]. Similarly, in a series of 60 juxtafacet cysts, Sabo et al. [39] found no difference in outcome for those patients undergoing fusion compared to those treated with cyst excision alone. In the largest series published so far, Lyons et al. reported that out of 194 patients treated surgically for synovial cysts, 18 (9.3%) underwent cyst excision and fusion as a first-line treatment, even though spondylolisthesis was observed in 50% of those 194 patients pre-operatively. Subsequent fusion had to be performed in only four patients because of delayed symptomatic spondylolisthesis. It is worth noting that of those four patients, only one had pre-operative evidence of spondylolisthesis [27] (Table 2). From the literature available to us, only 54 (38.3%) patients out of a total of 141 who had evidence of preoperative spondylolisthesis had fusion along with cyst excision. Cyst excision alone as a first-line treatment was deemed enough in 88.6% of the total patients treated. Thus, it seems that spondylolisthesis is neither an absolute indication for arthrodesis when operating on synovial cysts, nor does it increase spinal instability thus requiring late fusion, unless extensive, multi-level laminectomies are performed. Only 9 out of 499 patients (1.8%) in the literature reviewed had to undergo late fusion because of post-operative spinal instability. In our cases, all but one patient underwent flexion–extension radiographs at 6 and 12 months post-operatively. No signs of instability were present.
Table 2.
Overview of the number of patients, treatment and outcome in the largest case-series reviewed
| Author | N | Treatment | Outcome | Comments | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| C | LS | S | S + F | S + LF | E | G | F/P | |||
| Freidberg et al. [13] | 26 | 0 | 0 | 26 | 0 | 2 | 17 | 7 | 1 | |
| Howington et al. [16] | 28 | 0 | 0 | 27 | 1 | 0 | 20 | 3 | 5* | 3/5 had prior spinal surgery |
| Hsu et al. [17] | 19 | 11* | – | 8 | 0 | 0 | 3 | 4 | 1 | No sustained benefit; no report on subsequent surgery |
| Jonsson et al. [19] | 8 | 1 | 1 | 7 | 0 | 0 | 5 | 3 | 0 | |
| Lyons et al. [27] | 194 | 0 | 0 | 176 | 18 | 4 | 134* | 13 | 47 patients were lost at follow-up | |
| Metellus et al. [31] | 77 | 27 | 27 | 77 | 0 | 1 | 63 | 12 | 2 | |
| Sabo et al. [39] | 56 | 12 | 8 | 48* | 6 | 2 | 40 | 12 | 2 | Three patients developed a contralateral symptomatic cyst |
| Shah et al. [42] | 10 | 10 | 8 | 7 | 1 | 0 | 8 | 0 | ||
| Trummer et al. [45] | 19 | 0 | 0 | 19* | 0 | 0 | 17 | 2 | 0 | One patient had recurrence and was reoperated |
| Yarde et al. [47] | 0 | 0 | 6 | 2 | 0 | 5 (6)* | 2 | 1 (0) | One patient was reoperated with complete resolution of symptoms | |
N number of patients, C conservative treatment, LS late surgery (surgery after conservative treatment failure), S surgery, S + F surgery with fusion, S + LF surgery and late fusion (need for fusion at later time), E excellent, G good, F/P fair/poor, (*) refers to the comment
Development of a new synovial cyst after surgical removal is reported in the literature but is only rare [8, 16, 39, 42]. Recurrence of a previously removed LISC is reported in 5 (1%) cases. Equally rare are the reported perioperative complications (Table 3).
Table 3.
Reported complications in a total of 499 patients
| Complication | Number of patients (total n = 499) |
|---|---|
| CSFleak | 6 |
| Epidural hematoma | 2 |
| Discitis | 1 |
| Non-union after fusion | 1 |
| Seroma | 2 |
| DVT | 1 |
| Wound dehiscence | 1 |
| Perioperative death | 1 |
Conclusion
Even though uncommon, intraspinal synovial cysts seem to be a more common reason for low back and radicular pain than previously thought. It is likely that they are as prevalent as always, but are diagnosed with increasing frequency, partly due to the wide availability of more sophisticated imaging techniques. Their exact pathogenesis is unclear, but their preference for the L4/5 level, the most mobile in the spine, along with their association with spondylolisthesis and osteoarthritis and the fact that these cysts are an ailment of the older population, stress the role of a degenerative process. CT but mainly MRI can establish the diagnosis and help preoperative planning. Conservative treatment is an option in older, fragile patients, but usually yields less favorable results. Surgery is a safe treatment option and offers a higher possibility of a favorable outcome. The advantage of surgery is even more prominent in series with a long follow-up period. The various operative approaches do not seem to differ significantly from each other. The technique that enables complete resection of the cyst with minimal surgical trauma should, in theory, be preferred. However, the size of the cyst, the presence of other local pathology and the surgeon’s personal experience should direct the decision of surgical approach. Fusion as a first-line choice should be performed based on sound surgical judgment and not on the finding of spondylolisthesis alone.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00586-008-0673-2
References
- 1.Apostolaki E, Davies AM, Evans N, et al. MR imaging of lumbar facet joint synovial cysts. Eur Radiol. 2000;10:615–623. doi: 10.1007/s003300050973. [DOI] [PubMed] [Google Scholar]
- 2.Bhushan C, Hodges FJ, 3rd, Wityk JJ. Synovial cyst (ganglion) of the lumbar spine simulating extradural mass. Neuroradiology. 1979;18:263–268. doi: 10.1007/BF00327690. [DOI] [PubMed] [Google Scholar]
- 3.Bjorkengren AG, Kurz LT, Resnick D, et al. Symptomatic intraspinal synovial cyst. Orthopedics. 1994;613:618–620. [Google Scholar]
- 4.Budris DM (1991) Radiologic case study. Intraspinal lumbar synovial cyst. Orthopedics 14:613, 618–620 [DOI] [PubMed]
- 5.Casselman ES. Radiologic recognition of symptomatic spinal synovial cysts. Am J Neuroradiol. 1985;6:971–973. [PMC free article] [PubMed] [Google Scholar]
- 6.Cohen-Gadol AA, White JB, Lynch JJ, et al. Synovial cysts of the thoracic spine. J Neurosurg Spine. 2004;1:52–57. doi: 10.3171/spi.2004.1.1.0052. [DOI] [PubMed] [Google Scholar]
- 7.Davis R, Iliya A, Roque C, et al. The advantage of magnetic resonance imaging in diagnosis of a lumbar synovial cyst. Spine. 1990;15:244–246. doi: 10.1097/00007632-199003000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Deinsberger R, Kinn E, Ungersbock K. Microsurgical treatment of juxta facet cysts of the lumbar spine. J Spinal Disord Tech. 2006;19:155–160. doi: 10.1097/01.bsd.0000188660.31212.83. [DOI] [PubMed] [Google Scholar]
- 9.Doherty PF, Sherman BA, Stein C, et al. Bilateral synovial cysts of the thoracic spine: a case report. Surg Neurol. 1993;39:279–281. doi: 10.1016/0090-3019(93)90005-L. [DOI] [PubMed] [Google Scholar]
- 10.Doyle AJ, Merrilees M. Synovial cysts of the lumbar facet joints in a symptomatic population: prevalence on magnetic resonance imaging. Spine. 2004;29:874–878. doi: 10.1097/00007632-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 11.Eyster EF, Scott WR. Lumbar synovial cysts: report of eleven cases. Neurosurgery. 1989;24:112–115. doi: 10.1097/00006123-198901000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Finkelstein SD, Sayegh R, Watson P, et al. Juxta-facet cysts. Report of two cases and review of clinicopathologic features. Spine. 1993;18:779–782. doi: 10.1097/00007632-199305000-00020. [DOI] [PubMed] [Google Scholar]
- 13.Freidberg SR, Fellows T, Thomas CB, et al. Experience with symptomatic spinal epidural cysts. Neurosurgery. 1994;34:989–993. doi: 10.1097/00006123-199406000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Hemminghytt S, Daniels DL, Williams AL, et al. Intraspinal synovial cysts: natural history and diagnosis by CT. Radiology. 1982;145:375–376. doi: 10.1148/radiology.145.2.7134440. [DOI] [PubMed] [Google Scholar]
- 15.Hodges SD, Fronczak S, Zindrick MR, et al. Extradural synovial thoracic cyst. Spine. 1994;19:2471–2473. doi: 10.1097/00007632-199411000-00020. [DOI] [PubMed] [Google Scholar]
- 16.Howington JU, Connolly ES, Voorhies RM. Intraspinal synovial cysts: 10-year experience at the Ochsner Clinic. J Neurosurg. 1999;91(2 Suppl):193–199. doi: 10.3171/spi.1999.91.2.0193. [DOI] [PubMed] [Google Scholar]
- 17.Hsu KY, Zucherman JF, Shea WJ, et al. Lumbar intraspinal synovial and ganglion cysts (facet cysts). Ten-year experience in evaluation and treatment. Spine. 1995;20:80–89. doi: 10.1097/00007632-199501000-00015. [DOI] [PubMed] [Google Scholar]
- 18.Indar R, Tsiridis E, Morgan M, et al. Intraspinal lumbar synovial cysts: diagnosis and surgical management. Surgeon. 2004;2:141–144. doi: 10.1016/S1479-666X(04)80074-X. [DOI] [PubMed] [Google Scholar]
- 19.Jonsson B, Tufvesson A, Stromqvist B. Lumbar nerve root compression by intraspinal synovial cysts. Report of 8 cases. Acta Orthop Scand. 1999;70:203–206. doi: 10.3109/17453679909011263. [DOI] [PubMed] [Google Scholar]
- 20.Kao CC, Uihlein A, Bickel WH, et al. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. 1968;29:168–172. doi: 10.3171/jns.1968.29.2.0168. [DOI] [PubMed] [Google Scholar]
- 21.Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41:372–376. doi: 10.3171/jns.1974.41.3.0372. [DOI] [PubMed] [Google Scholar]
- 22.Khan AM, Synnot K, Cammisa FP, et al. Lumbar synovial cysts of the spine: an evaluation of surgical outcome. J Spinal Disord Tech. 2005;18:127–131. doi: 10.1097/01.bsd.0000156830.68431.70. [DOI] [PubMed] [Google Scholar]
- 23.Kjerulf TD, Terry DW, Jr, Boubelik RJ. Lumbar synovial or ganglion cysts. Neurosurgery. 1986;19:415–420. doi: 10.1097/00006123-198609000-00014. [DOI] [PubMed] [Google Scholar]
- 24.Koenigsberg RA. Percutaneous aspiration of lumbar synovial cyst: CT and MRI considerations. Neuroradiology. 1998;40:272–273. doi: 10.1007/s002340050584. [DOI] [PubMed] [Google Scholar]
- 25.Kouyialis AT, Boviatsis EJ, Korfias S, et al. Lumbar synovial cyst as a cause of low back pain and acute radiculopathy: a case report. South Med J. 2005;98:223–225. doi: 10.1097/01.SMJ.0000129792.92433.B6. [DOI] [PubMed] [Google Scholar]
- 26.Liu SS, Williams KD, Drayer BP, et al. Synovial cysts of the lumbosacral spine: diagnosis by MR imaging. Am J Neuroradiol. 1989;10:1239–1242. [PMC free article] [PubMed] [Google Scholar]
- 27.Lyons MK, Atkinson JL, Wharen RE, et al. Surgical evaluation and management of lumbar synovial cysts: the Mayo Clinic experience. J Neurosurg. 2000;93(1 Suppl):53–57. doi: 10.3171/spi.2000.93.1.0053. [DOI] [PubMed] [Google Scholar]
- 28.Marion PJ, Kahanovitz N. Lumbar-sacral radiculopathy secondary to intraspinal synovial cyst. Arch Phys Med Rehabil. 1995;76:1011–1013. doi: 10.1016/S0003-9993(95)81039-0. [DOI] [PubMed] [Google Scholar]
- 29.Martin D, Awwad E, Sundaram M (1990) Radiologic case study. Lumbar ganglion cyst causing radiculopathy. Orthopedics 13:1177, 1182–1183 [DOI] [PubMed]
- 30.Mercader J, Munoz Gomez J, et al. Intraspinal synovial cyst: diagnosis by CT. Follow-up and spontaneous remission. Neuroradiology. 1985;27:346–348. doi: 10.1007/BF00339570. [DOI] [PubMed] [Google Scholar]
- 31.Metellus P, Fuentes S, Adetchessi T, et al. Retrospective study of 77 patients harbouring lumbar synovial cysts: functional and neurological outcome. Acta Neurochir (Wien) 2006;148:47–54. doi: 10.1007/s00701-005-0650-z. [DOI] [PubMed] [Google Scholar]
- 32.Miwa M, Doita M, Takayama H, et al. An expanding cervical synovial cyst causing acute cervical radiculopathy. J Spinal Disord Tech. 2004;17:331–333. doi: 10.1097/01.bsd.0000095892.46978.6e. [DOI] [PubMed] [Google Scholar]
- 33.Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22:642–647. doi: 10.1097/00006123-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Parlier-Cuau C, Wybier M, Nizard R, et al. Symptomatic lumbar facet joint synovial cysts: clinical assessment of facet joint steroid injection after 1 and 6 months and long-term follow-up in 30 patients. Radiology. 1999;210:509–513. doi: 10.1148/radiology.210.2.r99fe60509. [DOI] [PubMed] [Google Scholar]
- 35.Pendleton B, Carl B, Pollay M. Spinal extradural benign synovial or ganglion cyst: case report and review of the literature. Neurosurgery. 1983;13:322–326. doi: 10.1097/00006123-198309000-00021. [DOI] [PubMed] [Google Scholar]
- 36.Ramieri A, Domenicucci M, Seferi A, et al. Lumbar hemorrhagic synovial cysts: diagnosis, pathogenesis, and treatment. Report of 3 cases. Surg Neurol. 2006;65:385–390. doi: 10.1016/j.surneu.2005.07.073. [DOI] [PubMed] [Google Scholar]
- 37.Rosenberg AE, Schiller AL. Tumors and tumor-like lesions of joints and related structures. In: Kelley WN, editor. Textbook of rheumatology, vol 2. 5. Philadelphia: WB Saunders; 1997. pp. 1593–1595. [Google Scholar]
- 38.Rousseaux P, Durot JF, Pluot M, et al. [Synovial cysts and synovialomas of the lumbar spine. Histo-pathologic and neuro-surgical aspects apropos of 8 cases] Neurochirurgie. 1989;35:31–39. [PubMed] [Google Scholar]
- 39.Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560–565. doi: 10.3171/jns.1996.85.4.0560. [DOI] [PubMed] [Google Scholar]
- 40.Sachdev VP, Savitz MH, Hindi Ai, et al. Synovial cysts of the lumbar facet joint. Mt Sinai J Med. 1991;58:125–128. [PubMed] [Google Scholar]
- 41.Sauvage P, Grimault L, Ben Salem D, et al. Lumbar intraspinal synovial cysts: imaging and treatment by percutaneous injection. Report of thirteen cases. J Radiol. 2000;81:33–38. [PubMed] [Google Scholar]
- 42.Shah RV, Lutz GE. Lumbar intraspinal synovial cysts: conservative management and review of the world’s literature. Spine J. 2003;3:479–488. doi: 10.1016/S1529-9430(03)00148-7. [DOI] [PubMed] [Google Scholar]
- 43.Song JK, Musleh W, Christie SD, et al. Cervical juxtafacet cysts: case report and literature review. Spine J. 2006;6:279–281. doi: 10.1016/j.spinee.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 44.Tillich M, Trummer M, Lindbichler F, et al. Symptomatic intraspinal synovial cysts of the lumbar spine: correlation of MR and surgical findings. Neuroradiology. 2001;43:1070–1075. doi: 10.1007/s002340100682. [DOI] [PubMed] [Google Scholar]
- 45.Trummer M, Flaschka G, Tillich M, et al. Diagnosis and surgical management of intraspinal synovial cysts: report of 19 cases. J Neurol Neurosurg Psychiatry. 2001;70:74–77. doi: 10.1136/jnnp.70.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Weyns F, Calenbergh F, Goffin J, et al. Intraspinal juxta-facet cysts: a case of bilateral ganglion cysts. Clin Neurol Neurosurg. 1992;94:55–59. doi: 10.1016/0303-8467(92)90120-R. [DOI] [PubMed] [Google Scholar]
- 47.Yarde WL, Arnold PM, Kepes JJ, et al. Synovial cysts of the lumbar spine: diagnosis, surgical management, and pathogenesis. Report of eight cases. Surg Neurol. 1995;43:459–464. doi: 10.1016/0090-3019(95)80090-4. [DOI] [PubMed] [Google Scholar]