Abstract
The association of occupational exposures and asthma were studied in 14151 adults, aged 25–59 years, from the general population of the French PAARC (Pollution Atmospherique et Affections Respiratoires Chroniques, 1975) Survey. Associations of asthma to specific jobs such as personal care workers, waiters, stock clerks were observed, with age, sex, smoking adjusted odds ratios between 1.5 and 1.7. Exposures to 18 asthmagenic agents (low, high molecular weight and mixed environment) were estimated by an asthma-specific job exposure matrix. Risks associated with asthma increased when excluding subjects with imprecise estimates of exposure. Risks further increased when increasing specificity of the definition of asthma considering jobs or specific agents such as industrial cleaning agents, latex, flour, highly reactive chemicals, and textiles. For example, for industrial cleaning agents, odds ratios increased from 1.55 (95% CI: 1.08, 2.23) for ever asthma, to 2.51 (95% CI: 1.33, 4.75) for asthma with airflow limitation, to 2.17 (95% CI: 1.41, 3.34) for asthma onset after age 14, and to 2.35 (95% CI: 1.38, 4.00) for asthma onset after beginning of current job. Results underlined the importance of the specificity of exposure and asthma definitions and indicated a deleterious role of occupational exposure on asthma, especially for cleaning agents.
Keywords: Adult, Asthma, etiology, Epidemiologic Methods, Female, France, epidemiology, Humans, Male, Middle Aged, Occupational Exposure, adverse effects, Occupations, classification, Population Surveillance, methods, Questionnaires, Risk Factors, Smoking, adverse effects
Keywords: asthma, occupational diseases, occupations, occupational exposures, job exposure matrix
Occupational asthma is commonly defined as asthma caused by exposure to agents at work (1–2), although some authors have included pre-existing asthma aggravated by occupational exposures (3); others have used the term work-related asthma for both conditions (4–7). In population-based studies, it is often impossible to identify occupational asthma, as information about the age of onset of asthma and its relation to the onset of exposure is not recorded (8–12). Thus, the proportion of asthma attributable to occupational exposure varies according to the definitions of asthma and exposure used, and is reported to vary from five to more than thirty percent in the US and Europe (3–6).
The strength of the association between occupational exposures and asthma may also be underestimated in workplace based studies due to the healthy worker effect. This selection bias is less important in population based studies; however, few population based studies have analysed the role of specific exposures (3–4, 8–9, 11–15), due, in part, to difficulties in obtaining unbiased, valid estimation of occupational exposures in large studies relying on questionnaires for exposure assessment (7, 16). Categorization of exposure based on job title alone, often recorded in population based studies, is considered a poor indicator of exposure to asthmagens (7, 16). Self-reported exposure, estimated by questionnaire, may lead to some degree of recall bias (16). More recently, expert review methods (16) and Job Exposure Matrices (JEM) (13–16) have been used in large populations in an attempt to provide greater precision in exposure estimates based on job titles. Two JEM have been used to study occupational risk factors for asthma, one which estimated exposure classified in three broad groups: biological dusts, mineral dusts, and fumes/gases (13) and a second which estimates exposures to specific asthmagenic agents (14).
In the French PAARC (Pollution Atmospherique et Affections Respiratoires Chroniques) Survey, in previous analyses five estimates of exposure, self-reported exposure (17–20), three cancer-specific JEM (18, 20–21) and a population-specific JEM (19) were used to study associations between occupational exposure and asthma or lung function. Positive associations between self-reported exposure to dusts, gases, and fumes and asthma were observed whereas no association was found when exposure was estimated by a JEM (18). Our objective was to investigate, in the PAARC Survey, the associations between occupational exposure (estimated using four methods suitable for large population studies) and asthma (defined in four ways) in an attempt to examine the role of increasing specificity of both definitions on associations seen.
MATERIALS AND METHODS
Population
The PAARC Survey was carried out, in 1975, in seven French cities, on 20310 subjects, aged twenty five to fifty-nine years, surveyed at home. More detailed protocol has been published elsewhere (17, 22). The primary aim was to investigate the effect of air pollution on respiratory outcomes; thus, households headed by industrial manual workers (mostly men) were excluded to reduce the effect of occupational exposure. Other manual workers such as craftsmen were included.
Smoking habits, asthma
The questionnaire was based on the British Medical Research Council/European Coal and Steel Community questionnaire. Subjects were classified in five categories as non smokers, ex-smokers, light, moderate and heavy smokers based on grams of tobacco smoked per day. Questions regarding asthma were “Have you ever had attacks of breathlessness with wheezing?”, “Have you ever had asthma attacks?” and if yes to one of the previous questions, subjects were asked: “Age at the first attack?”, “Age at the last attack?”. For this analysis ‘ever asthma’ was defined as a positive response to at least one of the two first questions. Additional definitions were used to characterise more specific phenotypes. A surrogate for severe asthma was estimated by combining a positive report of asthma symptoms with airflow limitation data, as no other markers of severity were available in the PAARC Survey. Thus, ‘asthma with airflow limitation’ was defined as ‘ever asthma’ plus FEV1/FVC less than 88% of predicted value in men and 89% in women, based on the European reference values (23). Two specific definitions of adult onset asthma were used, asthma onset at or after age fourteen and asthma onset after beginning of the current job. Fourteen years old was chosen because it corresponded, for many people born between 1916 and 1950 (ie. the PAARC generation), as the age of beginning work or apprenticeship.
Estimates of exposure
Four estimates of exposure were used and summarized in figure 1. First, self-reported exposure to dusts, gases, and fumes was estimated by response to this question “Were you exposed to dusts, gases or chemical fumes?” in the current or most recent occupation. Second, job titles, coded using French national codes, were grouped into twenty-nine categories, based on categorization schemes previously used by other authors (24, 25) and compared to a reference group of administrative and service jobs. Third, a population-specific JEM for ‘dusts, gases, and fumes’ was constructed using self-reported exposure and job codes as previously described (19). Briefly, each job code was classified as either ‘exposed to dusts, gases, and fumes’ or ‘not-exposed’, based on the proportion of subjects holding that job who declared themselves exposed. The exposure is estimated by job codes and then ascribed to all subjects with this job. The cut-off proportion to distinguish ‘exposed’ and ‘not-exposed’ jobs was selected a priori to ensure that the overall percentage of persons classified as ‘exposed’ to dusts, gases, and fumes would be equal whether one used the JEM or self report (figure 1). Fourth, an asthma-specific JEM (14) was used to estimate exposure to asthmagenic agents, after translation of French codes (26) into International Standard Classification of Occupations codes (ISCO88, 27). The asthma JEM (which assigns exposure estimates for all ISCO88 job codes) was developed for the EGEA (Epidemiological study on the Genetics and Environment of Asthma) survey (28) and was constructed to favour specificity over sensitivity (a job was classified as exposed only if the probability of exposure was expected to be high). For each ISCO88 code, the JEM classifies the job as ‘exposed’ or not to three non asthmagenic agents (chemicals (low level); irritants (not high peaks); exhaust fumes) and to 18 asthmagenic agents as previously described (14), further grouped as high molecular weight (HMW), low molecular weight (LMW) asthmagens or mixed environments (figure 1). The asthma JEM also identifies job codes for which its exposure estimates are likely to be poorly defined. Therefore, analyses using this JEM were repeated after exclusion of jobs with such poorly defined exposures.
FIGURE 1. Description of exposure assessment methods, PAARC Survey, 1975.
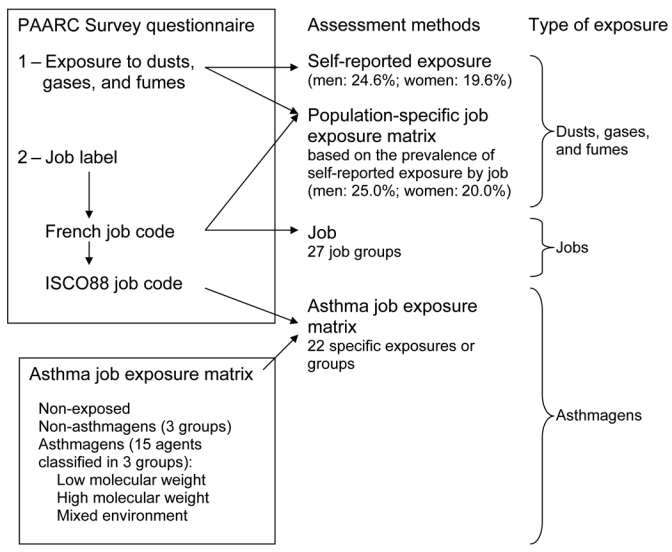
Population-specific job exposure matrix:
Very close to the prevalence of self-reported exposure by construction, corresponding at job level for men/women to jobs with more than 33/30% of positive response to self-reported exposure [Le Moual et al, Occup Environ Med 2000; 57: 126-32] (19).
Asthma job exposure matrix:
In the PAARC Survey, job label was not computerized and questionnaires were destroyed. Therefore it was not possible, to apply the recommended expert review step [Kennedy et al, Occup Environ Med 2000; 57: 635-41] (14). This step involves review of the exposure estimates assigned by the asthma job exposure matrix, for some poorly defined job codes using job label text.
As previously published (14), asthmagenic agents were classified in three groups as either high molecular weight (rodents; fish; arthropods or mites; latex; flour; other plants; bio aerosols; biological enzymes), low molecular weight (highly reactive chemicals; isocyanates; sensitising drugs; industrial cleaning agents; wood dusts; metal sensitisers) asthmagens or mixed environments (metal working fluids; agriculture; textile production; accidental exposure to high levels of irritant).
PAARC, Pollution Atmosphérique et Affections Respiratoires Chroniques.
ISCO888, International Standard Classification of Occupations codes.
Data analysis
Analysis were performed on 14151 subjects (7255 men, 6896 women), without missing data for asthma, job code, self-reported exposure to dusts, gases, and fumes, and JEM estimates. Analyses were performed for specific asthmagenic agents when at least 100 subjects were classified as exposed. Subjects with missing data for age of first and last asthma attacks (n=227) were included in the analyses of ‘ever asthma’ and ‘asthma with airflow obstruction’ but excluded in analyses of adult onset asthma. Of these 227 subjects, 89 percent reported only a positive response to “attacks of breathlessness with wheezing” but not to “asthma attacks”. Compared to asthmatics with age of onset after 14 years, subjects with missing values were more likely to be smokers (46% vs 36%), less likely to have airflow obstruction (22% vs 26%), but similar with respect to age, gender, and occupational exposure.
Attributable risks were calculated for the four definitions of asthma considering exposure to dusts, gases, and fumes and to asthmagenic agents, and by gender, as follows: “proportion exposed X (odds ratio – 1)” divided by “(proportion exposed X (odds ratio –1)) + 1”, using exposure prevalence estimates specific to this French population (which excludes households headed by manual workers).
RESULTS
Description of the population
Subjects were, on average, about forty-two years old (table 1). The prevalence of ‘ever asthma’ was seven percent in men and women and less than two percent for ‘asthma with airflow limitation’. The prevalence of adult onset asthma was higher in women than men. Twenty five percent of men and twenty percent of women declared themselves exposed to dusts, gases, and fumes. By design, the prevalence of exposure was similar according to the population-specific JEM. According to the asthma JEM, the prevalence of exposure to asthmagenic agents was about three times higher among women than men whereas the prevalence of exposure to non-asthmagenic agents was about three times higher in men than women. Almost half of the jobs held by women were considered to have imprecise estimates of exposure by the JEM, a proportion considerably less in men.
TABLE 1.
Description of the PAARC population in 1975
| Men (n=7255) | Women (n=6896) | |
|---|---|---|
| Age, mean (SD) | 43.0 (9.4) | 41.9(9.6) |
| Age at beginning of current job | 27.8 (8.7) | 26.5 (9.4) |
| Smoking habits: | ||
| Non smokers, percent | 25.2 | 71.0 |
| Ex-smokers, percent | 17.0 | 6.1 |
| Smokers, percent | 57.8 | 22.9 |
| Definitions of asthma | ||
| Ever asthma | 6.9 | 6.9 |
| Asthma with airflow limitation | ||
| Asthma and European reference values for airflow limitation (FEV1/FVC< 88% of predicted value in men, 89% in women), percent | 1.9(n=6880) | 1.6(n=6524) |
| Adult onset asthma | ||
| Asthma onset at or after 14 years old | 3.3 (n=7094) | 3.8(n=6816) |
| Asthma onset at or after beginning of current job | 1.8 (n=6988) | 2.2 (n=6706) |
| Occupational exposure | ||
| Self-reported exposure to dusts, gases, and fumes, percent | 24.6 | 19.6 |
| Occupational exposure estimated by the population-specific job exposure matrix, percent* | 25.0 | 20.0 |
| Occupational exposure estimated by an asthma-specific job exposure matrix † | ||
| Exposed to non-asthmagen substances, percent | 9.5 | 3.0 |
| Exposed to asthmagen substances, percent | 8.0 | 21.7 |
| Occupational exposure estimated by an asthma-specific job exposure matrix - Job with more precise estimates of exposure | (n=5178) | (n=5382) |
| Exposed to non-asthmagen substances, percent | 8.8 | 1.7 |
| Exposed to asthmagen substances, percent | 6.3 | 10.9 |
Similar to self-reported exposure by design [Le Moual et al, Occup Environ Med 2000; 57: 126–32] (19).
According to published matrix [Kennedy et al, Occup Environ Med 2000; 57: 635–41] (14).
FEV1, forced expiratory volume in one second.
FVC, forced vital capacity.
PAARC, Pollution Atmosphérique et Affections Respiratoires Chroniques.
Association between job title and different definitions of asthma
A significant excess of risk of ‘ever asthma’ was observed for stock clerks and an excess risk of borderline significance was observed for personal care workers and restaurant workers (table 2), with similar results for the three other definitions of asthma (not shown). For personal care workers, odds ratios were elevated (around 2.5) for all other definitions of asthma and associations were significant. Associations were significant or of borderline significance with odds ratios around or greater than two for cleaners, hairdressers, laboratory aids, bakers, textile workers, leather workers, restaurant workers, stock clerks and child care workers for at least one of the three other definitions of asthma.
TABLE 2.
Risk of asthma according to occupational groups and asthma definition, PAARC Survey, 1975
| Ever asthma n=14151 | |||
|---|---|---|---|
| Job | n | Odds ratio | CI 95% |
| Administrative, service (reference category)* | 8428 | 1 | - |
| Cleaners | 404 | 1.04 | 0.70, 1.54 |
| Nurses | 295 | 1.15 | 0.74, 1.80 |
| Hairdressers | 154 | 0.65 | 0.30, 1.40 |
| Laboratory assistants | 41 | 1.68 | 0.59, 4.78 |
| Wood workers | 38 | 1.11 | 0.34, 3.65 |
| Food workers | 195 | 0.98 | 0.55, 1.73 |
| Bakers, pastry-cooks | 130 | 1.11 | 0.58,2.12 |
| Chemical workers | 52 | 0.85 | 0.26, 2.75 |
| Electricity workers | 73 | 1.43 | 0.65,3.16 |
| Painters | 60 | 0.97 | 0.35, 2.69 |
| Construction workers | 138 | 0.71 | 0.32, 1.52 |
| Transport | 91 | 0.93 | 0.40,2.15 |
| Institution-based personal care workers | 176 | 1.57 | 0.96, 2.58 |
| Physiotherapists | 63 | 0.73 | 0.23, 2.34 |
| Medical doctors, midwives | 241 | 0.97 | 0.58, 1.62 |
| Dentists | 52 | 1.45 | 0.57, 3.66 |
| Pharmacists | 76 | 0.75 | 0.27, 2.06 |
| Child-care workers | 59 | 1.82 | 0.82, 4.05 |
| Building caretakers | 61 | 0.66 | 0.21,2.13 |
| Draughtspersons | 193 | 0.67 | 0.34, 1.31 |
| Freight handlers | 74 | 0.56 | 0.18, 1.80 |
| Stock clerks | 225 | 1.75 | 1.14,2.68 |
| Restaurant, hotel workers | 216 | 1.51 | 0.96, 2.37 |
| Mail carriers and sorting clerks | 75 | 0.76 | 0.27, 2.09 |
| Motor mechanics | 75 | 0.97 | 0.39, 2.42 |
| Textile workers | 342 | 0.94 | 0.60, 1.47 |
| Leather workers | 45 | 0.94 | 0.29, 3.04 |
| Other jobs, poorly defined or with less than 40 subjects | 2345 | 0.87 | 0.71, 1.07 |
Odds ratios were adjusted on age, smoking habits and sex.
The first 13 job sets are similar to those of Kogevinas et al [Am J Respir Crit Care Med 1996; 154 :137–43] (25).
PAARC, Pollution Atmospherique et Affections Respiratoires Chroniques.
CI, confidence interval.
Association between exposure to dusts, gases, and fumes and asthma
Associations between all four definitions of asthma and exposure to dusts, gases, and fumes were studied (table 3). As previously described, significant associations were found between asthma and self-reported exposure to dusts, gases, and fumes (18), but not for exposure using the population-specific JEM for dusts, gases, and fumes exposure. Using the three other definitions of asthma, conclusions were similar although odds ratios were slightly higher.
TABLE 3.
Odds ratios according to different definitions of asthma and occupational exposure, PAARC Survey, 1975
| Total | Ever asthma n=14151 | Asthma with airflow limitation n=13404 | Asthma onset at/after 14 years old n=13654 | Asthma onset at/after beginning of current job - n=13445 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Exposed/non exposed | Odds ratio | CI 95% | Odds ratio | CI 95% | Odds ratio | CI 95% | Odds ratio | CI 95% | |
| Asthmatic/non asthmatic | - | 976/13175 | 229/13175 | 479/13175 | 270/13175 | ||||
| Exposure to dusts, gases, and fumes | |||||||||
| Self-reported | 3134/11017 | 1.45 | 1.25, 1.67 | 1.51 | 1.17,2.01 | 1.47 | 1.20, 1.80 | 1.75 | 1.35,2.28 |
| Population-specific job exposure matrix | 2952/11199 | 1.02 | 0.87, 1.20 | 1.26 | 0.93, 1.70 | 1.12 | 0.90, 1.40 | 1.17 | 0.88, 1.56 |
| Asthma job exposure matrix | |||||||||
| Asthmagens, any | 2079/12072 | 1.10 | 0.92, 1.32 | 1.60 | 1.14,2.23 | 1.15 | 0.90, 1.48 | 1.24 | 0.90, 1.71 |
| High molecular weight agents | 950/12072 | 1.24 | 0.97, 1.59 | 1.52 | 0.93, 2.48 | 1.32 | 0.95, 1.85 | 1.21 | 0.77, 1.91 |
| Low molecular weight agents | 1001/12072 | 1.13 | 0.88, 1.44 | 1.61 | 1.04,2.49 | 1.25 | 0.90, 1.73 | 1.52 | 1.02,2.25 |
| Mixed environments or agents | 447/12072 | 0.98 | 0.67, 1.43 | 1.89 | 1.03,3.45 | 1.12 | 0.69, 1.83 | 1.16 | 0.63,2.16 |
| Job with more precise estimates of exposure - Asthma job exposure matrix | n= 10560 | ||||||||
| Asthmagens, any | 915/9645 | 1.17 | 0.90, 1.51 | 1.98 | 1.28,3.07 | 1.38 | 0.99, 1.94 | 1.74 | 1.17,2.60 |
| High molecular weight agents | 238/9645 | 1.59 | 1.04,2.45 | 1.67 | 0.67,4.14 | 2.03 | 1.18,3.48 | 2.09 | 1.05,4.17 |
| Low molecular weight agents | 820/9645 | 1.20 | 0.91, 1.56 | 1.87 | 1.17,2.99 | 1.40 | 0.98, 1.99 | 1.76 | 1.16,2.68 |
| Mixed environments or agents | 129/9645 | 1.05 | 0.53, 2.08 | 3.21 | 1.38,7.46 | 1.39 | 0.61,3.20 | 1.97 | 0.79, 4.91 |
Odds ratios were adjusted on age, smoking habits and sex.
PAARC, Pollution Atmosphérique et Affections Respiratoires Chroniques.
CI, confidence interval.
Associations between asthma and specific agents using the asthma-specific JEM
For non asthmagenic agents identified by the asthma JEM, no associations were found (table 3), whatever the definition of asthma used (not shown).
Overall, for asthmagenic agents no significant associations with ‘ever asthma’ were found, except for a borderline significant association for HMW agents. For asthma with airflow limitation, odds ratios were higher than for ‘ever asthma’ for exposure to any asthmagen, HMW, LMW, and mixed agents and associations were significant for all agents except HMW agents. Using the two definitions of adult onset asthma, intermediate odds ratios between asthma and asthma with airflow limitation were observed for exposure to any asthmagen, and each specific asthmagen.
After exclusion of subjects with jobs with imprecise estimates of exposure, all odds ratios were higher for all asthma definitions, with significantly elevated odds ratios for asthma after onset of the current job associated with any asthmagen, HMW, and LMW agents. For HMW agents, the increase in odds ratios across all definitions of asthma was greater than for the three other exposure classes. Analyses stratified by gender (not shown) indicated that the significant associations between exposure to asthmagens (all classes) identified by the JEM and asthma with airflow limitation were more pronounced among women while associations between exposures and asthma with onset after beginning of the current job were more pronounced among men.
Association between JEM specific asthmagen exposure estimates and asthma
Overall, results in analyses for specific asthmagens (not shown) with at least 100 subjects exposed (ie. HMW: arthropods, latex, flour; LMW highly reactive chemicals, sensitising drugs, industrial cleaning agents, metal sensitisers; and mixed agents: textiles) were consistent with those for grouped exposures. Significant associations were found between asthma and industrial cleaning agents for all definitions of asthma and all exposure estimates, with odds ratios (OR) varying from 1.51 (95%CI: 1.05, 2.16) to 2.51 (95%CI: 1.33, 4.75). A significant association was observed for latex (OR=1.37, 95%CI: 1.02, 1.86) whereas no significant associations were found for flour and highly reactive chemicals in relation to ‘ever asthma’. Associations became significant between exposure to flour and highly reactive chemicals and at least two of the more specific definitions of asthma with odds ratios about two times higher than for ‘ever asthma’. The associations between exposure to flour and asthma with airflow limitation and adult onset asthma were significant only for men (of note, in this survey, all asthmatic men exposed to flour were the lowest quintile for FEV1).
After exclusion of jobs with imprecise estimates of exposure, odds ratios increased further for latex (OR=2.11, 95% CI: 1.06, 4.21) and textile production jobs (OR=3.16, 95% CI: 1.13, 8.82) and associations were significant for two out of the three other definitions of asthma.
Exposure to highly reactive chemicals, cleaning agents, and latex were highly correlated and could not be examined in the same model. A model including a four-class variable (not exposed to asthmagens, exposed to latex alone, exposed to highly reactive chemicals alone, exposed to cleaning agents) showed significant associations for industrial cleaning agents (OR=1.50, 95% CI: 1.04, 2.18) with similar odds ratios in men and women and no associations for exposure to latex alone (OR=1.28, 95% CI: 0.89, 1.85) or highly reactive chemicals alone (OR=0.92, 95% CI: 0.58, 1.48). Similar associations were found after exclusion of poorly defined jobs or using either definitions of adult asthma onset. Significant associations were found for exposure to highly reactive chemicals (OR=2.25, 95% CI: 1.17, 4.33) and cleaning agents (OR=2.16, 95% CI: 1.12, 4.17) in relation to asthma with airflow limitation.
Asthma with airflow limitation
To examine the possibility that the associations seen between exposure and asthma with airflow limitation were more an indication of links between exposure and airflow limitation (than with asthma), we repeated the analyses among non-asthmatic subjects comparing those with and without airflow limitation. No association was found between self-reported exposure to dusts, gases, and fumes and airflow limitation. Associations of borderline significance were found for exposure to dusts, gases, and fumes estimated by the population-specific JEM and for any asthmagens estimated by the asthma JEM with an OR of 1.15. No associations were observed for any of the LMW agents or HMW except for arthropods or mites, risks not found for asthma. For mixed environments, an association of borderline significance was observed with an OR lower than for asthma. Using two other definitions of airflow limitation (FEV1 less than 80% of predicted value and FEV1/FVC less than 75 %), odds ratios were similar to those shown here.
Attributable risk
Estimations of attributable risk for occupational exposure and asthma varied depending the definitions of exposure and asthma used. Considering self-reported exposure to dusts, gases, and fumes, attributable risks varied from 9% (‘ever asthma’) to 14% (asthma onset after current job). Considering exposure to any asthmagens, attributable risks varied from 1% (ever asthma), to 3% (asthma onset after current job) to 8% (asthma with airflow limitation). Attributable risks also tended to increase when jobs with imprecise exposure estimates were excluded (eg. for asthma onset after current job, attributable risk increased from 3% to 7%).
DISCUSSION
In summary, these analyses showed that the strength of the associations observed between exposure and asthma differed according to different definitions of exposure and asthma and that increasing the specificity of the asthma definition and the occupational exposure estimates increased the strength of associations seen. Furthermore, the results indicated a deleterious role for occupational asthmagen exposure for both low and high molecular agents.
Specificity and appropriate exposure estimates
These analyses showed increases in odds ratios by increasing specificity of both exposure and disease. This is consistent with other results (12, 13, 14, 25, 29). For example, in a Spanish population based survey (25) and a Dutch survey on farmers (29), odds ratios increased after restricting the definition of asthma to include only subjects with bronchial hyper-responsiveness.
Our results suggest that it is not only important to favour specificity in the asthma definition, but also to take into account relevant exposure periods for occupational asthma (14). Ideally, to estimate the association between occupational exposures and asthma, complete occupational and school histories and complete asthma history (with onset and periods of remission) are needed in identify appropriate exposures windows. This is consistent with results of de Marco et al (30), who studied the association between disease and exposure before and after taking into account exposure at the time of the disease (25) or subjects without changes in employers (12) and found increased odds ratios in both cases. This is especially important for work-related asthma as the relevant exposure is more likely the exposure in the job held at the time of asthma onset or exacerbation. However, our results indicate that in large population-based surveys, where insufficient data are available to accurately define exposure windows, taking into consideration age of onset of asthma even in relation to the current job may provide more valid estimate of the risk of work-relatedness of asthma than simply assessing ‘ever asthma’ in relation to exposures. This was also seen in the Spanish component of the ECRHS (European Community Respiratory Health Survey), in which a higher risk was seen for occupational exposure for adult onset asthma (25).
A limitation of this study was that it was necessary to apply the asthma JEM without the recommended step of reviewing exposure estimates for some jobs using job title text (14). This step was designed so that known between-country differences in exposure risks could be incorporated into the estimates and to improve the specificity of estimates for very broadly defined job codes. In the initial report in which the asthma JEM was applied in the EGEA survey, analyses on about 450 subjects showed that the strength of association of asthmagen exposures to asthma increased when adding the review step (14). However, because only codes had been retained in the PAARC dataset, this step was not possible here. Our results suggest that the use of the asthma JEM was still valuable, even though the questionnaire contained only very basic information about job titles and only codes were available. Previous analyses of French, Dutch, and Norwegian community studies had suggested that to apply the JEM alone (without the review step) more than two thousand subjects are needed (20); similarly, in the ECRHS survey (15) with about 1500 subjects, odds ratios did not change appreciably after the review step. Similar to results seen in the EGEA study in which the asthma JEM was first used (14), in the current analysis, odds ratios increased when jobs with imprecise estimates of exposure were excluded.
Self-reported exposure to dusts, gases, and fumes
The positive association observed in this study between asthma and self-reported exposure to dusts, gases, and fumes is consistent with other studies in which odds ratios for this association were between 1.2 to 3.0 (9, 11, 13, 18). In contrast, in a previous analysis of the PAARC Survey (18) and in the ECRHS Survey (15), no association was found between asthma and exposure to dusts, gases, and fumes estimated by an independent JEM. This is consistent with the present negative results regarding exposure to dusts, gases, and fumes using the population-specific JEM and to non-asthmagens from the asthma JEM. An association between asthma and exposure to any dusts, gases, and fumes is not a priori expected unless there is a high prevalence of exposure to asthmagen agents in the studied population, or if there is reporting bias by asthmatic subjects. In the analysis here and in other surveys (9, 11, 18), odds ratios for the association between asthma and self-reported exposure to dusts, gases, and fumes were higher in women than in men which is consistent with the present observation of greater exposure of women to asthmagens. In summary, these findings suggest that assessing asthma risk using self-reported exposure assessed by a single imprecise question is not sufficiently accurate to be used as a sole exposure estimate as previously underlined (7, 31).
Risk of asthma according to job titles or specific asthmagens
Regarding job titles, associations found in the PAARC Survey are consistent with recent results of reported incidence of occupational asthma in specified jobs in France (34). For cleaning workers (8, 13, 25), restaurant workers (24, 32), personnel care workers (32), and bakers (1–3) our results are consistent with other surveys.
Studying asthmagens, for HMW agents, our results are consistent with results of the ECRHS study (15), using the same asthma JEM (14), except for latex where no association was found in the ECRHS (15) and EGEA (14) surveys. In 1975, subjects of the PAARC Survey were unlikely to have been exposed to latex; therefore the associations seen here most likely reflect the effect of an associated exposure in the same jobs, such as industrial cleaning agents. For LMW agents, our results are consistent with results in the EGEA study (14) where a risk of asthma was found for subjects exposed to industrial cleaning agents and highly reactive chemicals. For mixed environments, associations found for textile production jobs are consistent with other surveys (8, 12, 13, 33).
Our results and others suggest a deleterious role of cleaning agents on asthma (8, 13, 14, 25, 32, 34–35), and a high risk of asthma in cleaners (10) in both private homes (35) and offices (8, 13). The use of industrial cleaning agents in 1975 among PAARC subjects was also found to have a deleterious effect on both asthma and lung function (21). These associations are probably not due to the same agents in 1975 and now. Other workers such as personnel care workers could also be exposed to cleaning agents probably different from those used by cleaners. Further studies are needed to better estimate respiratory health in cleaning workers.
It is of interest that women were more exposed than men to asthmagenic agents and that the associations of asthmagenic agents with severe asthma were stronger in women than in men. Although the design of the PAARC Survey may explain part of the higher prevalence of exposure in women, it is well known that many occupations at risk such as healthcare workers, textile workers and cleaners are mainly female occupations (33).
In this study, asthma with ‘airflow limitation’ was used as a surrogate for severe asthma as it was not possible to study other dimensions of severity given the data available. The association between specific asthmagens and asthma severity has never been studied and the results here suggest that further analyses are needed to examine these associations. One can hypothesize that, if some asthmagens play a role in both exacerbation and development of asthma, associations will be seen between exposures and both asthma and adult asthma onset. In our analyses, for industrial cleaning agents, associations were significant for all asthma definitions, supporting the hypotheses that industrial cleaning agents may both induce new asthma and worsen existing asthma (33).
Finally, our finding that attributable risk estimates were lower using asthmagen exposure estimates than using exposure to dusts, gases, and fumes results is consistent with a recent report (5) in which risks varied from 5 to 13% for occupation or exposure known to cause occupational asthma and from 14 to 36% for more general exposure to dusts, gases, and fumes. Attributable risk can be calculated only on the hypothesis of causal association, which is probably not the case for dusts, gases, and fumes in general. Our results also emphasize the variability in attributable risk estimates and their dependence on the definitions of exposure and outcome used. The attributable risk estimates in this analysis of PAARC data are likely to be an underestimate of the true attributable risks, especially in men, as the population excluded manual worker heads of households.
In conclusion, our results suggest that assessment of associations between occupational exposures and asthma are improved with more precise estimates of relevant exposures and with clearer definitions of disease onset. Complete occupational and asthma histories, taking into account exposure windows according to asthma onset, are recommended. Our results also indicate that, in large population-based studies, useful information about work-relatedness of asthma can be obtained using coded job titles and an asthma JEM. An advantage of the use of job titles alone is that it allows the generation of hypothesis regarding unknown risks. Finally, to estimate attributable risk for occupational factors in asthma, accurate population-specific estimates of exposure to asthmagenic agents are needed.
Abbreviations
- CI
confidence interval
- OR
odds ratio
- JEM
Job Exposure Matrix
- PAARC
Pollution Atmosphérique et Affections Respiratoires Chroniques
- EGEA
Epidemiological study on the Genetics and Environment of Asthma
- ECRHS
European Community Respiratory Health Survey
- LMW
Low Molecular Weight
- HMW
High Molecular Weight
- FEV1
forced respiratory volume in one second
- FVC
forced vital capacity
- ISCO88
International Standard Classification of Occupations codes, 1988
References
- 1.Chan-Yeung M, Malo JL. Occupational asthma. N Engl J Med. 1995;333(2):107–12. doi: 10.1056/NEJM199507133330207. [DOI] [PubMed] [Google Scholar]
- 2.Venables KM, Chan-Yeung M. Occupational asthma. Lancet. 1997;349:1465–9. doi: 10.1016/S0140-6736(96)07219-4. [DOI] [PubMed] [Google Scholar]
- 3.Torén K, Brisman J, Olin AC, Blanc PD. Asthma on the job: work-related factors in new-onset asthma and in exacerbations of pre-existing asthma. Respir Med. 2000;94:529–535. doi: 10.1053/rmed.2000.0783. [DOI] [PubMed] [Google Scholar]
- 4.Blanc PD, Torén K. How much adult asthma can be attributed to occupational factors? Am J Med. 1999;107:580–7. doi: 10.1016/s0002-9343(99)00307-1. [DOI] [PubMed] [Google Scholar]
- 5.American Thoracic Society Statement: Occupational Contribution to the burden of Airway disease. Am J Respir Crit Care Med. 2003;167:787–97. doi: 10.1164/rccm.167.5.787. [DOI] [PubMed] [Google Scholar]
- 6.Airway allergy and worklife. Scand J Work Environ Health. 2001;27(6):422–5. [PubMed] [Google Scholar]
- 7.Liss GM, Tarlo SM. Work related asthma. Occup Environ Med. 2002;59:503–4. doi: 10.1136/oem.59.8.503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng TP, Hong CY, Goh LG, Wong ML, Koh KTC, Ling SL. Risks of asthma associated with occupations in a community-based case-control study. Am J Ind Med. 1994;25:709–18. doi: 10.1002/ajim.4700250510. [DOI] [PubMed] [Google Scholar]
- 9.Bakke P, Eide GE, Hanoa R, Gulsvik A. Occupational dust or gas exposure and prevalences of respiratory symptoms and asthma in a general population. Eur Respir J. 1991;4:273–8. [PubMed] [Google Scholar]
- 10.Arif AA, Whitehead LW, Delclos GL, Tortolero SR, Lee ES. Prevalence and risk factors of work related asthma by industry among United States workers: data from the third national health and nutrition examination survey (1988–94) Occup environ Med. 2002;59:505–11. doi: 10.1136/oem.59.8.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xu X, Christiani DC. Occupational exposures and physician-diagnosed asthma. Chest. 1993;104:1364–70. doi: 10.1378/chest.104.5.1364. [DOI] [PubMed] [Google Scholar]
- 12.Blanc PD. Occupational asthma in a national disability survey. Chest. 1987;92:613–17. doi: 10.1378/chest.92.4.613. [DOI] [PubMed] [Google Scholar]
- 13.Kogevinas M, Anto JM, Sunyer J, Tobias A, Kromhout H, Burney P the European Community Respiratory Health Survey Study Group. Occupational asthma in Europe and other industrialised areas: a population-based study. Lancet. 1999;353:1750–4. doi: 10.1016/s0140-6736(98)07397-8. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy SM, Le Moual N, Choudat D, Kauffmann F. Development of an asthma specific job exposure matrix and its application in the epidemiological study of genetics and environment in asthma (EGEA) Occup Environ Med. 2000;57:635–41. doi: 10.1136/oem.57.9.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zock JP, Cavallé N, Kromhout H, et al. Evaluation of specific occupational asthma risks in a community-based study with special reference to single and multiple exposure. J Expos Anal Environ Epid. doi: 10.1038/sj.jea.7500337. in press. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg M, Goldberg P. Measurement of occupational exposure and prevention: principal approaches to research. Prevention of respiratory diseases. In: Hirsch A, Goldberg M, Martin JP, Masse R, editors. Lung biology in health and disease. Vol. 68. New York: Marcel Dekker; 1993. pp. 167–92. [Google Scholar]
- 17.Krzyzanowski M, Kauffmann F. The relation of respiratory symptoms and ventilatory function to moderate occupational exposure in a general population. Int J Epidemiol. 1988;17:397–406. doi: 10.1093/ije/17.2.397. [DOI] [PubMed] [Google Scholar]
- 18.Hsairi M, Kauffmann F, Chavance M, Brochard P. Personal factors related to the perception of occupational exposure: an application of a job exposure matrix. Int J Epidemiol. 1992;21:972–80. doi: 10.1093/ije/21.5.972. [DOI] [PubMed] [Google Scholar]
- 19.Le Moual N, Bakke P, Orlowski E, et al. Performance of population specific job exposure matrices (JEMs): European collaborative analyses on occupational risk factors for chronic obstructive pulmonary disease with job exposure matrices (ECOJEM) Occup Environ Med. 2000;57:126–32. doi: 10.1136/oem.57.2.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Moual N, Bakke P, Kromhout H, et al. Relationship between occupational exposure, estimated by two job exposure matrices, and lung function in French, Dutch, and Norwegian community studies. Eur Respir Rev. 2001;11(80):91–7. [Google Scholar]
- 21.Le Moual N, Orlowski E, Schenker MB, Avignon M, Brochard P, Kauffmann F. Occupational exposures estimated by means of job exposure matrices in relation to lung function in the PAARC survey. Occup Environ Med. 1995;52:634–43. doi: 10.1136/oem.52.10.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Groupe Coopératif PAARC. Pollution atmosphérique et affections respiratoires chroniques ou à répétition. I Méthodes et sujets. Bull Europ Physiopathol Respir. 1982;18:87–99. [PubMed] [Google Scholar]
- 23.Quanjer PhH, Tammeling GJ. Summary of recommendations. In : Quanjer PhH. Standardized lung function testing. Bull Europ Physiopathol Respir. 1983;19(suppl 5):7–10. [Google Scholar]
- 24.Jaakkola JJ, Piipari Ritva, Jaakkola MS. Occupation and asthma: a population-based incident case-control study. Am J Epidemiol. 2003;158:981–7. doi: 10.1093/aje/kwg238. [DOI] [PubMed] [Google Scholar]
- 25.Kogevinas M, Anto JM, Soriano JB, Tobias A, Burney P the Spanish group of the European asthma Study. The risk of asthma attributable to occupational exposures. A population-based study in Spain. Am J Respir Crit Care Med. 1996;154:137–43. doi: 10.1164/ajrccm.154.1.8680669. [DOI] [PubMed] [Google Scholar]
- 26.Institut National de la Statistique et des Etudes Economiques. Code 2 du recensement de la population 1968. Code des métiers. Paris: Imprimerie Nationale; 1968. p. 319. [Google Scholar]
- 27.Internationnal Labour Office: International standard classification of occupations. Revised. Geneva: ILO; 1988. [Google Scholar]
- 28.Kauffmann F, Dizier MH, Annesi-Maesano I, et al. EGEA (Epidemiological study on the Genetics and Environment of Asthma, bronchial hyperresponsiveness and atopy) -descriptive characteristics. Clin exp allergy. 1999;29(suppl 4):17–21. [PubMed] [Google Scholar]
- 29.Preller L, Doekers G, Heederik Vermelen R, Vogelzang PFJ, Boleij JSM. Disinfectant use as a risk factor for atopic sensitization and symptoms consistent with asthma: an epidemiological study. Eur Respir J. 1996;9:1407–13. doi: 10.1183/09031936.96.09071407. [DOI] [PubMed] [Google Scholar]
- 30.de Marco R, Locatelli F, Cerveri F, et al. Incidence and remission of asthma: a retrospective study on the natural history of asthma in Italy. J Allergy Clin Immunol. 2002;110:228–35. doi: 10.1067/mai.2002.125600. [DOI] [PubMed] [Google Scholar]
- 31.Fritschi L, Siemiatycki J, Richardson L. Self-reported versus expert-assessed occupational exposures. Am J Epidemiol. 1996;144:521–7. doi: 10.1093/oxfordjournals.aje.a008959. [DOI] [PubMed] [Google Scholar]
- 32.Karjalainen A, Kurppa k, Martikainen R, Karjalainen J, Klaukka T. Exploration of asthma risk by occupation – extended analysis of an incidence study of the finnish population. Scan J Work Environ Health. 2002;28:49–57. doi: 10.5271/sjweh.646. [DOI] [PubMed] [Google Scholar]
- 33.Wai Y, Tarlo SM. Occupational lung disease in women. Eur Respir Mon. 2003;25:131–45. [Google Scholar]
- 34.Ameille J, Pauli G, Calastreng-Crinquand, et al. Reported incidence of occupational asthma in France, 1996–99: the ONAP programme. Occup Environ Med. 2003;60:136–41. doi: 10.1136/oem.60.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zock JP, Kogevinas M, Sunyer J, et al. Asthma risk, cleaning activities and use of specific cleaning products among Spanish indoor cleaners. Scan J Work Environ Health. 2001;27(1):76–81. doi: 10.5271/sjweh.590. [DOI] [PubMed] [Google Scholar]


