Abstract
Ebola virus (EBOV) causes outbreaks of a highly lethal hemorrhagic fever in humans. The virus can be transmitted by direct contact as well as by aerosol and is considered a potential bioweapon. Because direct immunization of the respiratory tract should be particularly effective against infection of mucosal surfaces, we previously developed an intranasal vaccine based on replication-competent human parainfluenza virus type 3 (HPIV3) expressing EBOV glycoprotein GP (HPIV3/EboGP) and showed that it is immunogenic and protective against a high dose parenteral EBOV challenge. However, because the adult human population has considerable immunity to HPIV3, which is a common human pathogen, replication and immunogenicity of the vaccine in this population might be greatly restricted. Indeed, in the present study, replication of the vaccine in the respiratory tract of HPIV3-immune guinea pigs was found to be restricted to undetectable levels. This restriction appeared to be based on both neutralizing antibodies and cellular or other components of the immunity to HPIV3. Surprisingly, even though replication of HPIV3/EboGP was highly restricted in HPIV3-immune animals, it induced a high level of EBOV-specific antibodies that nearly equaled that obtained in HPIV3-naïve animals. We also show that the previously demonstrated presence of functional GP in the vector particle was not associated with increased replication in the respiratory tract nor with spread beyond the respiratory tract of HPIV3-naive guinea pigs, indicating that expression and functional incorporation of the attachment/penetration glycoprotein of this systemic virus did not mediate a change in tissue tropism.
Keywords: Ebola, virus, vaccine, immunogenicity, respiratory, immunization, antibody
INTRODUCTION
Ebola virus (EBOV) causes sporadic outbreaks of severe hemorrhagic fever in the rain forests of Central Africa (Nkoghe et al., 2005) with a lethality in humans of up to 88% for species Zaire (Bulletin WHO, 1976; Nkoghe et al., 2005). The virus is transmitted by contact with infected patients or fluids and is thought to enter through breaks in the skin or inoculation of mucosal membranes (Geisbert and Jahrling, 2004; Jaax et al., 1995; Jaax et al., 1996). The virus also was demonstrated to infect non-human primates by laboratory generated aerosol (Johnson et al., 1995) and is considered a potential biological weapon (Salvaggio and Baddley, 2004). Development of a vaccine for EBOV is a priority. Two vectored vaccine candidates based on human adenovirus type 5 and vesicular stomatitis virus and a third candidate based on a virus-like particle, all delivered parenterally, were shown to be protective in non-human primates (Jones et al., 2005; Sullivan et al., 2000; Warfield et al., 2007). We are interested in the general issue of developing vectors for direct immunization of the respiratory tract, which frequently can be a portal of infection by highly pathogenic viruses. The induction of a local immune response in the respiratory tract would be advantageous for prevention of EBOV transmitted by contact with respiratory mucosa or by aerosol.
We previously developed an intranasal vaccine candidate against EBOV (HPIV3/EboGP) based on human parainfluenza virus type 3 (HPIV3) as a vector. HPIV3 is an enveloped RNA-containing virus of Family Paramyxoviridae that is a common cause of human pediatric disease (Karron and Collins, 2007). Its genome is a single negative-sense strand of RNA of 15,462 nt that encodes six essential viral proteins, namely the major nucleocapsid protein N, nucleocapsid phosphoprotein P, matrix protein M, fusion glycoprotein F, hemagglutinin-neuraminidase glycoprotein HN, and large polymerase protein L. HPIV3 also encodes accessory C and D proteins from overlapping open reading frames in the P gene, and there is genetic evidence for expression of a third protein, V. HPIV3 replicates primarily in the superficial cells of the lumen of the respiratory tract and remains largely restricted to that site (Zhang et al., 2005). Using reverse genetics, one or more open reading frames encoding foreign proteins can readily be placed under the control of independent sets of HPIV3 gene-start and gene-end transcription signals and inserted into the HPIV3 gene order (Skiadopoulos et al., 2002). Infection with HPIV3 induces both systemic and local respiratory tract immune responses to itself and, when used as a vector, to expressed foreign glycoproteins. Direct inoculation of HPIV3/EboGP into the respiratory tract of HPIV3-seronegative guinea pigs (Bukreyev et al., 2006b) and African green monkeys (Bukreyev et al., 2007) resulted in effective induction of EBOV-specific serum antibodies and protection against intraperitoneal challenge with a high dose of EBOV.
We previously noted that the foreign EBOV GP glycoprotein was incorporated into the HPIV3/EboGP vector particle (Bukreyev et al., 2006b). Furthermore, it appeared to be functional based on the observation that the vector partially lost its sensitivity to neutralization by HPIV3-specific antibodies and acquired substantial sensitivity to neutralization by anti-EBOV antibodies (Bukreyev et al., 2006b). In animals and humans, EBOV typically establishes a systemic infection resulting in high EBOV titers in internal organs and blood whereas, in contrast, HPIV3 is pneumotropic. Since EBOV GP functions in both attachment and penetration, its incorporation into the HPIV3 vector particle had the potential to result in an altered tissue tropism with possible increased replication of the vector in the respiratory tract or spread of the vector to various tissues beyond the respiratory tract. In the present study, we evaluated these possibilities in guinea pigs, an experimental animal that is permissive to both HPIV3 and guinea pig-adapted EBOV (Bukreyev et al., 2006b).
In addition, we investigated a potential complication of the use of HPIV3 as a vector. Because HPIV3 is a common human pathogen, most of the adult human population has substantial immunity due to prior natural exposure. This prior immunity would be expected to restrict replication of HPIV3/EboGP, although this effect might be offset by the presence of functional GP for which the human population is naïve. Reduction in vector replication could greatly reduce the immunogenicity of the expressed foreign antigen. This problem would not unique for an HPIV3-based vector, since several current human vaccine candidates are based on viral vectors that are common human pathogens (reviewed in Bukreyev et al., 2006a). For example, comparison of immunogenicity of several vaccinia virus-vectored and human adenovirus type 5-vectored vaccines in pre-clinical trials with rodents and non-human primates and in clinical studies demonstrated that preexisting immunity to the vector can reduce or completely abolish immunogenicity of these vaccines (Barouch et al., 2004; Casimiro et al., 2003; Fitzgerald et al., 2003; Kanesa-thasan et al., 2000; Lemckert et al., 2005; Sharpe et al., 2001; Sumida et al., 2004; Zhi et al., 2006). In particular, induction of EBOV-specific cellular and humoral responses by a recombinant adenovirus type 5 expressing EBOV GP in mice was reduced due to prior exposure to adenoviral vector (Yang et al., 2003). In the present study, we evaluated replication and immunogenicity of HPIV3/EboGP in guinea pigs that had recently been infected with HPIV3. We show here that, despite restriction of replication of the vaccine by pre-existing HPIV3-specific immunity, the expressed EBOV GP remained highly immunogenic.
RESULTS
Expression and packaging of EBOV GP does not change the tropism of the HPIV3 vector
We previously showed that expression of the EBOV GP glycoprotein by HPIV3/EboGP resulted in the functional incorporation of EBOV GP into the vector particle (Bukreyev et al., 2006b). This had the potential of altering the tissue tropism of HPIV3 to confer increased pulmonary replication or spread of the virus beyond the respiratory tract. We evaluated these possibilities in guinea pigs, an experimental animal that supports moderate levels of pulmonary HPIV3 replication, is very permissive to systemic replication and is readily killed by a low dose (< 1 PFU) of guinea pig-adapted EBOV (Bukreyev et al., 2006b). Since adaptation of EBOV to guinea pigs does not require mutations in the GP (Volchkov et al., 2000), guinea pig model should be a sensitive indicator of EBOV GP-mediated pathogenic effects.
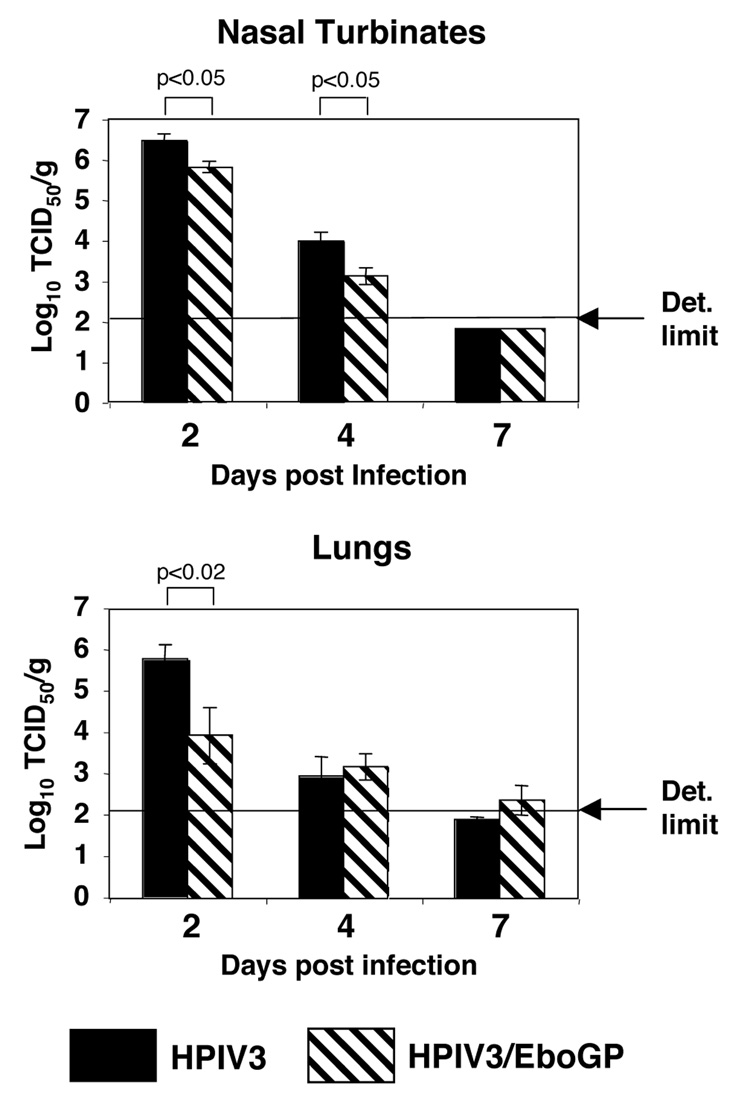
To test the possibility of enhanced pulmonary replication, HPIV3-seronegative guinea pigs were mock-infected or infected by the intranasal (IN) route with 4×105 50%-tissue-culture-infectious-doses (TCID50) of HPIV3 or HPIV3/EboGP. On days 2, 4, and 7 after inoculation, the animals were sacrificed, nasal turbinates and lungs were isolated, and the titers of HPIV3 or HPIV3/EboGP in the tissue extracts were determined by TCID50 titration on LLC-MK2 cell monolayers (Fig. 1). The data showed that HPIV3 efficiently replicated in both the upper and the lower respiratory tract with the highest virus titer detected on day 2, a somewhat lower titer on day 4, and little or no detectable virus on day 7. Compared to HPIV3, the HPIV3/EboGP virus replicated at similar or slightly reduced levels, depending on the location and time point (Fig. 1).
Fig. 1.
Replication of HPIV3 and HPIV3/EboGP in nasal turbinates (top panel) and lungs (bottom panel) of HPIV3-naive guinea pigs. Animals were infected by the intranasal (IN) route with 4×105 TCID50 of HPIV3 or HPIV3/EboGP. Animals were sacrificed on days 2 (five animals per group), 4 (six animals per group), and 7 (five animals per group) after inoculation, and nasal turbinates and lungs were isolated and virus titers were determined. Mean values are shown ± SE with the P values indicated at the top. The limits of detection are shown by the arrows: 2.11 and 2.15 log10 TCID50/ml for nasal turbinates and lungs, respectively. When virus was not detected in an individual animal, a value of one-half the limit of detection was assigned for the purpose of calculation.
We also evaluated the presence of viral antigen in the lower respiratory tract by immunohistochemistry. HPIV3-seronegative guinea pigs were infected with HPIV3 or HPIV3/EboGP as above, sacrificed on day 2, and the lungs were harvested and stained for HPIV3 antigen with polyvalent anti-HPIV3 antibodies raised against sucrose gradient-purified HPIV3 (Fig. 2). For both HPIV3- and HPIV3/EboGP-infected animals, viral antigen (stained brown) was detected in bronchi and bronchioles extending into inflammatory alveolar lesions. For both viruses, a moderate amount of antigen was detected in the bronchi (Fig. 2, A and B), less was detected in smaller airways (C and D), and even less in the alveoli (E and F). Generally, less antigen was detected in HPIV3/EboGP-infected animals compared to that in the HPIV3 control animals. Thus, there was evidence of attenuation rather than increased spread associated with expression of EBOV GP.
Fig. 2.
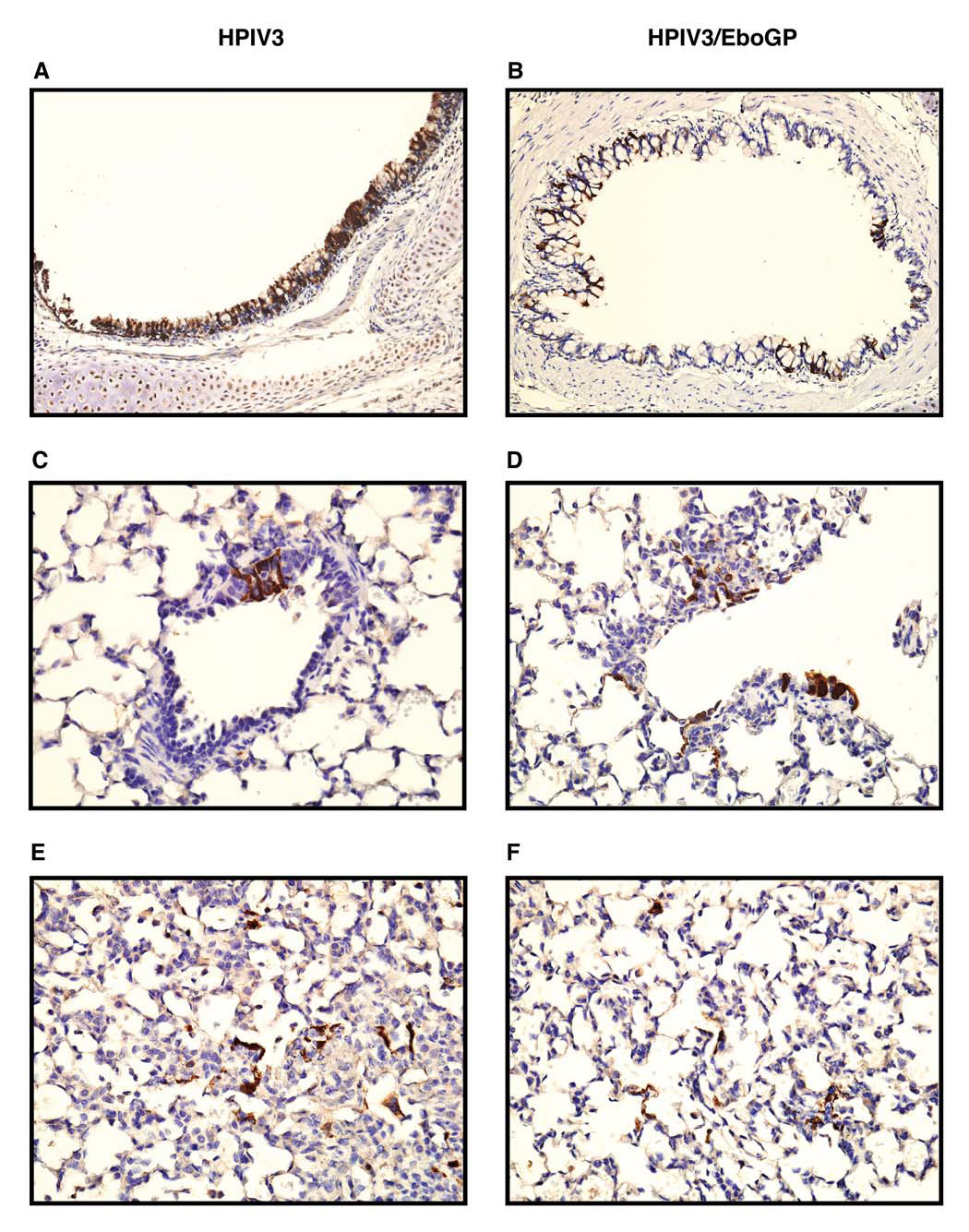
Immunohistochemical analysis of HPIV3 antigen distribution (brown) in the respiratory tract of guinea pigs infected with HPIV3 (panels A, C, E) or HPIV3/EboGP (panels B, D, F), with hematoxylin counterstain (blue). A, B. Diffuse (HPIV3) and focal (HPIV3/EboGP) infection of bronchial epithelial cells, 200X. C, D. Infection in bronchioles, 400X. E, F. Infection in alveolar interstitial lesions, 400X. No antigen was detected in the lung tissues of mock-infected animals (not shown).
Next, we tested the possibility that HPIV3/EboGP might spread to tissues beyond the respiratory tract. Groups of seronegative guinea pigs were inoculated with HPIV3 or HPIV3/EboGP. Two and four days after inoculation, the animals were sacrificed and samples of the peripheral blood, liver, kidney and spleen were collected. The peripheral blood samples and the tissue extracts were tested for presence of infectious virus by the limiting dilution assay as described above. Virus was not detected in any of the samples (not shown). Taken together, these data indicate that the presence of EBOV GP in the vector particles did not confer enhanced replication or promote spread of the HPIV3 vector beyond the respiratory tract.
Pre-existing immunity to HPIV3 restricts the replication of HPIV3/EboGP
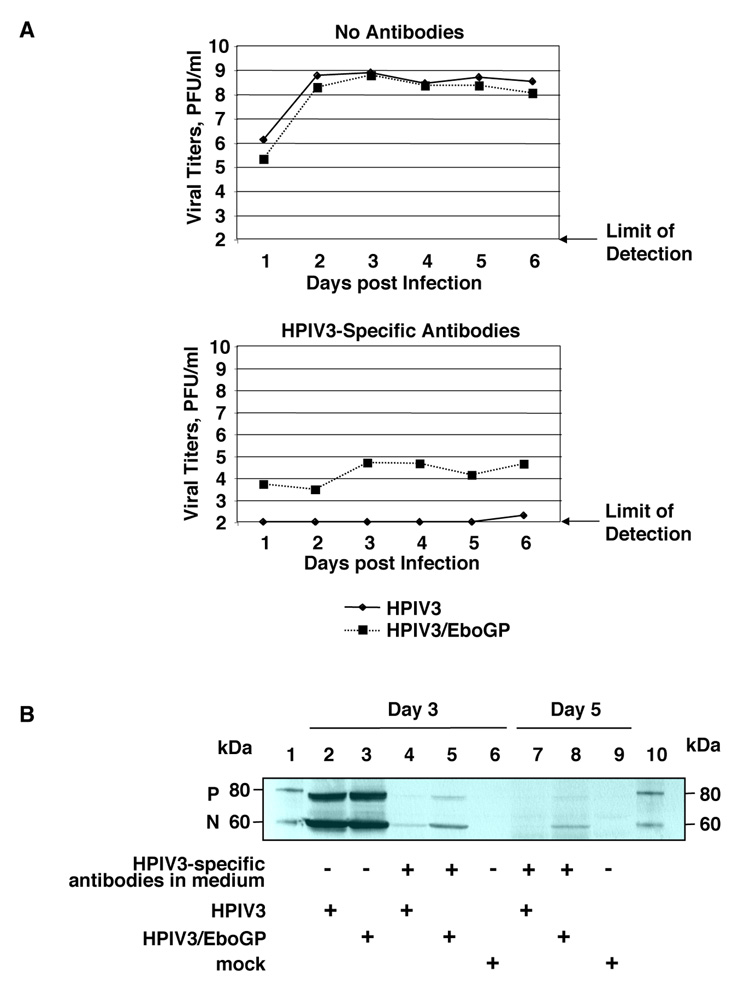
Since incorporation of the EBOV GP protein into the recombinant HPIV3 vector was previously observed to reduce its sensitivity to neutralization by HPIV3-specific antibodies in vitro (Bukreyev et al., 2006b), it was possible that this would enhance its ability to replicate in vitro and in vivo in presence of the HPIV3-specific immunity. This was evaluated in vitro by infecting replicate cultures of A549 cells with HPIV3 or HPIV3/EboGP at a multiplicity of infection (MOI) of 0.001 PFU/cell and, after an 80 min adsorption period, incubating the cultures with medium containing a 1:100 dilution of polyvalent HPIV3-specific antiserum. The cultures were incubated at 32°C and aliquots of the overlying medium were collected daily for virus titration by plaque assay. In cultures where the antiserum had not been added, each virus replicated efficiently (Fig. 3A, top). In cultures incubated in the presence of antiserum, HPIV3 was not detected on days 1 – 5, and only a very low, barely detectable titer was detected on day 6. In contrast, HPIV3/EboGP was recovered in the presence of anti-HPIV3 antibodies with titers ranging from 3.5 to 4.7 log10 PFU/ml (Fig. 3A, bottom), although these titers were much lower than that in the cells containing no antibodies (Fig. 3A, top). To confirm that this represented increased infection of the cell monolayers, cells were harvested on days 3 and 5 and were subjected to Western blot analysis with HPIV3-specific antiserum. This showed that, in the absence of HPIV3-specific antiserum in the medium, there was an abundant level of cell-associated HPIV3 proteins in cultures infected with either HPIV3 or HPIV3/EboGP, as expected (Fig. 3B, lanes 2 and 3). With the inclusion of HPIV3-specific antiserum, the level of intracellular HPIV3 protein was dramatically reduced for both HPIV3 and HPIV3/EboGP, an effect that was greater for HPIV3 than HPIV3/EboGP (Fig. 6, lane 4 versus 5 and 7 versus 8). Thus, while HPIV3/EboGP was somewhat resistant to neutralization by HPIV3-specific antiserum, multi-cycle infection by either virus was strongly inhibited by HPIV3-specific antibodies.
Fig. 3.
Replication of HPIV3 and HPIV3/EboGP in A549 cells in the presence of antibodies specific to HPIV3. Cell monolayers were infected at an input MOI of 0.001 PFU/cell and the subsequent incubation was performed in the presence or absence of neutralizing polyvalent HPIV3-specific antibodies. A. Analysis of infectious virus production. Aliquots of medium were collected daily and viral titers were determined by plaque titration. B. Analysis of intracellular viral proteins as an indication of virus replication. Cells were collected on days 3 and 5 post infection and total protein was subjected to Western blot analysis with polyvalent HPIV3-specific antiserum. Equal amounts of cells lysates were loaded on the gel. On day 5, the infected monolayers with no antibodies were completely destroyed by the viruses and therefore were not analyzed. Two bands corresponding to HPIV3 proteins P and N are shown. Lanes: 1, 10, Magic Mark XP protein markers with bands corresponding to 80 kDa and 60 kDa; 2, 4, 7, HPIV3-infected cells; 3, 5, 8, HPIV3/EboGP-infected cells; 6, 9, mock-infected cells. The HPIV3-specific neutralizing antibodies were present in the medium of cells analyzed in lanes 4, 5, 7, 8.
Fig. 6.
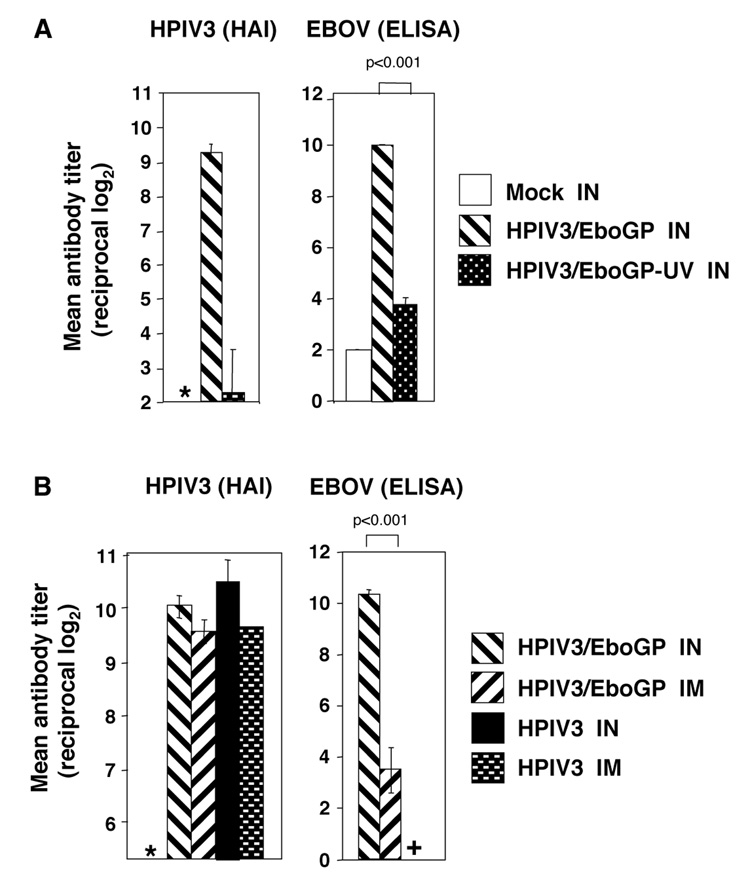
Effect of replication and route of immunization on the immunogenicity of HPIV3/EboGP. A. Effect of replication. Guinea pigs (four animals per group) were infected IN with HPIV3/EboGP at a dose of 4×106 TCID50 or with an equivalent amount of UV-inactivated virus. Sera were collected 29 days post-infection and the titers of HPIV3- and EBOV-specific serum antibodies were determined by HAI and ELISA respectively. Serum antibody titers are expressed as reciprocal log2 of endpoint dilutions and shown as mean titers ± SE with the P values indicated at the top. In sera of mock-infected animals (representing 5 animals from a separate experiment), the level of HPIV3-specific antibodies was below the detection level (2 log2), and is indicated with an asterisk. In the HPIV3/EboGP-UV group, the level of HPIV3-specific antibodies in three out of four animals was below the detection level, and the value of 2 log2 was assigned for calculation purposes. The detection limit of the HAI assay is 2.0 log2. B. Effect of the IN versus IM route of immunization. Guinea pigs were immunized with 4×106 TCID50 of HPIV3/EboGP by the IN or IM route (six animals per group), or 4×106 TCID50 of HPIV3 by the IM route (three animals). Sera were collected on day 30 after immunization and the titers of HPIV3- and EBOV-specific serum antibodies were determined as above. In addition, sera from nine animals collected on day 28 after IN infection with 4×106 TCID50 of HPIV3 from a previous experiment (Fig. 5) were analyzed in parallel for comparison. In an uninfected group (which consisted of two animals from a separate experiment), the level of HPIV3-specific antibodies was below the detection level, and is shown with an asterisk. In the HPIV3-immunized group, the level of EBOV-specific antibodies was below the detection level and is shown with a plus. The detection limit of the HAI assay was 5.32 log2.
Next, we tested the ability of the vaccine construct to replicate in animals immune to the HPIV3 vector. Guinea pigs were mock-infected or infected by the IN route with 4×105 TCID50 of HPIV3, and serum samples were collected 36 days later. As expected, all of the animals that received HPIV3 developed strong HPIV3-specific antibody responses as measured by an HPIV3-specific hemagglutination-inhibition (HAI) assay (van Wyke Coelingh, Winter, and Murphy, 1985), and all mock-infected animals remained HPIV3-seronegative (average reciprocal titers of 9.9±0.1 log2 and <2 log2, respectively). On day 40 after the primary infection, the animals were infected by the IN route with 4×106 TCID50 of HPIV3 or HPIV3/EboGP. On days 2, 4, and 7 after the second infection, animals were sacrificed, nasal turbinates and lungs were isolated, and the titers of HPIV3 or HPIV3/EboGP in the tissue extracts were determined as described above. Virus was not detected on any tested day for any virus in either the nasal turbinates or the lungs (data not shown), indicating that replication was strongly restricted in HPIV3-immune animals.
Restriction of HPIV3/EboGP replication in vivo is mediated by neutralizing antibodies and cellular or other components of the immune response
Next, we evaluated whether the restriction of HPIV3/EboGP replication in HPIV3-immune animals was mediated by the humoral or cellular component of the immune response, and whether there was a difference between HPIV3 and HPIV3/EboGP. This was done by measuring the restriction conferred by prior infection with HPIV3-1, a chimeric HPIV3 virus in which the two surface glycoproteins, HN and F, were replaced with their counterparts from serologically unrelated HPIV1, and which replicates in vitro and in vivo as efficiently as wild type HPIV1 and HPIV3 (Tao et al., 1998). The HN and F proteins are the only HPIV antigens that induce neutralizing antibodies (Karron and Collins, 2007), and there is no cross-protection in vivo between HPIV3 and HPIV1 (Tao et al., 2000); thus, any HPIV3-specific immunity induced by HPIV3-1 would involve only the internal virion proteins, would not involve neutralizing antibodies, and presumably would primarily involve cellular immunity (Tao et al., 1998). As a caveat, we cannot exclude the possibility that the internal proteins of HPIV3 might induce antibodies that do not neutralize the virus in vitro but might restrict replication in vivo; such antibodies have been described for several viruses, including rotavirus (Burns et al., 1996; Feng et al., 2002) and Sindbis virus (Mendoza, Stanley, and Griffin, 1988), although not for HPIV3 thus far.
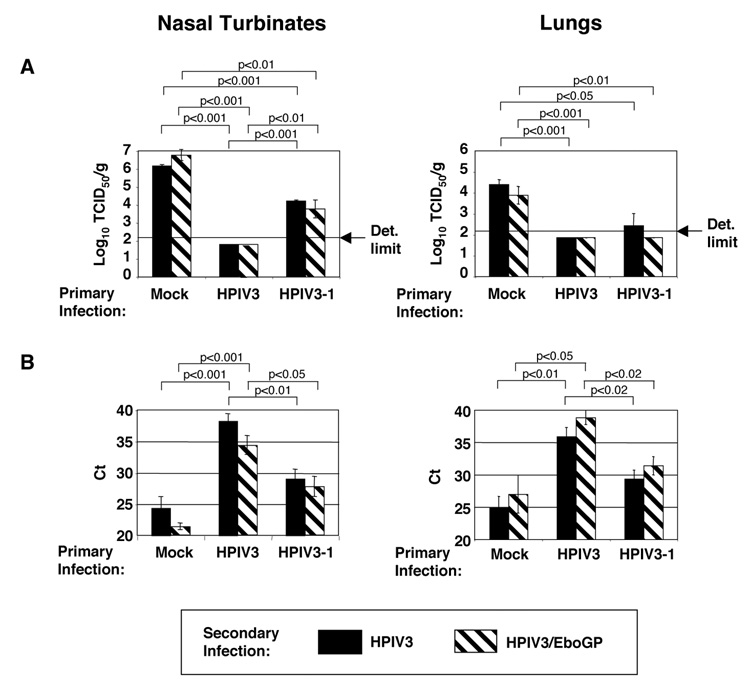
Guinea pigs were infected by the IN route with 4×105 TCID50 of HPIV3 or HPIV3-1, or were mock-infected, and serum samples were collected on day 27 and assayed for HPIV3-specific HAI antibodies. Infection with HPIV3 resulted in a reciprocal antibody titer of 11.7±0.4 log2, whereas there was no detectable HPIV3-specific response in HPIV3-1-infected or mock-infected animals (reciprocal titer <2 log2). We also analyzed these sera for the ability to neutralize HPIV3 and HPIV3/EboGP using an in vitro plaque reduction assay. This showed that sera from animals infected with HPIV3 completely neutralized HPIV3 and incompletely neutralized HPIV3/EboGP, as previously described (Introduction, and Bukreyev et al., 2006b), whereas neither virus was neutralized with the sera from HPIV3-1-immunized or mock-immunized animals (data not shown). Thus, the expected specificities were confirmed. Forty-two days after the primary infection, we challenged the animals by the IN route with 4×106 TCID50 of HPIV3 or HPIV3/EboGP. Two days after the second infection (which is the peak of viral replication in a primary infection, as shown in Fig. 1), the animals were sacrificed, and nasal turbinates and lungs were analyzed for presence of virus. Similar to the previous experiment, animals that had been mock-infected and challenged had equally high titers of HPIV3 and HPIV3/EboGP in both the lungs and nasal turbinates (Fig. 4A). In animals that had been immunized with HPIV3 and challenged, neither challenge virus was detected in either location (Fig. 4A). In contrast, in animals that had been immunized with HPIV3-1 and challenged, the HPIV3 and HPIV3/EboGP challenge viruses replicated in the nasal turbinates to levels that were approximately equivalent and were significantly reduced compared to that in animals that were initially mock-infected. In the lungs of HPIV3-1 immune animals, there was no detectable HPIV3/EboGP and only a low level of HPIV3 challenge virus (Fig. 4A).
Fig. 4.
Replication of HPIV3 and HPIV3/EboGP in the nasal turbinates (left panels) and lungs (right panels) of guinea pigs that had previously been mock-infected or infected with HPIV3 or HPIV3-1, as indicated. The initial infection with HPIV3 or HPIV3-1 was at a dose of 4×105 TCID50. The second infection with HPIV3 or HPIV3/EboGP was 42 days later at a dose of 4×106 TCID50. The animals (four per virus per day) were sacrificed 2 days later and nasal turbinates and lungs were isolated and used (A) for virus titration and (B) for isolation of total RNA and comparison of viral RNA concentrations by quantitative RT-PCR. In part A, the limits of detection (same as in Fig. 1) are indicated with arrows. The values represent (A) mean viral titers or (B) mean threshold concentration (Ct) ± SE with the P values indicated at the top. For quantitative RT-PCR of HPIV3/EboGP RNA in lungs of HPIV3-immune animals, three rather then four animals were analyzed.
In order to confirm that the reduction of the HPIV3/EboGP titers in HPIV3- or HPIV3-1-immune animals was an authentic in vivo effect and not the result of neutralization in vitro by HPIV-specific antibodies following harvest and tissue homogenization, we performed HPIV3 N and HN gene-specific quantitative reverse transcription (RT)-PCR assays using RNA extracted from the nasal turbinates and lung tissue samples. In this assay, the threshold cycle (Ct) is the number of cycles required for amplification of a sample into a detectable signal, and thus would be low for samples with high viral titers as determined by TCID50 assay and would be high for low-titer samples. The results of the N gene-specific assay are shown in Fig. 4B. Similar to the virus titration results (Fig. 4A), there was no significant difference in Ct between the two challenge viruses (HPIV3 and HPIV3/EboGP) in either of the immunization groups (HPIV3 and HPIV3-1) and at either anatomical location. In addition, the Ct values of the HPIV3-immunized groups were significantly higher than those of the mock groups, and the Ct values of the HPIV3-1 groups were significantly lower than those of the HPIV3 groups, and greater (although not significantly so) than the mock groups. Similar data were obtained with the HN gene-specific assay (not shown). Thus, on the basis of virus titration, HPIV3-1 was less protective than HPIV3 against HPIV3 and HPIV3/EboGP replication in the nasal turbinates, whereas there was no difference in the lungs (Fig. 4A), and on the basis of quantitative RT-PCR HPIV3-1 was less protective than HPIV3 at both locations.
The substantial but incomplete protection provided by HPIV3-1 compared to HPIV3 indicated that both the surface and the internal proteins of HPIV3 make contributions to restricting both HPIV3 and HPIV3/EboGP. With regard to the internal proteins, while we cannot exclude a possible contribution by antibodies not detectable by an in vitro neutralization assay, it seems likely that cellular immunity made the major contribution to this effect. In addition, the finding that HPIV3/EboGP was at least as restricted as HPIV3 by prior immunity to HPIV3-1 is a further indication that expression and incorporation of the foreign GP did not confer increased replication or substantial escape from HPIV3-specific immunity, in this case mediated by factors other than neutralizing antibodies.
Despite the lack of detectable replication, HPIV3/EboGP is highly immunogenic in HPIV3-immune animals
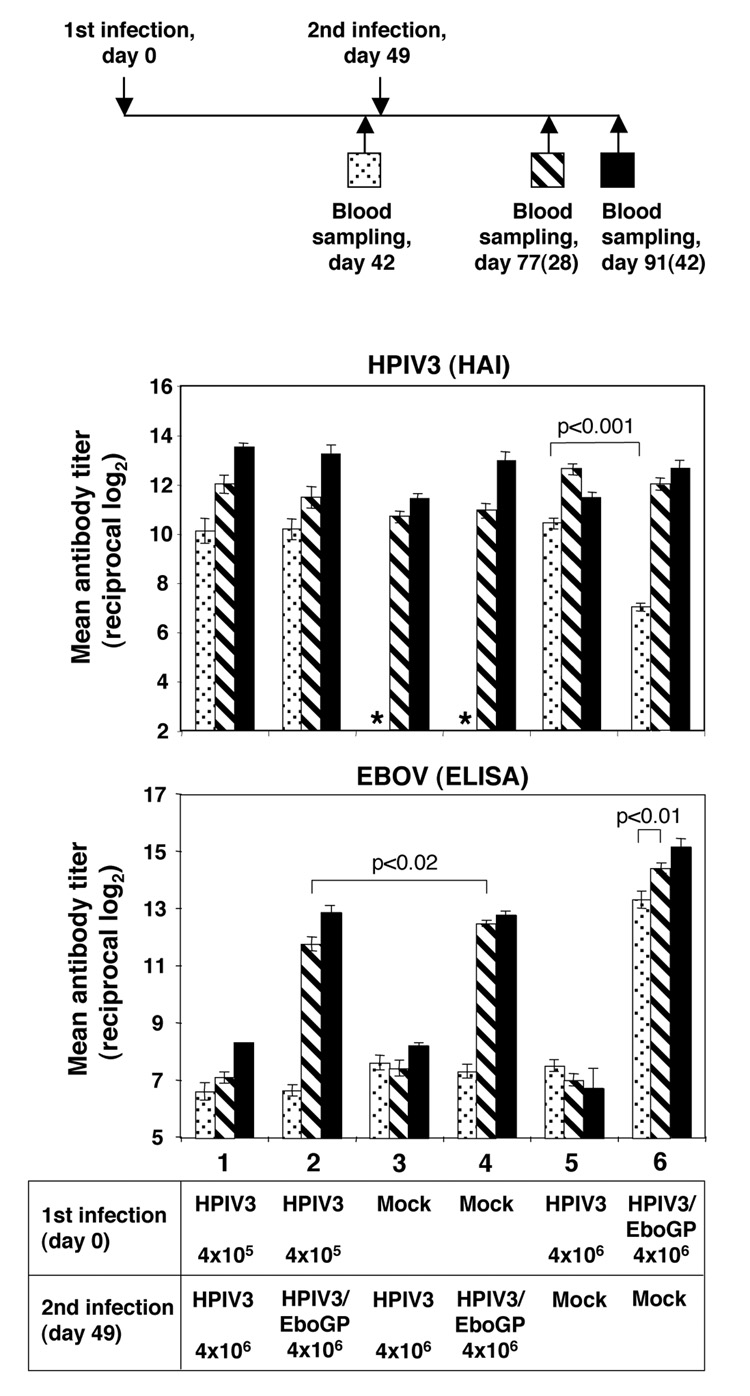
As noted in the Introduction, there are several instances of experimental vectored vaccines in which pre-existing immunity to the vector reduced or blocked the immune response to the expressed foreign antigen. Therefore, we compared the ability of HPIV3/EboGP to induce a serum antibody response to EBOV GP in guinea pigs that either possessed or lacked prior immunity to HPIV3. Following the experimental scheme in Fig. 5 (top panel), guinea pigs were infected by the IN route with 4×105 or 4×106 TCID50 of HPIV3, 4×106 TCID50 of HPIV3/EboGP, or were mock-infected, and serum samples were collected on day 42 after infection. Forty-nine days after the first infection, animals received a second infection by the IN route with 4×106 TCID50 of HPIV3, HPIV3/EboGP, or were mock-infected. Serum samples were collected 28 and 42 days after the second infection. All serum samples were analyzed for HPIV3-specific antibodies by HAI (Fig. 5, middle panel) and for EBOV-specific antibodies by enzyme-linked immunoadsorbent assay (ELISA) against inactivated, disrupted EBOV (bottom panel).
Fig. 5.
Immunogenicity of HPIV3/EboGP in guinea pigs that had previously been infected with HPIV3 or HPIV3/EboGP. Top panel: map of the experiment. The numbers in parentheses refer to the days after the second infection, and the symbols (dotted, cross-hatched, black) match those in the graphs below. Antibody responses: the anti-HPIV3 titers determined by HAI (middle panel) and the anti-EBOV titers determined by ELISA (bottom panel) from sera collected on day 42 following the first infection (dotted bars), and days 28 (cross hatched) and 42 (black) following the second infection. The antibody titers are expressed as reciprocal log2 of endpoint dilutions and shown as mean titers ± SE with the P values indicated at the top. Indicated at the bottom are: the group numbers (1 to 6) and the virus and dose used for the first and the second infections. Groups 1, 3 and 5 contained 10 animals each, and groups 2, 4 and 6 included 12 animals each. On day 42, the HPIV3-specific antibody titers in groups 3 and 4 were below the detection limit of the HAI assay (which is 2 log2), and are indicated with asterisks.
As expected, following the primary infection with HPIV3 (Fig. 5, middle panel, groups 1, 2, and 5) or HPIV3/EboGP (group 6), all of the animals developed an HPIV3-specific serum antibody response. In animals infected with HPIV3, the reciprocal titer of antibodies reached 10.1±0.4 log2 after infection with 4×105 TCID50 (groups 1 and 2) and 10.4±0.2 log2 after infection with 4×106 TCID50 (group 5). In comparison, infection with 4×106 TCID50 of HPIV3/EboGP (group 6) induced a lower HPIV3-specific antibody titer of 7.0±0.2 log2 (p<0.001). This might reflect the somewhat reduced replication of HPIV3/EboGP compared to HPIV3, as was observed in Fig. 1, as well as a possible reduction of the density of the HN protein on the surface of the viral particles due to incorporation of the GP protein (Bukreyev et al., 2006b). In any event, this difference largely disappeared with time, such that the titer of HPIV3-specific antibodies in the group that received a single dose of HPIV3/EboGP (group 6) was nearly the same at 77 or 91 days following the day 0 infection as in animals that received a single dose of HPIV3 (group 5).
Similar to the previous experiments, animals that were mock-infected and subsequently infected with HPIV3/EboGP (Fig. 5, bottom panel, group 4) developed high titers of serum antibodies specific for EBOV that, based on previous work, would be associated with complete protection against challenge with a highly lethal dose of EBOV (Bukreyev et al., 2006b). Surprisingly, a strong serum antibody response to EBOV was achieved even in animals that were previously infected with HPIV3 (group 2): the EBOV-specific antibody titer achieved in HPIV3-immune animals (group 2) was only slightly less than that achieved in non-HPIV3-immune animals (group 4) on day 28 following the second infection, and was essentially equivalent on day 42. These data indicate that, despite the restriction of HPIV3/EboGP replication in HPIV3-immune animals, the vaccine construct was highly immunogenic. In addition, we also observed a significant increase over time in the titer of EBOV-specific antibodies in animals that received a single dose of HPIV3/EboGP on day 0 (group 6): specifically, on days 77 and 91, the titers were increased 2.1-fold and 3.5-fold, respectively, compared to day 42. Thus, the response increased rather than decreased with time during this three-month interval.
Immunogenicity of HIV3/EboGP depends on its replication
Since EBOV GP is incorporated into the HPIV3/EboGP particle, it was possible that the GP-specific immune response induced by HPIV3/EboGP in HPIV3-immune animals was due to preformed GP contained in the inoculum. Thus, we investigated whether the immune response to EBOV GP depended on the replication of HPIV3/EboGP. We immunized four guinea pigs by the IN route with 4×106 TCID50 of HPIV3/EboGP and another four animals with UV-inactivated HPIV3/EboGP. The UV dose had been pre-calibrated to be the minimum necessary to inactivate infectivity, which was done to minimize the possibility that loss of immunogenicity might result from damage to viral protein. Twenty-nine days after inoculation, serum samples were collected and analyzed for the presence of serum antibodies specific to HPIV3 or EBOV as above. As in the previous experiments, all of the animals immunized with infectious HPIV3/EboGP developed high titers of serum antibodies specific for both HPIV3 and EBOV (Fig. 6A). In contrast, three of the four animals immunized with UV-inactivated HPIV3/EboGP remained HPIV3 seronegative while the remaining animal had a low level HPIV3-specific antibodies (titer 1:64). With regard to the EBOV-specific response, animals immunized with UV-HPIV3/EboGP had only very low levels of antibodies to EBOV.
The poor immunogenicity of UV-HPIV3/EboGP in HPIV3-naïve animals (Fig. 6A) suggested that the strong EBOV-specific responses to HPIV3/EboGP in HPIV3-immune animals (Fig. 5) depended on HPIV3/EboGP replication even though infectious progeny virus was not detected in the nasal turbinates and lung tissues (Fig. 4A). However, it also was conceivable that, in the HPIV3-immune animals, an antibody-mediated enhancement occurred independent of replication, such as through capture of antibody-virus complexes by dendritic cells and macrophages. To investigate this, we infected or mock-infected groups of guinea pigs by the IN route with 4×105 TCID50 of HPIV3. Forty-two days later, the animals were immunized by the IN route with 4×106 TCID50 of HPIV3/EboGP or with an equivalent amount of UV-HPIV3/EboGP. In both HPIV3-immune and non-immune animals, HPIV3/EboGP induced strong EBOV-specific antibody responses, as already seen, whereas the response to UV-HPIV3/EboGP was marginal (like that in Fig. 6A) and was not different between the immune and non-immune animals. These data suggest that pre-existing HPIV3-specific antibodies did not enhance the immunogenicity of UV-HPIV3/EboGP.
Immunogenicity of HIV3/EboGP depends on inoculation through the respiratory tract
As already noted, whereas HPIV3 infects the superficial cells of the respiratory tract and typically does not spread significantly beyond that site, EBOV causes a systemic infection. Although there was no detectable spread of viable HPIV3/EboGP to the blood, spleen, liver and kidneys following IN inoculation, it also was important to evaluate whether systemic infection might occur following inoculation by a parenteral route. To test this possibility, we infected six guinea pigs with HPIV3/EboGP by the IN route, six animals with HPIV3/EboGP by the IM route, and three animals with HPIV3 by IM route, using a dose of 4×106 TCID50 in each instance. Thirty days after immunization, serum samples were collected and analyzed for presence of antibodies specific for HPIV3 and EBOV as above. For comparison, sera from animals that had been infected IN with the same dose of HPIV3 in a previous experiment were examined in parallel.
The HPIV3-specific responses to IM infection with either virus were readily detectable and were only marginally reduced compared to IN infection (Fig. 6B, left panel). This was not surprising, since IM inoculation with respiratory syncytial virus had previously been shown to induce a titer of neutralizing serum antibodies that was one-third that of the high titer induced by IN infection, apparently reflecting an abortive replicative cycle at the site of IM injection (Prince et al., 1979). In contrast, IM infection with HPIV3/EboGP resulted in only a low level of EBOV-specific serum antibodies, with the average magnitude of 3.5±0.9 log2, that was 114-fold lower than that in the control animals immunized through the IN route in the same experiment (Fig. 6B, right panel). The reduced immunogenicity of HPIV3/EboGP given parenterally was interpreted as an indication that the virus did not efficiently infect cells or did not efficiently replicate following parenteral administration. The substantial response specific to HPIV3 HN detected by the HAI assay may reflect an unusually high immunogenicity of this protein. The lack of significant EBOV-specific response following the IM infection supports the idea that HPIV3/EboGP had a reduced rather than increased capability to replicate systemically, and also is consistent with the idea that the amount of protein contained in the inoculum is insufficient to be significantly immunogenic on its own in naive animals.
DISCUSSION
In this study, we evaluated the safety, replication, and immunogenicity of an intranasal HPIV3-vectored vaccine against EBOV in guinea pigs in the presence or absence of prior immunity to the HPIV3 vector. When HPIV3/EboGP was administered IN to non-immune animals, high levels of virus replication occurred and resulted in robust serum antibody responses to both the vector and the insert. The animals were not challenged with EBOV in this particular study, since we previously demonstrated that these levels of EBOV-specific antibodies are associated with a uniform protection against a highly lethal dose of EBOV (Bukreyev et al., 2006b). In the present study, we also showed that pulmonary replication of HPIV3/EboGP was slightly reduced compared to its HPIV3 parent, and that infectious virus could not be detected in the peripheral blood or in the liver, kidney, and spleen. In addition, parenteral inoculation with HPIV3/EboGP did not induce significant levels of serum antibodies to EBOV. Thus, even though EBOV GP was incorporated into the vector particle and conferred resistance to HPIV3-specific antibodies and sensitivity to EBOV-specific antibodies (evidence that it was functional in initiating infection), this did not result in increased pulmonary replication nor did it confer the ability to spread to and replicate detectably in peripheral tissues. This is noteworthy since EBOV GP mediates both viral attachment and entry, and thus would have the potential to alter tropism on its own. Guinea pigs are highly permissive to replication of guinea pig-adapted EBOV (which, as noted above, not require mutations in GP) and are very sensitive to virus-induced disease and death, and thus provided a sensitive test for increased pathogenicity due to EBOV GP. These findings form a precedent that is of general usefulness and relevance with regard to the issue of the biological safety of recombinant vectors the express foreign surface proteins and incorporate these proteins in the vector particle.
When HPIV3/EboGP was administered IN to HPIV3-immune animals, infectious virus could not be detected in nasal turbinate and lung tissues harvested on days 2, 4, and 7 following infection. This restriction of replication was mediated by both the antibody and cellular components of the immune response, which was determined using animals that had been immunized with a chimeric HPIV3-1 virus that expresses the “internal” proteins of HPIV3 and the surface neutralization antigens of HPIV1. Surprisingly, despite the lack of detectable replication of HPIV3/EboGP in the respiratory tract, its immunogenicity was essentially the same as that observed in HPIV3-naive animals, which is sufficient for protection against EBOV challenge (Bukreyev et al., 2006b). One caveat is that we did not directly measure cell-mediated responses to HPIV3/EboGP in HPIV3-immune animals, due to a lack of available reagents. Therefore, we cannot rule out the formal possibility that the cellular immune response was substantially reduced in HPIV3-immune animals. However, even without any contribution from cell-mediated immunity, the levels of EBOV-specific serum antibodies that were achieved would be consistent with substantial protection. In the present study, the mean reciprocal ELISA titers of EBOV-specific serum antibodies were approximately 1:3,500 on day 28 and 1:7,500 on day 42. Previous studies showed that passive EBOV-specific antibodies alone can provide substantial protection against EBOV challenge. In one study, guinea pigs were infected intraperitoneally with EBOV and immediately given EBOV-specific passive antibodies by the subcutaneous route. A dose of antibodies that conferred a serum ELISA titer of 1:80 – 1:160 when measured two days later provided complete protection against the day 0 infection with 10,000 PFU of guinea pig-adapted EBOV (Jahrling et al., 1999). In a comparable experiment in mice, a dose of antibodies that conferred a serum ELISA titer of approximately 1 : 6,400 when measured on day 1 provided high level protection against a day 0 challenge with 1,000 PFU of EBOV (Gupta et al., 2001). This suggests that the response achieved by HPIV3/EboGP in HPIV3-immune animals in the present study would be protective.
These data contrasted with studies involving other vector systems, in which the immunogenicity of human adenovirus type 5-vectored and vaccinia virus-vectored vaccines was significantly reduced or completely abolished by the presence of the vector-specific immunity (see Introduction). The mechanism by which the immunogenicity of these latter vectors is reduced in immune animals is unknown, but might include neutralization of the vector inoculum, more rapid destruction of vector-infected cells, and neutralization of progeny vector in the case of replication-competent vectors.
Several mechanisms by which HPIV3/EboGP retained its immunogenicity in HPIV3-immune animals can be suggested. One possibility was that the presence of functional EBOV GP in the vector particle conferred increased infectivity and spread in HPIV3-immune animals. In monolayer cell culture, we found that HPIV3/EboGP indeed was more resistant than HPIV3 to neutralization by HPIV3-specific antibodies and had a somewhat greater ability to spread under those conditions. Although this effect was modest under the conditions that were tested in vitro, it might be sufficient to confer increased immunogenicity in vivo. In addition, the IN route of administration might play a role in the ability to immunize despite pre-existing immunity to the vector. Specifically, the effectiveness of host immunity in the respiratory tract characteristically is incomplete due to the short-lived nature of mucosal immunity following a primary infection, the inefficiency by which serum antibodies gain access to the respiratory lumen, and the functional impairment of cytotoxic T lymphocytes in the lung (Vallbracht, Unsold, and Ehl, 2006). In addition, certain respiratory viruses such as the HPIVs and respiratory syncytial virus seem particularly able to partially evade host immunity and establish symptomatic re-infections whereas other respiratory viruses such as influenza virus and adenovirus are more strongly restricted by prior immunity. Although the basis behind the re-infectability of viruses such as HPIV3 is poorly understood, this may contribute to the effect observed here. A recent study showed that, when cotton rats that were immune to respiratory syncytial virus were re-infected with the virus, the level of intracellular viral RNA synthesis during the first 12–24 h of infection was nearly as high as in non-immune animals even though no infectious progeny virus was detected in the immune animals throughout the infection (Boukhvalova, Prince, and Blanco, 2007). Thus, prior immunity did not seem to restrict infection and the initial viral replicative cycle, which presumably would result in substantial antigen synthesis. In this context, it is noteworthy that a recent study demonstrated that activation of respiratory dendritic cells takes place within the first 24 h after infection of mice with influenza virus (Legge and Braciale, 2003), which is long before the peak of the virus replication in lungs. After that, respiratory dendritic cells become refractory to stimulation by the virus (Legge and Braciale, 2003). Therefore, the effective presentation of EBOV antigen may depend more on the initial infectability and initial replicative cycle of the virus and be less dependent on the magnitude of subsequent replication.
We had previously assumed that HPIV3-based vectors would not be sufficiently immunogenic in adolescents and adults due to the prevalence of immunity to this common human pathogen. However, the present study suggests that use of the pneumotropic HPIV3 vector and the topical route of immunization may provide for substantial immunization in immune individuals. Indeed, if the vector is restricted by host immunity but is nonetheless immunogenic, vaccine safety would be increased. However, it will be essential to confirm that HPIV3/EboGP is immunogenic in HPIV3-immune non-human primates, which are anatomically and phylogenetically more closely related to humans. That would be followed by clinical trials, which in the interest of safety would employ an attenuated version of HPIV3 as vector. Several such attenuated versions have been or presently are in clinical trials as pediatric intranasal HPIV3 vaccine candidates (Murphy and Collins, 2002). Since non-human primates are less permissive than humans to HPIV3 replication, results obtained in non-human primates using wild type HPIV3 as vector may be comparable to what would be observed in humans using an attenuated derivative as vector. We also are developing chimeric viruses in which the HN and F proteins of the HPIV3 vector are deleted and replaced by GP. This would provide a vector that would not be neutralized by HPIV3-specific antibodies against the major HN and F antigens. While this chimeric virus would remain sensitive to HPIV3-specific cellular immunity directed against “internal” HPIV3 proteins, that immune component is much less long-lived than neutralizing antibodies and likely would be less effective in restricting the vector. Finally, use of non-human respiratory paramyxoviruses such as Newcastle disease virus as a platform for intranasal vaccine against EBOV may also be a promising approach (Bukreyev et al., 2005).
MATERIALS AND METHODS
Viruses, cells, animals, and HPIV3-specific antiserum
Recombinant wild type HPIV3 and HPIV3/EboGP used in this study have been described previously (Bukreyev et al., 2006b; Durbin et al., 1997). UV-inactivation of HPIV3/EboGP was performed with a UV Stratalinker 1800 (Stratagene, La Jolla, CA) using a UV dose of 128 mJoules, which was determined to be the minimum dose required for complete inactivation of infectivity of the preparation. Rhesus monkey kidney LLC-MK2 and human A549 type II alveolar adenocarcinoma cells (American Type Culture Collection, Manassas, VA) were grown in Opti-MEM medium containing 2.5% fetal bovine serum (both from Invitrogen, Carlsbad, CA). HPIV3 and HPIV3/EboGP were grown and titrated in LLC-MK2 cells. Guinea pigs (strain Hartley, four to thirteen weeks old) were obtained from Charles River Laboratories (Wilmington, MA) and confirmed to be seronegative for HPIV3 by HAI using guinea pig erythrocytes (van Wyke Coelingh, Winter, and Murphy, 1985). For intranasal (IN) inoculation, animals were anesthetized by inhalation of methoxyflurane (Medical Developments International Limited, Springvale, Australia), and 100 µl of a viral suspension in Leibowitz L-15 medium (Invitrogen) was applied to each nostril. Intramuscular (IM) inoculations involved 100 µl of a viral suspension in L-15 medium per animal. To isolate internal organs or tissue samples, the animals were sacrificed by carbon dioxide inhalation. All procedures were performed in accordance with protocols and guidelines approved by the NIH Animal Care and Use Committee and were performed in a facility approved by the Association for Assessment and Accreditation of Laboratory Animal Care International. Polyvalent HPIV3-specific antiserum was prepared by hyperimmunizing rabbits with sucrose gradient-purified HPIV3.
Quantitative analysis of the viruses in animal tissues
Harvested tissues were weighed, homogenized in L-15 medium (Invitrogen) using Omni TH tissue homogenizer with disposable tips (Omni International, Marietta, GA) and clarified by low-speed centrifugation, and the resulting tissue suspensions were aliquoted and stored at −80°C until virus titration. Virus titers were determined by limiting dilution in LLC-MK2 cells and expressed as TCID50. In some cases, plaque titrations in LLC-MK2 cells also were performed, as previously described (Bukreyev et al., 2006b). For quantitative RT-PCR, total RNA was isolated from the tissue extracts using RNeasy mini kit (Qiagen, Valencia, CA) according manufacturer's recommendations, subjected to reverse transcription reaction with random hexamers and analyzed with TaqMan Gene Expression Assay (Applied Biosystems, Foster City, CA). The following sets of primers and probes were designed and produced by Applied Biosystems: HPIV3 N gene-specific set, forward primer 5′-CGGTGACACAGTGGATCAGATT-3′, reverse primer 5′-TGTTTCAACCATAAGAGTTACCAAGCT-3′, probe 5′-ACCGCATGATTGACCC-3′; HPIV3 HN-specific set, forward primer 5′-CACAAACACGTGCAAATTTTACACT-3′, reverse primer 5′-AGTTGCAGTATCCTTTAATCTGTGTGAT3′-, probe 5′-CCGGTGTTAAAATTTT-3′. In some cases, nasal turbinate and lung samples from HPIV3-immune animals were negative for viral RNA due to the high level of protection: these samples were assigned a Ct value of 40, which was the limit of detection, in order to calculate mean Ct ± SE.
Immunohistochemical analysis of animal tissues
Lung tissues were fixed in neutral buffered formalin and embedded in paraffin, and sections were cut at 4–5 microns. The sections were mounted on positively charged slides. Antigen retrieval from paraffin sections was performed in a food steamer (Sunbeam, Boca Raton, FL) with Diva decloaker solution (Biocare, Concord, CA). Immunostaining for HPIV3 antigens was performed using a 1:500 dilution of HIPV3-specific polyclonal antibodies and the Dako Envision rabbit HRP (DAB+) kit with HRP labeled polymer (Dako, Carpenteria, CA).
Analysis of antibody responses
HPIV3-specific serum antibody responses were determined by the above-mentioned HAI assay (van Wyke Coelingh, Winter, and Murphy, 1985). EBOV-specific serum antibody responses were determined by ELISA against EBOV particles that had been inactivated with gamma radiation, purified, and disrupted with Tween 20 (Bukreyev et al., 2006b). For Fig. 5, the assay was performed exactly as previously described (Bukreyev et al., 2006b). For Fig. 6, the assay was performed in essentially the same way, but with differences in the plates, some of the wash solutions, and the secondary antibody and detection chemistry. Specifically, the EBOV antigen was coated onto flat bottom Immulux HB plates (Dynex Technologies, Chantilly, VA). The coated plates were washed five times with phosphate buffered saline (Invitrogen) containing 20% Tween-20 (PBST), incubated for 1 h at 37°C with blocking buffer composed of phosphate buffered saline with 5% nonfat dry milk (Nestle, Solon, OH) and 1% bovine serum albumin fraction V (Roche USA, Indianapolis, IN), and washed as above. Various dilutions of guinea pig serum samples in blocking buffer were added and the plates were incubated for 1 h at 37°C and washed as above. Next, 50 µl of 1:500 dilution of alkaline phosphatase-conjugated goat anti-guinea pig IgG antibodies (Antibodies Incorporated, Davis, CA) in blocking buffer were added, incubated for 1 h at 37°C, and washed as above. To develop the plates, 100 µl per well of Alkaline Phosphatase Yellow (pNPP) Liquid Substrate System for ELISA (Sigma-Aldrich, St. Louis, MO) was added, the plates were incubated 20 min at room temperature, and the reaction was stopped by adding 50 µl per well of 1 N sodium hydroxide. Optical density was determined at 405 nm.
Statistical analysis of data
Differences were evaluated by Student's T-test and considered significant when P<0.05. Data are shown as means ± SE of the mean.
ACKNOWLEDGMENTS
We thank Ernest Williams and Fatemeh Davoodi for performing HAI assays, Jason Clardy and his staff for animal care work and collection of serum samples, and Lawrence J. Faucette and Elizabeth M. Williams for histotechnology assistance. This project was funded as a part of the Intramural Research Program of NIAID, NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- Barouch DH, Pau MG, Custers JH, Koudstaal W, Kostense S, Havenga MJ, Truitt DM, Sumida SM, Kishko MG, Arthur JC, Korioth-Schmitz B, Newberg MH, Gorgone DA, Lifton MA, Panicali DL, Nabel GJ, Letvin NL, Goudsmit J. Immunogenicity of recombinant adenovirus serotype 35 vaccine in the presence of pre-existing anti-Ad5 immunity. J Immunol. 2004;172(10):6290–6297. doi: 10.4049/jimmunol.172.10.6290. [DOI] [PubMed] [Google Scholar]
- Boukhvalova MS, Prince GA, Blanco JC. Respiratory syncytial virus infects and abortively replicates in the lungs in spite of preexisting immunity. J Virol. 2007;81(17):9443–9450. doi: 10.1128/JVI.00102-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Huang Z, Yang L, Elankumaran S, St Claire M, Murphy BR, Samal SK, Collins PL. Recombinant Newcastle disease virus expressing a foreign viral antigen is attenuated and highly immunogenic in primates. J Virol. 2005;79(21):13275–13284. doi: 10.1128/JVI.79.21.13275-13284.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Rollin PE, Tate MK, Yang L, Zaki SR, Shieh WJ, Murphy BR, Collins PL, Sanchez A. Successful topical respiratory tract immunization of primates against Ebola virus. J Virol. 2007;81(12):6379–6388. doi: 10.1128/JVI.00105-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Skiadopoulos MH, Murphy BR, Collins PL. Nonsegmented negative-strand viruses as vaccine vectors. J Virol. 2006a;80(21):10293–10306. doi: 10.1128/JVI.00919-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukreyev A, Yang L, Zaki SR, Shieh WJ, Rollin PE, Murphy BR, Collins PL, Sanchez A. A Single Intranasal Inoculation with a Paramyxovirus-Vectored Vaccine Protects Guinea Pigs against a Lethal-Dose Ebola Virus Challenge. J Virol. 2006b;80(5):2267–2279. doi: 10.1128/JVI.80.5.2267-2279.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulletin WHO. Ebola haemmorhagic fever in Zaire. 1976;56:271–293. [PMC free article] [PubMed] [Google Scholar]
- Burns JW, Siadat-Pajouh M, Krishnaney AA, Greenberg HB. Protective effect of rotavirus VP6-specific IgA monoclonal antibodies that lack neutralizing activity. Science. 1996;272(5258):104–107. doi: 10.1126/science.272.5258.104. [DOI] [PubMed] [Google Scholar]
- Casimiro DR, Chen L, Fu TM, Evans RK, Caulfield MJ, Davies ME, Tang A, Chen M, Huang L, Harris V, Freed DC, Wilson KA, Dubey S, Zhu DM, Nawrocki D, Mach H, Troutman R, Isopi L, Williams D, Hurni W, Xu Z, Smith JG, Wang S, Liu X, Guan L, Long R, Trigona W, Heidecker GJ, Perry HC, Persaud N, Toner TJ, Su Q, Liang X, Youil R, Chastain M, Bett AJ, Volkin DB, Emini EA, Shiver JW. Comparative immunogenicity in rhesus monkeys of DNA plasmid, recombinant vaccinia virus, and replication-defective adenovirus vectors expressing a human immunodeficiency virus type 1 gag gene. J Virol. 2003;77(11):6305–6313. doi: 10.1128/JVI.77.11.6305-6313.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durbin A, Hall S, Siew J, Whitehead S, Collins P, Murphy B. Recovery of infectious human parainfluenza virus type 3 from cDNA. Virology. 1997;235(2):232–232. doi: 10.1006/viro.1997.8697. [DOI] [PubMed] [Google Scholar]
- Feng N, Lawton JA, Gilbert J, Kuklin N, Vo P, Prasad BV, Greenberg HB. Inhibition of rotavirus replication by a non-neutralizing, rotavirus VP6-specific IgA mAb. J Clin Invest. 2002;109(9):1203–1213. doi: 10.1172/JCI14397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzgerald JC, Gao GP, Reyes-Sandoval A, Pavlakis GN, Xiang ZQ, Wlazlo AP, Giles-Davis W, Wilson JM, Ertl HC. A simian replication-defective adenoviral recombinant vaccine to HIV-1 gag. J Immunol. 2003;170(3):1416–1422. doi: 10.4049/jimmunol.170.3.1416. [DOI] [PubMed] [Google Scholar]
- Geisbert TW, Jahrling PB. Exotic emerging viral diseases: progress and challenges. Nat Med. 2004;10(12 Suppl):S110–S121. doi: 10.1038/nm1142. [DOI] [PubMed] [Google Scholar]
- Gupta M, Mahanty S, Bray M, Ahmed R, Rollin PE. Passive transfer of antibodies protects immunocompetent and imunodeficient mice against lethal Ebola virus infection without complete inhibition of viral replication. J Virol. 2001;75(10):4649–4654. doi: 10.1128/JVI.75.10.4649-4654.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaax N, Jahrling P, Geisbert T, Geisbert J, Steele K, McKee K, Nagley D, Johnson E, Jaax G, Peters C. Transmission of Ebola virus (Zaire strain) to uninfected control monkeys in a biocontainment laboratory. Lancet. 1995;346(8991–8992):1669–1671. doi: 10.1016/s0140-6736(95)92841-3. [DOI] [PubMed] [Google Scholar]
- Jaax NK, Davis KJ, Geisbert TJ, Vogel P, Jaax GP, Topper M, Jahrling PB. Lethal experimental infection of rhesus monkeys with Ebola-Zaire (Mayinga) virus by the oral and conjunctival route of exposure. Arch Pathol Lab Med. 1996;120(2):140–155. [PubMed] [Google Scholar]
- Jahrling PB, Geisbert TW, Geisbert JB, Swearengen JR, Bray M, Jaax NK, Huggins JW, LeDuc JW, Peters CJ. Evaluation of immune globulin and recombinant interferon-alpha2b for treatment of experimental Ebola virus infections. J Infect Dis. 1999;179 Suppl 1:S224–S234. doi: 10.1086/514310. [DOI] [PubMed] [Google Scholar]
- Johnson E, Jaax N, White J, Jahrling P. Lethal experimental infections of rhesus monkeys by aerosolized Ebola virus. Int J Exp Pathol. 1995;76(4):227–236. [PMC free article] [PubMed] [Google Scholar]
- Jones SM, Feldmann H, Stroher U, Geisbert JB, Fernando L, Grolla A, Klenk HD, Sullivan NJ, Volchkov VE, Fritz EA, Daddario KM, Hensley LE, Jahrling PB, Geisbert TW. Live attenuated recombinant vaccine protects nonhuman primates against Ebola and Marburg viruses. Nat Med. 2005;11(7):786–790. doi: 10.1038/nm1258. [DOI] [PubMed] [Google Scholar]
- Kanesa-thasan N, Smucny JJ, Hoke CH, Marks DH, Konishi E, Kurane I, Tang DB, Vaughn DW, Mason PW, Shope RE. Safety and immunogenicity of NYVAC-JEV and ALVAC-JEV attenuated recombinant Japanese encephalitis virus--poxvirus vaccines in vaccinia-nonimmune and vaccinia-immune humans. Vaccine. 2000;19(4–5):483–491. doi: 10.1016/s0264-410x(00)00191-2. [DOI] [PubMed] [Google Scholar]
- Karron RA, Collins PL. Parainfluenza Viruses. In: Knipe DM, Howley PM, Griffin DE, Lamb RA, Martin MA, Roizman B, Straus SE, editors. Fields Virology. 5 ed. 1. 2 vols. Philadelphia: Lippincott-Raven Publishers; 2007. [Google Scholar]
- Legge KL, Braciale TJ. Accelerated migration of respiratory dendritic cells to the regional lymph nodes is limited to the early phase of pulmonary infection. Immunity. 2003;18(2):265–277. doi: 10.1016/s1074-7613(03)00023-2. [DOI] [PubMed] [Google Scholar]
- Lemckert AA, Sumida SM, Holterman L, Vogels R, Truitt DM, Lynch DM, Nanda A, Ewald BA, Gorgone DA, Lifton MA, Goudsmit J, Havenga MJ, Barouch DH. Immunogenicity of heterologous prime-boost regimens involving recombinant adenovirus serotype 11 (Ad11) and Ad35 vaccine vectors in the presence of anti-ad5 immunity. J Virol. 2005;79(15):9694–9701. doi: 10.1128/JVI.79.15.9694-9701.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendoza QP, Stanley J, Griffin DE. Monoclonal antibodies to the E1 and E2 glycoproteins of Sindbis virus: definition of epitopes and efficiency of protection from fatal encephalitis. J Gen Virol. 1988;69(Pt 12):3015–3022. doi: 10.1099/0022-1317-69-12-3015. [DOI] [PubMed] [Google Scholar]
- Murphy BR, Collins PL. Live-attenuated virus vaccines for respiratory syncytial and parainfluenza viruses: applications of reverse genetics. J Clin Invest. 2002;110(1):21–27. doi: 10.1172/JCI16077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkoghe D, Formenty P, Leroy EM, Nnegue S, Edou SY, Ba JI, Allarangar Y, Cabore J, Bachy C, Andraghetti R, de Benoist AC, Galanis E, Rose A, Bausch D, Reynolds M, Rollin P, Choueibou C, Shongo R, Gergonne B, Kone LM, Yada A, Roth C, Mve MT. [Multiple Ebola virus haemorrhagic fever outbreaks in Gabon, from October 2001 to April 2002] Bull Soc Pathol Exot. 2005;98(3):224–229. [PubMed] [Google Scholar]
- Prince GA, Potash L, Horswood RL, Camargo E, Suffin SC, Johnson RA, Chanock RM. Intramuscular inoculation of live respiratory syncytial virus induces immunity in cotton rats. Infect Immun. 1979;23(3):723–728. doi: 10.1128/iai.23.3.723-728.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salvaggio MR, Baddley JW. Other viral bioweapons: Ebola and Marburg hemorrhagic fever. Dermatol Clin. 2004;22(3):291–302. doi: 10.1016/j.det.2004.03.003. vi. [DOI] [PubMed] [Google Scholar]
- Sharpe S, Polyanskaya N, Dennis M, Sutter G, Hanke T, Erfle V, Hirsch V, Cranage M. Induction of simian immunodeficiency virus (SIV)-specific CTL in rhesus macaques by vaccination with modified vaccinia virus Ankara expressing SIV transgenes: influence of pre-existing anti-vector immunity. J Gen Virol. 2001;82(Pt 9):2215–2223. doi: 10.1099/0022-1317-82-9-2215. [DOI] [PubMed] [Google Scholar]
- Skiadopoulos MH, Surman SR, Riggs JM, Orvell C, Collins PL, Murphy BR. Evaluation of the replication and immunogenicity of recombinant human parainfluenza virus type 3 vectors expressing up to three foreign glycoproteins. Virology. 2002;297(1):136–152. doi: 10.1006/viro.2002.1415. [DOI] [PubMed] [Google Scholar]
- Sullivan NJ, Sanchez A, Rollin PE, Yang ZY, Nabel GJ. Development of a preventive vaccine for Ebola virus infection in primates. Nature. 2000;408(6812):605–609. doi: 10.1038/35046108. [DOI] [PubMed] [Google Scholar]
- Sumida SM, Truitt DM, Kishko MG, Arthur JC, Jackson SS, Gorgone DA, Lifton MA, Koudstaal W, Pau MG, Kostense S, Havenga MJ, Goudsmit J, Letvin NL, Barouch DH. Neutralizing antibodies and CD8+ T lymphocytes both contribute to immunity to adenovirus serotype 5 vaccine vectors. J Virol. 2004;78(6):2666–2673. doi: 10.1128/JVI.78.6.2666-2673.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao T, Durbin AP, Whitehead SS, Davoodi F, Collins PL, Murphy BR. Recovery of a fully viable chimeric human parainfluenza virus (PIV) type 3 in which the hemagglutinin-neuraminidase and fusion glycoproteins have been replaced by those of PIV type 1. J Virol. 1998;72(4):2955–2961. doi: 10.1128/jvi.72.4.2955-2961.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao T, Skiadopoulos MH, Davoodi F, Riggs JM, Collins PL, Murphy BR. Replacement of the ectodomains of the hemagglutinin-neuraminidase and fusion glycoproteins of recombinant parainfluenza virus type 3 (PIV3) with their counterparts from PIV2 yields attenuated PIV2 vaccine candidates. J Virol. 2000;74(14):6448–6458. doi: 10.1128/jvi.74.14.6448-6458.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallbracht S, Unsold H, Ehl S. Functional impairment of cytotoxic T cells in the lung airways following respiratory virus infections. Eur J Immunol. 2006;36(6):1434–1442. doi: 10.1002/eji.200535642. [DOI] [PubMed] [Google Scholar]
- van Wyke Coelingh KL, Winter C, Murphy BR. Antigenic variation in the hemagglutinin-neuraminidase protein of human parainfluenza type 3 virus. Virology. 1985;143(2):569–582. doi: 10.1016/0042-6822(85)90395-2. [DOI] [PubMed] [Google Scholar]
- Volchkov VE, Chepurnov AA, Volchkova VA, Ternovoj VA, Klenk HD. Molecular characterization of guinea pig-adapted variants of Ebola virus. Virology. 2000;277(1):147–155. doi: 10.1006/viro.2000.0572. [DOI] [PubMed] [Google Scholar]
- Warfield KL, Swenson DL, Olinger GG, Kalina WV, Aman MJ, Bavari S. Ebola virus-like particle-based vaccine protects nonhuman primates against lethal Ebola virus challenge. J Infect Dis. 2007;196 Suppl 2:S430–S437. doi: 10.1086/520583. [DOI] [PubMed] [Google Scholar]
- Yang ZY, Wyatt LS, Kong WP, Moodie Z, Moss B, Nabel GJ. Overcoming immunity to a viral vaccine by DNA priming before vector boosting. J Virol. 2003;77(1):799–803. doi: 10.1128/JVI.77.1.799-803.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Bukreyev A, Thompson CI, Watson B, Peeples ME, Collins PL, Pickles RJ. Infection of ciliated cells by human parainfluenza virus type 3 in an in vitro model of human airway epithelium. J Virol. 2005;79(2):1113–1124. doi: 10.1128/JVI.79.2.1113-1124.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhi Y, Figueredo J, Kobinger GP, Hagan H, Calcedo R, Miller JR, Gao G, Wilson JM. Efficacy of Severe Acute Respiratory Syndrome Vaccine Based on a Nonhuman Primate Adenovirus in the Presence of Immunity Against Human Adenovirus. Hum Gene Ther. 2006;17(5):500–506. doi: 10.1089/hum.2006.17.500. [DOI] [PubMed] [Google Scholar]