Abstract
The infectivity of flavivirus particles depends on a maturation process that is triggered by the proteolytic cleavage of the precursor of the M protein (prM). This activation cleavage is naturally performed by ubiquitous cellular proteases of the furin family, which typically recognize the multibasic sequence motif R-X-R/K-R. Previously, we demonstrated that a tick-borne encephalitis virus (TBEV) mutant with an altered cleavage motif, R-X-R, produced immature, noninfectious particles that could be activated by exogenous trypsin, which cleaves after single basic residues. Here, we report the adaptation of this mutant to chymotrypsin, a protease specific for large, hydrophobic amino acid residues. Using selection pressure in cell culture, two different mutations conferring a chymotrypsin-dependent phenotype were identified. Surprisingly, one of these mutations (Ser85Phe) occurred three positions upstream of the natural cleavage site. The other mutation (Arg89His) arose at the natural cleavage position but involved a His residue, which is not a typical chymotrypsin cleavage site. Efficient cleavage of protein prM and activation by the heterologous protease were confirmed using various recombinant TBEV mutants. Mutants with only the originally selected mutations exhibited unimpaired export kinetics and were genotypically stable during at least six cell culture passages. However, in contrast to the wild-type virus or trypsin-dependent mutants, chymotrypsin-dependent mutants were not neurovirulent in suckling mice. Our results demonstrate that flaviviruses with altered protease specificities can be generated and suggest that this approach can be used for the construction of viral mutants or vectors that can be activated on demand and have restricted tissue tropism and virulence.
Enveloped viruses contain surface proteins that mediate and regulate fusion of viral and host cell membranes, a crucial step for viral entry. To ensure a proper and timely delivery of the viral nucleocapsid into the cell, fusion is usually triggered by a specific mechanism such as binding to cell-surface receptors and/or exposure to the acidic environment encountered by the virus after uptake into endosomal vesicles (5, 12). It is very important for the virus to make sure that the structural changes in its surface proteins that initiate fusion are not triggered prematurely or within an inappropriate environment. For instance, during transport to the cell surface, viral envelope proteins may encounter an acidic environment in late Golgi compartments, potentially resulting in structural changes that would destroy the fusion activity or interfere with particle release. A major mechanism that many viruses have evolved to prevent inappropriate triggering of the fusion process is the synthesis of the fusion-inducing protein in a precursor form that gets cleaved at a late stage before viral release—or even after release if the virus encounters proteases outside the cell (2, 23, 39, 45, 48, 56, 58). There are two major pathways of proteolytic activation of viral surface proteins. Either the fusion protein itself is subject to this activating cleavage or an auxiliary protein that is complexed with the fusion protein gets cleaved, freeing the fusion protein to undergo fusion-related conformational changes (30). In both cases, the proteolytic activation of fusion competence is a crucial step of the viral life cycle and thus represents a major determinant of viral virulence, host range, and tissue tropism.
Flaviviruses, i.e., members of the genus Flavivirus, family Flaviviridae, are small, enveloped viruses that contain only two surface proteins, both of which are carboxy-terminally anchored in the viral membrane (31). Fusion activation of flaviviruses is a typical example of the pathway in which cleavage of a precursor protein without intrinsic fusion capacity leads to the activation of fusion and viral infectivity. The large glycoprotein E carries the activities for both receptor binding and fusion. During assembly of virus particles in the lumen of the endoplasmic reticulum, protein E is complexed to prM, the precursor of the M protein. Immature flavivirus particles with prM-E heterodimers are fusion incompetent and are therefore protected from premature initiation of fusion during their transport through the exocytotic pathway, where they mature before being released from the cell (16, 49). Cleavage of protein prM results in the loss of its N-terminal domain, leaving the much smaller protein M associated with the membrane and inducing major structural rearrangements of the viral surface, including the organization of protein E into homodimers (1, 52). As a result, the mature virions that are released are fusion competent and infectious.
Cleavage of the flavivirus protein prM is normally carried out by the serine protease furin or related members of the family of prohormone-proprotein convertases (49). Furin is a major endoproteolytic processing enzyme of the secretory pathway. It is expressed ubiquitously in all tissues and shuttles between the trans-Golgi network, the cell surface, and endosomal compartments (37). It has an essential function in the processing of many cellular precursor proteins, such as prohormones (41). Its activity gets parasitized for the activation of bacterial toxins (9, 38) as well as viral precursor proteins (11, 49, 53, 55). Furin cleaves its substrates with narrow specificity after the highly conserved consensus sequence R-X-R/K-R, although cleavage of the minimal furin motif R-X-X-R has also been reported (13, 24, 38). All known sequences of flavivirus prM proteins contain a canonical furin cleavage site, and direct evidence for the central role of furin or a furin-like protease for cleavage of protein prM and maturation of flavivirus particles has been obtained (6, 49). Cleavage naturally takes place at a late stage of flavivirus exocytosis, although particles containing uncleaved protein prM are also observed to be released from infected cells together with mature virions in proportions depending on the virus and the growth conditions (10, 40, 56).
Flaviviruses have an approximately 11-kb-long, positive-stranded RNA genome that encodes three structural proteins (the capsid protein C and the two above-mentioned surface proteins prM and E) and seven nonstructural proteins in a single long open reading frame (31). The primary translation product, a polyprotein, is cleaved by viral and cellular proteases to form the individual viral proteins. The availability of infectious cDNA clones for major human pathogenic flaviviruses, such as yellow fever virus (4, 44), Japanese encephalitis virus (54, 57), West Nile virus (21, 47), the dengue viruses (20, 22, 28, 43), and tick-borne encephalitis virus (TBEV) (14, 32), facilitates the analysis of molecular determinants of infectivity and pathogenesis by reverse genetics. Using this approach, we have previously examined the dependence of viral infectivity of TBEV on the proteolytic cleavage of protein prM (6). The deletion of an Arg residue from the furin site within the TBEV protein prM sequence completely abolished the natural proteolytic activation and resulted in the exclusive release of immature, noninfectious virus particles. However, the remaining R-X-R sequence motif was still a potential substrate for the serine protease trypsin, which cleaves after single positively charged amino acid residues (Lys or Arg). Addition of trypsin converted the immature mutant particles into single-round infectious particles.
Trypsin is one of the major pancreatic enzymes and is abundant in the digestive tract. In addition, trypsin or trypsin-like proteases are present extracellularly in various tissues including the lung and brain. In vivo experiments have indicated that subcutaneous inoculation of mice with the trypsin-dependent TBEV mutant did not cause infection, whereas inoculation into the brain, where trypsin-like proteases are present, led to low-level infectivity. Revertants selected from this trypsin-dependent TBEV either had the cleavage site restored to a minimal furin substrate or exhibited various mutations in the N-terminal (“pr”) part of protein prM, which may have increased the susceptibility to trypsin-like proteases or reduced the capacity of protein prM to prevent protein E from undergoing the conformational changes necessary for membrane fusion (7).
In this study, we used selection pressure to further change the protease specificity of cleavage activation of TBEV. To accomplish this, the trypsin-dependent mutant was subjected to repeated cycles of cell culture passage in the presence of chymotrypsin. This protease is not naturally involved in any viral activation processes and differs strongly from trypsin- or furin-like proteases in its cleavage specificity. It preferentially cleaves after amino acids with large hydrophobic side chains, such as Trp, Phe, Tyr, or Leu, but not after the positively charged residues Arg and Lys. Like trypsin, chymotrypsin is a serine protease and one of the major pancreatic enzymes. However, unlike the ubiquitous furin and the trypsin-like proteases, which are found in many tissues, chymotrypsin activity is mostly restricted to the digestive tract. We now report on the successful isolation of chymotrypsin-adapted TBEV mutants. Mutations conferring this phenotype were identified, and engineered mutants with these and additional mutations were characterized with respect to cleavage specificity, activation, growth, and genetic stability in cell culture as well as neurovirulence in suckling mice. Our results demonstrate that it is possible to alter the specificity for activation of a flavivirus so that it uses a protease that is not naturally involved in viral fusion activation. This approach makes it feasible to design flavivirus strains, vaccines, or vectors that can be selectively activated in vitro and that have different tissue tropism in vivo from wild-type viruses.
MATERIALS AND METHODS
Virus and cells.
BHK-21 cells (ATCC CCL10) were grown under standard conditions in Eagle's minimal essential medium supplemented with 5% fetal calf serum (FCS), 1% glutamine, and 0.5% neomycin (growth medium) and were maintained in minimal essential medium supplemented with 0.5% FCS, 1% glutamine, and 0.5% neomycin, and buffered with 15 mM HEPES, pH 7.4 (maintenance medium).
All mutant constructs described in this study were derived from the infectious cDNA clone of the TBEV Western subtype prototypic strain Neudoerfl, which has been characterized in detail (33, 34), including the determination of its entire genomic sequence (GenBank accession no. U27495). Mutant prM(ΔR88), which was used for selection experiments, carries a single point mutation in protein prM (deletion of Arg88) that confers resistance to furin cleavage, and this mutant was previously characterized in detail (6).
RNA transcription and transfection.
In vitro transcription of RNA and transfection of BHK-21 cells by electroporation were performed as described previously (32). Briefly, capped RNA was synthesized using m7GpppG Cap analogue and reagents from the T7 Megascript kit (Ambion) according to the manufacturer's protocol. Template DNA was digested by DNase I incubation, and the quality of the RNA was checked by formalin-denaturing 1% agarose gel electrophoresis. For quantitative analysis, in vitro transcribed RNA was purified using an RNeasy Mini Kit (Qiagen) and quantitated spectrophotometrically. Equimolar amounts of the RNA were then subsequently introduced by electroporation into BHK-21 cells using a GenePulser apparatus (Bio-Rad).
Plasmids and cloning procedures.
Plasmid pTNd/c contains cDNA corresponding to the full-length genome of TBEV strain Neudoerfl (32), and RNA transcribed from this plasmid was used as a wild-type control. Construction of plasmids pTNd/c-prM(ΔR88) and pTNd/5′-prM(ΔR88), which encode the full-length genome and the 5′ one-third of the genome, respectively, and contain a deletion of Arg88 in protein prM, was described previously (6).
All mutant constructs described in this study were generated by introducing the respective mutations into plasmid pTNd/5′-prM(ΔR88) using a GeneTailor site-directed mutagenesis system (Invitrogen) and the oligonucleotides listed in Table 1. Fragments containing the desired mutations were then introduced into the full-length cDNA clone pTNd/c by taking advantage of unique restriction sites for SalI and SnaBI, located upstream of the 5′ end of the inserted genome and at nucleotide 1883 of the genome, respectively.
TABLE 1.
Oligonucleotides used for site-directed mutagenesis
| Construct | Sequence (5′→3′)a | Orientation |
|---|---|---|
| prM(ΔR88/S85F) | TGTGGGAAACAGGAAGGCTTTAGAACACGCTCAGTGCTGA | Sense |
| prM(ΔR88/R89H) | TGTGGGAAACAGGAAGGCTCTAGAACACACTCAGTGCTGA | Sense |
| prM(ΔR88/S85F/R86S/R89S) | TGTGGGAAACAGGAAGGCTTTTCAACATCGTCAGTGCTGA | Sense |
| prM(ΔR88/R86S/R89H) | TGTGGGAAACAGGAAGGCTCTTCAACACACTCAGTGCTGA | Sense |
| All constructs | GCCTTCCTGTTTCCCACAGCGTCCGTAC | Antisense |
Mutated nucleotides with respect to the original sequence of prM(ΔR88) are indicated in bold.
All plasmids were propagated in Escherichia coli strain HB101, and plasmid preparations were made using commercially available systems (Qiagen and Sigma). The sequences of all newly generated plasmids were verified by sequence analysis of all regions that were modified or inserted in the course of the cloning procedures.
Selection of mutants.
BHK-21 cells were transfected with in vitro transcribed RNA derived from plasmid pTNd/prM(ΔR88). After electroporation, cells were washed twice and allowed to grow in protease-free medium supplemented with 5% FCS. This growth medium was replaced after 10 h with medium containing only 2% FCS. Then, cells were grown for 3 days following three different protocols (experiments C1, C2, and C3). In experiment C1, medium was exchanged 24, 48, and 72 h posttransfection with serum-free medium containing 2.5 μg/ml chymotrypsin (Sigma). After a 3-h incubation period, the chymotrypsin-containing medium was replaced again with the protease-free growth medium containing 2% FCS. In experiment C2, the chymotrypsin incubation window was applied only twice (at 48 and 72 h posttransfection), and in experiment C3 only once (at 72 h posttransfection). In all experiments, cell culture supernatants were harvested 75 h after transfection and cleared of cell debris by low-speed centrifugation. Undiluted aliquots (200 μl) of the supernatants were used to inoculate fresh BHK-21 cells. During the first passage, virus growth was allowed to occur for 6 days, during which time cells were again incubated with protease-free growth medium containing 2% FCS that was replaced every 24 h with serum-free medium containing 2.5 μg/ml chymotrypsin for 3-h time periods. Five subsequent cell culture passages were performed in the same way using alternating growth conditions of protease-free growth medium and protease-containing activation medium, but virus was harvested already 3 days postinoculation. Infection of cells was monitored qualitatively throughout the passaging experiments by immunofluorescence assay (IFA) as described below, as well as by a four-layer enzyme-linked immunosorbent assay (ELISA) (17). For sequence analysis, the medium changes on day 3 were omitted to increase the virus concentration in the supernatants. Viral RNA was extracted as described elsewhere (19), reverse transcribed using a cDNA Synthesis System (Roche), and amplified by PCR using TBEV-specific primers. DNA sequences were determined using an ABI 310 Genetic Analyzer (Applied Biosystems).
Cell culture experiments and detection of protein E.
BHK-21 cells were transfected with in vitro transcribed RNA as described above. Sixteen hours after transfection, cells were washed twice and were allowed to grow in maintenance medium for 2 to 3 days. To study activation of viruses by different proteases, trypsin (Sigma) and chymotrypsin were added to the maintenance medium to a final concentration of 5 μg/ml.
The amount of protein E released into the cell culture supernatants was monitored using a four-layer ELISA as described elsewhere (17). For a quantitative determination of protein E concentrations, a denaturing sodium dodecyl sulfate ELISA (SDS-ELISA) was applied as described previously (16).
For IFA, cells were seeded in 24-well tissue culture plates containing glass coverslips and incubated under standard conditions. After 24 to 72 h, the cells were fixed and permeabilized using acetone-methanol (1:1), and intracellular expression of protein E was detected using a polyclonal rabbit anti-protein E serum and a fluorescein isothiocyanate-conjugated anti-rabbit antibody (Jackson Immunoresearch Laboratory).
Western blot analysis.
Supernatants from BHK-21 cells that had been transfected with equimolar amounts of in vitro transcribed RNA were harvested, and their protein E concentration was determined by SDS-ELISA. Aliquots containing 500 ng of protein E were then incubated for 2 h at 37°C with phosphate-buffered saline (PBS), 10 μg/ml trypsin, or 10 μg/ml chymotrypsin and then subjected to deoxycholate trichloroacetic acid precipitation and boiled in Laemmli sample buffer. Proteins were separated on a 15% polyacrylamide-SDS gel and subsequently transferred onto a polyvinylidene difluoride membrane. Blots were incubated overnight at 4°C in blocking solution (1% bovine serum albumin and 0.1% Tween 20 in PBS). Protein prM and its cleavage products were detected by incubation with a rabbit polyclonal serum that recognizes prM and M in blocking solution for 2 h at room temperature. Blots were washed three times for 5 min with blocking buffer, incubated for 90 min with anti-rabbit immunoglobulin G alkaline peroxidase conjugate (Amersham), and washed again as described above. Antibody-protein complexes were visualized immunoenzymatically using SigmaFast diaminobenzidine tablets (Sigma).
Animal experiments.
Litters (between 9 and 13 animals) of suckling Swiss albino mice were inoculated intracerebrally with 20 μl of cell culture supernatant containing 200 ng/ml protein E, as determined by SDS-ELISA. Animals were then monitored for signs of neurological disease over a period of 28 days. Brains of severely diseased mice were used to harvest virus. Mouse brain suspensions (20%, wt/vol) were prepared, homogenized, cleared by low-speed centrifugation, and stored at −80°C. The presence of virus in the brains of diseased mice was verified by reverse transcription-PCR and sequence analysis. Serum samples were drawn from surviving mice and tested for seroconversion using a previously described antibody ELISA (15).
RNA export.
BHK-21 cells were transfected with equimolar amounts of RNA (1 × 1012 RNA molecules) as described above and subsequently washed four times with growth medium to remove any noninternalized RNA. Approximately 1 × 106 cells were then seeded in 25-cm2 tissue culture flasks, and 140-μl aliquots of supernatants were collected at individual time points and cleared by low-speed centrifugation to remove cell debris. Viral RNA was extracted using commercially available systems (QIAamp Viral RNA Mini Kit or RNeasy Mini Kit, respectively; Qiagen) according to the manufacturer's protocol. The isolated RNA was then used as a template for cDNA synthesis using the iScript cDNA synthesis kit (Bio-Rad) according to the manufacturer's protocol. An aliquot of each cDNA preparation corresponding to 2.5 μl of the original cell culture supernatant was then used for quantitative real-time PCR analysis (Applied Biosystems) as described in an earlier publication (25).
RNA was quantitated by comparing the results to a standard curve prepared using a serial 10-fold dilution of spectrophotometrically quantitated, in vitro transcribed RNA.
RESULTS
Adaptation of a TBEV mutant to chymotrypsin activation is accompanied by sequence changes in protein prM.
It was shown previously that TBEV mutant prM(ΔR88) is resistant to cleavage by the host cell protease furin due to a deletion of an Arg residue from the canonical furin recognition site in protein prM (6). As shown in Fig. 1, the wild-type cleavage site R-T-R-R was changed to R-T-R in this mutant. Transfection of BHK-21 cells with in vitro transcribed prM(ΔR88) RNA results in the production of immature, noninfectious virus particles containing uncleaved prM protein. These particles can be activated by adding trypsin to the cell culture medium, presumably because it cleaves at one of the two remaining Arg residues. In the presence of trypsin, this mutant can be passaged repeatedly, but after a single passage in trypsin-free medium, only noninfectious particles are released.
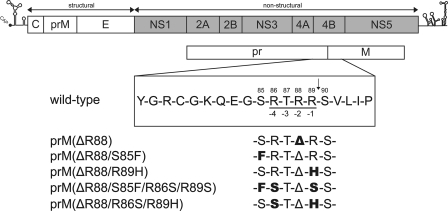
FIG. 1.
Genetic organization of TBEV. The amino acid sequences of the furin cleavage site and surrounding residues are listed below the diagram. The furin recognition sequence is underlined, and the numbering of its residues (−1 to −4) is relative to the site of cleavage, which is indicated by an arrow. Numbers at the top refer to the amino acid positions within protein prM. Arg88 was deleted in all mutants, indicated as Δ.
Inspection of the amino acid sequence of TBEV prM protein indicates that residues which may potentially be cleaved by chymotrypsin are present 14 amino acids upstream (Tyr) and 3 amino acids downstream (Leu) from the natural cleavage position (Fig. 1). In a first step, we wanted to examine whether mutant prM(ΔR88) could be activated by chymotrypsin. To this end, BHK-21 cells were transfected with in vitro transcribed prM(ΔR88) RNA, and standard passaging experiments were performed in parallel using cell culture medium containing trypsin, chymotrypsin, or no protease. In agreement with our previous observations, samples from trypsin-containing cultures readily infected fresh BHK-21 cells. However, no infected cells were observed with samples containing chymotrypsin or lacking protease after passaging of the supernatants, indicating that chymotrypsin was not able to activate mutant prM(ΔR88) under these conditions (data not shown). Apparently, the residues in the vicinity of the natural cleavage site which are potential substrates for chymotrypsin were either not cleaved under the experimental conditions or cleavage at these sites was not sufficient to render virions infectious.
Next, we sought to select for chymotrypsin-activated mutants by repeated blind passages of mutant prM(ΔR88) in cell culture to which the protease was added at various times. The selection protocol (as described in more detail in Materials and Methods) employed repeated cycles of growing cells in protease-free growth medium alternating with 3-h incubation periods with serum-free medium containing chymotrypsin. Infection of cells throughout these passages was detected by immunofluorescence staining of intracellular protein E and measurement of extracellular protein E by ELISA. This monitoring showed that virus was indeed being maintained and amplified through these passages. After five passages, aliquots of the supernatant were subjected to two further passages without chymotrypsin. In passage 6, viral particles were still released into the supernatant (as detected by ELISA), whereas no infectious virus was detectable in passage 7, suggesting that chymotrypsin-dependent mutants had been selected.
To determine the genetic basis for this phenotype, viral RNA from three independent passaging experiments (C1, C2, and C3, differing from each other by the number of chymotrypsin incubation window periods that were applied during the first 3 days after transfection) was purified from supernatants of the sixth passage. The region encoding the structural proteins was sequenced. Sequence changes were identified in all three cases and are summarized in Table 2. Significantly, each virus had an amino acid change in protein prM. In two of the cases, the same mutation, Arg89His, was observed, whereas the third sample contained the mutation Ser85Phe. Although chymotrypsin does not typically cleave after His residues, the fact that the Arg-to-His change emerged at prM residue 89, the precise position where cleavage naturally occurs, strongly suggests that this residue may be utilized by the protease in this particular sequence environment. The other selected amino acid, Phe, is one of the residues typically recognized by chymotrypsin. It emerged three positions upstream from the natural cleavage site, suggesting that prM cleavage at this upstream position can also yield infectious virus. Other mutations that were identified in the same samples were considered unlikely to be involved in the expression of the chymotrypsin-dependent phenotype. These included a conservative amino acid change in protein C, two silent nucleotide changes, and an identical amino acid change in protein E in each of the three samples. The change in E was of the type observed previously during passages of TBEV in BHK-21 cells and shown to be related to adaptation to the use of heparan sulfate for binding to the cell surface (26, 36).
TABLE 2.
Additional mutations of viruses passaged in the presence of chymotrypsin
| Experiment | Protein | Nucleotide substitutiona | Amino acid substitutionb |
|---|---|---|---|
| C1 | prM/M | C734T | S85F |
| E | G1333A | E122K | |
| C2 | prM/M | G743A | R89H |
| E | G1333A | E122K | |
| E | G1557A | ||
| C3 | C | A148G | I6V |
| prM/M | G743A | R89H | |
| prM/M | C888T | ||
| E | G1333A | E122K |
Numbering refers to the nucleotide position in the TBEV genome sequence.
Numbering refers to the amino acid residue within the indicated protein.
Mutations in protein prM confer cleavability by chymotrypsin; additional mutations abolish trypsin cleavage.
To obtain unambiguous evidence that the Arg89His and Ser85Phe mutations alone were both necessary and sufficient to make prM susceptible to chymotrypsin cleavage in the context of an immature virion, the mutations were introduced by reverse genetics into the full-length cDNA clone of mutant prM(ΔR88). The resulting mutants were designated prM(ΔR88/S85F) and prM(ΔR88/R89H), as depicted in Fig. 1.
First, the cleavage status of protein prM in particles generated by these mutants and their susceptibility to cleavage by either chymotrypsin or trypsin were analyzed. RNAs of mutants prM(ΔR88/S85F), prM(ΔR88/R89H), and the original mutant prM(ΔR88) as well as wild-type virus RNA were synthesized by in vitro transcription of the appropriate full-length cDNA clones, and approximately equimolar amounts were introduced into BHK-21 cells by electroporation. Viral particles were harvested from the supernatants, and aliquots containing equal amounts of protein E were incubated with trypsin or chymotrypsin, or mock incubated and then subjected to SDS-polyacrylamide gel electrophoresis. Proteins prM and M were visualized by Western blot analysis using a polyclonal antibody that has previously been shown to recognize both prM and mature M (as well as an additional band believed to be an M dimer because its N-terminal sequence corresponds to that of the mature M protein) (49). As expected, the wild-type virus was found to contain primarily the mature M protein (Fig. 2A), which is generated by furin cleavage (1, 27, 56). In addition, the wild-type sample also contained a small proportion of uncleaved protein prM. In contrast, mutant prM(ΔR88) contained exclusively uncleaved protein prM and no protein M; i.e., all of the virus particles were in their immature state. The same was found to be the case for the two new mutants prM(ΔR88/S85F) and prM(ΔR88/R89H), which also exhibited only prM but no M bands (Fig. 2B).
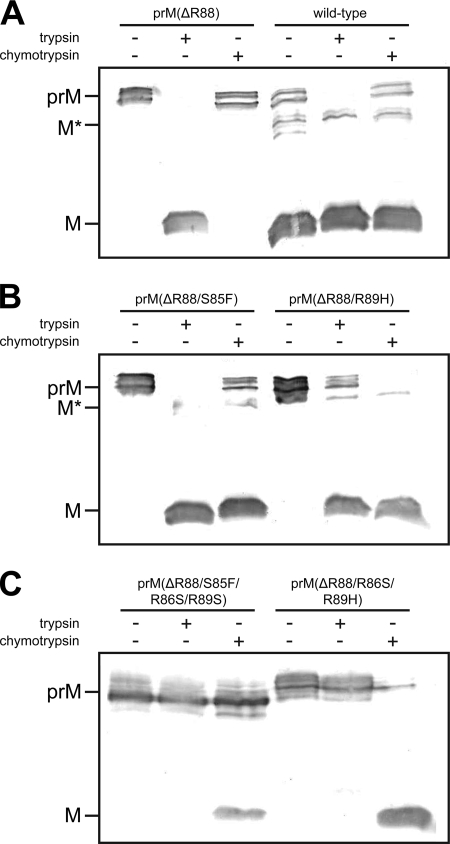
FIG. 2.
Processing of protein prM after in vitro protease treatment. BHK-21 cells were transfected with either wild-type and prM(ΔR88) (A), prM(ΔR88/S85F) and prM(ΔR88/R89H) (B), or prM(ΔR88/S85F/R86S/R89S) and prM(ΔR88/R86S/R89H) (C) RNAs. Cell culture supernatants were harvested 72 h later; samples were normalized by SDS-ELISA to a final concentration of 500 ng of protein E and incubated with PBS containing either 10 μg ml−1 trypsin or 10 μg ml−1 chymotrypsin as indicated. Processing of prM was then visualized by immunoblotting using a polyclonal serum raised against protein prM. M* refers to the putative M dimer (see text).
Incubation with trypsin significantly altered the prM cleavage status in the case of all four viruses, and in each case, protein prM was apparently converted to protein M. In mutants prM(ΔR88) and prM(ΔR88/S85F), the conversion was apparently very efficient as there was no residual prM band visible after trypsin treatment. Also in the case of the wild-type virus control, the band corresponding to residual protein prM that was not cleaved by furin disappeared as a consequence of trypsin treatment, whereas the M-dimer band, as expected, was not affected. In the case of mutant prM(ΔR88/R89H), protein prM was apparently converted to M, but this process appeared to be less efficient for this mutant, as indicated by the presence of a distinct band of still-uncleaved prM protein.
Incubation with chymotrypsin resulted in the cleavage of the prM proteins of both mutants, prM(ΔR88/S85F) and prM(ΔR88/R89H). As expected, no cleavage by chymotrypsin was observed in the cases of the original mutant, prM(ΔR88), and the residual prM band seen in the wild-type virus control also did not change after incubation with chymotrypsin. The cleavage patterns shown in Fig. 2 further suggest that chymotrypsin cleavage was more efficient in the case of mutant prM(ΔR88/R89H) than with mutant prM(ΔR88/S85F), where a distinct prM band remained visible in the chymotrypsin-treated sample.
From these data it was concluded that both the S85F and the R89H mutations conferred susceptibility to chymotrypsin cleavage to protein prM without affecting its susceptibility to trypsin cleavage, presumably due to the remaining Arg residues at or near to the cleavage site. Furthermore, it is interesting that cleavages predicted from the amino acid sequence to occur at the natural cleavage site after residue 89 overall appeared to be more efficient than those cleavages predicted to occur further upstream [as seen for mutant prM(ΔR88/R89H) incubated with trypsin, or mutant prM(ΔR88/S85F) incubated with chymotrypsin].
Mutants prM(ΔR88/S85F) and prM(ΔR88/R89H) contain two or one Arg residues, respectively, within the prM cleavage region (Fig. 1), and these residues may have been recognized by trypsin in the previous experiment. To test this, these Arg residues were changed to Ser by site-specific mutagenesis, thus generating two additional mutants termed prM(ΔR88/S85F/R86S/R89S) and prM(ΔR88/R86S/R89H) (Fig. 1). Mutant particles were produced, subjected to protease treatment, and analyzed by Western blotting as before. The results shown in Fig. 2C provide evidence that these mutants were indeed resistant to trypsin as no conversion of protein prM into M was observed upon incubation with this protease. Susceptibility to chymotrypsin was retained in these mutants although the conversion of protein prM to M appeared to be less efficient in the case of mutant prM(ΔR88/S85F/R86S/R89S) than with the parental mutant prM(ΔR88/S85F), and some uncleaved prM remained after treatment.
Proteolytic activation of infectivity in cell culture depends on cleavability of protein prM but also has additional constraints.
Having examined the sensitivity of each of our mutants to cleavage by trypsin or chymotrypsin, we wanted to analyze the correlation between cleavability and activation of infectivity in cell culture. Equimolar amounts of all mutant RNAs, including the previously characterized mutant prM-(ΔR88) as a control, were introduced by electroporation into BHK-21 cells. At day 1 posttransfection, cells were stained by indirect IFA with a polyclonal antibody directed against protein E. As shown in Fig. 3 (middle column), very similar staining patterns were observed at this time for all of the virus mutants. This indicates that the level of expression of viral proteins was approximately equal for all of the mutants, given that transfection efficiency is typically more than 90% in this experimental system and that viral spread is not yet detected at this time point. At the same time, the media of separate wells from the same transfections were supplemented with trypsin or chymotrypsin or left without exogenous protease. Three days posttransfection, aliquots from these cultures were transferred to inoculate naïve BHK-21 cells. Three days after that, infection of these cells was analyzed by IFA. As expected, no infection was detected in any of the samples that had not been supplemented with protease, confirming that all five of the mutants produced only immature, noninfectious virus particles (data not shown).
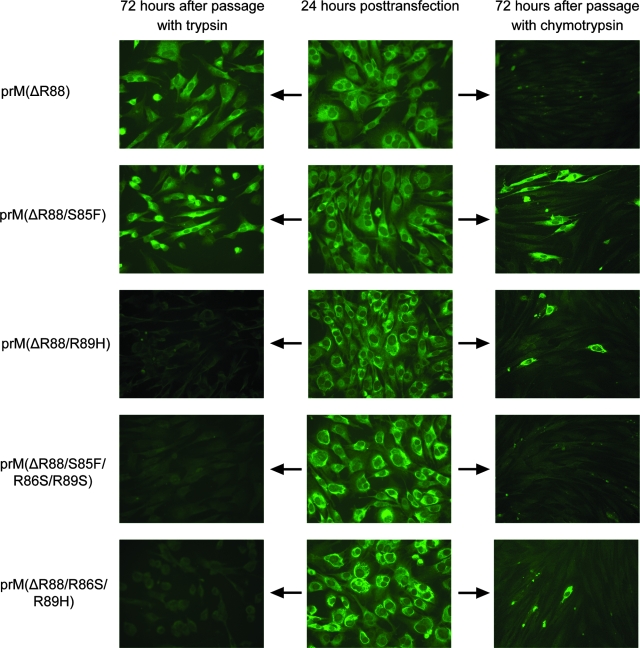
FIG. 3.
Activation of mutant viruses by exogenous proteases. BHK-21 cells were transfected with the indicated constructs, and either trypsin or chymotrypsin was added to the medium to a final concentration of 5 μg ml−1. After 72 h, supernatants were transferred to naïve BHK-21 cells as indicated by the arrows. Expression of protein E was monitored using an indirect IFA.
Samples to which the protease trypsin had been added yielded positive results in the cases of mutants prM(ΔR88) and prM(ΔR88/S85F) but were negative for the other three mutants (Fig. 3, left column). This result matched expectations in the cases of mutants prM(ΔR88) and prM(ΔR88/S85F) since the preceding experiments had shown that the prM proteins of these mutants were efficiently cleaved by trypsin. Moreover, the lack of activation observed for mutants prM(ΔR88/S85F/R86S/R89S) and prM(ΔR88/R86S/R89H) is in good agreement with the observed resistance of these mutants to trypsin cleavage. However, the negative result obtained for mutant prM(ΔR88/R89H) was surprising because some, albeit relatively inefficient, cleavage of prM by trypsin had been observed with this mutant (Fig. 2B). Several independent experiments confirmed the inability to activate mutant prM(ΔR88/R89H) with trypsin under our standard experimental conditions. Even inoculation of fresh cells with a threefold larger aliquot of supernatant after additional incubation with double the concentration of trypsin yielded only a very small number of isolated positive cells, and it was impossible to further propagate virus from these cultures (data not shown). Thus, it can be concluded that activation of mutant prM(ΔR88/R89H) with trypsin, in spite of the observed susceptibility of protein prM to cleavage, is very inefficient.
Samples that had been supplemented with chymotrypsin were successfully passaged in the cases of mutants prM(ΔR88/S85F), prM(ΔR88/R89H), and prM(ΔR88/R86S/R89H), but mutants prM(ΔR88) and prM(ΔR88/S85F/R86S/R89S) could not be passaged (Fig. 3, right column). This was consistent with the in vitro cleavage results, with the exception of mutant prM(ΔR88/S85F/R86S/R89S), which could not be activated despite its partial susceptibility to cleavage by chymotrypsin (Fig. 2C). Independent experiments applying more stringent cleavage conditions also did not result in activation of this mutant (data not shown).
The experiments described above confirm that cleavage of protein prM is necessary for activation of viral infectivity. However, prM cleavage may not always be sufficient, as exemplified by mutant prM(ΔR88/R89H) treated with trypsin and mutant prM(ΔR88/S85F/R86S/R89S) treated with chymotrypsin, suggesting that some mutants may face additional constraints.
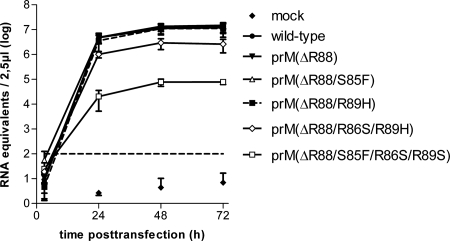
In an attempt to identify factors that restrict the viability of prM cleavage mutants, we set out to determine whether the mutations introduced into protein prM had an impact on fundamental parameters such as viral RNA replication, packaging, and release from cells. For this purpose, BHK-21 cells were transfected with equimolar amounts of either wild-type TBEV RNA or mutant RNA, and intracellular and extracellular RNA levels were monitored by quantitative PCR over a time period of 3 days. The determination of intracellular RNA levels revealed no significant differences in RNA replication efficiency between any of the mutants and the wild-type virus control (data not shown). However, extracellular RNA levels indicated significant differences in the rate of release of RNA-containing particles, as shown in Fig. 4. Whereas mutants prM(ΔR88), prM(ΔR88/S85F), and prM(ΔR88/R89H) were indistinguishable from the wild-type virus control with respect to RNA export, mutant prM(ΔR88/S85F/R86S/R89S) exhibited a severe defect, releasing at least 2 orders of magnitude less RNA at all time points. Mutant prM(ΔR88/R86S/R89H) also showed a reduced capacity for RNA release at days 2 and 3, but the impairment of this mutant was not as pronounced as that observed for mutant prM(ΔR88/S85F/R86S/R89S). Visual inspection of the cells by light microscopy indicated that mutant prM(ΔR88/R86S/R89H) and particularly mutant prM(ΔR88/S85F/R86S/R89S) were more cytotoxic than the other mutants or wild-type virus. This observation was confirmed by measurement of the enzymatic activity of lactate dehydrogenase in the supernatants, which gets released from disintegrating cells (data not shown). A deficiency in particle export has previously been observed to be linked with increased cytotoxicity of TBEV in BHK-21 cells (46).
FIG. 4.
RNA export kinetics of cleavage site mutants. The amount of viral RNA in cell culture supernatants of BHK-21 cells transfected with the indicated constructs was determined by real-time PCR. Values obtained for mock-transfected cells were below the cutoff value (102 RNA equivalents) at all time points. Values shown represent the mean of three independent experiments, each measured in duplicates. Error bars indicate the standard deviations.
Thus, it can be concluded that the additional mutations that were engineered into mutant prM(ΔR88/S85F/R86S/R89S) interfered with assembly and/or release of RNA-containing virus particles, and this deficiency is likely to be a major cause for the above-described failure to produce infectious prM(ΔR88/S85F/R86S/R89S) particles.
Neurovirulence in suckling mice correlates with the mutant's ability to be activated by trypsin, whereas chymotrypsin-dependent mutants cause no infection.
Suckling mice are highly susceptible for TBEV infection. It has been observed previously that intracranial inoculation is an approximately 100-fold more sensitive system for this virus than the usual cell culture (35). A trypsin-like protease activity capable of activating Sendai virus or influenza A virus was recently identified in rat brain (29). In a previous study, we demonstrated that mutant prM(ΔR88) has low-level infectivity upon intracranial inoculation of suckling mice (7).
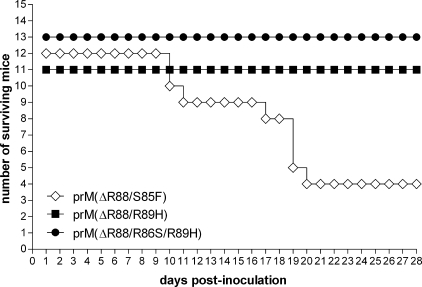
In order to investigate how activation in cell culture correlates with infectivity in vivo, litters of suckling mice were inoculated intracerebrally with cell culture supernatants containing equal amounts (based on E protein content) of mutants prM(ΔR88/S85F), prM(ΔR88/R89H), or prM(ΔR88/R86S/R89H). Mutant prM(ΔR88/S85F/R86S/R89S) was excluded from this and subsequent experiments due to its observed export defect and our inability to activate this mutant with any of the proteases. Mice were monitored for signs of neurological disease and survival over a period of 28 days. As shown in Fig. 5, mutant prM(ΔR88/S85F), which is readily activated by both trypsin and chymotrypsin, caused lethal infection in two-thirds of the animals, with a mean survival time of 15.6 ± 4.5 days. This result is similar to what was observed previously for mutant prM(ΔR88) (7). In that study, a similar infection experiment with mutant prM(ΔR88), which is activated by trypsin only, caused lethal infection in 34% of the animals with a mean survival time of 17.6 ± 3.6 days. In contrast, wild-type virus usually kills 100% of the animals within 7.2 (±1.5) days (35).
FIG. 5.
Neurovirulence of mutant viruses upon intracranial inoculation of suckling mice. Supernatants of transfected BHK-21 cells were normalized by SDS-ELISA to contain equal amounts of protein E (200 ng/ml). Survival of mice was monitored over a time period of 28 days.
In contrast, neither mutant prM(ΔR88/R89H) nor prM(ΔR88/R86S/R89H) killed any of the mice, suggesting that these mutants were unable to establish a productive infection in the brains of these animals. Both of these mutants are efficiently activated in cell culture by chymotrypsin but not by trypsin. Their apparent apathogenicity is in agreement with the presumption that there is no chymotrypsin-like proteolytic activity in brain tissue. Furthermore, this result is in good agreement with the observation that mutant prM(ΔR88/R89H), even though it is susceptible to cleavage by trypsin, cannot be activated efficiently by this protease. Serum samples drawn at the end of the observation period and analyzed for the presence of TBEV-specific antibody indicated no seroconversion for any of the mice inoculated with prM(ΔR88/R86S/R89H). However, one of the mice inoculated with mutant prM(ΔR88/R89H) had acquired TBEV-specific antibodies, suggesting that this mouse had succumbed to an abortive infection by this mutant.
One can conclude from these data that TBEV mutants that can be activated by trypsin in cell culture retain some infectivity in brain tissue probably due to the presence of a trypsin-like protease, but mutants that require chymotrypsin for activation are deficient for replication in tissues devoid of this protease, such as the brain.
Chymotrypsin-activated mutants remain genetically stable during multiple passages.
Next, we investigated whether the chymotrypsin-activated mutants were able to spontaneously acquire an altered phenotype, i.e., to increase viral fitness in the presence of this protease or revert to a chymotrypsin-independent phenotype. To analyze genetic stability, serial passage experiments in the presence of chymotrypsin were performed with mutants prM(ΔR88/S85F), prM(ΔR88/R89H), and prM(ΔR88/R86S/R89H), which can be activated by this protease. In parallel, wild-type virus was also passaged in the presence of chymotrypsin as a control. To increase selection pressure, passages were performed under limiting-dilution conditions; i.e., a log10 dilution series of supernatant from each round of infection was prepared and used for the next round of infection. Supernatant from the well inoculated with the highest dilution yielding a positive value in ELISA 3 days postinoculation was used for the subsequent round of infection.
These dilution experiments indicated that, in the presence of chymotrypsin, the three mutants typically could be detected in dilutions up to 105 and 107, whereas the wild-type control scored positive up to a dilution of 108 in ELISA, as is typical for TBEV after acquiring a heparan-sulfate-adapted phenotype in BHK-21 cell cultures (36). To better characterize the specific infectivity of the mutants in comparison with the wild-type virus, preparations standardized by quantitative PCR to contain equal numbers of RNA molecules (taken as a measurement for the number of virus particles) were incubated with chymotrypsin, and the endpoint dilution titers were determined on BHK-21 cells. Under these conditions, the specific infectivity of wild-type virus was found to be 103.5 particles per infectious unit (i.u.), whereas mutants prM(ΔR88/S85F) and prM(ΔR88/R89H) achieved values of 105 particles/i.u., and mutant prM(ΔR88/R86S/R89H) had a value of only 106.5 particles/i.u.
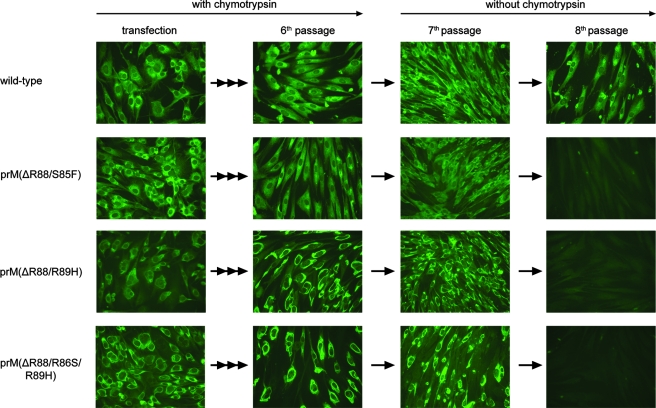
The limiting-dilution infection protocol was applied for six serial passages without noticeable changes in cytotoxicity or intracellular protein expression pattern, as monitored by IFA (Fig. 6), or protein export, monitored by ELISA (data not shown). In order to test whether any of the mutants had lost their dependency on chymotrypsin activation in the course of these passages, two subsequent passages using undiluted aliquots of supernatant as inocula were performed in the absence of protease. As also shown in Fig. 6, all three of the mutants were infectious for the first passage after removal of chymotrypsin but did not produce any infectious particles thereafter; i.e., they were single-round infectious. In contrast, the wild-type control had remained independent of chymotrypsin and could readily be carried through both of the passages in the absence of protease. Thus, there were no phenotypic changes observed in the course of this passaging experiment.
FIG. 6.
Infectivity of cleavage site mutants in cell culture. BHK-21 cells were transfected with wild-type or mutant RNAs as indicated on the left. Chymotrypsin was added to the cell culture medium to a final concentration of 5 μg ml−1. Supernatants were harvested 72 h posttransfection and transferred onto naïve BHK-21 cells. Every 3 to 4 days, supernatants were harvested and further passaged for a total of six times in the presence of exogenous chymotrypsin (as indicated at the top). The seventh and eighth passages were carried out in the absence of the protease.
To verify the genetic stability of the mutants, the RNA sequences coding for proteins prM and E were determined after the sixth passage by reverse transcription-PCR and found to be completely unchanged except for the commonly observed point mutations in protein E providing heparan-sulfate adaptation: E51K, E277K, and E122K for mutants prM(ΔR88/S85F), prM(ΔR88/R89H), and prM(ΔR88/R86S/R89H), respectively. Importantly, the modifications providing susceptibility to activation by chymotrypsin were found to be genetically stable.
DISCUSSION
This study describes the generation and characterization of prM cleavage mutants of TBEV. These mutants are activated by treatment with chymotrypsin and, when this protease is present in the medium, can be readily passaged in cell culture without reverting to the wild-type sequence or having other genotypic adaptations occur for at least six successive passages. These observations represent the first demonstration that flavivirus mutants that are activated by a heterologous protease with nonnatural cleavage specificity can be obtained and are genetically stable. Proteolytic activation of flaviviruses is naturally performed by the ubiquitous cellular protease furin (or related proteases) during a late stage of viral exocytosis (49). Previous studies had shown that cleavage of protein prM, which protects the fusion protein E from prematurely attaining fusion competence, is normally required for viral infectivity. A rare exception to that rule was described previously for TBEV: a pseudorevertant selected in mice exhibited a low level of infectivity even without prM cleavage, probably due to structural instability in the domain of prM that normally protects protein E from undergoing low-pH-induced conformational changes (7). Furthermore, it has been demonstrated that the addition of exogenous trypsin can substitute for furin cleavage (6). Trypsin cleaves after single basic amino acid residues, whereas furin requires a multibasic motif for cleavage. We now show that mutants can be selected that are activated by a protease which has a cleavage specificity very different from furin or trypsin. The mutants described in this study carry point mutations in protein prM that create new cleavage sites for chymotrypsin, a protease that is specific for amino acids with large, hydrophobic side chains, rather than basic residues, which are the only substrates recognized by furin and trypsin.
In order to generate such mutants, we chose to apply a selection approach in cell culture rather than to introduce specific mutations by reverse genetics based on theoretical considerations. A selection process provides room for the emergence of unexpected mutations which create optimal solutions under the particular growth conditions. Indeed, some properties of the mutants obtained here were surprising, as noted below.
In one case, a Phe residue was selected at position 85 of protein prM. While Phe is a typical substrate for chymotrypsin, the position of this selected mutation three residues upstream from the natural cleavage site was unexpected. Due to the absence of an atomic structure of this functionally important protein region, it is unknown which positions are both accessible to cleavage and able to initiate the large structural reorganization required for the conversion to infectious mature virus particles. Our results indicate that position 85 is both accessible to cleavage and appropriate for initiating the maturation process. In contrast, results obtained with mutant prM(ΔR88/R89H) treated with trypsin suggested that although cleavage at position 86 [which has the only basic residue that could serve as a potential substrate for trypsin in this region of mutant prM(ΔR88/R89H)] is also possible, this cleavage largely failed to render the virus infectious. Even extended cleavage conditions yielded only a minute level of infectivity. It is possible that the cleavage product interferes with structural rearrangements that are necessary for attaining infectivity. An alternative explanation may be that cleavage at position 86 results in a partial denaturation of the viral surface proteins that abolishes their functional integrity. In any case, although cleavage of protein prM was found to be necessary to attain infectivity in the cases of all of the mutants described in this study, the data also indicate that in some cases cleavage may not be sufficient to achieve functional activation.
In another case, a mutation was selected at the natural cleavage position, residue 89, but the amino acid was changed to a His residue, which is not a typical site for chymotrypsin cleavage. Apparently, however, this residue was readily recognized within the sequence context of the prM cleavage site.
In keeping with the notion that an evolutionary process driven by selection pressure may be more efficient than rational design, it is noteworthy that both mutations identified by the selection procedure provided phenotypes which were essentially unimpaired with respect to assembly and release of RNA-containing particles. In contrast, mutants carrying additional engineered mutations exhibited a degree of impairment of these functions. Apparently, this region of protein prM is quite sensitive to structural perturbations, and the introduction of inappropriate mutations is likely to be detrimental for the assembly and/or exocytosis of viral particles. Therefore, one can predict that major sequence changes in this region will not be easily tolerated by TBEV or other flaviviruses. Indeed, preliminary mutagenesis experiments aiming at engineering TBEV mutants containing potential cleavage sites for matrix metalloproteases or other heterologous proteases have so far produced only mutants with severely impaired release of viral particles, confirming the notion that this region is highly sensitive to structural perturbations (unpublished observations).
Activation of fusion competence, and thus viral infectivity, by a proteolytic cleavage event is commonly used by enveloped viruses. In general, there are two major pathways to proteolytic activation. First, the protein that mediates fusion itself gets cleaved and thus attains fusion competence. This mechanism is commonly used by class I fusion proteins. Second, an auxiliary protein, such as the flavivirus prM protein, is cleaved rather than the fusion protein, and this type of activation is seen in viruses with class II fusion proteins (30).
A well-studied example among the class I fusion proteins is the influenza virus hemagglutinin protein. There is ample evidence for the decisive role of the cleavage of the influenza hemagglutinin in determining the tissue tropism, pathogenicity, and virulence phenotype of this important pathogen (51). Strains of this virus that have a multibasic cleavage site that is recognized by furin, which is present in many cell types, can cause severe systemic infections and are highly pathogenic. In contrast, viruses with monobasic cleavage sites are cleaved only by trypsin-like proteases, which are present extracellularly in certain tissues such as the lung or the intestines. Consequently, viruses with monobasic sites tend to be less pathogenic and cause localized infections of these tissues. Moreover, influenza mutants with specificities for heterologous proteases such as elastase or chymotrypsin have been selected or engineered (42, 50). The highly restricted replication properties of these mutants in vivo may be used for the design of new live virus vaccines (8, 50). Similar to influenza virus, flaviviruses with restricted and defined tissue tropism may be generated by engineering mutants with specificity for various proteases. The data obtained for furin-deficient TBEV mutants described in this and a previous study have already shown that mutants that can be activated by trypsin retain a certain level of infectivity in the brain tissue of suckling mice, whereas mutants requiring chymotrypsin did not. These observations are in good agreement with the fact that trypsin-like protease activity, but not chymotrypsin, is likely to be present in brain tissues. It will be interesting to study further the tissue tropism of these mutants in vivo, in particular, their ability to replicate in the lung or the intestines.
Alphaviruses have a class II fusion protein (E1) that is structurally very similar to the flavivirus E protein. Its fusion competence is also attained by proteolytic cleavage of a second protein, but, in contrast to the flavivirus M protein, the protein that remains anchored in the viral membrane (E2) is relatively large, remains in heterodimeric association with the fusion protein E1, and mediates cellular attachment. Chymotrypsin-dependent mutants of the alphavirus Semliki Forest virus have been engineered and found to be very useful tools in a range of functional and structural studies as well as in the design of safe alphavirus-based gene delivery vectors (3, 18). The mutants described in this study open up similar avenues for the investigation of flaviviruses or the design of flavivirus-based vector systems.
Acknowledgments
We gratefully acknowledge contributions by Gabriel O'Riordain and the excellent technical assistance of Silvia Röhnke. We are indebted to Steven L. Allison for many helpful discussions and for his valuable assistance during the preparation of the manuscript.
This project was funded by a grant from the Austrian Fonds zur Förderung der wissenschaftlichen Forschung (FWF-P16376).
Footnotes
Published ahead of print on 18 June 2008.
REFERENCES
- 1.Allison, S. L., J. Schalich, K. Stiasny, C. W. Mandl, C. Kunz, and F. X. Heinz. 1995. Oligomeric rearrangement of tick-borne encephalitis virus envelope proteins induced by an acidic pH. J. Virol. 69695-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Allison, S. L., K. Stiasny, K. Stadler, C. W. Mandl, and F. X. Heinz. 1999. Mapping of functional elements in the stem-anchor region of tick-borne encephalitis virus envelope protein E. J. Virol. 735605-5612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berglund, P., M. Sjoberg, H. Garoff, G. J. Atkins, B. J. Sheahan, and P. Liljestrom. 1993. Semliki Forest virus expression system: production of conditionally infectious recombinant particles. Biotechnology 11916-920. [DOI] [PubMed] [Google Scholar]
- 4.Bredenbeek, P. J., E. A. Kooi, B. Lindenbach, N. Huijkman, C. M. Rice, and W. J. Spaan. 2003. A stable full-length yellow fever virus cDNA clone and the role of conserved RNA elements in flavivirus replication. J. Gen. Virol. 841261-1268. [DOI] [PubMed] [Google Scholar]
- 5.Earp, L. J., S. E. Delos, H. E. Park, and J. M. White. 2005. The many mechanisms of viral membrane fusion proteins. Curr. Top. Microbiol. Immunol. 28525-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elshuber, S., S. L. Allison, F. X. Heinz, and C. W. Mandl. 2003. Cleavage of protein prM is necessary for infection of BHK-21 cells by tick-borne encephalitis virus. J. Gen. Virol. 84183-191. [DOI] [PubMed] [Google Scholar]
- 7.Elshuber, S., and C. W. Mandl. 2005. Resuscitating mutations in a furin cleavage-deficient mutant of the flavivirus tick-borne encephalitis virus. J. Virol. 7911813-11823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gabriel, G., H. Garn, M. Wegmann, H. Renz, A. Herwig, H. D. Klenk, and J. Stech. 2008. The potential of a protease activation mutant of a highly pathogenic avian influenza virus for a pandemic live vaccine. Vaccine 26956-965. [DOI] [PubMed] [Google Scholar]
- 9.Gordon, V. M., K. R. Klimpel, N. Arora, M. A. Henderson, and S. H. Leppla. 1995. Proteolytic activation of bacterial toxins by eukaryotic cells is performed by furin and by additional cellular proteases. Infect. Immun. 6382-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guirakhoo, F., F. X. Heinz, C. W. Mandl, H. Holzmann, and C. Kunz. 1991. Fusion activity of flaviviruses: comparison of mature and immature (prM-containing) tick-borne encephalitis virions. J. Gen. Virol. 721323-1329. [DOI] [PubMed] [Google Scholar]
- 11.Hallenberger, S., V. Bosch, H. Angliker, E. Shaw, H. D. Klenk, and W. Garten. 1992. Inhibition of furin-mediated cleavage activation of HIV-1 glycoprotein gp160. Nature 360358-361. [DOI] [PubMed] [Google Scholar]
- 12.Harrison, S. C. 2005. Mechanism of membrane fusion by viral envelope proteins. Adv. Virus Res. 64231-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hatsuzawa, K., K. Murakami, and K. Nakayama. 1992. Molecular and enzymatic properties of furin, a Kex2-like endoprotease involved in precursor cleavage at Arg-X-Lys/Arg-Arg sites. J. Biochem. 111296-301. [DOI] [PubMed] [Google Scholar]
- 14.Hayasaka, D., T. S. Gritsun, K. Yoshii, T. Ueki, A. Goto, T. Mizutani, H. Kariwa, T. Iwasaki, E. A. Gould, and I. Takashima. 2004. Amino acid changes responsible for attenuation of virus neurovirulence in an infectious cDNA clone of the Oshima strain of tick-borne encephalitis virus. J. Gen. Virol. 851007-1018. [DOI] [PubMed] [Google Scholar]
- 15.Heinz, F. X., C. Mandl, R. Berger, W. Tuma, and C. Kunz. 1984. Antibody-induced conformational changes result in enhanced avidity of antibodies to different antigenic sites on the tick-borne encephalitis virus glycoprotein. Virology 13325-34. [DOI] [PubMed] [Google Scholar]
- 16.Heinz, F. X., K. Stiasny, G. Puschner-Auer, H. Holzmann, S. L. Allison, C. W. Mandl, and C. Kunz. 1994. Structural changes and functional control of the tick-borne encephalitis virus glycoprotein E by the heterodimeric association with protein prM. Virology 198109-117. [DOI] [PubMed] [Google Scholar]
- 17.Heinz, F. X., W. Tuma, F. Guirakhoo, and C. Kunz. 1986. A model study of the use of monoclonal antibodies in capture enzyme immunoassays for antigen quantification exploiting the epitope map of tick-borne encephalitis virus. J. Biol. Stand. 14133-141. [DOI] [PubMed] [Google Scholar]
- 18.Jain, S. K., S. DeCandido, and M. Kielian. 1991. Processing of the p62 envelope precursor protein of Semliki Forest virus. J. Biol. Chem. 2665756-5761. [PubMed] [Google Scholar]
- 19.Kandolf, R., and P. H. Hofschneider. 1985. Molecular cloning of the genome of a cardiotropic coxsackie B3 virus: full-length reverse-transcribed recombinant cDNA generates infectious virus in mammalian cells. Proc. Natl. Acad. Sci. USA 824818-4822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kapoor, M., L. Zhang, P. M. Mohan, and R. Padmanabhan. 1995. Synthesis and characterization of an infectious dengue virus type-2 RNA genome (New Guinea C strain). Gene 162175-180. [DOI] [PubMed] [Google Scholar]
- 21.Khromykh, A. A., and E. G. Westaway. 1994. Completion of Kunjin virus RNA sequence and recovery of an infectious RNA transcribed from stably cloned full-length cDNA. J. Virol. 684580-4588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kinney, R. M., S. Butrapet, G. J. Chang, K. R. Tsuchiya, J. T. Roehrig, N. Bhamarapravati, and D. J. Gubler. 1997. Construction of infectious cDNA clones for dengue 2 virus: strain 16681 and its attenuated vaccine derivative, strain PDK-53. Virology 230300-308. [DOI] [PubMed] [Google Scholar]
- 23.Klenk, H. D., and W. Garten. 1994. Host cell proteases controlling virus pathogenicity. Trends Microbiol. 239-43. [DOI] [PubMed] [Google Scholar]
- 24.Klimpel, K. R., S. S. Molloy, G. Thomas, and S. H. Leppla. 1992. Anthrax toxin protective antigen is activated by a cell surface protease with the sequence specificity and catalytic properties of furin. Proc. Natl. Acad. Sci. USA 8910277-10281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kofler, R. M., V. M. Hoenninger, C. Thurner, and C. W. Mandl. 2006. Functional analysis of the tick-borne encephalitis virus cyclization elements indicates major differences between mosquito-borne and tick-borne flaviviruses. J. Virol. 804099-4113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kroschewski, H., S. L. Allison, F. X. Heinz, and C. W. Mandl. 2003. Role of heparan sulfate for attachment and entry of tick-borne encephalitis virus. Virology 30892-100. [DOI] [PubMed] [Google Scholar]
- 27.Kuhn, R. J., W. Zhang, M. G. Rossmann, S. V. Pletnev, J. Corver, E. Lenches, C. T. Jones, S. Mukhopadhyay, P. R. Chipman, E. G. Strauss, T. S. Baker, and J. H. Strauss. 2002. Structure of dengue virus: implications for flavivirus organization, maturation, and fusion. Cell 108717-725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lai, C. J., B. T. Zhao, H. Hori, and M. Bray. 1991. Infectious RNA transcribed from stably cloned full-length cDNA of dengue type 4 virus. Proc. Natl. Acad. Sci. USA 885139-5143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Le, T. Q., M. Kawachi, H. Yamada, M. Shiota, Y. Okumura, and H. Kido. 2006. Identification of trypsin I as a candidate for influenza A virus and Sendai virus envelope glycoprotein processing protease in rat brain. Biol. Chem. 387467-475. [DOI] [PubMed] [Google Scholar]
- 30.Lescar, J., A. Roussel, M. W. Wien, J. Navaza, S. D. Fuller, G. Wengler, G. Wengler, and F. A. Rey. 2001. The fusion glycoprotein shell of Semliki Forest virus: an icosahedral assembly primed for fusogenic activation at endosomal pH. Cell 105137-148. [DOI] [PubMed] [Google Scholar]
- 31.Lindenbach, B. D., and C. M. Rice. 2001. Flaviviridae: the viruses and their replication, p. 991-1041. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 4th ed. Lippincott Williams & Wilkins, Philadelphia, PA.
- 32.Mandl, C. W., M. Ecker, H. Holzmann, C. Kunz, and F. X. Heinz. 1997. Infectious cDNA clones of tick-borne encephalitis virus European subtype prototypic strain Neudoerfl and high virulence strain Hypr. J. Gen. Virol. 781049-1057. [DOI] [PubMed] [Google Scholar]
- 33.Mandl, C. W., F. X. Heinz, and C. Kunz. 1988. Sequence of the structural proteins of tick-borne encephalitis virus (Western subtype) and comparative analysis with other flaviviruses. Virology 166197-205. [DOI] [PubMed] [Google Scholar]
- 34.Mandl, C. W., F. X. Heinz, E. Stockl, and C. Kunz. 1989. Genome sequence of tick-borne encephalitis virus (Western subtype) and comparative analysis of nonstructural proteins with other flaviviruses. Virology 173291-301. [DOI] [PubMed] [Google Scholar]
- 35.Mandl, C. W., H. Holzmann, T. Meixner, S. Rauscher, P. F. Stadler, S. L. Allison, and F. X. Heinz. 1998. Spontaneous and engineered deletions in the 3′ noncoding region of tick-borne encephalitis virus: construction of highly attenuated mutants of a flavivirus. J. Virol. 722132-2140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mandl, C. W., H. Kroschewski, S. L. Allison, R. Kofler, H. Holzmann, T. Meixner, and F. X. Heinz. 2001. Adaptation of tick-borne encephalitis virus to BHK-21 cells results in the formation of multiple heparan sulfate binding sites in the envelope protein and attenuation in vivo. J. Virol. 755627-5637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Molloy, S. S., E. D. Anderson, F. Jean, and G. Thomas. 1999. Bi-cycling the furin pathway: from TGN localization to pathogen activation and embryogenesis. Trends Cell Biol. 928-35. [DOI] [PubMed] [Google Scholar]
- 38.Molloy, S. S., P. A. Bresnahan, S. H. Leppla, K. R. Klimpel, and G. Thomas. 1992. Human furin is a calcium-dependent serine endoprotease that recognizes the sequence Arg-X-X-Arg and efficiently cleaves anthrax toxin protective antigen. J. Biol. Chem. 26716396-16402. [PubMed] [Google Scholar]
- 39.Moulard, M., and E. Decroly. 2000. Maturation of HIV envelope glycoprotein precursors by cellular endoproteases. Biochim. Biophys. Acta 1469121-132. [DOI] [PubMed] [Google Scholar]
- 40.Murray, J. M., J. G. Aaskov, and P. J. Wright. 1993. Processing of the dengue virus type 2 proteins prM and C-prM. J. Gen. Virol. 74175-182. [DOI] [PubMed] [Google Scholar]
- 41.Nakayama, K. 1997. Furin: a mammalian subtilisin/Kex2p-like endoprotease involved in processing of a wide variety of precursor proteins. Biochem. J. 327625-635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Orlich, M., D. Linder, and R. Rott. 1995. Trypsin-resistant protease activation mutants of an influenza virus. J. Gen. Virol. 76625-633. [DOI] [PubMed] [Google Scholar]
- 43.Pryor, M. J., R. C. Gualano, B. Lin, A. D. Davidson, and P. J. Wright. 1998. Growth restriction of dengue virus type 2 by site-specific mutagenesis of virus-encoded glycoproteins. J. Gen. Virol. 792631-2639. [DOI] [PubMed] [Google Scholar]
- 44.Rice, C. M., A. Grakoui, R. Galler, and T. J. Chambers. 1989. Transcription of infectious yellow fever RNA from full-length cDNA templates produced by in vitro ligation. New Biol. 1285-296. [PubMed] [Google Scholar]
- 45.Salminen, A., J. M. Wahlberg, M. Lobigs, P. Liljestrom, and H. Garoff. 1992. Membrane fusion process of Semliki Forest virus. II. Cleavage-dependent reorganization of the spike protein complex controls virus entry. J. Cell Biol. 116349-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schrauf, S., P. Schlick, T. Skern, and C. W. Mandl. 2008. Functional analysis of potential carboxy-terminal cleavage sites of tick-borne encephalitis virus capsid protein. J. Virol. 822218-2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Shi, P. Y., M. Tilgner, M. K. Lo, K. A. Kent, and K. A. Bernard. 2002. Infectious cDNA clone of the epidemic West Nile virus from New York City. J. Virol. 765847-5856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Skehel, J. J., and D. C. Wiley. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69531-569. [DOI] [PubMed] [Google Scholar]
- 49.Stadler, K., S. L. Allison, J. Schalich, and F. X. Heinz. 1997. Proteolytic activation of tick-borne encephalitis virus by furin. J. Virol. 718475-8481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stech, J., H. Garn, M. Wegmann, R. Wagner, and H. D. Klenk. 2005. A new approach to an influenza live vaccine: modification of the cleavage site of hemagglutinin. Nat. Med. 11683-689. [DOI] [PubMed] [Google Scholar]
- 51.Steinhauer, D. A. 1999. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 2581-20. [DOI] [PubMed] [Google Scholar]
- 52.Stiasny, K., S. L. Allison, A. Marchler-Bauer, C. Kunz, and F. X. Heinz. 1996. Structural requirements for low-pH-induced rearrangements in the envelope glycoprotein of tick-borne encephalitis virus. J. Virol. 708142-8147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stieneke-Grober, A., M. Vey, H. Angliker, E. Shaw, G. Thomas, C. Roberts, H. D. Klenk, and W. Garten. 1992. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 112407-2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sumiyoshi, H., C. H. Hoke, and D. W. Trent. 1992. Infectious Japanese encephalitis virus RNA can be synthesized from in vitro ligated cDNA templates. J. Virol. 665425-5431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Volchkov, V. E., H. Feldmann, V. A. Volchkova, and H. D. Klenk. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc. Natl. Acad. Sci. USA 955762-5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wengler, G., and G. Wengler. 1989. Cell-associated West Nile flavivirus is covered with E+pre-M protein heterodimers which are destroyed and reorganized by proteolytic cleavage during virus release. J. Virol. 632521-2526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yun, S. I., S. Y. Kim, C. M. Rice, and Y. M. Lee. 2003. Development and application of a reverse genetics system for Japanese encephalitis virus. J. Virol. 776450-6465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zhang, X., M. Fugere, R. Day, and M. Kielian. 2003. Furin processing and proteolytic activation of Semliki Forest virus. J. Virol. 772981-2989. [DOI] [PMC free article] [PubMed] [Google Scholar]