Abstract
Adaptation of avian influenza viruses for replication and transmission in the human host is believed to require mutations in the hemagglutinin glycoprotein (HA) which enable binding to human α2-6 sialosides and concomitant reduction in affinity for avian α2-3 linked sialosides. Here, we show by glycan microarray analyses that the two mutations responsible for such specificity changes in 1957 H2N2 and 1968 H3N2 pandemic viruses, when inserted into recombinant HAs or intact viruses of some recent avian H5N1 isolates (clade 2.2), impart such attributes. This propensity to adapt to human receptors is primarily dependent on arginine at position 193 within the receptor binding site, as well as loss of a vicinal glycosylation site. already have Widespread occurrence of these susceptible H5N1 clade 2.2 influenza strains has already occurred in Europe, the Middle East, and Africa. Thus, these avian strains should be considered ‘high-risk’, because of their significantly lower threshold for acquiring human receptor specificity and, therefore, warrant increased surveillance and further study.
Keywords: Influenza, glycan array, hemagglutinin, receptor specificity, H5N1
Introduction
The H5N1 avian influenza virus is now firmly established on three continents and is threatening further globalization in the coming months/years. The ongoing concern is whether the avian H5N1 virus will evolve to allow efficient human-to-human transmission, which could potentially initiate a deadly pandemic. The hemagglutinins (HAs) of avian H5N1 viruses can be currently separated into ten distinct phylogenetic clades (0 to 9).1 Due to increased diversity, clade 2 viruses were recently further sub-divided into 5 second-order clades (clades 2.1 to 2.5). The HAs of avian H5N1 viruses that have infected humans since 2003 can be grouped essentially into only two of these phylogenetic clades. Clade 1 viruses, isolated mainly in China, Cambodia, Thailand and Vietnam, were responsible for most documented human infections in Asia during 2004 to 2005 and in Thailand during 2006. Clade 2 viruses, present in birds in China and Indonesia during 2003–2004, then began to spread westwards during 2005 and reached the Middle East, Europe and Africa in 2006. Significantly, these latter clade 2 viruses have been responsible for most human infections since late 2005 (Figure 1 and Table 1). 2; 3 The likelihood that the H5N1 virus can cause a pandemic in humans by reassortment with current human viruses, as demonstrated for the H2 and H3 pandemics in 1957 and 1968, is the subject of ongoing debate.4–6 Direct adaptation to humans is more challenging for the virus since it must acquire the ability not only to enter, but also efficiently replicate in the critical upper airway cells of the new host, involving optimization of many steps in viral replication. The virus must also be transmissible from human-to-human to spread in the population which is a distinct property from entry and replication. Although a number of factors determine host range restriction and pathogenicity 7, a recent study of the 1918 pandemic virus in a ferret model highlighted the receptor specificity of the influenza hemagglutinin (HA) as a critical determinant.8 Recent in vitro investigations of certain HA mutations on the H5N1 virus receptor binding also suggest the critical role of receptor specificity in infection of the upper human airway.9–14
Fig. 1.
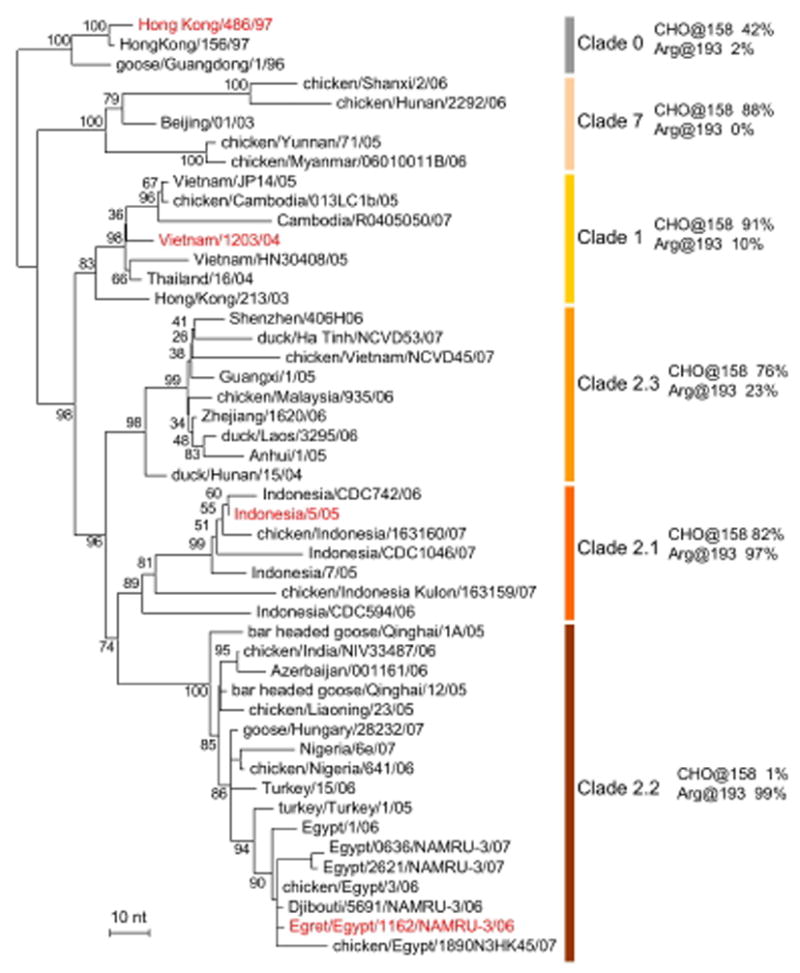
Phylogenetic tree of selected hemagglutinin genes from H5N1 viruses. Phylogenetic trees were inferred from nucleotide sequences by the neighbor-joining method. The lengths of the horizontal lines are proportional to the numbers of nucleotide differences, as indicated by the scale bars. Bootstrap analysis values >90% are shown. The numerical fractions denote the frequency of the specified amino acids in each clade among all H5 HAs of the Goose/Guangdong/96 (H5N1) lineage available in public databases. Strains used in this study are highlighted in red text, and all but the Egret06 virus were isolates from humans infected by H5N1 avian viruses. Only clades whose viruses have infected humans are shown. For a full tree, readers should consult reference 1 or the WHO website.
Table 1.
Phylogenetic origin of H5N1 viruses from confirmed human infections. Numbers relect only laboratory-confirmed cases reported to WHO, and does not include the 2003 single clade 7 infection from China.
| H5N1 clade | 2004 | 2005 | 2006 | 2007 | 2008* |
|---|---|---|---|---|---|
| Clade 1 | 44 | 35 | 5 | 1 | 0 |
| Clade 2 | 0 | 31 | 95 | 77 | 10 |
Totals as of February 2nd, 2008.
A characteristic of human influenza viruses is a pronounced preference for binding to α2-6 linked sialic acids, while avian viruses recognize receptors with α2-3 linked sialic acids. Several reports have documented mutants of H5N1 that have some modest affinity for α2-6 sialic acids11–13. However, these reports only studied viruses from clade 1 and, although different assay methods were used, a consistent feature of these mutants is that they still retained predominant avian-type specificity for α2-3 linked sialic acids.11–13 In this report, we have analyzed recent avian H5N1 viruses from different evolutionary clades that have been reported to infect humans and assess their propensity to acquire human receptor specificity. Our studies have focused on Clade 1 and Clade 2.1 and 2.2 viruses because these clades have been responsible for >90% of the human infections since 2003. We have used glycan array analyses 9–11; 15, covering a wide range of natural sialosides (Table 2) to compare and contrast the receptor binding capabilities of natural and mutated avian influenza viruses, both as recombinant HAs (rHAs) 11; 16, and as corresponding viruses produced by reverse genetics.17–19
Table 2.
Sialic acid-linked glycans represented on the glycan microarray. The table is color coded according to Figures 2, 3, 4, and 6.
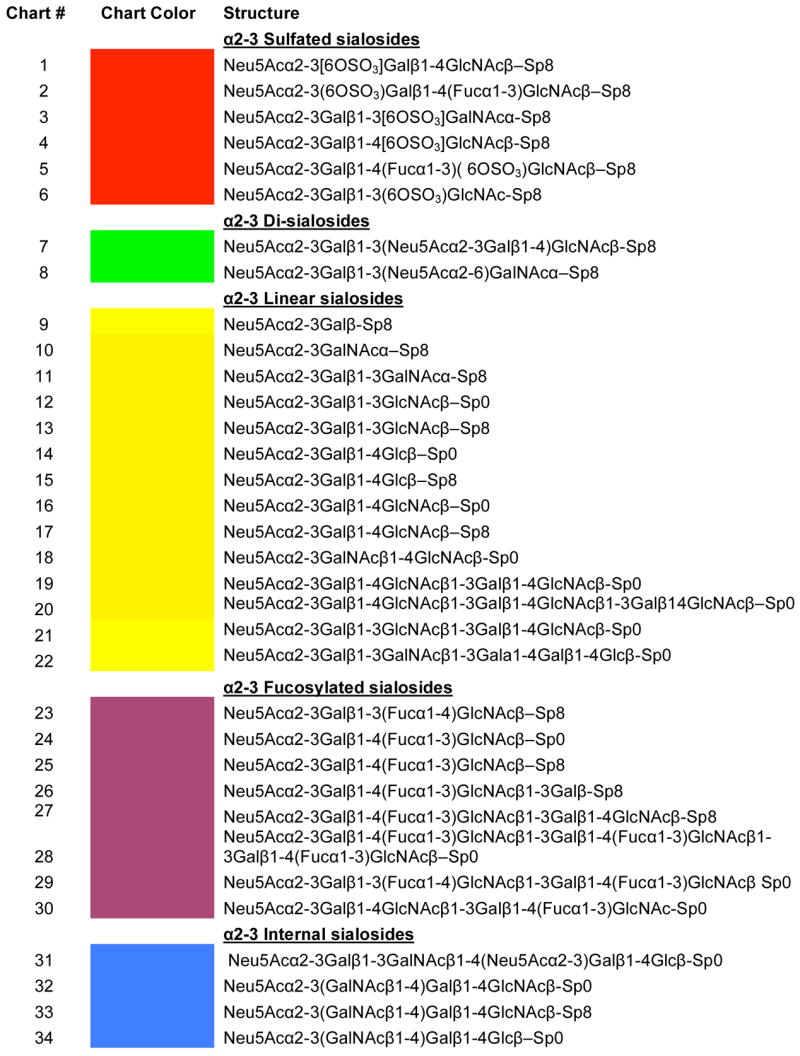
| ||
|
Key: Neu5Ac = Sialic acid; OSO3 = sulfate; Gal = galactose; Fuc = fucose; GlcNAc = N-Acectyl-D-glucosamine; GalNAc = N-acetyl-D-galactosamine; Glc = glucose; Man = mannose; SP0 = -(CH2)2-NH2; SP8 = -(CH2)3-NH2; SP9 = -(CH2)5-NH2; SP10 = -NHCOCH2NH2; G = Glycine.
Results
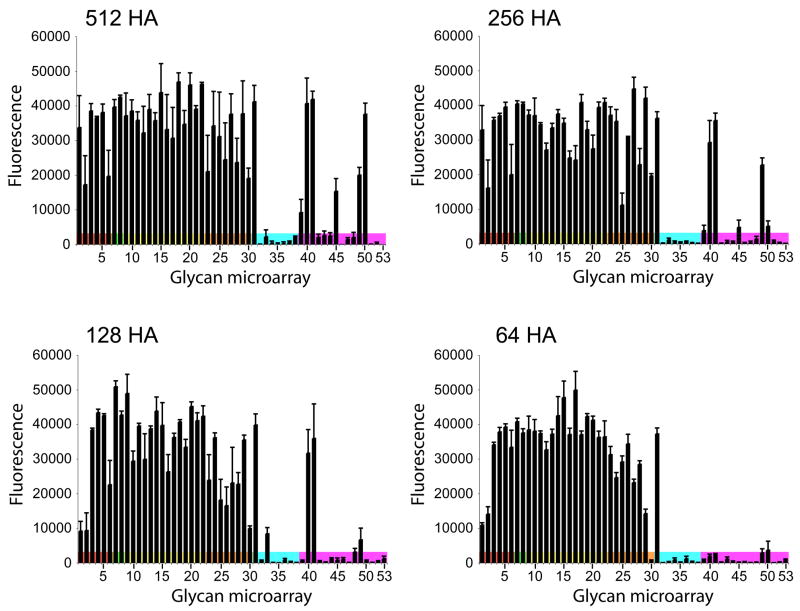
We selected diverse representative hemagglutinins from the different clades of circulating avian H5N1 influenza viruses isolated from humans. To compare results of different virus preparations on glycan microarrays, optimization experiments revealed that it is necessary to use comparable HA titers since high viral titers lead to signal saturation of strong binders and exaggerates the signals (and the physiological/biological relevance) for weak binding glycans, while suboptimal titers only detect binding to high affinity ligands (Figure 2). How effectively a virus binds to the representative glycans can be tested by assaying at different virus dilutions. As seen for A/Vietnam/1203/2004 (Viet04; Figure 2), this virus has a strong preference to bind α2-3 sialosides, but weak binding to certain α2-6 sialosides, including biantennary (#40, 41) and long chain (#49, 50) glycans, is revealed as virus titers are increased (128 to 512). Dilution to a HA titer of 64 resulted in complete loss of the α2-6 signals, while binding to the α2-3 glycans is minimally affected. Each experiment, therefore, requires careful titration of the virus on the array to derive meaningful data. In our experiments, an HA titer of 128 appeared to be optimal for comparison of receptor specificity, and produces sufficient binding to evaluate receptor specificity without saturation of signals to high affinity glycans and exaggeration of signals to lower affinity glycans.
Fig. 2.
Assessment of viral dilutions on detection of sialoside ligands on the glycan microarray. Examples of the dilution series performed on the glycan microarray for virus suspensions. Viet04 wild type was analyzed in 2-fold serial dilutions for hemagglutination (HA) titers ranging from 512 to 64.
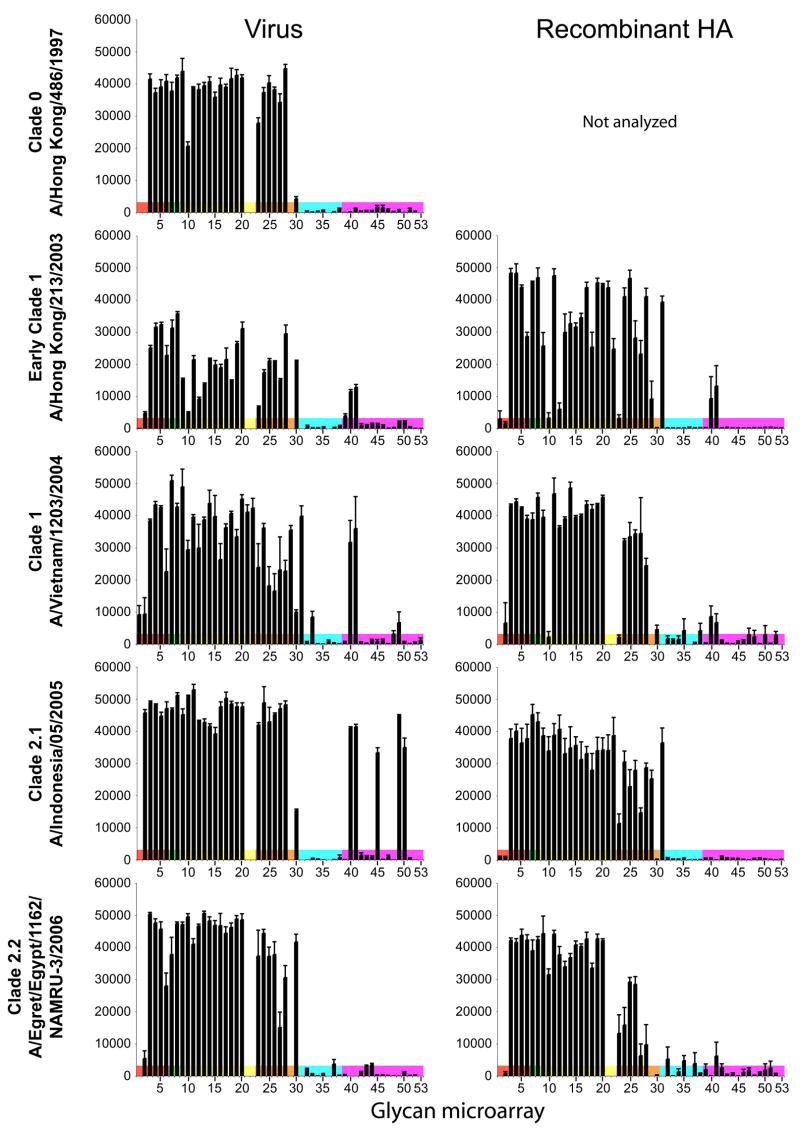
Representatives from a number of clades were analyzed (Figure 3). The Clade 0, A/Hong Kong/486/1997 virus is one of the original (progenitor) H5N1 viruses (Row 1). Between 1997 and 2003, no human infections were recorded. From 2003, the viruses sampled corresponded to an early clade 1 strain: A/Hong Kong/213/2003 (HK213; row 2); a later clade 1 strain: A/Vietnam/1203/2004 (Viet04; row 3); a clade 2.1 strain: A/Indonesia/05/2005 (Indo05; row 4), and a more recent clade 2.2 avian isolate: A/Egret/Egypt/1162/NAMRU-3/2006 (Eret06; row 5). As anticipated, experiments with both H5 virus and recombinant protein revealed HA bound extensively to the panel of α2-3 glycans (Figure 3). However, all assays with the HK213 and Viet04 viruses (both clade 1), as well as A/Indonesia/05/2005 (Indo05; clade 2.1), revealed some additional, albeit less extensive, binding to α2-6 sialosides, in particular to biantennary glycans (#40, 41 in Figure 3). Furthermore the A/Hong Kong/213/2003 (HK213) strain was of particular interest because a previous study reported an increase in human-type α2-6 specificity and identified a Ser227Asn mutation as a possible cause.20 However, our results suggest no increase in α2-6 binding for this particular strain. Glycan microarray analyses of A/Vietnam/1203/2004 (Viet04) and HK213 viruses revealed similar binding profiles with specific interaction of HK213 only to α2-6 biantennary structures (#40, 41) (Figure 3). A/Indonesia/05/2005 (Indo05) also had similar binding profiles, but with enhanced binding to several monovalent α2-6 sialosides, including 6′-sialylactose (#45) and long chain sialosides (#49, 50)(Figure 3). Only the clade 0 human virus, A/Hong Kong/486/1997 (HK486) and the clade 2.2 Egyptian virus, A/Egret/Egypt/1162/NAMRU-3/2006 (Egret06), isolated from an egret, failed to bind to α2-6 sialosides.
Fig. 3.
Comparison of receptor specificity of representative H5N1 viruses (column 1) and corresponding recombinant HAs (column 2) using a glycan microarray. A number of HAs from 1997 to 2005 isolated from human infections were analyzed and compared. Viruses were analyzed at a HA titer of 128 per 50μl while 15 μg of recombinant HA was used for the complementary analysis. Binding to different categories of glycans on the array are highlighted as follows: red, α2-3 sulfated; green, α2-3 di-sialylated, yellow, linear α2-3 sialosides; orange, fucosylated α2-3 sialosides; blue, α2-3 internal sialosides; and pink α2-6 ligands in same order as listed for the α2-3 sialosides (see Table 2 for name list and structures). Because additional glycans were added to the microarrays during the course of this study, glycans # 1, 21, 22, 29, 31, 36 and 53 are absent on certain graphs.
H2/H3 adaptive mutations
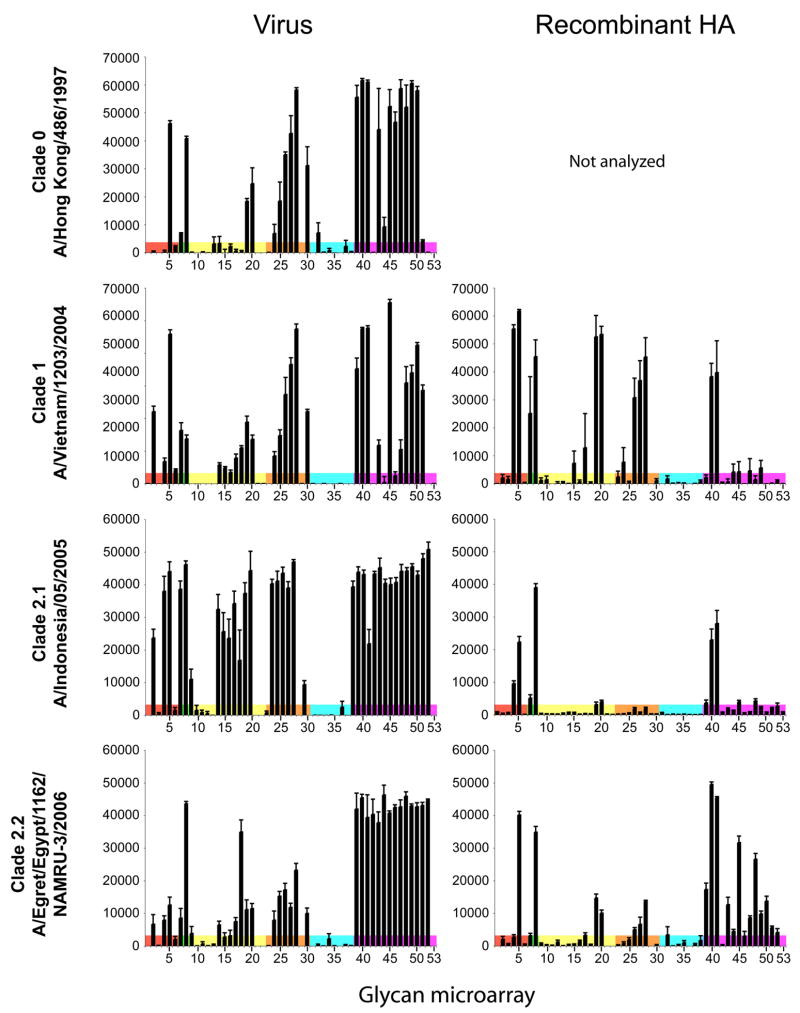
The previous two human influenza pandemics in 1957 and 1968 resulted from introduction of avian virus hemagglutinins, H2 and H3 respectively, into the currently circulating human virus population by gene reassortment. In each case, the HAs adapted to human-type receptor specificity through two amino acid mutations in the receptor binding pocket (Gln226Leu, Gly228Ser; LS).21; 22 In our earlier studies on the Viet04 strain (clade 1), one of the most highly pathogenic strains in ferret and mouse models 23; 24, we studied the effect of these mutations, as well as 190/225 mutations found to switch receptor specificity in H1N1 viruses, and only the introduction of H2/H3 mutations into the recombinant H5 HA resulted in reduced α2-3 binding, and facilitated a relatively modest interaction with α2-6 biantennary glycans.11 To further investigate the potential for such mutations to adapt the H5 HA to human-type receptor specificity, we have now evaluated the effect of these same mutations in viruses that represent more recent clades. Mutant viruses were generated by reverse genetics, as well as their corresponding rHAs using a baculovirus expression system, from clade 0 (HK486-LS), clade 1 (Viet04-LS), 2.1 (Indo05-LS from clade 2.1) and clade 2.2 (Egret06-LS) viruses and all were analyzed on the glycan microarray.
For avian viruses to adapt for efficient human-to-human transmission, it is thought that mutations in the HA are required that can simultaneously decrease α2-3 binding, while increasing α2-6 specificity.25 For the recombinant HA experiments (Figure 4, right column), introduction of H2 and H3 serotype mutations (Gln226Leu, Gly228Ser) produced a significant reduction in α2-3 binding, when compared to their wild-type counterparts (Figure 3). For α2-6 binding, however, a highly significant increase was only observed for clade 2.2 Egret06-LS, where binding to a greater range of α2-6 sialosides was apparent compared to the highly restricted interaction for clade 1 and 2.1 HAs with biantennary sugars (#40, 41). For intact viruses, a similar pattern was noted, with Egret06-LS again showing the most significant increase in binding to human-type α2-6 receptors and concomitant decrease in interaction with avian-type α2-3 receptors (Figure 4, left column). Gln226Leu/Gly228Ser mutations into the progenitor H5N1 virus (A/Hong Kong/486/1997) resulted in a binding profile similar to Viet04-LS with dual α2-3/α2-6 specificity (Figure 4, left column). The predominant binding to avian type receptors appeared to be for fucosylated α2-3 sialosides with the sialyl-Lewis X structure (NeuAcα2-3Galβ1-4(Fucα1-3)GlcNAc- (#24-28), although linear, long-chain sialosides were also bound (#19, 20, 30).
Fig. 4.
Impact of LS mutations propensities of recent H5N1 isolates to bind human-type receptors. Mutations responsible for adaptation of the 1968 H3 pandemic strain (Gln226Leu, Gly228Ser) to human-type receptor specificity were introduced into H5N1 viruses by reverse genetics (column 1) and the corresponding recombinant HAs (column 2). Mutations in the clade 1 strain, A/Vietnam/1203/2004 (Row 2) and a clade 2.1 strain; A/Indonesia/05/2005 (Row 3) both show reduced avian α2-3 specificity, and acquire weak binding to α2-6 glycans, in particular to α2-6 biantennary glycans (#40, 41). Most striking is the effect of the same mutations on the clade 2.2 avian virus, A/Egret/Egypt/1162/NAMRU-3/2006 (row 4), which shows substantially reduced avian α2-3 specificity, and significant binding to a wide spectrum of α2-6 glycans. Virus and recombinant HAs were analyzed as in Figure 3.
Clade-specific differences
Until recently, viruses circulating since 2003 fell into two phylogenetic clades (clade 1 and 2, with the latter further divided into sub-clades 2.1, 2.2 and 2.3). The basis of this study was to analyze and compare viruses from these two clades that had infected humans. Clade 1 viruses were prevalent for most documented human infections during 2004–2005, while clade 2 viruses have dominated 2005–2007 (Table 1). 2; 3 Recently, the H5N1 nomenclature has been revised and with ten distinct phylogenetic clades (0 to 9) now defined.1 Despite this revision, all avian H5N1 viruses that have infected humans since 2003, except for one case from Beijing, China in 2003 (clade 7), can still be grouped into only two phylogenetic clades (clade 1 and 2; see Figure 1 and Table 1). Our analysis of the RBD structure, with respect to known sequences of clade 1 and 2 H5N1 viruses, identified two residues at positions 158 and 193 (in H3 numbering) that can be considered clade-specific differences (Figure 1). At position 193, clades 1 and 2.3 HAs have Lys as the predominant residue, whereas clades 2.1 and 2.2 HAs contain contain an Arg (Figure 1). Structurally, this residue could affect receptor specificity as it resides on the α-helix that sits atop the RBD (Figure 5A). Another important feature in the evolution of H5N1 viruses has been acquisition of a glycosylation site at position 158, atop and to one side of the RBD (Figure 5B). Although glycosylation is a critical feature for immune escape by masking antigenic sites 26; 27, this effect is not considered a major selective force in unvaccinated birds 28. In addition, glycosylation has a role in RBD function and specificity, although often overlooked (Figure 5B). Binding data using the glycan microarray, as well as cell-based assays using intact viruses, have already shown that N-linked glycans close to the RBD in other HA subtypes can affect receptor binding through steric hindrance or other mechanisms. 10; 29; 30 Whereas the majority of H5N1 viruses have acquired a glycosylation site at 158, recent clade 2.2 H5N1 isolates that have spread into Europe, Africa and the Middle East, notably lack this carbohydrate-attachment site (Figure 1).
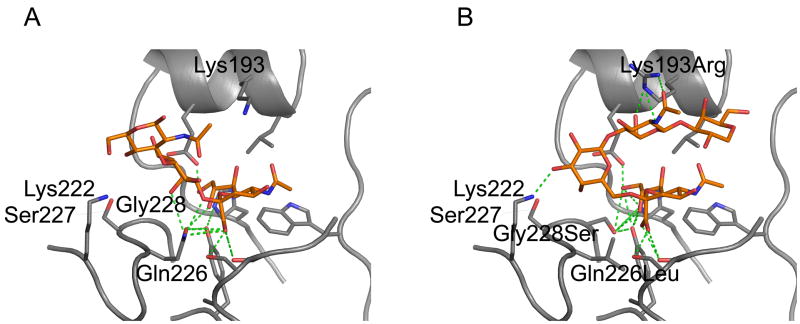
Fig. 5.
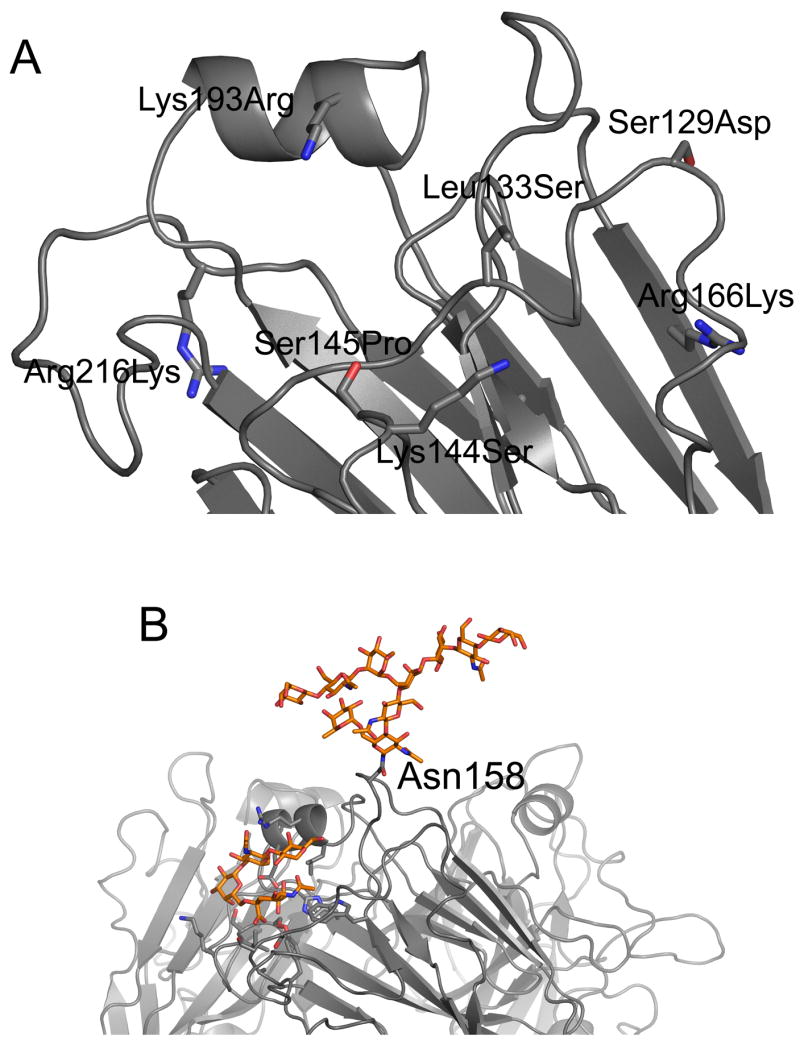
Relationship of clade-specific mutations to the receptor binding domain of H5 HA. A) Structural model showing amino acid differences in and around the RBD of A/Indonesia/05/2005 compared to A/Vietnam/1203/2004. Seven changes are highlighted (with the Viet04 sequence labeled first), but only two, at positions 133 and 193, are within the RBD and likely to directly affect receptor binding. B) Structural model of the Viet04 HA trimer illustrating the direction that α2-6 sialosides exit the HA RBD and the role that a vicinal glycosylation site may play in steric hindrance. One monomer of the trimer was modeled with the lactoseries pentasaccharide, LSTc from the swine H9 HA co-crystal structure (pdb:1JSI) 31 in the RBD. A biantennary glycan, commonly found on influenza viruses 40; 41, was manually appended to the glycosylation site at Asn158 to illustrate the size of such a structure and how it may influence access to the RBD.
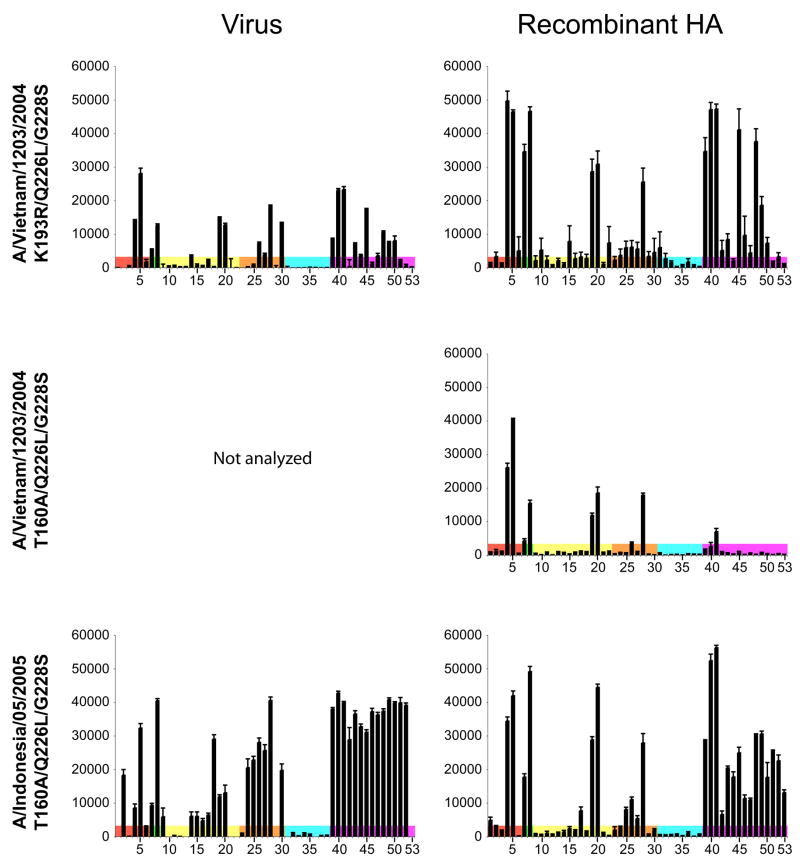
To determine the role of these two clade-dependent differences on the propensity of the clade 2.2 (Egret06) virus to acquire a predominant human-type α2-6 specificity via introduction of the Gln226Leu, Gly228Ser (LS) mutations, we constructed additional mutants using the Viet04-LS and Indo05 HA frameworks. Introduction of the clade 2.1/2.2 specific Lys193Arg mutation onto the clade 1 Viet04-LS HA framework (Viet04-RLS), resulted in a significant increase in binding to α2-6 glycans, but only a marginal reduction for avian α2-3 sialosides for the recombinant HA (cf. Figure 4, row 2 and Figure 6, row 1). The improved α2-6 binding of recombinant Viet04-RLS HA was superior to that of recombinant Indo05-LS HA (Figure 4, row 3) which already has a natural Arg at position 193, suggesting that other features might also contribute to receptor specificity. Removal of the glycosylation site at Asn158 (Asn-Ser-Thr to Asn-Ser-Ala) on the Viet04 framework (Viet04-ALS) resulted in very weak α2-3 and α2-6 binding (Figure 6, row 2), whereas this same mutation on the Indo05 framework (Indo05-ALS) not only greatly reduced α2-3 binding, but also substantially increased α2-6 specificity for both recombinant HA (Figure 6, row 3). Effects of these mutations on their corresponding virus (Figure 6) are less obvious and may be due to avidity effects. Comparison of the Indo05 HA to Viet04 HA reveals a further six residues that differ in and around the RBD (Figure 5A) and, of these, Leu133Ser is within the binding site and may further affect specificity for α2-6 residues. Interestingly, the RBD of a swine H9 interacts with the α2-6 receptor analog, LS-Tetrasaccharide c (LSTc), through hydrogen bonds between the glucose of the receptor analog and residues 131 and 133 of H5 HA. 31
Fig. 6.
Analysis of clade-specific mutations that increase propensity for binding to human-type receptors. Mutants were generated to assess the effect of Arg193 on the clade 1 strain, A/Vietnam/1203/2004 (Viet04-RLS, Row 1) and glycosylation at position 158 in HA on clade 1 (Viet04-ALS, Row 2) and clade 2.1 strain, A/Indonesia/05/2005 (Indo05-ALS, row 3), in addition to human H3 and H2 serotype mutations (Gln226Leu/Gly228Ser). The equivalent viruses shown were generated by reverse genetics and revealed a similar binding profile compared to the recombinant HA. Viruses were analyzed at an HA titer of 128. Because additional glycans were added to the microarrays during the course of this study, glycans #1, 21, 22, 29, 31, 36 and 53 are absent from some of the graphs.
Discussion
It is clear then from our results and others (Figure 3 and a previous report 12) that recent avian viruses (2003–2005) isolated from humans exhibit weak affinity for α2-6 sialosides, particularly for α2-6 biantennary glycans. In the experiments reported here, the corresponding rHAs in fact show little α2-6 binding (Figure 3, right column), and illustrates that increased valency of the HAs on the intact virus surface amplifies the signal for weak interactions with carbohydrate ligands on the array that are likely non-physiological (Figure 1). Fortunately, the natural mutations that have accumulated in the evolution of these H5N1 viruses since 1996/7 have not yet enabled human-to-human transmission, although a number of individuals have been infected, many of whom have died. Whether or not pre-existing mutations in the wild-type viruses have facilitated this incidence of human infection, or, in fact, were selected for during replication in the human host is unknown.
Certain terrestrial birds, such as quail and chicken, have recently been shown to present both human and avian types of receptors in the trachea and intestine.32–34 Thus, prolonged circulation of these viruses in terrestrial birds, such as domestic chickens, may provide a possible route for the virus to develop the receptor specificity needed for efficient human infection.35 Clade 2.1 viruses have circulated extensively in Indonesian poultry since 2003, and that country has reported the most cases of human infection with H5N1 so far. Interestingly, in support of this hypothesis, our analysis of a wild-type, avian isolate, clade 2.2 Egret06 virus revealed only avian α2-3 receptor specificity with no detectable binding to human-type receptors (Figure 3).
In light of the global public health concern with H5N1, it is critical to not only understand fully, but also anticipate, what mutations might enable H5N1 viruses to evolve into a pandemic influenza strain, either directly or via reassortment with an existing human virus. Our previous results 11 indicated that the two mutations known to convert H3 serotypes from avian to human receptor specificity, could constitute a possible route for adaptation of clade 1 H5N1 viruses to human receptors. However, although some highly restricted binding to biantennary α2-6 sugars was acquired, substantial residual binding activity for a wide range of avian-type α2-3 sugars still predominated.
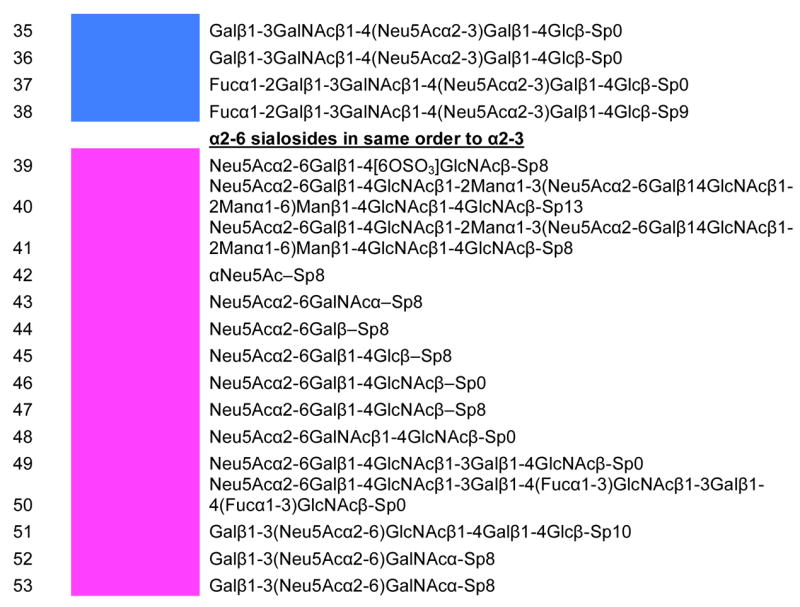
In this study, we focused on the evolution of current H5N1 viral strains some of which were not available at the time of our previous study. We have now identified two natural mutations at positions 193 and 158 in the HA envelope glycoprotein which substantially enhance binding of recombinant H5N1 HAs to human-type receptors when combined with the ‘receptor-switching’ substitutions of pandemic H3 viruses. Interestingly, acquisition of Arg193 and loss of a glycosylation site at Asn158 have both arisen in clade 2.2 viruses that have recently spread into Europe, the Middle East and Africa. Arg193 is a specific feature of clades 2.1 and 2.2 and increases affinity for α2-6 sialosides, in combination with the receptor-switching H3 mutations, possibly through acquisition of multiple hydrogen bonds to the third GlcNAc sugar of these sialylated glycans (Figure 7). Significantly, the H3 receptor-switching mutations (Gln226Leu/Gly228Ser) have a much more significant effect on these recent viruses. Several human influenza viruses have recently been demonstrated to exhibit preference for long chain α2-6 sialosides 10; 14; 36, a specificity that has been proposed by Chandrasekharan et al. to be characteristic of human viruses required for efficient replication and transmission in humans.14 In this study, it is notable, however, that the clade 2 viruses with the Gln226Leu/Gly228Ser mutations exhibit broad specificity for sialosides with the Neu5Acα2-6Gal sequence, that include, but are not limited to, long chain sialosides (e.g. glycans 49, 50).
Fig. 7.
Structural models for binding of sialosaccharides in the RBD of the Viet04 HA. Truncated fragments of human lactoseries tetrasaccharides a and c (LSTa and LSTc) receptor analogs were modeled into the RBD of the Viet04 strain (PDB:2FK0 11) by superimposing the structures of H5 A/Duck/Singapore/3/97 and H9 A/Swine/Hong Kong/9/98 HAs (PDB:1JSN and 1JSI 31) with α2-3 and α2-6 analogs bound. Residues were substituted from the Viet04 model (A) to yield a model for (B) the mutant RLS. Putative hydrogen bonds between the sialoside and the RBD are shown as hashed green lines. Figures were generated with MacPymol 42.
Our results highlight the complexity in assessing the likelihood of adaptation to human receptor specificity from analyses of only one influenza strain. We have shown that the effect of single or multiple mutations on the framework of one strain may not produce an equivalent result on another from a different clade. These findings underscore the importance of continuing to assess how the virus is evolving in real time in susceptible hosts, and the need to constantly evaluate new virus isolates with respect to mutations that could substantially alter or influence receptor specificity or virulence. Thus, immediate access to, and evaluation of, current and emerging strains is of critical importance. Our goal has been to ascertain which mutations could constitute a viable route for H5N1 viruses to adapt to human receptors. The two H3 mutations that are so effective in our in vitro experiments on certain natural H5N1 strains have not yet occurred in nature and there may be some, as yet, unidentified reasons why avian H5N1 viruses cannot readily adapt in vivo via this route. One possibility is that such viruses are not viable in birds, precluding transmission to a new mammalian host that would allow such mutations to be maintained and enriched. Hence, previous suggestions of intermediate hosts 32–34, rather than direct avian-to-human adaptation, may be the route that this virus will take should it adapt successfully. Secondly, Lys193, which predominates in pre-2003 strains, and/or the glycosylation site at 158 (that emerged in Asian sequences 2002–2003), might have influenced the course of evolution of the RBD so that such human adaptation has so far been suppressed.
Thus, for adaptation to a human host, the probability that a clade 1 avian H5N1 virus would acquire four simultaneous mutations at positions 158, 193, 226 and 228 is extremely low. However, the acquisition of an Arg at position 193, and the recent emergence of viruses that lack a glycosylation site at position 158, are natural features of the clade 2.2 family that is circulating in Europe, the Middle East and Africa. Thus, the number of mutations required to change receptor specificity is now reduced to only two, as seen from our studies with the clade 2.2 Egypt06 virus and rHA (Figure 3, row 5 and Figure 4, row 4). Although these features/mutations identified here enable the HA from recent isolates to exhibit increased preference for α2-6 glycans, it still remains to be seen whether such changes in receptor specificity will allow H5N1 to establish efficient replication and facilitate/sustain human-to-human transmission since the other genes in the virus are still avian in origin and their role in human adaptation is still largely unknown. These current studies also highlight the functional, but variable, interdependence of multiple structural elements within and vicinal to the RBD that can influence receptor specificity. Such an intimate understanding of this host-pathogen interaction that assesses the role played by each residue in the RBD in determining receptor specificity is essential for designing intervention strategies and for assessing the risk of the emergence of future pandemics.
Materials and Methods
Cloning Recombinant HAs
Based on H3 numbering 37, cDNAs encoding residues 11–329 (HA1) and 1–176 (HA2) of the ectodomains of the hemagglutinins (HAs) from wild type A/Hong Kong/213/2003, A/Indonesia/05/2005 and A/Egret/Egypt/1162/NAMRU-3/06 were cloned into the baculovirus transfer vector, pAcGP67-A (BD Biosciences Pharmingen, San Jose, CA). The construct for A/Vietnam/1203/2004 (Viet04) has been described previously 11. In a similar fashion to the construct used for expression of the 1918 influenza virus HA for structural studies 16, all constructs incorporated a C-terminal thrombin cleavage site, a ‘foldon’ sequence 38 and a hexa-His tag at the extreme C-terminus of the construct to enable protein purification. Once sequence verified, the plasmids were used as templates for derivation of mutants. Primers containing point mutations around the receptor-binding site were designed using the online QuikChange® Primer Design Program (http://www.stratagene.com), synthesized by Retrogen, Inc. (San Diego, CA) and used with QuickChange® II XL or QuikChange® Multi Site-Directed Mutagenesis kits (Stratagene) to generate mutant HAs. Transfection and virus amplification were carried out as described previously 10; 11; 16.
Expression and Purification
Expression from Trichoplusia ni (Hi5) cells (Invitrogen, Carlsbad, CA) has been described previously 11. For a typical preparation, protein was prepared from two 10-stack CellSTACK™ culture chambers (Corning Inc.) and soluble HA was recovered from the culture supernatant and purified by metal affinity chromatography and ion-exchange chromatography (IEX). Samples were centrifuged to remove insect ferritin, and transferred to a clean tube. A typical yield of pure protein is approximately 2–5 mg per preparation. Samples (100–150 μg of HA protein), diluted with 10 mM Tris-HCl, 50 mM NaCl, pH 8.0 to 1 mg/mL, were set aside for glycan microarray analysis.
Virus generation
Reassortant viruses were generated from plasmids by a reverse genetics approach 17–19. Viral HA and neuraminidase cDNAs were cloned into a pPolI plasmid vector under control of the human polymerase I promoter and the mouse RNA polymerase I terminator. All viruses generated by reverse genetics carried the HA and NA of the avian H5N1 viruses and the internal genes (PB1, PB2, PA, NP, M and NS) of A/Puerto Rico/8/34 (PR8). To generate viruses with amino acid changes in the HA, mutations were introduced into pPolI–HA using an overlap extension PCR approach 39, and resulting plasmids were sequenced verified. Viruses derived by plasmid transfection of HK293 cells were propagated in MDCK or eggs. Viruses recovered by reverse genetics replicated as efficiently as the parental stocks in eggs or MDCK cells (HA titers of mutant viruses were ≤2-fold of corresponding WT parental viruses). The HA1 of resulting virus stocks were sequenced to detect the emergence of possible revertants during amplification. Sequence analysis of the Viet04-LS virus stock revealed 10–30% RNA quasi-species at several loci, whereas the other viruses analyzed during this study had quasi-species levels below the 10% detection threshold.
Glycan Array Fabrication and Glycan Array Analyses
Microarray printing and recombinant HA analysis have been described previously 10; 11; 15. Imprinted slides used were either obtained from the Consortium for Functional Glycomics (CFG) (glycan microarray version 2.1; see www.functionalglycomics.org for further information), or from the CDC from slides produced specifically for influenza research for the CDC using the CFG glycan library (CDC version 1 slides; see Table 2 for glycans used for analyses in these experiments). Briefly, for analysis using recombinant HA, HA-antibody complexes were prepared by mixing recombinant HA (15 μg), mouse anti-penta-His-Alexa Fluor488 (Qiagen, Valencia, CA) and anti-mouse-IgG-Alexa Fluor488 (Invitrogen, Carlsbad, CA) in a molar ratio of 4:2:1, respectively. These prepared mixtures of complexes were incubated for 15 min on ice, diluted to 1 mL with a phosphate-buffered saline buffer containing 3 % (w/v) bovine serum albumin (PBS-BSA) and incubated on the microarray slide in a humidified chamber for 1 hour. Slides were subsequently washed by successive rinses in PBS with 0.05 % Tween-20 (PBS-T), PBS, and deionized water, then immediately subjected to imaging as previously described 15. Virus were analyzed on the microarray as described 15, but with the following modification. Virus stocks were inactivated by treatment with β-propiolactone (BPL; 0.05%) for 3 days at 4°C. Titers were determined using 0.5% turkey red blood cells. Since these cells contain both α2-3 and α2-6 sialoglycans, virus quantification errors due to receptor specificity differences among the viruses should be reduced. Virus preparations were diluted to 1 mL into PBS-BSA at hemagglutination (HA) titers >32 per 50μl. Virus suspensions were applied to slides and the slides were incubated in a closed container and subjected to gentle agitation for 1 hour. Unbound virus was washed off with brief sequential washes in PBS-T and PBS. Slides were then immediately incubated with an anti-H5N1 antibody (30 mins); a biotinylated anti-sheep-IgG antibody (30 mins) and a streptavidin-Alexa Fluor 488 conjugate (30 mins) with brief PBS-T/PBS washes after each incubation. After the final PBS-T/PBS washes, slides were briefly washed in de-ionized water and dried by a gentle steam of air or nitrogen gas and immediately subjected to imaging, as previously described 15. For maximal information, different virus dilutions were analyzed using an HA titer range from 1024 to 32. (Results refer to the HA units per 50μl deduced from a standard hemagglutination inhibition assay). For the majority of samples, an HA titer of 128 units appeared to be a good approximation for maximal information gain. Typically, experiments were conducted in groups of 20 slides, which were affixed to a custom designed 40 slide frame. Accordingly, all slides received simultaneous treatments and wash steps.
Acknowledgments
The work was supported by grants AI058113 (IAW), GM062116 (JP, IAW) and GM060938 (JP) and partial support from CA058896 and AI42266 (IAW). Glycan microarrays were obtained from the Consortium for Functional Glycomics (funded by GM062116), and from the Centers for Disease Control that were produced for the CDC with the CFG glycan library. We thank Yumi Matsuoka and Terrence Tumpey (CDC) for virus cDNAs, and S. Ferguson and P. Carney (The Scripps Research Institute) for expert technical assistance. We also thank the WHO Global Influenza Program Surveillance Network, as well as Triono Soendoro and Endang Sedyaningsih (National Institute of Health, Research and Development, Ministry of Health, Indonesia), Patrick Blair (NAMRU-2, Jakarta, Indonesia), the Ministry of Health and Population of Egypt, Kenneth Earhart and Marshall Monteville (NAMRU-3, Cairo, Egypt), for providing materials. This is publication 18709 from The Scripps Research Institute. Glycan microarray data presented here will be made available on line through the Consortium for Functional Glycomics website upon publication (http://www.functionalglycomics.org).
References
- 1.WHO/OIE/FAO H5N1 Evolution Working Group. Towards a unified nomenclature system for the highly pathogenic avian influenza H5N1 viruses. Emerg Infect Dis. 2008 doi: 10.3201/eid1407.071681. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Global Influenza Program Surveillance Network. Evolution of H5N1 Avian Influenza Viruses in Asia. Emerg Infect Dis. 2005;11:1515–1521. doi: 10.3201/eid1110.050644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Webster RG, Govorkova EA. H5N1 influenza--continuing evolution and spread. N Engl J Med. 2006;355:2174–2177. doi: 10.1056/NEJMp068205. [DOI] [PubMed] [Google Scholar]
- 4.Antonovics J, Hood ME, Baker CH. Molecular virology: was the 1918 flu avian in origin? Nature. 2006;440:E9. doi: 10.1038/nature04824. [DOI] [PubMed] [Google Scholar]
- 5.Gibbs MJ, Gibbs AJ. Molecular virology: was the 1918 pandemic caused by a bird flu? Nature. 2006;440:E8. doi: 10.1038/nature04823. [DOI] [PubMed] [Google Scholar]
- 6.Taubenberger JK, Reid AH, Lourens RM, Wang R, Jin G, Fanning TG. Molecular virology: Was the 1918 pandemic caused by a bird flu? (Reply) Nature. 2006;440:E9–E10. doi: 10.1038/nature04823. [DOI] [PubMed] [Google Scholar]
- 7.Neumann G, Kawaoka Y. Host range restriction and pathogenicity in the context of influenza pandemic. Emerg Infect Dis. 2006;12:881–886. doi: 10.3201/eid1206.051336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tumpey TM, Maines TR, van Hoeven N, Glaser L, Solórzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, García-Sastre A. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 9.Stevens J, Blixt O, Paulson JC, Wilson IA. Glycan microarray technologies: tools to survey host specificity of influenza viruses. Nat Rev Microbiol. 2006;4:857–864. doi: 10.1038/nrmicro1530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stevens J, Blixt O, Glaser L, Taubenberger JK, Palese P, Paulson JC, Wilson IA. Glycoarray analysis of the hemagglutinins from modern and pandemic influenza viruses reveals different receptor specificities. J Mol Biol. 2006;355:1143–1155. doi: 10.1016/j.jmb.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science. 2006;312:404–410. doi: 10.1126/science.1124513. [DOI] [PubMed] [Google Scholar]
- 12.Yamada S, Suzuki Y, Suzuki T, Le MQ, Nidom CA, Sakai-Tagawa Y, Muramoto Y, Ito M, Kiso M, Horimoto T, Shinya K, Sawada T, Kiso M, Usui T, Murata T, Lin Y, Hay A, Haire LF, Stevens DJ, Russell RJ, Gamblin SJ, Skehel JJ, Kawaoka Y. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 13.Yang ZY, Wei CJ, Kong WP, Wu L, Xu L, Smith DF, Nabel GJ. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science. 2007;317:825–828. doi: 10.1126/science.1135165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chandrasekaran A, Srinivasan A, Raman R, Viswanathan K, Raguram S, Tumpey TM, Sasisekharan V, Sasisekharan R. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nature Biotech. 2008;26:107–113. doi: 10.1038/nbt1375. [DOI] [PubMed] [Google Scholar]
- 15.Blixt O, Head S, Mondala T, Scanlan C, Huflejt ME, Alvarez R, Bryan MC, Fazio F, Calarese D, Stevens J, Razi N, Stevens DJ, Skehel JJ, van Die I, Burton DR, Wilson IA, Cummings R, Bovin N, Wong CH, Paulson JC. Printed covalent glycan array for ligand profiling of diverse glycan binding proteins. Proc Natl Acad Sci USA. 2004;101:17033–17038. doi: 10.1073/pnas.0407902101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens J, Corper AL, Basler CF, Taubenberger JK, Palese P, Wilson IA. Structure of the uncleaved human H1 hemagglutinin from the extinct 1918 influenza virus. Science. 2004;303:1866–70. doi: 10.1126/science.1093373. [DOI] [PubMed] [Google Scholar]
- 17.Fodor E, Devenish L, Engelhardt OG, Palese P, Brownlee GG, Garcia-Sastre A. Rescue of influenza A virus from recombinant DNA. J Virol. 1999;73:9679–82. doi: 10.1128/jvi.73.11.9679-9682.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hoffmann E, Webster RG. Unidirectional RNA polymerase I-polymerase II transcription system for the generation of influenza A virus from eight plasmids. J Gen Virol. 2000;81:2843–2847. doi: 10.1099/0022-1317-81-12-2843. [DOI] [PubMed] [Google Scholar]
- 19.Neumann G, Kawaoka Y. Genetic engineering of influenza and other negative-strand RNA viruses containing segmented genomes. Adv Virus Res. 1999;53:265–300. doi: 10.1016/s0065-3527(08)60352-8. [DOI] [PubMed] [Google Scholar]
- 20.Gambaryan A, Tuzikov A, Pazynina G, Bovin N, Balish A, Klimov A. Evolution of the receptor binding phenotype of influenza A (H5) viruses. Virology. 2006;344:432–438. doi: 10.1016/j.virol.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 21.Rogers GN, Paulson JC, Daniels RS, Skehel JJ, Wilson IA, Wiley DC. Single amino acid substitutions in influenza hemagglutinin change receptor binding specificity. Nature. 1983;304:76–78. doi: 10.1038/304076a0. [DOI] [PubMed] [Google Scholar]
- 22.Connor RJ, Kawaoka Y, Webster RG, Paulson JC. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology. 1994;205:17–23. doi: 10.1006/viro.1994.1615. [DOI] [PubMed] [Google Scholar]
- 23.Govorkova EA, Rehg JE, Krauss S, Yen HL, Guan Y, Peiris M, Nguyen TD, Hanh TH, Puthavathana P, Long HT, Buranathai C, Lim W, Webster RG, Hoffmann E. Lethality to ferrets of H5N1 influenza viruses isolated from humans and poultry in 2004. J Virol. 2005;79:2191–2198. doi: 10.1128/JVI.79.4.2191-2198.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maines TR, Lu XH, Erb SM, Edwards L, Guarner J, Greer PW, Nguyen DC, Szretter KJ, Chen LM, Thawatsupha P, Chittaganpitch M, Waicharoen S, Nguyen DT, Nguyen T, Nguyen HH, Kim JH, Hoang LT, Kang C, Phuong LS, Lim W, Zaki S, Donis RO, Cox NJ, Katz JM, Tumpey TM. Avian influenza (H5N1) viruses isolated from humans in Asia in 2004 exhibit increased virulence in mammals. J Virol. 2005;79:11788–11800. doi: 10.1128/JVI.79.18.11788-11800.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zambon M. Lessons from the 1918 influenza. Nat Biotech. 2007;25:433–434. doi: 10.1038/nbt0407-433. [DOI] [PubMed] [Google Scholar]
- 26.Perdue ML, Suarez DL. Structural features of the avian influenza virus hemagglutinin that influence virulence. Vet Microbiol. 2000;74:77–86. doi: 10.1016/s0378-1135(00)00168-1. [DOI] [PubMed] [Google Scholar]
- 27.Baigent SJ, McCauley JW. Glycosylation of haemagglutinin and stalk-length of neuraminidase combine to regulate the growth of avian influenza viruses in tissue culture. Virus Res. 2001;79:177–185. doi: 10.1016/s0168-1702(01)00272-6. [DOI] [PubMed] [Google Scholar]
- 28.Lee CW, Senne DA, Suarez DL. Effect of vaccine use in the evolution of Mexican lineage H5N2 avian influenza virus. J Virol. 2004;78:8372–8381. doi: 10.1128/JVI.78.15.8372-8381.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Klenk HD, Wagner R, Heuer D, Wolff T. Importance of hemagglutinin glycosylation for the biological functions of influenza virus. Virus Res. 2002;82:73–75. doi: 10.1016/s0168-1702(01)00389-6. [DOI] [PubMed] [Google Scholar]
- 30.Marinina VP, Gambarian AS, Bovin NV, Tuzikov AB, Shilov AA, Sinitsyn BV, Matrosovich MN. The effect of losing glycosylation sites near the receptor-binding region on the receptor phenotype of the human influenza virus H1N1. Mol Biol (Mosk) 2003;37:550–555. [PubMed] [Google Scholar]
- 31.Ha Y, Stevens DJ, Skehel JJ, Wiley DC. X-ray structures of H5 avian and H9 swine influenza virus hemagglutinins bound to avian and human receptor analogs. Proc Natl Acad Sci USA. 2001;98:11181–11186. doi: 10.1073/pnas.201401198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gambaryan A, Webster R, Matrosovich M. Differences between influenza virus receptors on target cells of duck and chicken. Arch Virol. 2002;147:1197–1208. doi: 10.1007/s00705-002-0796-4. [DOI] [PubMed] [Google Scholar]
- 33.Wan H, Perez DR. Quail carry sialic acid receptors compatible with binding of avian and human influenza viruses. Virology. 2006;346:278–286. doi: 10.1016/j.virol.2005.10.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Guo CT, Takahashi N, Yagi H, Kato K, Takahashi T, Yi SQ, Chen Y, Ito T, Otsuki K, Kida H, Kawaoka Y, Hidari KI, Miyamoto D, Suzuki T, Suzuki Y. The quail and chicken intestine have sialyl-Gal sugar chains responsible for the binding of influenza A viruses to human type receptors. Glycobiology. 2007 doi: 10.1093/glycob/cwm038. Advance Access published March 27. [DOI] [PubMed] [Google Scholar]
- 35.Taubenberger JK, Morens DM, Fauci AS. The next influenza pandemic: can it be predicted? JAMA. 2007;297:2025–2027. doi: 10.1001/jama.297.18.2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kumari K, Gulati S, Smith DF, Gulati U, Cummings RD, Air GM. Receptor binding specificity of recent human H3N2 influenza viruses. Virol J. 2007;4:42. doi: 10.1186/1743-422X-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weis WI, Brunger AT, Skehel JJ, Wiley DC. Refinement of the influenza virus hemagglutinin by simulated annealing. J Mol Biol. 1990;212:737–761. doi: 10.1016/0022-2836(90)90234-D. [DOI] [PubMed] [Google Scholar]
- 38.Frank S, Kammerer RA, Mechling D, Schulthess T, Landwehr R, Bann J, Gou Y, Lustig A, Bächinger HP, Engel J. Stabilization of short collagen-like triple helices by protein engineering. J Mol Biol. 2001;308:1081–1089. doi: 10.1006/jmbi.2001.4644. [DOI] [PubMed] [Google Scholar]
- 39.Urban A, Neukirchen S, Jaeger KE. A rapid and efficient method for site-directed mutagenesis using one-step overlap extension PCR. Nucl Acids Res. 1997;25:2227–2228. doi: 10.1093/nar/25.11.2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Keil W, Geyer R, Dabrowski J, Dabrowski U, Niemann H, Stirm S, Klenk HD. Carbohydrates of influenza virus. Structural elucidation of the individual glycans of the FPV hemagglutinin by two-dimensional 1H N.M.R and methylation analysis. EMBO J. 1985;4:2711–2720. doi: 10.1002/j.1460-2075.1985.tb03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mir-Shekari SY, Ashford DA, Harvey DJ, Dwek RA, Schulze IT. The glycosylation of the influenza A virus hemagglutinin by mammalian cells. A site-specific study. J Biol Chem. 1997;272:4027–4036. doi: 10.1074/jbc.272.7.4027. [DOI] [PubMed] [Google Scholar]
- 42.Delano WL. The Pymol Molecular Graphics System. 2002 http://www.pymol.org.