Abstract
Objective
To determine gaps in knowledge and barriers to care for diabetic eye disease in Hispanic individuals in Baltimore, Maryland.
Methods
Interviews with a random sample of self-reported Hispanic individuals (n=349), and a convenience sample of Hispanic individuals with diabetes (n=204). Four groups were constructed: without diabetes, with and without a family history of diabetes, newly diagnosed with diabetes, and diagnosed with diabetes more than 1 year before the study.
Results
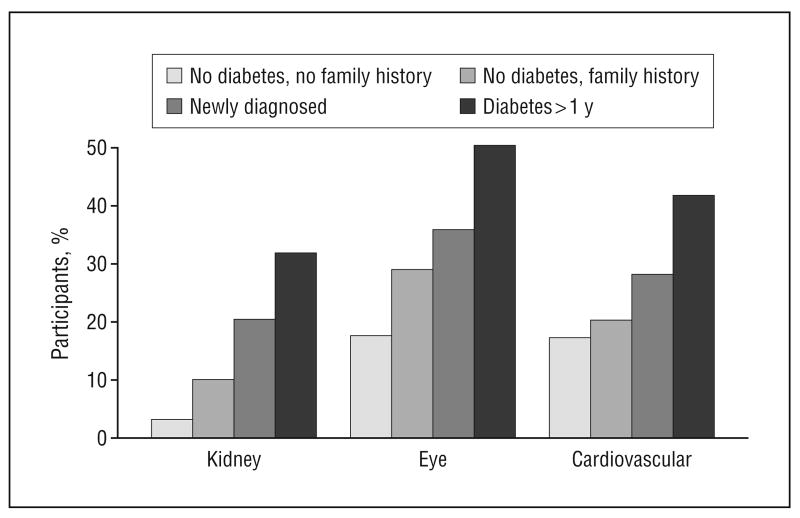
Less than 10% of participants preferred reading in English; 50% reported having providers who do not speak Spanish as a barrier to care. Knowledge of eye disease as a consequence of diabetes was reported by 18% of nondiabetic participants with no family history, 29% of nondiabetic participants with a family history, 36% of newly diagnosed diabetic patients, and 52% of participants diagnosed with diabetes more than 1 year before the study. Only 16%, 28%, 13%, and 34%, respectively, knew that strict control could prevent eye problems, and 33%, 51%, 31%, and 48%, respectively, knew that dilated eye examinations were important. A total of 30% of diabetic participants had had an eye examination in the previous year.
Conclusions
Knowledge of the ocular complications of diabetes is low. The frequency of eye examinations among Hispanic individuals with diabetes is less than the national average for Hispanic individuals. Culturally appropriate health education and innovations to reduce barriers to eye care are needed.
In recent decades the prevalence of diabetes has been steadily increasing worldwide, and projections of the year 2030 indicate that the United States, along with China and India, will have the largest number of people with diabetes.1,2 The health consequences of uncontrolled diabetes and the repercussions for health care costs are immense.3,4 In the United States, diabetes is more likely to affect minority populations.5 In 1 study, compared with non-Hispanic white individuals, the ratio of age- and sex-standardized prevalence of diabetes was 1.9 for Hispanic individuals and 1.6 for African American individuals.6 Diabetes prevalence is expected to increase by 44% by the year 2020; this increase will disproportionately affect Hispanic persons, for whom the projected increase is 107%.3,5 This increase is especially alarming, as the Hispanic population is the largest growing minority community, with a population estimated to double by 2025.7 Currently, 1 in 5 Hispanic persons older than 40 years has diabetes, and almost half have diabetic retinopathy.8,9
There is a suggestion that Hispanic individuals are more likely to have more severe signs of diabetic retinopathy compared with non-Hispanic white individuals, after adjusting for duration,10,11 but others have found no difference after adjusting for level of control.8 The limited use of health care services in minority groups may make them more susceptible to the complications of uncontrolled diabetes. In addition, a substantial proportion of those with diabetes are unaware of their condition, although already presenting signs of moderate to severe diabetic retinopathy.8,12 The importance of appropriate and timely care for diabetic retinopathy or macular edema is paramount, as it is the leading cause of visual loss among working-age Hispanic individuals.13,14
As part of a project to create and evaluate novel methods of disseminating health education messages and materials on diabetes and diabetic retinopathy to the Hispanic community, we conducted a survey within a random sample of Hispanic persons living in Baltimore, supplemented with a convenience sample of Hispanic persons with diabetes. The purpose of this article is to report the gaps in knowledge and the perceived barriers to eye care for diabetic eye disease in the Hispanic community, according to the level of personal experience with diabetes.
Methods
Study Population
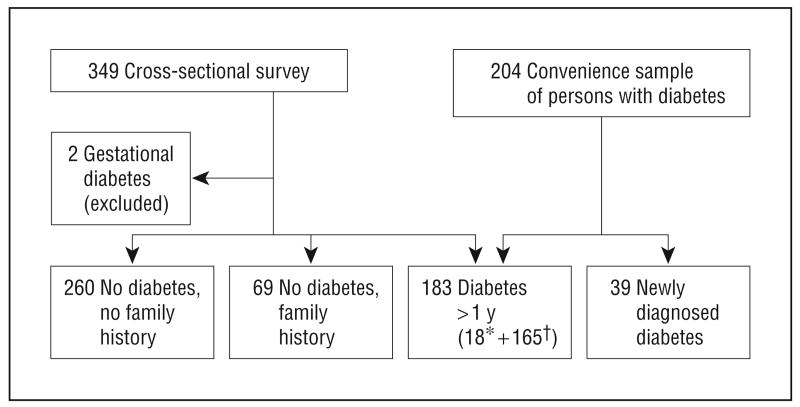
Twelve Baltimore city block groups with a proportion of more than 15% Hispanic individuals were identified from the year 2000 census; 8 were randomly selected. All houses in the selected block groups were screened for eligibility, defined as the presence of at least 1 self-reported Hispanic person aged 21 years or older. All Hispanic household members were listed and 1 was selected at random to participate. A total of 383 eligible households were identified, and of the randomly selected eligible members, 349 agreed to participate (response rate, 91%). Two women with gestational diabetes were excluded from this report, leaving 347 participants, of whom 18 had diabetes. The sample was supplemented with a cohort of 204 Hispanic individuals with diabetes identified at neighborhood clinics and health fairs in the Baltimore metropolitan area. The composition of the final group is shown in Figure 1.
Figure 1.
Stratification groups of study population. Asterisk indicates population from cross-sectional survey; dagger, population from convenience sample.
The research protocol was approved by the Johns Hopkins Medical Institutions review board and followed the tenets of the Declaration of Helsinki. After informed written consent was obtained, participants were asked to respond to an extensive questionnaire administered by a trained bilingual interviewer.
Data Collection
The questionnaire included 3 main sections: (1) basic demographic information regarding age, sex, education, literacy, and acculturation; (2) health and health care–seeking behaviors, such as overall health status, place of routine health care, medical insurance status, providers of health advice, difficulties that Hispanic persons encounter when seeking care, and places to obtain health information; (3) diabetes and diabetic retinopathy knowledge that included questions on the key points of knowledge of diabetes, diabetic eye disease, and appropriate eye care–seeking behavior. In addition, if the respondent had diabetes, specific questions about his or her diabetes, such as type of medication, date of onset or diagnosis, and any diabetic complications such as renal or eye problems were asked. Questions were also asked regarding eye care–seeking behavior, specifically whether a dilated eye examination was performed in the past year and where the examination took place. Any prior eye treatment for diabetes or other eye conditions was also ascertained. A sample of the questions related to diabetes knowledge is shown in Table 1. Questions related to knowledge were open-ended. Possible correct answers and incorrect answers were developed in advance, and the questions were scored for number of items correct and incorrect.
Table 1. Sample of Questions Related to Diabetes and Diabetic Eye Disease.
| Question | Example of Correct Answer | Example of Incorrect Answer |
|---|---|---|
| What is diabetes? | High blood glucose | Don't know |
| What can be done to keep diabetes under control? | Take medicine for sugar | Pray, hygiene |
| Why is it important to keep diabetes under control? | To prevent heart problems | So children do not get it |
| Can you do anything to prevent the eye disease? | Control blood glucose | No, use glasses |
| When it starts, does diabetic eye disease have any symptoms? | No, you can have it and not know it | Yes, you can't see |
| Can you do anything to prevent blindness once you have eye disease? | See an eye doctor | No |
For analysis purposes, 4 groups were created: participants without diabetes and with no reported history of diabetes in their immediate family, participants with no diabetes but with a family history, participants with diabetes for 1 year or more, and participants with newly diagnosed (within 1 year) diabetes (Figure 1).
For categorical outcomes, the χ2 test was used to test for significant differences in participants' characteristics by group. For continuous outcomes (eg, age, duration of diabetes) significant differences between strata were evaluated using a t test. Logistic regression models were built to identify independent factors associated with knowledge of the vision consequences of uncontrolled diabetes and of having an eye examination within the previous 2 years for persons with diabetes.
Results
The 18 participants with diabetes identified in the cross-sectional survey were compared with participants with diabetes from the convenience sample. The participants from the cross-sectional survey were an average of 4 years younger and more likely to be women (80% vs 40%). In terms of access to health care, the 2 groups reported similar rates of having medical insurance (35% vs 25%), a routine place to go for health care (61% vs 56%), and a dilated eye examination in the last year (28% vs 32%) for the cross-sectional and convenience sample, respectively.
Characteristics of those with and without diabetes are shown in Table 2. Participants with diabetes were an average of 13 years older and more likely to report fair to poor health. More than 86% of all respondents preferred reading Spanish, only 24% had more than a high school education, and less than a quarter reported having health insurance. The majority of respondents sought information about health from clinics, community centers, family, and friends. Only 5% of persons without diabetes and 2% of those with diabetes reported getting health information from written material or the internet.
Table 2. Demographic Characteristics by Diabetes Status.
| Characteristic | Persons Without Diabetes (n=329) | Persons With Diabetes (n=222) |
|---|---|---|
| Mean (SD) age, y | 35 (11) | 48 (12)a |
| Female, % | 43 | 46 |
| Education, % | ||
| None | 6 | 8 |
| Some elementary school | 37 | 43 |
| Some high school | 33 | 26 |
| Complete high school or more | 24 | 24 |
| Language reading preference, % | ||
| Not able to read | 5 | 8 |
| Spanish | 86 | 85 |
| English | 4 | 1 |
| Both (no preference) | 5 | 6 |
| Years of residency in Baltimore, % | ||
| <1 | 19 | 20 |
| 1 to <5 | 45 | 35 |
| ≥5 | 36 | 45a |
| Self-reported health status, % | ||
| Poor | 7 | 17a |
| Fair | 31 | 47 |
| Good | 53 | 32 |
| Very good or excellent | 9 | 3 |
| Have a place to go for routine care | 28 | 57a |
| Have health insurance | 20 | 26 |
| Needed care during last year, % | ||
| No | 53 | 18 |
| Yes, did not receive care | 10 | 3 |
| Yes, received care | 37 | 79a |
| Source of health information, % | ||
| Health or community center | 60 | 60 |
| Family and friends | 10 | 11 |
| Written materials; internet | 5 | 2a |
| Reported provider not speaking Spanish as a barrier to accessing care | 51 | b |
Differences significant at P<.05.
Question was not asked of the diabetic cohort.
More than 40% of the respondents did not have a routine place to go for health care, although this differed greatly by the presence or absence of diabetes (28% vs 57%, respectively). The mean age at diagnosis of diabetes was 41 years, with an average duration of 6.2 years (Table 3). There were significant differences by sex in the way diabetes was managed, as men were less likely to have ever visited an eye care provider than women (38% vs 55%, P=.01). About one-third of participants with diabetes reported ever using natural remedies for their disease, and 2% reported currently treating their diabetes with natural remedies only.
Table 3. Diabetes Duration and Type of Treatment in Participants With Diabetes.
| Characteristic | Men
(n=120) |
Women
(n=102) |
Total
(n=222) |
|---|---|---|---|
| Mean (SD) age at diagnosis, y | 41.7 (11.0) | 41.1 (11.7) | 41.4 (11.3) |
| Mean (SD) duration of diabetes, y | 6.0 (7.4) | 6.4 (6.5) | 6.2 (7.0) |
| Ever taken insulin, % | 34 | 46 | 39 |
| Ever taken pills, % | 82 | 87 | 84 |
| Ever used natural remedies, % | 32 | 28 | 31 |
| Current treatment, %a | |||
| Insulin | 17 | 17 | 17 |
| Pills | 54 | 63 | 58 |
| Diet only | 17 | 11 | 14 |
| Natural remedies | 2 | 3 | 2 |
| No treatment | 11 | 7 | 9 |
| Years since last dilated eye examination, % | |||
| <1 | 29 | 36 | 32 |
| 1 to <2 | 4 | 9 | 8 |
| ≥2 | 4 | 10 | 7 |
| Never | 62 | 45 | 53b |
Refers to primary mode of treatment.
P<.05.
Participants with a duration of diabetes of more than 1 year or with a family member with diabetes had similar levels of knowledge about how to treat and control diabetes, with almost 90% giving all correct answers to the question “What can a person with diabetes do to treat and control diabetes?” In contrast, 69% of those without diabetes and with no family history, and 79% of newly diagnosed participants with diabetes gave all correct answers to the same question. The number of answers that a respondent was willing to give differed by group; 37% of persons who had had diabetes for more than a year stated 3 or more ways to keep diabetes under control, compared with only 20% of the group without diabetes and with a family history, 13% of the newly diagnosed group, and 10% of the group without diabetes and with no family history (Table 4). Respondents were less knowledgeable about the consequences of diabetes if the disease was not being controlled, with half of persons with diabetes for more than 1 year and 36% of newly diagnosed participants reporting knowing that uncontrolled diabetes could cause eye disease (Figure 2).
Table 4. Diabetes Knowledge by Level of Experience With Diabetesa.
| Percentage
|
|||||
|---|---|---|---|---|---|
| No. of Answers | Answer | No Diabetes, No Family History | No Diabetes With Family History | Newly Diagnosed | Diabetes > 1 y |
| 1 | Total, No. (%) | 145 (56) | 16 (23) | 13 (33) | 33 (18) |
| Correct | 57.9 | 81.3 | 53.9 | 90.9 | |
| 2 | Total, No. (%) | 89 (34) | 39 (57) | 21 (54) | 81 (45) |
| 1 Correct | 10.1 | 5.1 | 9.5 | 3.7 | |
| 2 Correct | 87.6 | 94.9 | 90.5 | 96.3 | |
| ≥3 | Total, No. (%) | 26 (10) | 14 (20) | 5 (13) | 68 (37) |
| All wrong | 0 | 0 | 0 | 0 | |
| Some correct | 26.9 | 21.4 | 0 | 16.2 | |
| All correct | 73.1 | 78.6 | 100.0 | 83.8 | |
| Total | Total, No. (%) | 260 (100) | 69 (100) | 39 (100) | 182 (100) |
| All wrong | 24.2 | 4.4 | 15.4 | 1.7 | |
| Some correct | 6.2 | 7.2 | 5.1 | 7.7 | |
| All correct | 69.6 | 88.4 | 79.4 | 90.7 | |
Proportion of correct answers to the question, “What can a person with diabetes do to treat and control diabetes?”
Figure 2.
Percentage of participants reporting knowledge that kidney, eye, and cardiovascular disease could be the result of uncontrolled diabetes, stratified by level of experience with diabetes.
We created a multivariate model predicting whether participants know that uncontrolled diabetes can cause eye disease. The 2 main factors were the length of time a person had diabetes, with the group who had diabetes for more than a year being more likely to know about diabetic eye disease, and having a family member affected. Those with newly diagnosed diabetes were no more likely to know that diabetes can cause eye disease than persons without diabetes and with no family members with diabetes. In addition, those who completed high school were 2.5 times more likely to know that diabetes can cause eye disease (Table 5).
Table 5. Predictors of Knowledge That Uncontrolled Diabetes Could Cause Eye Disease.
| Characteristic | OR (95% CI) |
|---|---|
| Age (per year increment) | 1.01 (0.99-1.03) |
| Female | 1.32 (0.89-2.00) |
| Education | |
| Less than secondary | 1.00 |
| Some secondary | 1.51 (0.95-2.34) |
| High school or more | 2.48 (1.50-4.01)a |
| Length of stay in the United States, y | |
| <1 | 1.00 |
| 1 to <5 | 0.92 (0.54-1.57) |
| >5 | 1.25 (0.72-1.57) |
| No diabetes, no family history | 1.00 |
| No diabetes, family history | 3.66 (1.94-6.89)a |
| Newly diagnosed with diabetes | 1.21 (0.56-2.64) |
| With diabetes >1 y | 4.03 (2.41-6.76)a |
Abbreviations: CI, confidence interval; OR, odds ratio.
P<.05.
Less than half of the participants who had had diabetes for more than 1 year and only 30% of those with newly diagnosed diabetes reported regular visits to an ophthalmologist as a way to prevent vision loss from diabetic eye disease (Figure 3). Almost half of the participants who had had diabetes for more than 1 year and 79% of the participants with newly diagnosed diabetes had never had a dilated eye examination (Figure 3).
Figure 3.
Control of diabetic eye disease. A, Percentage of participants reporting that treatment, diet/exercise, and regular visits to an eye care provider are ways to prevent eye disease as a complication of diabetes. B, Reported time of participants' last dilated eye examination, stratified by level of experience with diabetes.
We also examined the predictors of participants with diabetes reporting that they have had a dilated eye examination in the last 2 years (Table 6). Older age, residing in the United States for 5 or more years, and having insurance were significantly associated with having had a dilated eye examination. Compared with those who were diagnosed with diabetes more than 1 year before the study, persons with newly diagnosed diabetes were much less likely to have had an eye examination.
Table 6. Predictors of Having a Dilated Eye Examination in the Past 2 Years in Persons With Diabetes.
| Characteristic | OR (95% CI) |
|---|---|
| Age (per year increment) | 1.06 (1.02-1.09)a |
| Female | 1.96 (0.94-4.08) |
| Education | |
| Less than secondary | 1.00 |
| Some secondary | 1.18 (0.50-2.78) |
| High school or more | 1.55 (0.62-3.85) |
| Length of stay in the United States, y | |
| <1 | 1.00 |
| 1 to <5 | 2.78 (0.94-8.28) |
| >5 | 4.14 (1.48-11.57)a |
| Newly diagnosed with diabetes | 0.21 (0.06-0.85)a |
| Having health insurance | 3.11 (1.41-6.89)a |
Abbreviations: CI, confidence interval; OR, odds ratio.
P<.05.
Comment
The level of knowledge of the adverse consequences of uncontrolled diabetes was low: half of participants with a diagnosis of diabetes more than 1 year prior and one-third of newly diagnosed participants knew that uncontrolled diabetes could cause eye disease; a slightly lower but similar proportion reported knowledge of diabetes causing cardiovascular disease. Significantly lower proportions (32% of participants with diabetes for more than a year and 20% of newly diagnosed participants) reported that kidney disease could be caused by uncontrolled diabetes. The higher level of awareness of eye and cardiovascular disease compared with kidney disease was expected, as these complications are more frequently seen in persons with type 2 diabetes.15 We do not feel there was bias resulting in higher levels of knowledge of eye disease as a consequence of diabetes, because all participants and interviewers were recruited through the Hispanic Apostolate, not through the Wilmer Eye Institute.
The lack of correct information about diabetes and diabetic eye disease in this population of Hispanic individuals should be of great concern. A classic approach to lack of knowledge is to increase awareness using health education materials. However, our data are consistent with findings in other studies that Hispanic individuals are less likely to use available diabetes brochures and other forms of educational materials because of the materials' complexity level.16 Hispanic individuals with more than a high school education were more likely to report knowledge of the ocular morbidity caused by uncontrolled diabetes, suggesting that current diabetes health education efforts are only reaching the educated Hispanic audience. In our sample, 43% of persons without diabetes and more than 50% of persons with diabetes had less than a high school education, and less than 10% choose English as their preferred reading language. To reach the Hispanic community in Baltimore, it is first important for diabetes educational materials to be in Spanish, at a reading level that is compatible with the educational level of the majority of the target population. Second, distribution of the materials should be through channels that are easily accessible by the majority of the Hispanic community. In our study, less than 5% of participants reported getting health information from written materials (brochures, books, internet); the majority relied on verbal communication from health clinics, community centers, family, and friends. This is consistent with the findings of a study of diabetic retinopathy screening among Hispanics,17 which aimed to increase awareness of diabetic retinopathy and compliance with eye exams. They found that the use of more personalized strategies such as phone calls, door-to-door visits, and flexible scheduling were more effective in increasing compliance than the passive distribution of educational brochures.
Lack of education also affects the likelihood that complication rates of diabetes will be higher. In a population-based study of Hispanic persons in Arizona,12 the group with diabetes who had less education was more likely to have moderate to severe retinopathy compared with those with a high school education or more. In another study of older Mexican Americans, those with less than a high school education were more likely to report diabetes complications than those with a high school education; 38% of these complications were eye problems.18 These results suggest that the lack of awareness of the consequences of uncontrolled diabetes may result in less metabolic control and higher incidence of complications.
The American Diabetes Association recommends annual eye examinations for people with type 2 diabetes.19 In our sample, 68% of persons with diabetes had not had an eye examination in the past year, and more than half had not had an eye examination in the previous 5 years. These proportions are similar to those of a study of a population-based sample of Hispanic individuals with diabetes in Los Angeles,20 but very different from the results of other studies. In a study of Hispanic individuals in Arizona,12 the reported rate of eye exams within the last 2 years was 70%. In national samples, the rates of reporting not having had an eye examination were 25% to 30%, and 34% to 43% for non-Hispanic white individuals and Hispanic individuals, respectively.21,22 The discrepancy between the national estimates for Hispanic individuals and our estimates for Hispanic individuals in Baltimore may reflect differences in the socioeconomic status of the group who participated in the national samples. Our sample was from Baltimore's inner city and composed mostly of individuals who had recently emigrated from Mexico and Central America. Also, the Hispanic population in Baltimore has few options for eye care professionals who serve their community in particular, and the data may reflect barriers to access.
Less than one-third of the newly diagnosed participants with diabetes knew that periodic visits to an ophthalmologist were important to prevent vision loss due to diabetic eye disease, and most had never had an eye examination. Although this group has been recently diagnosed, their contact with a health care provider did not result in knowledge of how to prevent or treat the potential ocular complications of diabetes. Moreover, of those with diabetes who reported visiting an eye care provider in the previous year, only 28% knew that an annual eye examination was recommended by the American Diabetes Association as the standard of care. These data suggest that target audiences for educational programs should not only include Hispanic patients with diabetes, but also their health care providers. In particular, diabetic clinics serving Hispanic patients should include bilingual health professionals who can explain the key elements of a successful diabetes self-management program and follow-up care to their patients.15,22-24
Financial constraints are a major barrier to accessing health care. Independent of education level, noncompliance with treatment and annual eye examinations were strongly associated with not having health insurance, in our population as well as in others.20,25-27 The absence of coverage is not exclusive to the Hispanic community, but it would be instructive to see what can be done if such barriers are minimized. Successful approaches to meeting the American Diabetes Association standards of care for underserved Hispanic patients have been reported.23,28 A demonstration project in California aimed to improve diabetes care for underinsured, primarily Hispanic, patients.23 This program included a case management nurse who was both bilingual and bicultural, group education, access to medication, and access to at least 1 free screening retinal examination. The ophthalmic services were performed on site, often the same day as a clinic visit. The results showed significant improvements in accessing clinical care, self-awareness, and understanding of diabetes. In particular, 90% of the participants in the intervention group underwent retinal examinations within 18 months of initiation of the program, compared with only 6% in the control group. Although the cost of routine care was higher under the program, there was an overall decrease in cost due to reduced hospital expenditures.29
There are some limitations to our study. While we had excellent participation in the baseline survey, we supplemented the group of Hispanic participants with diabetes through convenience sampling, recruitment through local community clinics, and festivals. Thus, we cannot conclude that the group with diabetes reflects all Hispanic individuals with diabetes in Baltimore, or that their level of knowledge or reported practices is representative. However, our results are similar to other studies that have evaluated population-based samples of Hispanic individuals with diabetes in Los Angeles and Arizona, providing some evidence that our findings are not biased. Our data on eye examinations are reported rather than based on chart review, so they may be overestimates of dilated eye examinations, although we took care to explain what was involved in such an examination. This problem is common to all the studies reporting the previous history of eye exams.
The level of awareness about diabetes and what a person can do to control diabetes is reasonable in this population of Hispanic individuals. However, knowledge of ocular complications and how to prevent them was very low in the Hispanic community, particularly among persons with diabetes. Persons with newly diagnosed diabetes were especially at risk, having a lack of knowledge of diabetic eye disease similar to those without diabetes, with no family history, and with a low rate of ever having had an eye examination. The frequency of dilated eye examinations among people with diabetes was unacceptable, and places this population at risk of visual loss. These deficiencies need to be rectified with a culturally appropriate health education campaign, and with innovative ways to reduce barriers to health care.
Acknowledgments
Funding/Support: This project was supported by grant EY015900 from the National Eye Institute.
Footnotes
Author Contributions: Dr Muñoz had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Financial Disclosure: None reported.
Additional Information: Dr West is a Research to Prevent Blindness Senior Scientific Investigator.
Contributor Information
Beatriz Muñoz, Dana Center for Preventive Ophthalmology, Wilmer Eye Institute, Baltimore, Maryland.
Michael O'Leary, Dana Center for Preventive Ophthalmology, Wilmer Eye Institute, Baltimore, Maryland.
Fannie Fonseca-Becker, Center for Communication Programs, Johns Hopkins University, Baltimore, Maryland.
Evelyn Rosario, the Hispanic Apostolate, Baltimore, Maryland.
Isabel Burguess, the Hispanic Apostolate, Baltimore, Maryland.
Marcela Aguilar, Center for Communication Programs, Johns Hopkins University, Baltimore, Maryland.
Cynthia Fickes, the Hispanic Apostolate, Baltimore, Maryland.
Sheila K. West, Dana Center for Preventive Ophthalmology, Wilmer Eye Institute, Baltimore, Maryland.
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21(9):1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 2.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27(5):1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 3.Hogan P, Dall T, Nikolov P American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26(3):917–932. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Standards of medical care in diabetes: 2006. Diabetes Care. 2006;29(suppl 1):S4–S42. [PubMed] [Google Scholar]
- 5.Narayan KMV, Boyle JP, Thompson TJ, Sorensen SW, Williamson DF. Lifetime risk of diabetes mellitus in the United States. JAMA. 2003;290(14):1884–1890. doi: 10.1001/jama.290.14.1884. [DOI] [PubMed] [Google Scholar]
- 6.Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose and impaired glucose tolerance in US adults: the Third National Health and Nutrition Examination Survey (NHANES) 1988-1994. Diabetes Care. 1998;21(4):518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 7.National Population Projections. [February 15, 2007];US Census Bureau Web site. http://www.census.gov/population/www/projections/natsum-T3.html.
- 8.West SK, Klein R, Rodriguez J, et al. Diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Diabetes Care. 2001;24(7):1204–1209. doi: 10.2337/diacare.24.7.1204. [DOI] [PubMed] [Google Scholar]
- 9.Varma R, Torres M, Pena F, Klein R, Azen SP Los Angeles Latino Eye Study Group. Prevalence of diabetic retinopathy in adult Latinos: LALES. Ophthalmology. 2004;111(7):1298–1306. doi: 10.1016/j.ophtha.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Wong TY, Klein R, Islam FM, et al. Diabetic retinopathy in a multi-ethnic cohort in the US. Am J Ophthalmol. 2006;141(3):446–455. doi: 10.1016/j.ajo.2005.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Emanuele N, Sacks J, Klein R, et al. Ethnicity, race, and baseline retinopathy correlates in the veterans affairs diabetes trial. Diabetes Care. 2005;28(8):1954–1958. doi: 10.2337/diacare.28.8.1954. [DOI] [PubMed] [Google Scholar]
- 12.West SK, Muñoz B, Klein R, et al. Risk factors for type II diabetes and diabetic retinopathy in a Mexican-American population: Proyecto VER. Am J Ophthalmol. 2002;134(3):390–398. doi: 10.1016/s0002-9394(02)01595-7. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez J, Sanchez R, Muñoz B, et al. Causes of blindness and visual impairment in a population-based sample of U.S. Hispanics. Ophthalmology. 2002;109(4):737–743. doi: 10.1016/s0161-6420(01)01008-9. [DOI] [PubMed] [Google Scholar]
- 14.Cotter SA, Varma R, Ying-Lai M, Azen SP, Klein R Los Angeles Latino Eye Study Group. Causes of low vision and blindness in adult Latinos: the Los Angeles Latino Eye Study. Ophthalmology. 2006;113(9):1574–1582. doi: 10.1016/j.ophtha.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 15.Wendel CS, Shah JH, Duckworth WC, Hoffman RM, Mohler MJ, Murata GH. Racial and ethnic disparities in the control of cardiovascular disease risk factors in Southwest American veterans with type 2 diabetes: the Diabetes Outcomes in Veterans Study. BMC Health Serv Res. 2006;6:58. doi: 10.1186/1472-6963-6-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brown SA, Hanis CL. Culturally competent diabetes education for Mexican Americans: the Starr County Study. Diabetes Educ. 1999;25(2):226–236. doi: 10.1177/014572179902500208. [DOI] [PubMed] [Google Scholar]
- 17.Navuluri RB. Diabetic Retinopathy screening among Hispanics in Lea County, New Mexico. J Health Care Poor Underserved. 2000;11(4):430–443. doi: 10.1353/hpu.2010.0791. [DOI] [PubMed] [Google Scholar]
- 18.Otiniano ME, Black SA, Ray LA, Markides KS. Correlates of diabetes complications in Mexican-American elders. Ethn Dis. 2002;12(2):252–258. [PubMed] [Google Scholar]
- 19.American College of Physicians, American Diabetes Association, American Academy of Ophthalmology. Screening guidelines for diabetic retinopathy. Ann Intern Med. 1992;116(8):683–685. [PubMed] [Google Scholar]
- 20.Paz SH, Varma R, Klein R, Wu J, Azen SP. Noncompliance with vision care guidelines in Latinos with type 2 diabetes mellitus: the Los Angeles Latino Eye Study. Ophthalmology. 2006;113(8):1372–1377. doi: 10.1016/j.ophtha.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 21.Correa-de-Araujo R, McDermott K, Moy E. Gender differences across racial and ethnic groups in the quality of care for diabetes. Womens Health Issues. 2006;16(2):56–65. doi: 10.1016/j.whi.2005.08.003. [DOI] [PubMed] [Google Scholar]
- 22.Thackeray R, Merrill RM, Neiger BL. Disparities in diabetes management practice between racial and ethnic groups in the United States. Diabetes Educ. 2004;30(4):665–675. doi: 10.1177/014572170403000418. [DOI] [PubMed] [Google Scholar]
- 23.Philis-Tsimikas A, Walker C, Rivard L, et al. Improvement in diabetes care of underinsured patients enrolled in Project Dulce. Diabetes Care. 2004;27(1):110–115. doi: 10.2337/diacare.27.1.110. [DOI] [PubMed] [Google Scholar]
- 24.Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans. Diabetes Care. 2002;25(2):259–268. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kuo YF, Raji MA, Markides KS, Ray LA, Espino DV, Goodwin JS. Inconsistent use of diabetes medications, diabetes complications, and mortality in older Mexican-Americans over a 7-year period. Diabetes Care. 2003;26(11):3054–3060. doi: 10.2337/diacare.26.11.3054. [DOI] [PubMed] [Google Scholar]
- 26.Schneider EC, Zaslavsky AM, Epstein AM. Racial disparities in quality of care for enrollees in medicare managed care. JAMA. 2002;287(10):1288–1294. doi: 10.1001/jama.287.10.1288. [DOI] [PubMed] [Google Scholar]
- 27.Oladele CRW, Barnett E. Racial/ethnic and social class differences in preventive care practices among person with diabetes. BMC Public Health. 2006;6:259. doi: 10.1186/1471-2458-6-259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Heuer LJ, Hess C, Batson A. Cluster clinics for migrant Hispanic farmworkers with diabetes: perceptions, successes, and challenges. Rural Remote Health. 2006;6(1):469. [PubMed] [Google Scholar]
- 29.Gilmer TP, Philis-Tsimikas A, Walker C. Outcomes of Project Dulce: culturally specific diabetes management program. Ann Pharmacother. 2005;39(5):817–822. doi: 10.1345/aph.1E583. [DOI] [PubMed] [Google Scholar]