Abstract
Diaphragm myopathy has been described in patients with heart failure (HF), with alterations in myosin heavy chains (MHC) expression. The pathways that regulate MHC expression during HF have not been described, and myogenic regulatory factors (MRFs) may be involved. The purpose of this investigation was to determine MRF mRNA expression levels in the diaphragm. Diaphragm muscle from both HF and control Wistar rats was studied when overt HF had developed, 22 days after monocrotaline administration. MyoD, myogenin and MRF4 gene expression were determined by RT-PCR and MHC isoforms by polyacrylamide gel electrophoresis. Heart failure animals presented decreased MHC IIa/IIx protein isoform and MyoD gene expression, without altering MHC I, IIb, myogenin and MRF4. Our results show that in HF, MyoD is selectively down-regulated, which might be associated with alterations in MHC IIa/IIx content. These changes are likely to contribute to the diaphragm myopathy caused by HF.
Keywords: diaphragm muscle, heart failure, myogenic regulatory factors, myosin heavy chain, Wistar rats
Heart failure (HF) is characterized by reduced tolerance to exercise because of early fatigue and dyspnoea (Wilson & Mancini 1993). Limb-muscle fatigue has been partly attributed to a shift from myosin heavy chain (MyHC) I ‘slow’ to MyHC II ‘fast’ (Simonini et al. 1996; Vescovo et al. 1998; Carvalho et al. 2003), whereas a shift from MyHC II to MyHC I in diaphragm muscle may contribute to dyspnoea in this syndrome (Tikunov et al. 1996; De Sousa et al. 2001). However, the skeletal muscle-specific molecular regulatory mechanisms that alter MHC expression in the diaphragm during HF are not known.
Different pathways regulate skeletal muscle MHC expression (Allen et al. 2001); these include myogenic regulatory factors (MRFs), a family of transcriptional factors that control the expression of several skeletal muscle-specific genes (Hughes et al. 1993, 1999). The family has four members: MyoD, myogenin, Myf5 and MRF4. Myogenic regulatory factors form dimers with ubiquitous E proteins (e.g. E12 or E47) resulting in heterodimeric complexes that bind to the E-box consensus DNA sequence (5′-CANNTG-3′) found in the regulatory region of many muscle-specific genes (Murre et al. 1989). During embryogenesis, MRFs are critical for establishing myogenic lineage and controlling terminal differentiation of myoblasts (Parker et al. 2003). Previous studies have suggested that myogenin and MyoD may also be involved in establishing and maintaining slow and fast mature muscle fibre phenotype; myogenin is expressed at higher levels than MyoD in slow muscles, whereas the opposite is true for fast muscles (Hughes et al. 1993; Voytik et al. 1993). Similarly, MyoD is associated with the expression of fast type IIX and IIB MHC isoforms (Hughes et al. 1993, 1997; Mozdziak et al. 1998; Seward et al. 2001).
Recently in our laboratory, we have shown that mRNA relative expression of MyoD in Soleus and Extensor Digitorum Longus (EDL) muscles and that of MRF4 in Soleus muscle were significantly reduced, whereas myogenin was not changed in either muscle in Wistar rats with monocrotaline-induced HF; thus showing a potential role for MRFs in limb skeletal muscle myopathy during this syndrome (Carvalho et al. 2006). It would also be interesting to analyse whether MRFs gene expression in diaphragm, because of the fact that during HF, this muscle's work tends to increase both at rest and during exercise whereas limb muscle work tends to decrease (Tikunov et al. 1997). Therefore, this investigation was undertaken to examine MRFs mRNA and MHC protein expression in diaphragm skeletal muscle of rats with monocrotaline-induced HF.
Materials and methods
Experimental model
Fifteen weaned male Wistar rats (80–100 g) were obtained from the Central Animal House at São Paulo State University. Heart failure was experimentally induced in nine rats (HF group) by a single intra-peritoneal injection of 30 mg/kg monocrotaline, a widely accepted HF model (Vescovo et al. 1989, 1998; Dalla Libera et al. 1999, 2001, 2004; Leineweber et al. 2002). Monocrotaline is a pyrrolizidine alkaloid that induces pulmonary hypertension with severe right ventricle hypertrophy and failure (Vescovo et al. 1989; Reindel et al. 1990) without itself producing direct changes in skeletal muscle (Vescovo et al. 1998). Monocrotaline-treated rats were allowed to eat freely from a supply of standard rat chow. Six controls rats were injected with saline and fed the same amount of food as consumed by the HF rats on the previous day. Heart failure and Control groups were studied after the development of tachypnea and laboured respiration in the HF group, which occurred 22 days after monocrotaline administration. Heart failure was documented at killing by the presence of pleural and peritoneal effusions, and severe atrial and ventricular hypertrophy and dilatation. At time of the study, all animals were anaesthetized with sodium pentobarbital (50 mg/kg), and killed. Body weight (BW) was measured. The left and right portions of the costal diaphragm were isolated and immediately frozen in liquid nitrogen and stored at −80 °C. Left ventricle weight with inter-ventricular septum included (LVW) and right ventricle weight (RVW) normalized to BW (LVW/BW and RVW/BW respectively) were used as ventricular hypertrophy indexes. This experiment was approved by the Ethics Committee of the Bioscience Institute, UNESP, Botucatu, SP, Brazil.
Electrophoretic separation of MHC
Myosin heavy chains isoform analysis was performed by sodium dodecyl sulphate polyacrylamide gel electrophoresis (SDS-PAGE). Six to ten serial cross sections (12 μm thick) of frozen left costal diaphragm were placed in 450 μl of a solution containing 10% (wt/vol) glycerol, 5% (v/v) 2-mercaptoethanol, 2.3% (wt/vol) SDS and 0.9% (wt/vol) Tris–HCl (pH6.8) for 10 min at 60 °C. Small quantities of the extracts (6 μl) were loaded on a 7–10% SDS-PAGE separating gel with a 4% stacking gel, run overnight (19–21 h) at 120 V and silver stained. Myosin heavy chains isoforms were identified according to molecular mass and their relative percentages were quantified by densitometry. Identification of fast and slow isoforms was accomplished by comigration of EDL muscle samples with a control animal used as pattern.
RT- PCR analysis of mRNA for MRF
Total RNA was extracted from right portions of the costal diaphragm muscles with TRIzol Reagent (Invitrogen Life Technologies, Carlsbad, CA, USA), which is based on the guanidine thiocyanate method. Frozen muscles were mechanically homogenized on ice in 1 ml of ice-cold TRIzol reagent. Total RNA was solubilized in Rnase-free H2O, incubated in Dnase I (Invitrogen Life Technologies, Carlsbad, CA, USA) to remove any DNA present in the sample, and quantified by measuring optical density (OD) at 260 nm. RNA purity was ensured by obtaining an OD ratio of approximately 2.0 at 260–280 nm. Two micrograms of RNA were reverse transcribed with random hexamer primers and Superscript II RT in a total volume of 21 μl, according to standard methods (Invitrogen Life Technologies). Control No RT reactions were performed in which the RT enzyme was omitted. The Control No RT reactions were PCR amplified to ensure no DNA contamination of the RNA. One microlitre of cDNA was then amplified using 0.2 mm of each primer (Table 1), 1× PCR buffer minus Mg, 1.5 mm of MgCl2, 0.2 mm of deoxyribonucleotide triphosphates and 1 unit of Platinum Taq DNA Polymerase (Invitrogen Life Technologies) in a final volume of 25 μl.
Table 1.
Oligonucleotide primers used in PCR amplification of reverse transcribed RNA
| Product | Accession no. | Sequence | Start position | TA (°C) | Cycles | PCR length (bp) |
|---|---|---|---|---|---|---|
| MyoD | NM_176079 | 5′-GACGGCTCTCTCTGCTCCTT | 259 | 60 | 32 | 543 |
| 5′-GTCTGAGTCGCCGCTGTAGT | 801 | |||||
| Myogenin | NM_017115 | 5′-TGCCACAAGCCAGACTACCCACC | 828 | 63 | 31 | 245 |
| 5′-CGGGGCACTCACTGTCTCTCAA | 1072 | |||||
| MRF-4 | NM_013172 | 5′-AGAGACTGCCCAAGGTGGAGATTC | 471 | 63 | 32 | 272 |
| 5′-AAGACTGCTGGAGGCTGAGGCATC | 742 | |||||
| Cyclophylin | M19533 | 5′-ACGCCGCTGTCTCTTTTC | 9 | 57.7 | 32 | 440 |
| 5′-TGCCTTCTTTCACCTTCC | 431 |
TA, annealing temperature.
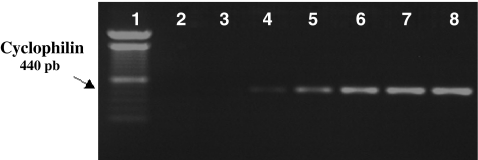
After reverse transcriptase reaction, the first-strand cDNA mixture was subjected to polymerase chain reaction. Target cDNA (MyoD, myogenin, MRF4 and cyclophilin) were amplified in different tubes by using aliquots from total cDNA. The number of polymerase chain reaction cycles was adjusted to avoid amplification system saturation. It is important to select the appropriate number cycles so that the amplification product is clearly visible on an agarose gel and can be quantified, but also that amplification is on exponential range and has not a plateau yet. This standard was realized to each specific PCR amplification (Figure 1). Primer pairs for MyoD were designed from sequences published in GenBank; myogenin and MRF4 primer sequences were as per Smith et al. (1994). Amplification products were identified by their sizes after electrophoresis on 1.0% agarose gel and stained with ethidium bromide. Images were captured and the bands corresponding to each gene were quantified by densitometry as Integrated Optical Density. The PCR products were run in duplicate on a different gel for each gene, and results averaged. The PCR products were normalized to the housekeeping gene cyclophilin (Alway et al. 2002; Siu et al. 2004).
Figure 1.
Representative gel of cyclophilin to determination the number cycles during PCR. Determination of number of cycles for the cyclophilin (1 = pattern molecular weight, 2 = 16 cycles; 3 = 20 cycles; 4 = 24 cycles; 5 = 28 cycles, 6 = 32 cycles; 7 = 36 cycles; 8 = 40 cycles). Product of cyclophilin PCR with 440 bp. We used 32 cycles because of the exponential phase.
Statistical methods
Data are expressed as mean ± standard error (SE). Comparisons were made between Control and HF groups. The Student's unpaired t-test was used in to analysis MRF gene expression. Myosin heavy chain isoform percentages were submitted to multivariate statistical analysis of repeated measures for two independents groups (Profile Analysis) and the Bonferroni test. Significance level was P < 0.05.
Results
Anatomical data
Table 2 shows anatomical data from Control and HF groups. At 22 days, all monocrotaline-treated rats showed signs of HF at postmortem examination including atrium hypertrophy, right ventricular hypertrophy (RVW/BW ≥ 0.80), ascite, pleural effusions and liver congestion. No alterations were found in control rats.
Table 2.
Experimental group anatomical data
| Experimental groups | ||
|---|---|---|
| Control (n = 6) | HF (n = 9) | |
| BW (g) | 158.4 ± 3.5 | 154.6 ± 8.4 |
| LV wt (g) | 0.37 ± 0.006 | 0.45 ± 0.02* |
| RV wt (g) | 0.10 ± 0.007 | 0.34 ± 0.02*** |
| AT wt (g) | 0.06 ± 0.005 | 0.1 ± 0.01** |
| LV/Body wt (mg/g) | 2.35 ± 0.04 | 2.99 ± 0.14* |
| RV/Body wt (mg/g) | 0.65 ± 0.05 | 2.22 ± 0.08*** |
| AT/Body wt (mg/g) | 0.38 ± 0.03 | 0.65 ± 0.01* |
| LV w/d | 4.12 ± 0.04 | 4.69 ± 0.054*** |
| RV w/d | 4.14 ± 0.021 | 4.78 ± 0.07* |
| AT w/d | 3.40 ± 0.22 | 5.24 ± 0.002** |
| Liver w/d | 3.16 ± 0.07 | 3.59 ± 0.036*** |
| Lung w/d | 4.83 ± 0.18 | 5.18 ± 0.17 |
Values are means ± SE.
n, number of animals; HF, heart failure group; BW, body weight; LV, left ventricle weight; RV, right ventricle weight; AT, atrium weight; and w/d, wet-to-dry weight.
P < 0.05, **P < 0.001, ***P < 0.0001: statistical significance vs. control group.
There was no significant difference in BW between HF and control groups. Heart weight was greater in HF than in control group, as demonstrated by LVW, RVW and atrium (AT) and heart hypertrophy indexes (LVW/BW, RVW/BW and ATW/BW). There was no significant difference in lung wet/dry ratio between control and HF groups. The wet RV, LV, AT and liver wet/dry ratio were greater in HF than in control group.
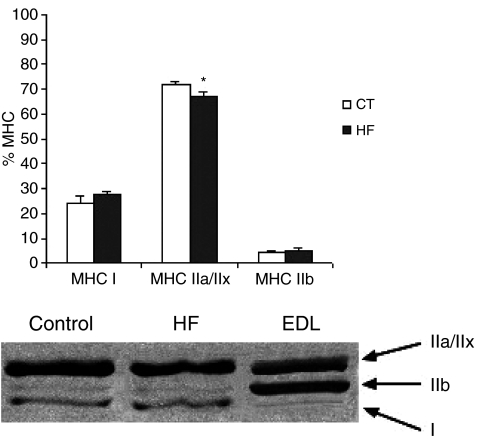
MHCs electrophoretic pattern
In diaphragm muscle, three MHC isoforms were separated, MHC I, MHC IIa/MHC IIx and MHC IIb. The difference in electrophoretic migration between MHC IIa and MHC IIx was very small, and it was not possible to quantify them separately. Consequently, we collapsed the sum of MHC IIa and MHC IIx (Bernocchi et al. 2003). MHC I and MHC IIb were not different between groups (CT = 23.97 ± 2.96%vs. HF = 27.86 ± 1.27% and CT = 4.24 ± 2.02%vs. HF = 4.93 ± 1.87% respectively). MHC IIa/IIx were lower in HF than in CT (CT = 71.79 ± 0.97%vs. HF = 67.21 ± 1.36%, P < 0.05; Figure 2).
Figure 2.
Percentage distribution of myosin heavy chain (MHC), MHC I, MHC IIa/IIx and MHC IIb in diaphragm muscle from control and heart failure groups. Control Extensor Digitorum Longus muscle was used as a pattern. *P < 0.05 vs. control group P < 0.05.
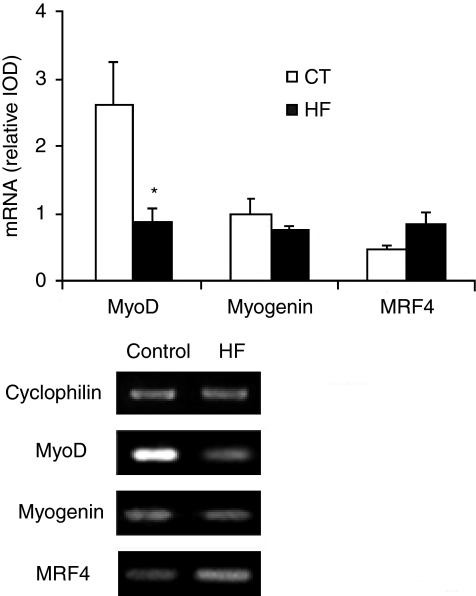
MRF mRNA levels in diaphragm estimated by semi-quantitative RT-PCR
MyoD mRNA levels were lower in HF than in CT (CT = 2.63 ± 0.63 vs. HF = 0.88 ± 0.19, P < 0.05; Figure 3). Myogenin expression was similar in both groups (CT = 1.0 ± 0.21 vs. HF = 0.74 ± 0.08). MRF4 expression was similar in both groups (CT = 0.85 ± 0.05 vs. HF = 0.74 ± 0.16). The MyoD to Myogenin mRNA ratio was less in HF than in CT (CT = 2.90 ± 0.79 vs. HF = 1.30 ± 0.31, P < 0.05).
Figure 3.
MyoD, myogenin and MRF4 mRNA content from rat diaphragm muscle estimated by RT-PCR in Control and heart failure groups. Samples were run in duplicate on different gels for each gene, and results averaged. PCR products were visualized with ethidium bromide staining. PCR quantification was by densitometric analysis of the product as integrated optical density. Gene expressions were normalized to cyclophilin from the same RT product. Normalized data are expressed as means ± SE. *Data are significantly different from Controls at P < 0.05.
Discussion
This investigation was undertaken to examine MRFs mRNA and MHC protein expression in the rat diaphragm skeletal muscle with monocrotaline-induced HF. This is the first study showing that HF decreased the relative mRNA level of MyoD without changes in mRNA relative expression of myogenin and MRF4 in the diaphragm muscle. Although during HF, diaphragm muscle work tends to increase both at rest and during exercise whereas limb muscle work tends to decrease (Tikunov et al. 1997), we have shown similar results in a previous study for MyoD and Myogenin mRNA relative expression in Soleus and EDL limb muscles using the monocrotaline HF model.
There is substantial evidence suggesting that MRFs are important regulators in the expression of muscle-specific proteins (Hughes et al. 1993; Parker et al. 2003). Myogenin is expressed at higher levels than MyoD in slow muscles, whereas the opposite is true for fast muscles (Hughes et al. 1993; Voytik et al. 1993). Similarly, MyoD is associated with expression of fast type IIx and IIb MHC isoforms (Hughes et al. 1993, 1997; Seward et al. 2001).
Alterations in MRF expression may be directly involved in controlling fibre type-specific gene expression in response to external signals such as hypothyroidism, chronic low-level frequency stimulation, cross-reinnervation, denervation and hindlimb suspension (Eftimie et al. 1991; Mozdziak et al. 1998; Carlsen & Gundersen 2000). In our study, the reduction in MyoD mRNA expression might be associated with the decrease in fast MHC IIa/IIx protein isoform expression seen in diaphragm muscle. The degree of decline in MyoD mRNA appeared more extensive than MHC IIa/IIx and this fact may be related to the different methods used to analyse the MRFs and MHCs.
To our knowledge, few studies have analysed the mRNA MRFs expression that might be associated with alterations in MHC protein isoform expression in diaphragm muscle during HF. Staib et al. (2002) showed a change in MHC protein isoform expression in diaphragm of mice MyoD −/−. MyoD deletion resulted in a significant shift from MHC IIb toward both MHC IIa and MHC IIx showing a shift in diaphragm MHC phenotype from fast to slow. Additionally, a study in diaphragm muscle from rats subjected to mechanical ventilation showed a decreased MyoD mRNA level and diminished fast MHC IIa and IIb mRNA expression; the authors suggested muscle phenotypic adaptation toward a slower profile considering the reduced MyoD/myogenin ratio, as observed in our study (Racz et al. 2003).
The causes of down-regulation in MyoD mRNA expression during HF are still unknown; however, neurohormones and cytokine activation may contribute (Anker et al. 1999). This last point has undergone considerable debate because tumour necrosis factor-alpha (TNF-α) is markedly increased in humans and animals with chronic HF (Anker et al. 1999; Levine et al. 1990; McMurray et al. 1991). Li et al. (2000) demonstrated that elevated circulating levels of TNF-α provoke contractile dysfunction in the diaphragm through an endocrine mechanism which is thought to be mediated by oxidative stress. One hallmark of TNF-α action is the activation of nuclear factor Kappa B (NFκB), a ubiquitous transcription factor normally inactive and sequestered in the cytoplasm through association with IκB (Guttridge et al. 2000). TNF-α exposure leads to the degradation of IκB, allowing NFκB translocation to the nucleus where it down-regulates MyoD mRNA at a posttranscriptional level (Israël 2000). On the other hand, the cooperative activity of TNF/Interferon (IFN) could reduce MyoD mRNA expression, mediated the repression of the fast MyHC promoter (Acharyya et al. 2004). Given that MyoD binding to the fast MyHC promoter is required for myosin expression in fast-twitch muscles (Wheeler et al. 1999), it is tempting to speculate that cytokine-induced suppression of fast MyHC transcription is regulated by NF-κB through the inhibited synthesis of MyoD.
This mechanism may partially explain the down-regulation of MyoD that we found in diaphragm muscle. However, further studies need to be conducted to demonstrate this mechanism during HF.
In our investigation, myogenin and MRF4 mRNA relative expression did not change during HF. It has been shown that myogenin is involved with oxidative gene expression and metabolic enzyme activity (Hughes et al. 1999; Ekmark et al. 2003; Siu et al. 2004), whereas MRF4 is expressed mainly after birth and is likely to have a role in skeletal muscle maintenance (Hughes et al. 1997). The concept that MRF4 is involved in regulating maturation events and maintaining adult skeletal muscle is further sustained by the fact that MRF4 is not expressed at substantial levels in limb until very late in foetal development (Hinterberger et al. 1991) and is also present at higher levels in postnatal muscle (Voytik et al. 1993; Hughes et al. 1997). Thus, both myogenin and MRF4 seem not to be involved with changes in fibre type-specific myosin heavy chain expression during HF.
In summary, our results show that in HF, MyoD is selectively down-regulated, which might be associated with alterations in MHC IIa/IIx content. It is interesting that only MyoD is responsive, suggesting that this protein might be a key player in diaphragm function in HF. These changes are likely to contribute to diaphragm alterations caused by HF. Further studies are needed to map the complexity of this phenomenon and develop strategies to minimize the effects of HF on diaphragm myopathy.
Acknowledgments
The authors thank José Carlos Georgette and Sueli Cruz Michelin for technical assistance. This work is part of the MSc thesis presented by FLP to Universidade Estadual de Campinas – UNICAMP, in 2005. Grant support: FAPESP (Proc: 04/01516-1).
References
- Acharyya S, Ladner KJ, Nelsen LL, et al. Cancer cachexia is regulated by selective targeting of skeletal muscle gene products. J. Clin. Invest. 2004;114:370–378. doi: 10.1172/JCI20174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen DL, Sartorius CA, Sycuro LK, Leinwand LA. Different pathways regulate expression of the skeletal myosin heavy chain genes. J. Biol. Chem. 2001;276:43524–43533. doi: 10.1074/jbc.M108017200. [DOI] [PubMed] [Google Scholar]
- Alway SE, Degens H, Lowe DA, Krishnamurthy G. Increased myogenic repressor Id mRNA and protein levels in hindlimb muscles of aged rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002;282:R411–R422. doi: 10.1152/ajpregu.00332.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anker SD, Ponikowski PP, Clark AL, et al. Cytokines and neurohormones relating to body composition alterations in the wasting syndrome of chronic heart failure. Eur. Heart J. 1999;20:683–693. doi: 10.1053/euhj.1998.1446. [DOI] [PubMed] [Google Scholar]
- Bernocchi P, Cargnoni A, Vescovo G, et al. Skeletal muscle abnormalities in rats with experimentally induced heart hypertrophy and failure. Basic Res. Cardiol. 2003;98:114–123. doi: 10.1007/s003950300001. [DOI] [PubMed] [Google Scholar]
- Carlsen H, Gundersen K. Helix-loop-helix transcription factors in electrically active and inactive skeletal muscle. Muscle Nerve. 2000;23:1374–1380. doi: 10.1002/1097-4598(200009)23:9<1374::aid-mus8>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Carvalho RF, Cicogna AC, Campos GE, et al. Myosin heavy chain expression and atrophy in rat skeletal muscle during transition from cardiac hypertrophy to heart failure. Int. J. Exp. Pathol. 2003;84:201–206. doi: 10.1046/j.1365-2613.2003.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carvalho RF, Cicogna AC, Campos GE, et al. Heart failure alters MyoD and MRF4 expressions in rat skeletal muscle. Int. J. Exp. Pathol. 2006;87:219–225. doi: 10.1111/j.1365-2613.2006.00475.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalla Libera L, Zennaro R, Sandri M, Ambrosio GB, Vescovo G. Apoptosis and atrophy in rat slow skeletal muscle in chronic heart failure. Am. J. Physiol., Cell Physiol. 1999;277:C982–C986. doi: 10.1152/ajpcell.1999.277.5.C982. [DOI] [PubMed] [Google Scholar]
- Dalla Libera L, Ravara B, Angelini A, et al. Beneficial effects on skeletal muscle of the angiotensin II type 1 receptor blocker irbesartan in experimental heart failure. Circulation. 2001;103:2195–2200. doi: 10.1161/01.cir.103.17.2195. [DOI] [PubMed] [Google Scholar]
- Dalla Libera L, Ravara B, Volterrani M, et al. Beneficial effects of GH/IGF-1 on skeletal muscle atrophy and function in experimental heart failure. Am. J. Physiol., Cell. Physiol. 2004;286:C138–C144. doi: 10.1152/ajpcell.00114.2003. [DOI] [PubMed] [Google Scholar]
- De Sousa E, Veksler V, Bigard X, Mateo P, Serrurier B, Ventura-Clapier R. Dual influence of disease and increased load on diaphragm muscle in heart failure. J. Mol. Cell. Cardiol. 2001;33:699–710. doi: 10.1006/jmcc.2000.1336. [DOI] [PubMed] [Google Scholar]
- Eftimie R, Brenner HR, Buonanno A. Myogenin and MyoD join a family of skeletal muscle genes regulated by electrical activity. Proc. Natl Acad. Sci. USA. 1991;88:1349–1353. doi: 10.1073/pnas.88.4.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ekmark M, Gronevick E, Schjerling P, Gundersen K. Myogenin induces higher oxidative capacity in pre-existing mouse muscle fibers after somatic DNA transfer. J. Physiol. 2003;548:259–269. doi: 10.1113/jphysiol.2002.036228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttridge DC, Mayo MW, Madrid LV, Wang CY, Baldwin AS., Jr NF-kappaB-induced loss of MyoD messenger RNA: possible role in muscle decay and cachexia. Science. 2000;289:2363–2366. doi: 10.1126/science.289.5488.2363. [DOI] [PubMed] [Google Scholar]
- Hinterberger TJ, Sassoon DA, Rhodes SJ, Konieczny SF. Expression of the muscle regulatory factor MRF4 during somite and skeletal myofiber development. Dev. Biol. 1991;147:144–156. doi: 10.1016/s0012-1606(05)80014-4. [DOI] [PubMed] [Google Scholar]
- Hughes SM, Taylor JM, Tapscott SJ, Gurley CM, Carter WJ, Peterson CA. Selective accumulation of MyoD and myogenin mRNAs in fast and slow muscle is controlled by innervation and hormones. Development. 1993;118:1137–1147. doi: 10.1242/dev.118.4.1137. [DOI] [PubMed] [Google Scholar]
- Hughes SM, Koyshi K, Rudnicki M, Maggs AM. MyoD protein is differentially accumulated in fast and slow skeletal muscle fibres and required for normal fibre type balance in rodents. Mech. Dev. 1997;61:151–163. doi: 10.1016/s0925-4773(96)00631-4. [DOI] [PubMed] [Google Scholar]
- Hughes SM, Chi MM, Lowry OH, Gundersen K. Myogenin induces a shift of enzyme activity from glycolytic to oxidative metabolism in muscles of transgenic mice. J. Cell Biol. 1999;145:633–642. doi: 10.1083/jcb.145.3.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israël A. The IKK complex: an integrator of all signals that activate NF-kappaB? Trends Cell Biol. 2000;10:129–133. doi: 10.1016/s0962-8924(00)01729-3. [DOI] [PubMed] [Google Scholar]
- Leineweber K, Brandt K, Wludyka B, et al. Ventricular hypertrophy plus neurohumoral activation is necessary to alter the cardiac beta-adrenoceptor system in experimental heart failure. Circ. Res. 2002;91:1056–1062. doi: 10.1161/01.res.0000045088.59360.b7. [DOI] [PubMed] [Google Scholar]
- Levine B, Kalman J, Mayer L, Fillit HM, Packer M. Elevated circulating levels of tumor necrosis factor in severe chronic heart failure. N. Engl. J. Med. 1990;323:236–241. doi: 10.1056/NEJM199007263230405. [DOI] [PubMed] [Google Scholar]
- Li X, Moody MR, Engel D, et al. Cardiac-specific overexpression of tumor necrosis factor-alpha causes oxidative stress and contractile dysfunction in mouse diaphragm. Circulation. 2000;102:1690–1696. doi: 10.1161/01.cir.102.14.1690. [DOI] [PubMed] [Google Scholar]
- McMurray J, Abdullah I, Dargie HJ, Shapiro D. Increased concentrations of tumor necrosis factor in ‘cachectic’ patients with severe chronic heart failure. Br. Heart J. 1991;66:356–358. doi: 10.1136/hrt.66.5.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozdziak PE, Greaser ML, Schultz E. Myogenin, MyoD, and myosin expression after pharmacologically and surgically induced hypertrophy. J. Appl. Physiol. 1998;84:1359–1364. doi: 10.1152/jappl.1998.84.4.1359. [DOI] [PubMed] [Google Scholar]
- Murre C, McCaw PS, Vaessin H, et al. Interactions between heterologous helix-loop-helix proteins generate complexes that bind specifically to a common DNA sequence. Cell. 1989;58:537–544. doi: 10.1016/0092-8674(89)90434-0. [DOI] [PubMed] [Google Scholar]
- Parker MH, Seale P, Rudnicki MA. Looking back to the embryo: defining transcriptional networks in adult myogenesis. Nat. Rev. Genet. 2003;4:497–507. doi: 10.1038/nrg1109. [DOI] [PubMed] [Google Scholar]
- Racz GZ, Gayan-Ramirez G, Testelmans D, et al. Early changes in rat diaphragm biology with mechanical ventilation. Am. J. Respir. Crit. Care Med. 2003;168:297–304. doi: 10.1164/rccm.200206-541OC. [DOI] [PubMed] [Google Scholar]
- Reindel JF, Ganey PE, Wagner JG, Slocombe RF, Roth RA. Development of morphologic, hemodynamic, and biochemical changes in lungs of rats given monocrotaline pyrrole. Toxicol. Appl. Pharmacol. 1990;106:179–200. doi: 10.1016/0041-008x(90)90239-q. [DOI] [PubMed] [Google Scholar]
- Seward DJ, Haney JC, Rudnicki MA, Swoap SJ. bHLH transcription factor MyoD affects myosin heavy chain expression pattern in a muscle-specific fashion. Am. J. Physiol., Cell Physiol. 2001;280:C408–C413. doi: 10.1152/ajpcell.2001.280.2.C408. [DOI] [PubMed] [Google Scholar]
- Simonini A, Massie BM, Long CS, Qi M, Samarel AM. Alterations in skeletal muscle gene expression in the rat with chronic congestive heart failure. J. Mol. Cell. Cardiol. 1996;28:1683–1691. doi: 10.1006/jmcc.1996.0158. [DOI] [PubMed] [Google Scholar]
- Siu PM, Donley DA, Bryner RW, Alway SE. Myogenin and oxidative enzyme gene expression levels are elevated in rat soleus muscles after endurance training. J. Appl. Physiol. 2004;97:277–285. doi: 10.1152/japplphysiol.00534.2004. [DOI] [PubMed] [Google Scholar]
- Smith CK, II, Janney MJ, Allen RE. Temporal expression of myogenic regulatory genes during activation, proliferation, and differentiation of rat skeletal muscle satellite cells. J. Cell. Physiol. 1994;159:379–385. doi: 10.1002/jcp.1041590222. [DOI] [PubMed] [Google Scholar]
- Staib JL, Swoap SJ, Powers SK. Diaphragm contractile dysfunction in MyoD gene-inactivated mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2002;283:R583–R590. doi: 10.1152/ajpregu.00080.2002. [DOI] [PubMed] [Google Scholar]
- Tikunov BA, Mancini D, Levine S. Changes in myofibrillar protein composition of human diaphragm elicited by congestive heart failure. J. Mol. Cell. Cardiol. 1996;28:2537–2541. doi: 10.1006/jmcc.1996.0245. [DOI] [PubMed] [Google Scholar]
- Tikunov BA, Mancini D, Levine S. Chronic congestive heart failure elicits adaptations of endurance exercise in diaphragmatic muscle. Circulation. 1997;95:910–916. doi: 10.1161/01.cir.95.4.910. [DOI] [PubMed] [Google Scholar]
- Vescovo G, Jones SM, Harding SE, Poole-Wilson PA. Isoproterenol sensitivity of isolated myocytes from rats with monocrotaline-induced right-sided hypertrophy and heart failure. J. Mol. Cell. Cardiol. 1989;21:1047–1061. doi: 10.1016/0022-2828(89)90803-1. [DOI] [PubMed] [Google Scholar]
- Vescovo G, Ceconi C, Bernocchi P, et al. Skeletal muscle myosin heavy chain expression in rats with monocrotaline-induced cardiac hypertrophy and failure. Relation to blood flow and degree of muscle atrophy. Cardiovasc. Res. 1998;39:233–241. doi: 10.1016/s0008-6363(98)00041-8. [DOI] [PubMed] [Google Scholar]
- Voytik SL, Przyborski M, Badylak SF, Konieczny SF. Differential expression of muscle regulatory factor genes in normal and denervated adult rat hindlimb muscle. Dev. Dyn. 1993;198:214–224. doi: 10.1002/aja.1001980307. [DOI] [PubMed] [Google Scholar]
- Wheeler MT, Snyder EC, Patterson MN, Swoap SJ. An E-box within the MHC IIB gene is bound by MyoD and is required for gene expression in fast muscle. Am. J. Physiol. 1999;276:C1069–C1078. doi: 10.1152/ajpcell.1999.276.5.C1069. [DOI] [PubMed] [Google Scholar]
- Wilson JR, Mancini DM. Factors contributing to the exercise limitation of heart failure. J. Am. Coll. Cardiol. 1993;22:93A–98A. doi: 10.1016/0735-1097(93)90469-h. [DOI] [PubMed] [Google Scholar]