Abstract
Inhalational anthrax is a rare but potentially fatal infection in man. The common marmoset (Callithrix jacchus) was evaluated as a small non-human primate (NHP) model of inhalational anthrax infection, as an alternative to larger NHP species. The marmoset was found to be susceptible to inhalational exposure to Bacillus anthracis Ames strain. The pathophysiology of infection following inhalational exposure was similar to that previously reported in the rhesus and cynomolgus macaque and humans. The calculated LD50 for B. anthracis Ames strain in the marmoset was 1.47 × 103 colony-forming units, compared with a published LD50 of 5.5 × 104 spores in the rhesus macaque and 4.13 × 103 spores in the cynomolgus macaque. This suggests that the common marmoset is an appropriate alternative NHP and will be used for the evaluation of medical countermeasures against respiratory anthrax infection.
Keywords: Bacillus anthracis, inhalational, marmoset
Anthrax is an infection caused by the Gram-positive, aerobic, spore-forming bacterium Bacillus anthracis. Infection can follow intradermal inoculation, ingestion or inhalation of spores. The pathogenesis of the disease varies depending on the route of infection and the exposure dose, although, in a susceptible host, bacteriaemia is the common final sequela. For a disease, such as anthrax, which is a rare but potentially fatal infection in man, much emphasis is placed on satisfactory animal models for the development of medical countermeasures, since efficacy testing in conventional phase III clinical trials is neither feasible nor ethical. A number of species have been used to test the efficacy of prophylaxes and therapies for anthrax, including mouse (Turnbull 1986; Welkos et al. 1986; Varughese et al. 1999; Flick-Smith et al. 2002, 2005), guinea pig (McBride et al. 1998; Fellows et al. 2001), Syrian hamster (Rodentia spp.) (Fellows et al. 2002), rabbit (Lagomorpha spp.) (Fellows et al. 2001; Pitt et al. 2001) and non-human primates (NHP; Fellows et al. 2001; Ivins et al.1992, 1996, 1998). Amongst the latter, macaques (cynomolgus and rhesus) have been used, and there is a single reference to a trial in chimpanzees (Albrink & Goodlow 1959); of these NHP, most work has been carried out in rhesus macaques. Studies with macaques at high levels of biocontainment, however, pose particular challenges and are constrained by size and maintenance.
The achievement of robust animal models of human anthrax infection has not been easy. Mice have been found to be particularly susceptible to the capsule surrounding the bacteria (Welkos et al. 1986; Flick-Smith et al. 2005), so that the assessment of any prophylaxis or therapy based on, for example, inactivating the toxins of anthrax, is difficult but can be circumvented by using a non-encapsulated anthrax strain; guinea-pigs are particularly sensitive to aerosol challenge with the organism, whilst variable protection against parenteral challenge has been seen in guinea pigs vaccinated with the current licensed anthrax vaccine (Little & Knudson 1986; Turnbull et al. 1986, 1988; Ivins et al. 1994; Fellows et al. 2001). Rhesus macaques represent a highly evolved model, but have been observed to have some inherent resistance to aerosolized anthrax infection, which may be age related, since juvenile macaques appear to be more resistant than mature adults (unpublished data).
Nevertheless, the rhesus macaque (Macaca mulatta) has been used extensively in anthrax research, with the emphasis to date being on the assessment of vaccine efficacy against inhalational anthrax (Belton et al. 1956; Henderson et al. 1956; Albrink & Goodlow 1959; Friedlander et al. 1993; Fritz et al. 1995; Ivins et al. 1996, 1998). The pathology of the inhalational form of the disease in this species is similar to that of humans, making it a relevant model (Albrink et al. 1960; Turnbull et al. 1986; Fritz et al. 1995). The pathology of inhalational anthrax in cynomolgus macaques (Macaca fascicularis) has also been reported (Brachman et al. 1966; Dalldorf & Kaufmann 1966; Vasconcelos et al. 2003).
Much of the existing data on the NHP response to anthrax infection has arisen from vaccine studies with rhesus macaques. Survival rates in excess of 85% were reported for macaques given the current US licensed anthrax vaccine adsorbed (AVA), up to 100 weeks prior to challenge, whilst full protection against aerosol challenge has been reported for macaques given either the AVA (Ivins et al. 1996, 1998) or newer recombinant Protective Antigen (rPA) (Ivins et al. 1998; Williamson et al. 2005) vaccines. These studies have also generated data, which have allowed some characterization of the macaque immune response and a comparison with man, necessary to identify immune correlates of protection (Rowland et al. 2001; Williamson et al. 2005). Currently, there is an urgent requirement to evaluate the efficacy of post-exposure vaccination in conjunction with antibiotic therapy, in the rabbit and/or NHP models, in order to predict the human response.
In recent years, the common marmoset (Callithrix jacchus), a New World NHP species, has become more widely used in applied biomedical research (Smith et al. 2001). At Dstl Porton Down, a substantial amount of work has already been carried out to investigate the marmoset as a model in immunological research, as part of a larger body of work to investigate the potential long-term effects of multiple vaccination and pyridostigmine administration in the context of Gulf War deployment. During this programme, marmosets were demonstrated to respond to the existing UK licensed anthrax vaccine, suggesting they may have utility as a potential efficacy model of anthrax and reagents for the detection of marmoset immune markers, by immunoassay and by flow cytometric analysis have been identified (Griffiths et al. 2006; Hornby et al. 2006). In addition, in comparison to macaque species, the marmoset's small size and relative ease of maintenance in captivity have implications for housing and husbandry under the stringent laboratory conditions needed for the investigation of dangerous pathogens, such as anthrax.
The present study was designed to evaluate the marmoset as a model of anthrax infection and bridge this to published data for the rhesus and cynomolgus macaques and human. This model will then be used in the enhanced development of relevant antimicrobials and vaccines.
Materials and methods
Experimental animals
All animal studies were carried out in accordance with the Scientific Procedures Act (Animals) 1986, and the Codes of Practice for the Housing and Care of Animals Used in Scientific Procedures, 1989. The licence application underwent a local ethical review process before submission to the UK Home Office.
Common marmosets (C. jacchus) were obtained from the Dstl Porton breeding colony as healthy sexually mature animals, aged between 36 and 60 months old (weighing between 320 and 480 g at the start of the trial). They were housed as female/vasectomized male pairs in specially adapted cages within a negative pressure rigid-walled isolator. The animals were given species-appropriate environmental enrichment such as access to forage mix containing preferred food items, sleeping boxes and puzzle feeders. They were allowed to acclimatize to the isolator for 1 day prior to the start of the trial. Throughout the trial, regular checks (at least every 4 h) were maintained and behaviour, vocalization and activity characteristics monitored. A pro-forma was used to record the behaviour.
Spore preparation
Spores of the virulent Ames strain of Bacillus anthracis were prepared on manganese sulphate sporulation agar in Roux bottles as previously described (Jones et al. 1995), except that, to avoid inducing premature germination, the isopropanol wash and heat shock treatment were omitted. The spore pellets were washed three times in sterile distilled water and finally made up to 150 ml in sterile distilled water. The spore concentration was determined to be 6.71 × 108/ml.
Aerosol generation
A 3-jet Collison nebulizer was used to generate aerosol particles suspended in sterile distilled water. The particle size of the aerosol produced in this manner is approximately 1–3 μm in range (as determined by an Anderson sampler). The aerosol was conditioned in a modified Henderson apparatus (Henderson 1952; Druett 1969) and the aerosol stream was maintained at 50–55% relative humidity and 22 ± 3 °C.
Animal challenges
Marmosets were anaesthetized with 25 mg/kg ketamine intra-muscularly (i.m.) prior to exposure and were challenged either singly or in pairs. They were placed in a head-only exposure chamber (plethysmograph tube) and exposed for 10 min to a dynamic aerosol. The total accumulated tidal volume and minute volume for each animal during challenge was determined by whole body real-time plethysmography with a Fleisch pneumotachograph (EMMS, Bordon, Hampshire, UK). Samples of the aerosol stream were collected for 1 min during exposures using all-glass impingers (AGI) into distilled water to determine the bacterial concentrations per ml. The exposure dose of B. anthracis per animal was calculated using the formula:
where a is the impinger count (cfu/ml); b the impinger volume (ml); c the minute volume of animal (ml/min); d the exposure time (min); e the impinger flow rate (l/min); f the impinger sample time (min).
This was the estimated dose the animal has been exposed to but not necessarily retained. (The minute volume for one animal was not recorded and the total exposed dose for this animal was calculated on a minute volume of 40 ml/min). All animal challenges were conducted within a rigid half-suit isolator sited within a containment level 3 animal laboratory. Following exposure, animals were transferred from the challenge isolator (in a safe procedure) and returned to their home cages, within the housing isolator, and allowed to recover from the anaesthetic. During recovery, animals were placed on a bedding sheet under an infrared lamp. Post-exposure marmosets were monitored 4-hourly, day and night and video footage of their activity in the home cage was collected continuously. On the appearance of a pre-determined set of clinical signs, which included dyspnoea, partial paralysis, piloerection and unresponsiveness to stimuli animals were humanely culled by terminal anaesthesia (sodium pentabarbitone overdose i.m.).
Lethal dose determination (LD50): The Dixon method for small samples (Dixon & Fotheringhamn 1993) was employed to estimate the LD50 for B. anthracis Ames strain in the marmoset. This was repeated three times to obtain three separate estimates. A log increase or decrease in cfu was used at each step-up or step-down stage. All challenged animals were observed for a period of up to 10 days post-infection.
Presence of viable bacteria in organs and blood
At the end of the study, samples of lung, liver, spleen, kidney, brain, lymph node tissue (mesenteric, tracheo-bronchial, mediastinal) and blood were taken. Organs were removed aseptically and homogenized in 2 ml nutrient broth in a tissue homogenizer (Medicon, BD Biosciences, UK). The presence or absence of bacteria was determined after plating of 0.25 ml tissue homogenate (after 1:10 serial dilutions in nutrient broth) onto blood agar plates (in duplicate). Plates were incubated for 48 h at 37 °C in air prior to observation. For enumeration of bacteria in blood, 0.1 ml of blood was diluted in nutrient broth and plated out in duplicate as described above. Counts were expressed as cfu per ml of blood.
Histopathological studies
Tissues were fixed in 10% buffered formalin solution and processed for paraffin wax embedding using standard techniques. Sections (5 ± 2 μm) were cut and stained with haematoxylin and eosin (H&E). Selected sections were Gram stained.
Results
Determination of the LD50 of Bacillus anthracis Ames strain in the marmoset
The results for animal weight, exposure dose, plethysmography data and time to death are summarized in Table 1. A total of 12 animals were exposed to challenge doses ranging from 1.4 × 101 to 1.9 × 105 cfu B. anthracis. Six animals survived (50%) to the experimental end-point (10 days post-challenge). Animal age did not affect survival.
Table 1.
Summary of animal weight, age, plethysmography data, exposure dose and time to death data
| Gender | Age (years) | Weight (g) | Minute volume (ml/min) | Colony forming unit per ml (aerosol) | Total exposed dose (cfu) | Time to death (h) |
|---|---|---|---|---|---|---|
| F | 6 | 444 | 45.6 | 4.98 × 105 | 1.9 × 105 | 40 |
| M | 6 | 384 | NA | 3.41 × 105 | 1.1 × 105 | 69 |
| M | 5 | 478 | 56.7 | 2.95 × 105 | 1.4 × 105 | 140 |
| M | 6 | 340 | 72.3 | 2.67 × 104 | 1.6 × 104 | S |
| F | 3 | 372 | 65.5 | 2.68 × 104 | 1.5 × 104 | S |
| F | 4 | 394 | 61.8 | 2.33 × 104 | 1.2 × 104 | S |
| F | 5 | 342 | 65.1 | 4.40 × 104 | 2.4 × 104 | 72 |
| F | 4 | 342 | 79.6 | 5.57 × 103 | 3.7 × 103 | 76 |
| M | 6 | 428 | 76.3 | 3.97 × 103 | 2.5 × 103 | S |
| F | 6 | 452 | 92.1 | 2.97 × 102 | 2.3 × 102 | 60 |
| M | 4 | 324 | 121.3 | 4.19 × 102 | 4.2 × 102 | S |
| M | 4 | 370 | 66.6 | 4.90 × 101 | 1.4 × 101 | S |
S, survived; NA, not available.
A geometric mean LD50 value of 1.47 × 103 cfu (95% confidence limits 7.19–2.95 × 105) was calculated by obtaining a mean of the LD50 values from each of the staircase procedures (n = 3). The LD50 values obtained were normalized (logging values), as these LD50 values were not normally distributed. Thus, a dose of 1 × 105 cfu approximates to 100 LD50, with a 1.0% chance that this dose will fall in the 95% confidence interval of 1 LD50 range. No significant difference in susceptibility to B. anthracis could be detected between males and females in this experiment; however, the power of the test (Fishers exact test) was low.
Clinical observations
Times to death ranged from 40 to 140 h and did not correlate statistically with exposed dose. Clinical signs appeared very precipitously (usually within an hour prior to euthanasia or death) and included dyspnoea, disorientation and a reduced response to external stimuli. When such clinical signs were observed, the animal was promptly humanely culled.
Gross pathology
Gross pathological observations from the six animals which died from disease within 10 days of challenge included: splenomegaly (2/6 animals), hepatomegaly (1/6), lung haemorrhages (3/6) and enlarged, haemorrhagic mediastinal and tracheo-bronchial lymph nodes (1/6). Gross pathological features observed in the six animals which survived until day 10 post-infection were fewer but included lung haemorrhages (1/6) and minor meningeal haemorrhages (1/6).
Histopathology
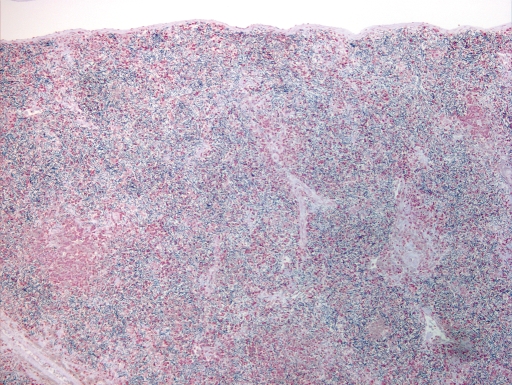
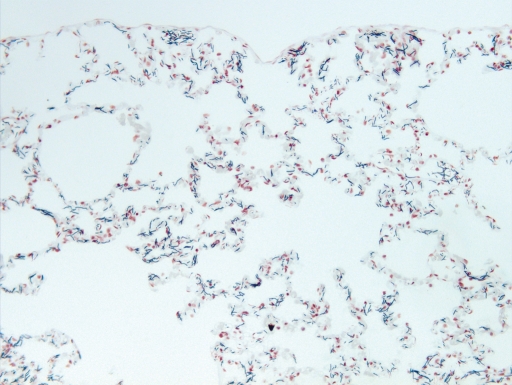
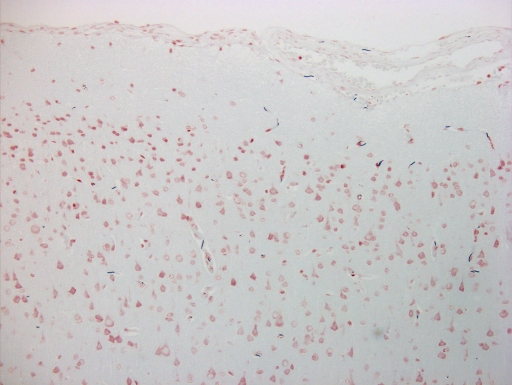
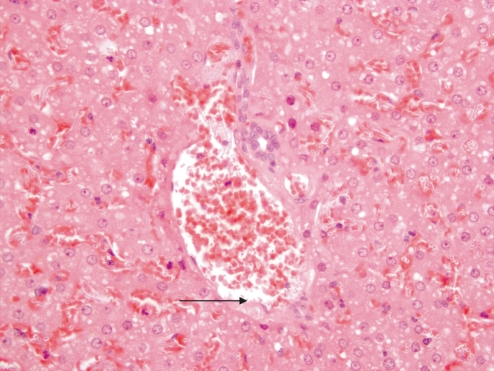
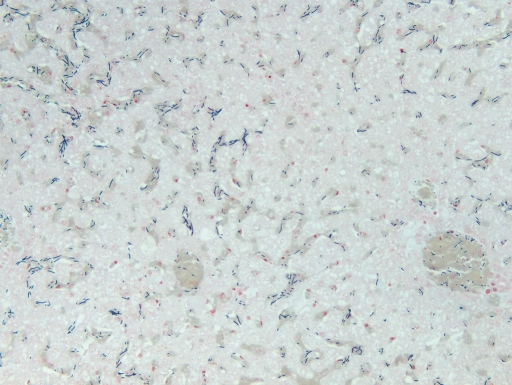
Histopathological changes observed in those animals that died before the end of the experiment (day 10 post-infection), are summarized in Table 2. Histopathological observations in these animals included interstitial pneumonia, diffuse hepatic congestion and fibrin deposition with mats of bacilli in the spleen (Figures 1–5). The spleen was the organ most affected, with numerous bacilli visible. Scattered bacilli were also seen in the brain (Figure 2) and numerous bacilli were seen within the capillaries in the lungs (Figure 5).
Table 2.
Summary of the histopathological changes in animals that died before the end of the experiment (up to day 10 post-infection)
| Organ | Microscopical findings | Number affected (%) |
|---|---|---|
| Brain | Intravascular bacteriawithin meningesand neuropil Gliosis with widening ofVirchow–Robin's spaces | 4/6 (66) 1/6 (16) |
| Heart | Congestion, haemorrhage,fibrin and oedema | 2/6 (33) |
| Liver | Sinusoid bacteria; acuteinflammation, single cellnecrosis, fibrinoid necrosisof vessel walls | 5/6 (83) |
| Lung | Extra- and intra-vascularbacteria; congestion, oedema,haemorrhage, acuteinflammation and fibrin | 5/6 (83) |
| Spleen | Extracellular bacteria;lymphoid depletion, necrosis, fibrin and haemorrhage,acute inflammation | 6/6 (100) |
| Lymph node (mediastinal and tracheo-bronchial) | Intra-vascular bacteria;fibrin and secondary follicular development | 2/2 (100) |
| Kidney | Extravascular bacteria; fibrin;haemorrhage, congestion; some tubular necrosis andacute inflammation | 4/6 (66) |
Figure 1.
Gram stained spleen section from marmoset taken at necropsy (day 4 post-challenge) infected with 1.0 × 103 cfu by the aerosol route. Numerous black bacilli were evident. 10× magnification.
Figure 5.
Gram stained lung section from marmoset taken at necropsy (day 4 post-challenge) infected with 1.0 × 103 cfu by the aerosol route. Mild alveolar congestion was evident with numerous bacilli within capillaries. 20× magnification.
Figure 2.
Haemotoxylin and eosin stained brain (cerebral cortex) section from marmoset taken at necropsy (day 4 post-challenge) infected with 1.0 × 103 cfu by the aerosol route. Scattered bacilli are evident by Gram staining within capillaries and leptomeningeal vessels. 20× magnification.
Figure 3.
Haemotoxylin and eosin stained liver section from marmoset taken at necropsy (day 4 post-challenge) infected with 1.0 × 103cfu by the aerosol route. Evidence of fibrinoid necrosis of the hepatic vessel (arrowed) and numerous bacilli and neutrophils are present. 40× magnification.
Figure 4.
Gram stained liver section from marmoset taken at necropsy (day 4 post-challenge) infected with 1.0 × 103 cfu by the aerosol route. Numerous bacilli within sinusoids and vessels were evident. 20× magnification.
Mediastinal and tracheo-bronchial lymph tissue (where recovered), showed secondary follicular development with focal fibrin deposition, within a germinal centre. Relatively small numbers of bacilli were present within vessels.
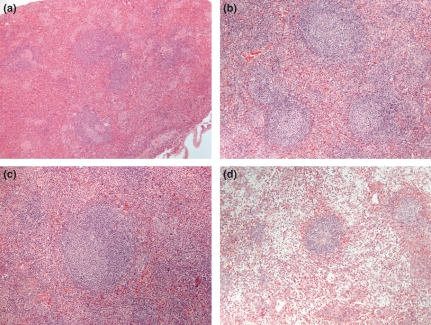
The lymphoid tissues, especially the spleen, provided the greatest predictor as to the overall condition of the animal. A grading scale was applied to the spleen to enhance and simplify the interpretation of samples shown in Figure 6 and comprised four stages:
Figure 6.
(a–d) Splenic grading system (a) Grade 1: normal spleen, (b) Grade 2: cellularly dense red pulp with white pulp lymphoid follicle, (c) Grade 3: less dense red pulp with prominent germinal centre, (d) Grade 4: depleted red pulp replaced with fibrin and bacilli. All at 10× magnification.
Normal spleen
Expanded germinal centres present, some quiescent white pulp, no megakaryocytes noted.
Expanded germinal centre with mitoses noted throughout the spleen; no megakaryocytes present.
Depleted red and white pulp, lacking in macrophage and lymphocyte populations.
All animals that died during the trial were found to have splenic changes graded as 3. All animals surviving to the end of the trial had splenic changes graded as 2 or below. Histological examination of those animals which survived to the end of the trial, and were culled, showed predominantly normal histology with no pathology in organs other than the spleen, regardless of the initial exposed dose.
Bacterial cell counts in tissues
Bacillus anthracis was present in the blood of all animals that died before 10 days post-infection (counts >105 cfu/ml), with the exception of one animal that received 1 × 104 cfu, where no bacteriaemia was detected. All organs tested from animals which succumbed (lungs, liver, spleen, kidney, trachobronchial and mediastinal lymph nodes and brain) also contained B. anthracis at post-mortem. No bacteria were detected in the blood or organs of any animal that survived to the end of the trial.
Discussion
This study suggests that the pathology resulting from inhalationally acquired anthrax infection in the marmoset is similar to that observed in respiratory anthrax infection in both cynomologus and rhesus macaques, and in humans.
Particle size has been shown to be important to the eventual disease outcome for B. anthracis where aerosol droplets that contained single organisms (approximately 1 μm) were more infective (in terms of mortality), than particles larger than 5 μm in diameter. Indeed, B. anthracis delivered as small particles was 17 times more infective for guinea pigs than when bacteria were delivered in 12 μm particles (Druett et al. 1953). In this study, and those of others (Druett et al. 1953; Vasconcelos et al. 2003), the generation of infectious aerosols was achieved using a Collison nebulizer in conjunction with a contained Henderson apparatus. The primary feature of this system was the ability to generate, and deliver to the alveoli, small infectious, monodispersed particles, of less than 5 μm with a mean diameter of 1–2 μm (Henderson 1952; May 1973). The bacterial strain used in this study is the same as in the previous reports (Fritz et al. 1995; Vasconcelos et al. 2003), and, therefore, these studies are comparable in terms of bacterial strain and particle size.
The minute volume data determined in this study are comparable with those published previously (Bergers et al. 2004) for an anaesthetized marmoset, although the frequency of breathing of the marmosets in this study was approximately half that of the animal in the published study (data not shown). Although ketamine was used in both studies, the difference in doses used may have led to the observed differences in breathing frequency. An aerosol retention value, in marmosets, of 11% has been published (Bergers et al. 2004). Therefore, the calculation of a retention value was not determined in the present study as this would have required the use of a greater number of animals. Instead, the exposed dose was calculated and found to be consistent with other studies (Vasconcelos et al. 2003).
The mean LD50 value of B. anthracis Ames strain by the aerosol route for marmosets was 1.47 × 103cfu (95% confidence limits 7.2 × 103 − 2.95 × 105) in this study. This compares with an LD50 value of 6.1 × 104 cfu (95% confidence limits 3.48 − 11 × 104 cfu) in the cynomolgus macaque for the same strain and route (Vasconcelos et al. 2003), although a value of 4.13 × 103 cfu (95% confidence limits, 1.98 to 8.63 × 103 cfu) has also been reported (Glassman 1966). In the rhesus macaque, the Ames strain LD50 was 5.5 × 104 spores by the aerosol route (Ivins et al. 1996).
The wide range around this LD50 value in marmosets may reflect some individual variation in response, but could also be attributed to the small number of animals used to derive the value. The marmoset, however, appears to fall into the intermediately susceptible category with other NHP and humans [the current accepted human inhalational dose was reported to be from 2.5–55 × 103, spores (Soviet Biological Warfare Threat 1986)]. Marmosets that succumbed had a mean time-to-death of 3.2 days post-infection, which is comparable to that reported for the cynomolgus (Vasconcelos et al. 2003) and rhesus (Fritz et al. 1995) macaques. In this study, however, unlike that reported in the cynomolgus macaque, no dose–response relationship was noted in the time-to-death data. This has been reported previously in murine models of B. anthracis infection (Flick-Smith et al. 2005) and may be due to the sporulating nature of this organism (i.e. the propensity of spores to lie latent in the mammalian host and to cause disease in a non-dose-related manner).
High bacterial counts were detected in the blood of all animals that died and this is consistent with the reports of other NHP studies and also with reported human cases of inhalational anthrax from the Sverdlosk incident in the Soviet Union (Abramova et al. 1993).
Gross pathological observations in those animals, which died are consistent with observations in other NHP models of inhalational anthrax as well as human cases. Haemorrhage and oedema were the main features of the disease in those organs examined in this study. However, the relative proportions of organs affected in the marmoset differed from the proportions reported previously in cynomolgus and rhesus macaques. The main gross pathological difference observed in the marmoset compared with other NHP and humans was the relatively high incidence of haemorrhage observed in the lungs (50%) and the absence of meningeal haemorrhage (although this was seen in one surviving animal). This lack of meningeal haemorrhage may be a reflection of the small number of animals challenged and hence may not be truly representative of the disease in marmosets. The Ames strain of B. anthracis used in this study has been shown previously to cause meningeal haemorrhages in NHP (Vasconcelos et al. 2003) so this is, therefore, not a strain-specific phenomenon.
Histopathological findings in marmosets that survived challenge up to day 10 post-challenge were generally within normal limits. No bacilli were observed in any tissue, regardless of the initial dose administered, in five of six animals. The exception to this was a single animal which received a 100 cfu challenge; the histopathological profile in this animal was consistent with that seen in those animals, which died of the disease during the 10 days post-challenge. This suggests that this animal would have succumbed to infection had it not been culled at 10 days post-challenge.
Histopathological findings in those animals that died were consistent with some of the findings reported previously in respiratory anthrax infection in both humans and other NHP. Pulmonary oedema and haemorrhage were common features in the marmoset, cynomolgus monkeys and humans. However, acute interstitial pneumonia, although a common feature in the marmoset, was found infrequently in the cynomolgus or rhesus macaque.
The spleen was the organ most affected in the marmoset and provided the greatest predictor as to the overall condition of the animal. The histological features observed included lymphoid depletion, necrosis, fibrin deposition, haemorrhage and acute inflammation. These features are consistent with reported findings in both rhesus (Fritz et al. 1995) and cynomolgus (Vasconcelos et al. 2003) macaques, as well as in guinea pigs (Ross 1955) and rabbits infected with B. anthracis (Zaucha et al. 1998).
Meningitis has been reported in cynomologus and rhesus monkeys as well as humans infected by the inhalational route with B. anthracis after microscopic examination of brain tissue. In this study, although bacteria were noted intravascularly within the meninges and neuropil, haemorrhage was not present. As fibrinoid necrosis of vessel walls was noted in spleen and liver tissue, it would be expected that similar degenerative changes and subsequent haemorrhage would be seen in the brain. Again, this may represent a real species difference in organ susceptibility or it may be an infrequent feature of the disease not represented here due to the small numbers of animals used.
In this study, the common marmoset proved to be susceptible to inhaled challenge with B. anthracis delivered as small particle aerosols; the disease seen closely resembled the inhalational form of anthrax seen in other NHP and humans in terms of infectious dose, mortality, gross pathology and microscopic observations. This suggests that the common marmoset offers an alternative to larger NHP anthrax models, and may be appropriate for the evaluation of medical countermeasures against respiratory anthrax infection.
Acknowledgments
The authors would like to thank the animal technicians involved in this study and Rob Gwyther for statistical advice. Source of support was from Defense Advanced Research Projects Agency (DARPA), a subcontract of DAMD17-03-2-0042.
References
- Abramova FA, Grinberg LM, Yampolskaya OV, Walker DH. Pathology of inhalational anthrax in 42 cases from the Sverdlosk outbreak of 1979. Proc. Natl. Acad. Sci. 1993;90:2291–2294. doi: 10.1073/pnas.90.6.2291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Albrink WS, Goodlow RJ. Experimental inhalation anthrax in Chimpanzee. Am. J. Path. 1959;35:1055–1059. [PMC free article] [PubMed] [Google Scholar]
- Albrink WS, Brooks SM, Biron RE, Kopel M. Human inhalation anthrax. Am. J. Path. 1960;36:457–471. [PMC free article] [PubMed] [Google Scholar]
- Belton FC, Darlow HM, Henderson DW. The use of anthrax antigen to immunise man and monkey. Lancet. 1956;8:476–479. doi: 10.1016/s0140-6736(56)91968-7. [DOI] [PubMed] [Google Scholar]
- Bergers WA, van de Meent-van der Horst D, Joosen MJA. Respiration-based measurment of a lung deposition of a fluorescent dextrane aerosol in a marmoset monkey. Inhal. Tox. 2004;16:141–146. doi: 10.1080/08958370490270963. [DOI] [PubMed] [Google Scholar]
- Brachman PS, Kaufmann AF, Dalldorf FG. Industrial inhalation anthrax. Bact. Rev. 1966;30:646–657. doi: 10.1128/br.30.3.646-659.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalldorf FG, Kaufmann A. Studies on Inhalation Anthrax: III. Morphologic Studies. Fort Detrick: United States Army Biological Center; 1966. Technical manuscript 290. [Google Scholar]
- Dixon WJ, Fotheringhamn N. Application of staircase bioassays in pharmaceutical research. Drug Info. J. 1993;27:741–751. [Google Scholar]
- Druett HA. A mobile form of the Henderson apparatus. J. Hyg. 1969;67:437–448. doi: 10.1017/s0022172400041851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druett HA, Henderson DW, Packman L, Peacock S. Studies on respiratory infection. I. The influence of particle size on respiratory infection with anthrax spores. J. Hyg. 1953;51:359–371. doi: 10.1017/s0022172400015795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fellows PF, Linscott MK, Ivins BE, et al. Efficacy of a human anthrax vaccine in guinea pigs, rabbits and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine. 2001;19:3241–3247. doi: 10.1016/s0264-410x(01)00021-4. [DOI] [PubMed] [Google Scholar]
- Fellows PF, Linscott MK, Little SF, et al. Anthrax vaccine efficacy in golden Syrian hamsters. Vaccine. 2002;20:1421–1424. doi: 10.1016/s0264-410x(01)00461-3. [DOI] [PubMed] [Google Scholar]
- Flick-Smith HC, Walker NJ, Gibson P, et al. A recombinant carboxy terminal domain of protective antigen of Bacillus anthracis protects mice against anthrax infection. Infect. Immun. 2002;70:1653–1656. doi: 10.1128/IAI.70.3.1653-1656.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flick-Smith HC, Waters EL, Walker NJ, et al. Mouse model characterisation for anthrax vaccine development: comparison of an inbred and an outbred mouse strain. Microb. Pathog. 2005;38:33–40. doi: 10.1016/j.micpath.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Friedlander AM, Welkos SL, Pitt MLM, et al. Postexposure prophylaxis against experimental inhalation anthrax. J. Infect. Dis. 1993;167:1239–1242. doi: 10.1093/infdis/167.5.1239. [DOI] [PubMed] [Google Scholar]
- Fritz DL, Jaxx NK, Lawrence WB, et al. Pathology of experimental inhalation anthrax in the rhesus monkey. Lab. Invest. 1995;73:691–702. [PubMed] [Google Scholar]
- Glassman HN. Industrial inhalation of anthrax; discussion. Bact. Rev. 1966;30:657–659. [Google Scholar]
- Griffiths GD, Hornby RJ, Jagger CP, et al. Development of methods to measure humoral immune responses against selected antigens in the common marmoset (Callithrix jacchus) and the effect of pyridostigmine bromide administration. Int. Immunopharm. 2006;6:1755–1764. doi: 10.1016/j.intimp.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Henderson DW. An apparatus for the study of airborne infection. J. Hyg. (Camb.) 1952;50:53–68. doi: 10.1017/s0022172400019422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson DW, Peacock S, Belton FC. Observations on the prophylaxis of experimental pulmonary anthrax in monkeys. J. Hyg. 1956;54:2836. doi: 10.1017/s0022172400044272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornby RJ, Pearce PC, Bowditch AP, et al. Multiple vaccine and pyridostigmine bromide interactions in the common marmoset Callithrix jacchus: immunological and endocrinological effects. Int. Immunopharm. 2006;6:1765–1779. doi: 10.1016/j.intimp.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Ivins BE, Welkos SL, Little SF, et al. Immunisation against anthrax with Bacillus anthracis protective antigen combined with adjuvants. Infect. Immun. 1992;60:662–668. doi: 10.1128/iai.60.2.662-668.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivins BE, Fellows PF, Nelson GO. Efficacy of a standard human anthrax vaccine against Bacillus anthracis spore challenge in guinea pigs. Vaccine. 1994;12:872–874. doi: 10.1016/0264-410x(94)90027-2. [DOI] [PubMed] [Google Scholar]
- Ivins BE, Fellows PF, Pitt MLM, et al. Efficacy of a standard human anthrax vaccine against Bacillus anthracis spore challenge in rhesus monkeys. Salisbury Med. Bull. 1996;87:125–126. [Google Scholar]
- Ivins BE, Pitt ML, Fellows PF, et al. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in Rhesus macaques. Vaccine. 1998;16:1141–1148. doi: 10.1016/s0264-410x(98)80112-6. [DOI] [PubMed] [Google Scholar]
- Jones MN, Beedham RJ, Turnbull PCB, et al. Efficacy of the UK human anthrax vaccine in guinea pigs against aerosolised spores of Bacillus anthracis. Salisbury Med. Bull. 1996;87(Suppl.):127–128. [Google Scholar]
- Little SF, Knudson GB. Comparative efficacy of Bacillus anthracis live spore vaccine and protective antigen vaccine against anthrax in the guinea pig. Infect. Immun. 1986;52:509–512. doi: 10.1128/iai.52.2.509-512.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- May KR. The Collison nebuliser: description, performance and application. Aero. Sci. 1973;4:235–243. [Google Scholar]
- McBride BW, Mogg A, Telfer JL, et al. Protective efficacy of a recombinant protective antigen against Bacillus anthracis challenge and assessment of immunological markers. Vaccine. 1998;16:810–817. doi: 10.1016/s0264-410x(97)00268-5. [DOI] [PubMed] [Google Scholar]
- Pitt ML, Little S, Ivins BE, et al. In vitro correlate of immunity in an animal model of inhalational anthrax. Vaccine. 2001;19:4768–4773. doi: 10.1016/s0264-410x(01)00234-1. [DOI] [PubMed] [Google Scholar]
- Ross JM. On the histopathology of experimental anthrax in the guinea pig. Br. J. Exp. Pathol. 1955;36:336–339. [PMC free article] [PubMed] [Google Scholar]
- Rowland CA, Williamson ED, Jones SM. Proceedings of the 4th International Conference on Anthrax. Maryland: Annapolis; 2001. Intracellular detection of PA-specific IL4 following immunisation with a novel and current anthrax vaccines in Rhesus Macaques; p. 46. [Google Scholar]
- Smith D, Trennery P, Farningham D, Klapwijk J. The selection of marmoset monkeys (Callithrix jacchus) in pharmaceutical toxicology. Lab. Anim. 2001;35:117–130. doi: 10.1258/0023677011911444. [DOI] [PubMed] [Google Scholar]
- Soviet Biological Warfare Threat. Washington DC: Defence Intelligence Agency, US Dept of Defence; 1986. 1986; Publication DST-161OF-057-86. [Google Scholar]
- Turnbull PC. Anthrax vaccines: past, present and future. Vaccine. 1986;9:533–539. doi: 10.1016/0264-410x(91)90237-z. [DOI] [PubMed] [Google Scholar]
- Turnbull PCB, Broster MG, Carman JA, et al. Development of antibodies to protective antigen and lethal factor components of anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Infect. Immun. 1986;52:356–363. doi: 10.1128/iai.52.2.356-363.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull PCB, Leppla SH, Broster MG, et al. Antibodies to anthrax toxin in humans and guinea pigs and their relevance to protective antigen. Med. Microbiol. Immunol. 1988;177:293–303. doi: 10.1007/BF00189414. [DOI] [PubMed] [Google Scholar]
- Varughese M, Teixeira AV, Liu S, Leppla SH. Identification of a receptor-binding region within domain 4 of the protective antigen component of anthrax toxin. Infect. Immun. 1999;67:1860–1865. doi: 10.1128/iai.67.4.1860-1865.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasconcelos D, Barnewall R, Babin M, et al. Pathology of inhalation anthrax in cynomologus monkeys (Macaca fascilaris) Lab. Invest. 2003;83:1201–1209. doi: 10.1097/01.lab.0000080599.43791.01. [DOI] [PubMed] [Google Scholar]
- Welkos SL, Keener TJ, Gibbs PH. Differences in susceptibility of inbred mice to Bacillus anthracis. Infect. Immun. 1986;51:795–800. doi: 10.1128/iai.51.3.795-800.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson ED, Hodgson I, Walker NJ, et al. Immunogenicity of recombinant protective antigen and efficacy against aerosol challenge with anthrax. Infect. Immun. 2005;73:5978–5987. doi: 10.1128/IAI.73.9.5978-5987.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaucha GM, Pitt LM, Estep J, et al. The pathology of experimental anthrax in rabbits exposed by inhalation and subcutaneous inoculation Arch. Path. Lab. Med. 1998;122:982–992. [PubMed] [Google Scholar]