Abstract
Objective
The objective of this study was to assess, with knee radiography, joint space narrowing (JSN) and its relationship to meniscal tears, anterior cruciate ligament (ACL) ruptures, articular cartilage erosion, and duration of pain in patients with knee osteoarthritis.
Materials and methods
A total of 140 patients who had knee osteoarthritis and underwent primary total knee replacement (TKR) surgery, with unicompartmental medial tibiofemoral JSN (grade 1 or greater) and normal lateral compartments, were recruited. Polytomous logistic regression was used to assess the relationship between JSN and risk factors.
Results
All patients with JSN were categorized as grade 1 (n = 14, 10.0%), grade 2 (n = 64, 45.7%), or grade 3 (n = 62, 44.3%). Women presented with indications for a TKR at a younger age than men (mean age, 69 vs 73 years, P < 0.05). There were 123 (87.9%) meniscal tears and 58 (41.4%) partial (insufficient or attenuated ACL fibers) and 10 (7.1%) complete ACL ruptures; 115 of 134 (85.8%) patients had moderate to severe cartilage erosion. A higher grade of JSN was correlated with a higher frequency of meniscal tears [odds ratio (OR) 6.00, 95% CI 1.29–27.96 for grade 2 vs grade 1 JSN] and duration of knee pain (OR 1.25, 95% CI 1.01–1.53 for grade 3 vs grade 1 JSN). A higher grade of JSN was not correlated with a higher frequency of ACL rupture or articular cartilage erosion.
Conclusion
A higher grade of JSN is associated with a higher frequency of meniscal tears and long duration of knee pain in patients with knee osteoarthritis.
Keywords: Articular cartilage, Knee, Meniscus, Osteoarthritis, Pain, Radiography
Introduction
Knee osteoarthritis is a common cause of disability in aged people. Total knee replacement (TKR) surgery is commonly used to treat those patients with intractable symptoms of knee osteoarthritis after conservative treatment failure. Radiography is a commonly accessible tool for assessing knee osteoarthritis, especially in the end stage of the disease.
Joint space narrowing (JSN) on radiography is generally attributed to loss of articular cartilage in the osteoarthritic knee. A number of studies have discussed the potential risk factors for osteoarthritic changes of the knee and their relationship to JSN. Osteoarthritic knee occurs frequently 10 to 20 years after the diagnosis of a tear in the anterior cruciate ligament (ACL) or meniscus [1]. In older people, meniscal tears are commonly observed in a load-transmitting compartment with knee osteoarthritis [2–7]. Meniscal subluxation and degeneration have each contributed to the prediction of JSN on radiography [8]. Meniscal tears, therefore, could be hypothesized as contributing to a proportional change in JSN in end-stage osteoarthritis of the knee.
A study of patients with knee pain but no radiographic findings of knee osteoarthritis showed that most had significant articular cartilage degeneration at arthroscopy [9]. In another study, there was also no association of articular cartilage loss and radiographic JSN in patients with progressive osteoarthritic knee [10]. However, progression of knee osteoarthritis may exacerbate the severity of knee pain, leading to subsequent TKR [11, 12]. Duration of knee pain, therefore, could be related to JSN seen on radiography.
Additional variables associated with individual patients, such as age, sex, and obesity, can add to the variation in the outcome of osteoarthritic knee [1]. A better understanding of these variables may improve future prevention and treatment strategies.
Few studies have reported a relationship of JSN on radiography to contributing factors in patients with end-stage osteoarthritis of the knee [13, 14]. In this study, we attempted to evaluate the relationships of radiographic JSN with meniscal tears, ACL ruptures, cartilage erosion, and duration of knee pain in patients with unicompartmental knee osteoarthritis of the medial tibiofemoral joint before TKR.
Materials and methods
The study was approved by our institutional review board. Informed consent was waived because this retrospective study was limited to the analysis of patients’ records.
Selection of patients
Between January 2001 and August 2005, 193 consecutive patients were identified from a computer search of patients who had knee osteoarthritis and underwent primary TKR in one institution. There were 156 women (mean age ± standard deviation, 69.0 ± 7.8 years) and 37 men (72.4 ± 6.9 years). The medical records and preoperative knee radiographs of each patient were reviewed retrospectively.
The medial and lateral tibiofemoral joints of the knee of each patient were evaluated separately for the absence or presence of JSN and osteophytes. Inclusion criteria for patient selection were unicompartmental medial tibiofemoral JSN (grade 1 or greater) and a normal lateral compartment (JSN grade 0). Exclusion criteria were JSN grade 1 or more and osteophytes (intermediate size, proliferating or mushroom-like) in the lateral compartment. After exclusions, there were 113 women [mean age, 69.4 years; range, 50–85 years; body mass index (BMI) 28.2 kg/m2] and 27 men (mean age, 72.6 years; range, 53–84 years; BMI, 26.5 kg/m2).
All medical records were reviewed for the demographic characteristics of patients. The items included age on the day of hospitalization before TKR, sex, height and weight, and duration of knee pain. All primary TKRs were performed by one of five experienced orthopedic surgeons, and 94.3% of TKRs were performed by one surgeon (W.P.H.).
X-ray films for interpretation were taken an average of 35 days (range, 1–298 days; 96.4% less than 4 months) before the TKR. All patients had standing anterior–posterior radiographs (Shimadzu, MU125 M, Japan) on two legs with both knees fully extended. The focus-film distance was 110 cm. Approximately half of the patients also received skyline patellofemoral radiographs. The images obtained before 2003 were displayed by hard copy films; the later 70 images were displayed by using a picture archiving and communication system (PACS) viewer with a 2,560 × 2,048 pixel monitor (Barco, MGD 521 MK II, Belgium).
Two radiologists (W.P.C. and G.S.H), each with 15 years’ experience in musculoskeletal system imaging, interpreted all radiographs together without awareness of the clinical data of the subjects, and a consensus of interpretation was reached. The observers evaluated the severity and distribution of the JSN and osteophytes in the osteoarthritic knee using a semiquantitative grading system (score, 0 to 3). The severity of JSN was graded as 0 = normal, 1 = mild or 1–33% narrowing of the joint space, 2 = moderate or 34–66% narrowing of the joint space, and 3 = severe or 67–100% narrowing of the joint space [15]. Osteophytes were graded as 0 = absent, 1 = small beaklike, 2 = intermediate size, and 3 = proliferating or mushroom-like osteophyte [16]. Although osteophytes are an important sign of early osteoathritic knee [17], the dependent variable in our study was radiographic JSN. Therefore, only JSN was used in the analysis.
Before interpretation of all radiographs in this study, the two observers met to assess test–retest reliability of grading JSN on a separate sample of 30 films of osteoarthritic knees, which showed 100% agreement with quantitative measurement of the joint space on the PACS.
The menisci were classified by absence or presence of tears based on visual inspection, as documented on the surgical reports. The ACL was evaluated as intact, partially torn (insufficient or attenuated fibers), or completely torn (complete rupture), as described on the surgical records. Data for partial and complete ruptures of the ACL were combined for risk-factor analysis.
Owing to incomplete data on cartilage erosion from arthroscopy, we used pathology findings for assessing cartilage erosion. One of the two pathologists read the reports on the histologic specimens of each knee obtained from TKR as noted on the medical records. Articular cartilage erosion of the tibial plateau or femoral condyles was recorded as grade 1 = superficial or mild erosion, grade 2 = moderate erosion, and grade 3 = severe erosion. The highest grades shown were used to represent the severity of articular cartilage erosion.
The duration of knee pain was obtained from the medical records of the outpatient clinics where the X-rays films were ordered. The admission records for TKR had the weight and height of the patients. The BMI was calculated as weight (kg) divided by height squared (m2).
Data for the BMI index calculation were unavailable for two patients, data on the duration of knee pain was not clearly recorded for 36 patients, and data on the erosion of the articular cartilage of the tibiofemoral compartment was not available for six subjects. There was no unreported ACL status on surgical reports.
Statistical analysis
Because one knee per subject was studied on radiography, analyses in this study were knee- and subject-specific. Student’s t test was used to assess the continuous variables. Differences between proportions were assessed by chi-square or Fisher’s exact test. All tests were two-sided, and P values less than or equal to 0.05 were considered significant.
The risk factors were evaluated by polytomous logistic regression. The JSN grade was a dependent variable; independent variables were age, sex, BMI, presence of a torn meniscus or ACL, and erosion of the articular cartilage. Odds ratio (OR) was estimated with a 95% confidence interval (CI). Statistical analysis was performed using the SAS/STAT V8.2 system (SAS Institute, Cary, NC, USA) and Stata 8.0 software.
Results
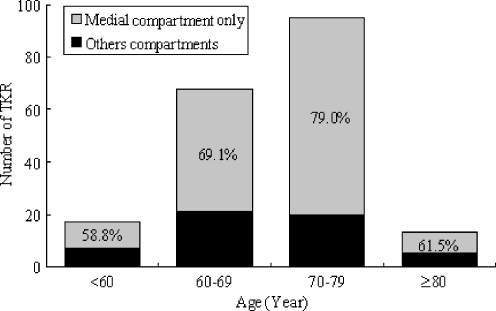
Among 193 patients who had a diagnosis of osteoarthritis of the knee and underwent primary TKR, 140 (72.5%) patients had unicompartmental medial tibiofemoral osteoarthritis (Fig. 1), 70 of the right knee and 70 of the left.
Fig. 1.
Age distribution of 193 patients with knee osteoarthritis who underwent primary total knee replacement (TKR) surgery. The proportions of diseased compartments are divided into two groups: medial compartment only and other compartments
Women presented with indications for a TKR at a younger age than men (mean, 69.4 vs 72.6 years; Table 1). Women had a higher BMI than men, but the difference was not significant. The duration of knee pain was similar for both sexes. There were 123 (87.9%) meniscal tears, 58 (41.4%) partial (insufficient or attenuated ACL fibers) and 10 (7.1%) complete ACL ruptures, and 115 out of 134 (85.8%) patients with moderate to severe cartilage erosion of the tibiofemoral joints. The unicompartmental medial tibiofemoral osteoarthritis was categorized as JSN grade 1 in 10.0% (14), grade 2 in 45.7% (64), and grade 3 in 44.3% (62).
Table 1.
Characteristics of the 140 patients with unicompartmental medial tibiofemoral osteoarthritis who underwent primary total knee replacement surgery
| Characteristica | Men (n = 27) | Women (n = 113) | P value |
|---|---|---|---|
| Age, mean ± SD years | 72.6 ± 7.3 | 69.4 ± 7.1 | 0.04 |
| BMI, mean ± SD kg/m2b | 26.5 ± 3.7 | 28.2 ± 4.3 | 0.06 |
| Duration of knee pain, mean ± SD yearsb | 6.3 ± 5.9 | 6.4 ± 5.3 | 0.94 |
| Meniscal tear | 23 (85.2) | 100 (88.5) | 0.74 |
| ACL rupture | 9 (33.3) | 59 (52.2) | 0.08 |
| Partialc | 7 (25.9) | 51 (45.1) | 0.06 |
| Complete | 2 (7.4) | 8 (7.1) | 1.00 |
| Cartilage erosionb | 26 (100.0) | 108 (100.0) | – |
| Mild | 3 (11.5) | 16 (14.8) | Referent |
| Moderate | 5 (19.2) | 29 (26.9) | 1.00 |
| Severity | 18 (69.2) | 63 (58.3) | 0.76 |
BMI Body mass index, SD standard deviation, ACL anterior cruciate ligament
aExcept where otherwise indicated, values are the number (%).
bIncomplete data were estimated.
cIndicates attenuated or insufficient fibers
Ignoring all other factor effects, we noted that the presence of meniscal tears was correlated with a higher grade of JSN (OR 6.00, 95% CI 1.29–27.96 for grade 2 vs grade 1; Table 2). A longer duration of knee pain (per year of increase in knee pain) increased the risk of a higher JSN grade (OR 1.25, 95% CI 1.01–1.53 for grade 3 vs grade 1). ACL ruptures and grade of cartilage erosion of the tibiofemoral joints did not show any clear relationship with the severity of JSN grade. No statistical differences in age, sex, or BMI were observed among JSN grades.
Table 2.
Results of polytomous logistic regression analysis of risk factors for medial tibiofemoral joint space narrowing (JSN), presented with odds ratio (95% confidence interval), with grade 1 JSN as the reference group
| Grade 2 JSN | Grade 3 JSN | |
|---|---|---|
| Sex (men referent) | 1.91 (0.44–8.35) | 0.78 (0.19–3.17) |
| Age | 0.94 (0.86–1.02) | 0.94 (0.86–1.03) |
| BMI† | 1.04 (0.90–1.20) | 1.07 (0.93–1.24) |
| Duration of knee paina | 1.21 (0.99–1.48) | 1.25 (1.01–1.53)* |
| Meniscal tear | 6.00 (1.29–27.96)* | 2.36 (0.61–9.16) |
| ACL rupture | 0.94 (0.30–2.99) | 0.94 (0.30–2.99) |
| Cartilage erosiona | ||
| Mild | 1.00 (referent) | 1.00 (referent) |
| Moderate | 1.28 (0.24–6.70) | 0.90 (0.17–4.87) |
| Severity | 2.31 (0.48–11.26) | 2.30 (0.49–11.55) |
BMI Body mass index, ACL anterior cruciate ligament
*P < 0.05 (pain, P = 0.036; meniscal tear, P = 0.023)
aIncomplete data were estimated.
Discussion
The prevalence of meniscal tears is high in older people with osteoarthritis of the knee. Bhattacharyya et al. [2] reported that a medial meniscal tear was detected in 86% of patients with symptomatic osteoarthritis of the knee, similar to our findings (88%). In unicompartmental medial tibiofemoral osteoarthritis, the presence of medial meniscal tears resulted in a sixfold risk of grade 2 versus grade 1 JSN, compared with the 2.36-fold risk of grade 3 vs grade 1 JSN. Ding et al. [18] reported that meniscal tear was associated with cartilage defect and with the prevalence of radiographic osteoarthritic knee in a nonosteoarthritic adult population, suggesting that meniscal tear appeared to be an early event in the disease process and may be a risk factor for knee cartilage damage and articular structural changes. It is an interesting finding that torn menisci do not lead to a close association with severe JSN, as seen in our study.
The unremarkable outcome of meniscal tears relating to higher JSN grade in our study can reasonably be explained by meniscal extrusion in advanced stages of osteoarthritic knee. Meniscal extrusion is a common finding in patients with osteoarthritis of the knee, and increasing meniscal extrusion was correlated with the severity of JSN [8, 19, 20]. Gale et al. [19] reported that, in the symptomatic osteoarthritic knee, mean medial meniscal extrusion was 5.1 mm, which was higher than that of the asymptomatic subjects (2.8 mm). Hunter et al. [8] concluded that both meniscal position and degeneration accounted for a substantial proportion of the variance explained in radiographic JSN, and a change in meniscal position accounted for a substantial proportion of change in JSN. The macroscopic and histologic findings indicated that the medial meniscus can be preserved well in severe osteoarthritis even if the joint space has already disappeared [20]. If meniscal extrusion precedes JSN, the displaced meniscus may be saved from severe degeneration [21]. However, Boegård et al. [17] reported a high prevalence of MRI-detected cartilage defects in the tibiofemoral joint with the presence of marginal osteophytes in the same joint, no matter whether JSN was present or not.
A previous report indicated that 23% of symptomatic subjects with knee osteoarthritis had complete ACL ruptures [6]. Ruptures of the ACL can change tibiofemoral kinematics, which can affect the lateral tibia, resulting in no association between the joint space width of the medial compartment and ACL ruptures of an injured knee [22, 23]. This may, in part, explain the lack of correlation between ACL ruptures and the severity of medial JSN in our study.
The severity of cartilage erosion and JSN grade were not correlated in our study. Previous reports have stated that changes in the articular cartilage in the medial tibiofemoral compartment were less marked, even where there was a linear correlation between mean cartilage volume and radiographic JSN [24, 25]. Kijowski et al. [9] reported that 55% of patients with articular cartilage degeneration within the tibiofemoral joint diagnosed at arthroscopy had no radiographic evidence of osteoarthritis according to the Ahlback grading scale [26]. It is well known that the Ahlback grading scale is based exclusively on the severity of JSN on radiography in the diagnosis of tibiofemoral knee osteoarthritis. Radiographic JSN is not a reliable tool for assessing cartilage status in patients with early osteoarthritis or in chronic knee pain [21, 27]. Results of our study also suggested that joint space status may not be an appropriate predictor of tibiofemoral cartilage erosion in end-stage osteoarthritic knee.
Severity of joint pain can be used to predict subsequent JSN or as an indicator for operation [11, 28]. A painful knee and limitation of movement are the main indications for TKR surgery. Previous reports have shown that patients who had osteoarthritis of the knee with meniscal tears or ACL ruptures had not experienced more painful knees, and meniscal tears may not affect the functional status of the knee [6, 19]. Results of our study indicated that a longer duration of knee pain also could increase the risk of a higher JSN grade. This relationship has not been statistically analyzed before.
Our data showed no relationship between age and JSN grade. Because the study design was based on patients having TKR, the mean age of our subjects was 70 years, so they were older than in other cross-sectional studies [29]. Previous data have shown that age accounts for a significant linear decrease in both lateral and medial femoral cartilage thickness [30]. However, age may not affect the progression of osteoarthritic knee among the elderly [31]. Our population was older and the knee condition may have come to an unchanging end-stage.
Women presented with indications for a TKR at a younger age than men, but the proportions of the JSN grades were not different between the sexes. Therefore, we cannot say whether women or men would develop a higher JSN grade. We may consider that the disease would progress to a similar status for the two sexes at the end-stage of osteoarthritis of the medial tibiofemoral joints.
There was a trend but no statistical relationship between BMI and JSN grade in our data. Previous research has indicated that BMI can predict JSN when JSN is equal to zero at onset but not in those with more severe disease [32]. The effect of BMI is limited to knees in which moderate malalignment exists, especially in the severity of medial tibiofemoral osteoarthritis [33, 34]. The focus of the malalignment of the joint and the excess load from increased weight should be taken into account.
Our data showed that almost three quarters of the patients with knee osteoarthritis who underwent primary TKR had unicompartmental medial tibiofemoral JSN. Younger patients, aged less than 60 years, had a lower proportion (59%) of medial tibiofemoral osteoarthritis. The natural aging process could explain this phenomenon, and BMI is not necessarily a factor. That the severity of knee osteoarthritis is less marked in the patellofemoral and lateral tibiofemoral compartment has been well documented [13]. Our results similarly showed that the lateral tibiofemoral compartment was relatively rarely involved in osteoarthritis of the knee.
There were several limitations to our study. It was a cross-sectional and hospital-based investigation, so longitudinal and population inferences are limited. The radiographic technique could be suboptimal for imaging the tibiofemoral joint space, reducing the sensitivity in detecting JSN [35]. Future investigations should include examination of the knee in semiflexion with fluoroscopic guidance for optimal visualization of the joint space [36]. Semiquantitative assessment with radiography may not be ideal for JSN analysis, but the potential bias was minimized by test–retest reliability analysis by the two observers before this study began. In this retrospective study, determination of the duration of knee pain was not precise, and also the time when patients presented with pain was not necessarily the start of osteoarthritis.
In conclusion, a higher grade of JSN is associated with a higher frequency of meniscal tears and long duration of knee pain in patients with knee osteoarthritis.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35:1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85-A:4–9. doi: 10.2106/00004623-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Fukuda Y, Takai S, Yoshino N, et al. Impact load transmission of the knee joint-influence of leg alignment and the role of meniscus and articular cartilage. Clin Biomech (Bristol, Avon) 2000;15:516–521. doi: 10.1016/S0268-0033(00)00013-9. [DOI] [PubMed] [Google Scholar]
- 4.Maffulli N, Binfield PM, King JB. Articular cartilage lesions in the symptomatic anterior cruciate ligament-deficient knee. Arthroscopy. 2003;19:685–690. doi: 10.1016/s0749-8063(03)00403-1. [DOI] [PubMed] [Google Scholar]
- 5.Almekinders LC, Pandarinath R, Rahusen FT. Knee stability following anterior cruciate ligament rupture and surgery. The contribution of irreducible tibial subluxation. J Bone Jnt Surg Am. 2004;86:983–987. doi: 10.1302/0301-620X.86B7.15157. [DOI] [PubMed] [Google Scholar]
- 6.Hill CL, Seo GS, Gale D, Totterman S, Gale ME, Felson DT. Cruciate ligament integrity in osteoarthritis of the knee. Arthritis Rheum. 2005;52:794–799. doi: 10.1002/art.20943. [DOI] [PubMed] [Google Scholar]
- 7.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthr Cartil. 1995;3:261–267. doi: 10.1016/S1063-4584(05)80017-2. [DOI] [PubMed] [Google Scholar]
- 8.Hunter DJ, Zhang YQ, Tu X, et al. Change in joint space width: hyaline articular cartilage loss or alteration in meniscus? Arthritis Rheum. 2006;54:2488–2495. doi: 10.1002/art.22016. [DOI] [PubMed] [Google Scholar]
- 9.Kijowski R, Blankenbaker D, Stanton P, Fine J, Smet AD. Arthroscopic validation of radiographic grading scales of osteoarthritis of the tibiofemoral joint. AJR Am J Roentgenol. 2006;187:794–799. doi: 10.2214/AJR.05.1123. [DOI] [PubMed] [Google Scholar]
- 10.Raynauld JP, Martel-Pelletier J, Berthiaume MJ, et al. Long term evaluation of disease progression through the quantitative magnetic resonance imaging of symptomatic knee osteoarthritis patients: correlation with clinical symptoms and radiographic changes. Arthritis Res Ther. 2006;8:R21. doi: 10.1186/ar1875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dieppe P, Cushnaghan J, Young P, Kirwan J. Prediction of the progression of joint space narrowing in osteoarthritis of the knee by bone scintigraphy. Ann Rheum Dis. 1993;52:557–563. doi: 10.1136/ard.52.8.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spector TD, Dacre JE, Harris PA, Huskisson EC. Radiological progression of osteoarthritis: an 11 year follow up study of the knee. Ann Rheum Dis. 1992;51:1107–1110. doi: 10.1136/ard.51.10.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chitnavis J, Sinsheimer JS, Suchard MA, Clipsham K, Carr AJ. End-stage coxarthrosis and gonarthrosis. Aetiology, clinical patterns and radiological features of idiopathic osteoarthritis. Rheumatology. 2000;39:612–619. doi: 10.1093/rheumatology/39.6.612. [DOI] [PubMed] [Google Scholar]
- 14.Cushner FD, La Rosa DF, Vigorita VJ, Scuderi GR, Scott WN, Insall JN. A quantitative histologic comparison: ACL degeneration in the osteoarthritic knee. J Arthroplasty. 2003;18:687–692. doi: 10.1016/S0883-5403(03)00256-0. [DOI] [PubMed] [Google Scholar]
- 15.Chan WP, Lang P, Stevens MP, et al. Osteoarthritis of the knee: comparison of radiography, CT, and MR imaging to assess extent and severity. AJR Am J Roentgenol. 1991;157:799–806. doi: 10.2214/ajr.157.4.1892040. [DOI] [PubMed] [Google Scholar]
- 16.Kindynis P, Haller J, Kang HS, et al. Osteophytosis of the knee: anatomic, radiologic, and pathologic investigation. Radiology. 1990;174:841–846. doi: 10.1148/radiology.174.3.2305068. [DOI] [PubMed] [Google Scholar]
- 17.Boegård T, Rudling O, Petersson IF, Jonsson K. Correlation between radiographically diagnosed osteophytes and magnetic resonance detected cartilage defects in the tibiofemoral joint. Ann Rheum Dis. 1998;57:401–407. doi: 10.1136/ard.57.7.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ding C, Martel-Pelletier J, Pelletier JP, et al. Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: a cross-sectional study. J Rheumatol. 2007;34:776–784. [PubMed] [Google Scholar]
- 19.Gale DR, Chaisson CE, Totterman SM, Schwartz RK, Gale ME, Felson D. Meniscal subluxation: association with osteoarthritis and joint space narrowing. Osteoarthr Cartil. 1999;7:526–532. doi: 10.1053/joca.1999.0256. [DOI] [PubMed] [Google Scholar]
- 20.Sugita T, Kawamata T, Ohnuma M, Yoshizumi Y, Sato K. Radial displacement of the medial meniscus in varus osteoarthritis of the knee. Clin Orthop. 2001;387:171–177. doi: 10.1097/00003086-200106000-00023. [DOI] [PubMed] [Google Scholar]
- 21.Adams JG, McAlindon T, Dimasi M, Carey J, Eustace S. Contribution of meniscal extrusion and cartilage loss to joint space narrowing in osteoarthritis. Clin Radiol. 1999;54:502–506. doi: 10.1016/S0009-9260(99)90846-2. [DOI] [PubMed] [Google Scholar]
- 22.Logan M, Dunstan E, Robinson J, Williams A, Gedroyc W, Freeman M. Tibiofemoral kinematics of the anterior cruciate ligament (ACL)-deficient weightbearing, living knee employing vertical access open “interventional” multiple resonance imaging. Am J Sports Med. 2004;32:720–726. doi: 10.1177/0095399703258771. [DOI] [PubMed] [Google Scholar]
- 23.Buckland-Wright JC, Lynch JA, Dave B. Early radiographic features in patients with anterior cruciate ligament rupture. Ann Rheum Dis. 2000;59:641–646. doi: 10.1136/ard.59.8.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cicuttini FM, Wluka AE, Forbes A, Wolfe R. Comparison of tibial cartilage volume and radiologic grade of the tibiofemoral joint. Arthritis Rheum. 2003;48:682–688. doi: 10.1002/art.10840. [DOI] [PubMed] [Google Scholar]
- 25.Bennett LD, Buckland-Wright JC. Meniscal and articular cartilage changes in knee osteoarthritis: a cross-sectional double-contrast macroradiographic study. Rheumatology (Oxf) 2002;41:917–923. doi: 10.1093/rheumatology/41.8.917. [DOI] [PubMed] [Google Scholar]
- 26.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Suppl. 1968;227:7–72. [PubMed] [Google Scholar]
- 27.Fife RS, Brandt KD, Braunstein EM, et al. Relationship between arthroscopic evidence of cartilage damage and radiographic evidence of joint space narrowing in early osteoarthritis of the knee. Arthritis Rheum. 1991;34:377–382. doi: 10.1002/art.1780340402. [DOI] [PubMed] [Google Scholar]
- 28.Mazzuca SA, Brandt KD, Schauwecker DS, et al. Severity of joint pain and Kellgren-Lawrence grade at baseline are better predictors of joint space narrowing than bone scintigraphy in obese women with knee osteoarthritis. J Rheumatol. 2005;32:1540–1546. [PubMed] [Google Scholar]
- 29.Lanyon P, O'Reilly S, Jones A, Doherty M. Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis. 1998;57:595–601. doi: 10.1136/ard.57.10.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karvonen RL, Negendank WG, Teitge RA, Reed AH, Miller PR, Fernandez-Madrid F. Factors affecting articular cartilage thickness in osteoarthritis and aging. J Rheumatol. 1994;21:1310–1318. [PubMed] [Google Scholar]
- 31.Felson DT, Zhang Y, Hannan MT, et al. The incidence and natural history of knee osteoarthritis in the elderly. The Framingham Osteoarthritis Study. Arthritis Rheum. 1995;38:1500–1505. doi: 10.1002/art.1780381017. [DOI] [PubMed] [Google Scholar]
- 32.Wolfe F, Lane NE. The longterm outcome of osteoarthritis: rates and predictors of joint space narrowing in symptomatic patients with knee osteoarthritis. J Rheumatol. 2002;29:139–146. [PubMed] [Google Scholar]
- 33.Felson DT, Goggins J, Niu J, Zhang Y, Hunter DJ. The effect of body weight on progression of knee osteoarthritis is dependent on alignment. Arthritis Rheum. 2004;50:3904–3909. doi: 10.1002/art.20726. [DOI] [PubMed] [Google Scholar]
- 34.Sharma L, Lou C, Cahue S, Dunlop DD. The mechanism of the effect of obesity in knee osteoarthritis: the mediating role of malalignment. Arthritis Rheum. 2000;43:568–575. doi: 10.1002/1529-0131(200003)43:3<568::AID-ANR13>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 35.Vignon E, Piperno M, Le Graverand MP, et al. Measurement of radiographic joint space width in the tibiofemoral compartment of the osteoarthritic knee: comparison of standing anteroposterior and Lyon schuss views. Arthritis Rheum. 2003;48:378–384. doi: 10.1002/art.10773. [DOI] [PubMed] [Google Scholar]
- 36.Boegård T, Rudling O, Petersson IF, et al. Postero-anterior radiogram of the knee in weight-bearing and semiflexion. Comparison with MR imaging. Acta Radiol. 1997;38:1063–1070. doi: 10.1080/02841859709172132. [DOI] [PubMed] [Google Scholar]