Abstract
Objectives
To determine the relationship between functional outcome and abnormalities of heart rate & rhythm after the Fontan operation.
Methods
The NHBLI Pediatric Heart Network conducted a cross sectional analysis of patients who had undergone a Fontan procedure at the 7 network centers. Analysis was based on 521 patients with an ECG (n=509) and/or bicycle exercise test (n=404). The Child Health Questionnaire parent report and the O2 consumption at the anaerobic threshold were used as markers of functional outcome.
Results
Various Fontan procedures had been performed: intracardiac lateral tunnel (59%), atrio-pulmonary connection (14%), extracardiac later tunnel (13%), and extracardiac conduit (11%). Prior volume unloading surgery was performed in 389 patients; Bi-directional Glenn (70%) and Hemi-Fontan (26%). A history of atrial tachycardia was noted in 9.6% of patients and 13.1% of patients had a pacemaker. Lower resting heart rate and higher peak heart rate were each weakly associated with better functional status, as defined by higher anaerobic threshold (R = -0.18, p=0.004 and R = 0.16, p=0.007, respectively) and higher Child Health scores for physical functioning (R = -0.18, p<0.001 and R = 0.17, p=0.002, respectively). Higher anaerobic threshold was also independently associated with younger age and an abnormal P-axis. Resting bradycardia was not associated with anaerobic threshold or Child Health scores.
Conclusions
In pediatric patients (6-18 yrs) following the Fontan procedure, a lower resting heart rate and a higher peak heart rate are each independently associated with better physical function as measured by anaerobic threshold and Child Health scores. However, these correlations are weak suggesting that other, non-rhythm and non-rate, factors may have a greater impact on the functional outcome of pediatric Fontan patients.
Introduction
Heart rate and rhythm disorders, such as sinus node dysfunction and atrial tachycardia, are common and potentially important late morbidities of the Fontan operation (1-10). The incidence of late sinus node dysfunction following the Fontan operation has been reported to be about 15% (1-3), but may occur in up to 44% of patients in selected series (4). The incidence of atrial tachycardia is 16-17% at approximately 5 years following the Fontan procedure (1;5) and reaches 50% by 12 years (1). Further, sinus node dysfunction and atrial tachycardia can result in significant symptoms and co-morbidities requiring interventions, including medication (11), pacing (12), catheter ablation (13), and surgery (14) and may also be associated with an increased risk for late death (7;12;15;16). However, little is known about the impact of heart rate and rhythm disorders on the daily lives of pediatric patients who have undergone the Fontan operation.
The goal of this study was to analyze heart rate and rhythm data from a large group of Fontan patients studied with a uniform protocol in order to define the incidence of heart rate and rhythm abnormalities in this patient population and to determine the impact of these abnormalities on quantifiable measures of functional outcome.
Methods
Fontan Cross-Sectional Study
This report is based on data from the Fontan Cross-Sectional Study executed by the Pediatric Heart Disease Clinical Research Network of the National Heart Lung and Blood Institute. The primary aim of this main study was to assess the correlation between functional health status and measures of ventricular performance in children ages 6 to 18 years who have undergone a Fontan procedure. Details regarding the structure of the Pediatric Heart Network and the general methods of the Fontan Cross-Sectional Study have been reported previously (17). Informed consent was obtained and data was collected at each of the participating centers according to the rules of each institution's internal review board.
Heart Rate, Heart Rhythm, and Functional Analysis – Patient Sample
There were 546 subjects enrolled in the Fontan Cross-Sectional Study. Twenty-five patients were excluded from this analysis of heart rate and rhythm: In 17, neither an ECG or exercise test were available; seven had undergone surgical conversion of the Fontan circuit, which may have had an impact on arrhythmia development(14); and one had second degree AV block, leaving 521 subjects in the analytic dataset.
Some additional exclusions were applied for selected heart rate and rhythm analyses. Patients with a pacemaker may have had a falsely elevated heart rate at rest and during exercise, while patients taking antiarrhythmic drugs may have had a falsely lowered heart rate. Thus the physiologic relationship between underlying heart rate and outcome in these patients might not be accurately identified. To avoid this possibility, 34 subjects with a rate-responsive pacemaker (n=5) and/or who were currently treated with beta-blockers or class III antiarrhythmics (n=30) were excluded from all heart rate analyses, and 43 subjects with a paced rhythm on resting ECG were excluded from the resting heart rate analysis.
Functional Outcome Measures
The Child Health Questionnaire (CHQ) Parent Report (CHQ-PF50) and the oxygen consumption (volume O2/kg/min)) at the anaerobic threshold (VAT) during exercise testing were used as measures of functional outcome. The Parent Report CHQ provides physical (CHQ-p) and psychosocial (CHQ-ps) summary scores to describe the well-being of children 5 to 18 years of age (18). This instrument has been used extensively to establish functional outcome in normal children as well as pediatric patients with various diseases and is among the most reliable tools for this purpose (19). For this study, VAT was used as the marker for exercise performance, since it is less effort dependent than other measures and reflects performance at lower levels of exercise.
ECG
A standard 12 lead electrocardiogram (ECG) was performed in the supine position and recorded at 25 mm/sec sweep speed with a 10 mm/mV amplitude. All ECG's were performed at supine rest and before any exercise testing. Bradycardia was defined as a resting heart rate less than the 5th percentile for age (20).
Exercise Testing
A 12-lead ECG was continuously monitored during the exercise protocol. Arterial oxygen saturation was measured transcutaneously at rest and continuously during exercise. Maximal exercise testing was performed using a standard ramp protocol on an electronically braked cycle ergometer (21).
Oxygen consumption (VO2) and carbon dioxide production (VCO2) were measured continously. VAT was measured using the V-slope method in those children in whom it could be accurately determined.
Peak heart rate percent predicted of normal for age was calculated as (peak heart rate/(220 – age))×100. Chronotropic index (22) was calculated as (peak heart rate - resting heart rate) /(0.925×(220 - age - resting heart rate)).
Statistical Analysis
Groups were defined by resting heart rate < 5th percentile, peak heart rate < 75% of predicted for age, history vs. no history of atrial tachycardia, and current vs. no pacemaker use. A Fisher exact test was used when comparing the distributions of a categorical variable by group and the Wilcoxon rank sum test was used for comparison of the distribution of most continuous variables. Student's t-test was used to compare the distributions of resting heart rate. The Pearson rank correlation coefficient was used to estimate the association between pairs of continuous measures. Multivariate linear regression was used to identify independent predictors of functional outcome, defined as VAT and CHQ-p (physical) summary score. A p-value of <0.05 was considered statistically significant.
Results
Enrollment, Demographics and History
Of the 521 subjects in the analytic cohort, 509 had a supine ECG, 404 completed a bicycle exercise test with VAT measured in 311, and 489 had analyzable CHQ-p summary scores.
Table 1 displays patient demographics. The mean age at enrollment was 11.9±3.4 years (median 11.3) and at the Fontan procedure was 3.4±1.9 years (median 2.8). There were more males (61%) than females. Of 389 patients who had undergone a staged second procedure, many more (70%) underwent the bidirectional Glenn (BDG) than the hemi-Fontan (HF). The intracardiac lateral tunnel was the most frequent form of Fontan procedure seen in these patients (59%) and the 3 other major forms were equally distributed amongst the remainder of the patients. Sixty-eight patients (13%) had a pacemaker at the time of the study. Fifty patients (10%) had a history of atrial tachycardia, defined as atrial tachycardia noted in the medical record or present on the study ECG or exercise test.
Table 1. Fontan Cross-Sectional Study Patient Characteristics for 521 Subjects with an ECG or undergoing an Exercise Test.
| Characteristic | n | Result |
|---|---|---|
| Age at enrollment, yr (median) | 521 | 11.9±3.4 (11.3) |
| Age at Fontan procedure, yr (median) | 521 | 3.4±1.9 (2.8) |
| Male | 521 | 315 (60.5%) |
| Race | 519 | |
| White | 411 (79.2%) | |
| Black | 55 (10.6%) | |
| Asian | 14 (2.7%) | |
| Other | 39 (7.5%) | |
| Type of Volume | 389 | |
| Unloading Surgery | ||
| Bi-directional Glenn | 272 (69.9%) | |
| Hemi-Fontan | 101 (26.0%) | |
| Other | 16 (4.1%) | |
| Fontan Type | 521 | |
| Atriopulmonary connection | 72 (13.8%) | |
| Intracardiac lateral tunnel | 307 (58.9%) | |
| Extracardiac lateral tunnel | 62 (11. %) | |
| Extracardiac conduit | 69 (13.2 %) | |
| Other | 11 (2.1%) | |
| Current Pacemaker | 521 | 68 (13.1%) |
| History of Atrial Tachycardia | 521 | 50 (9.6%) |
Heart Rate and Rhythm
Resting Rhythm
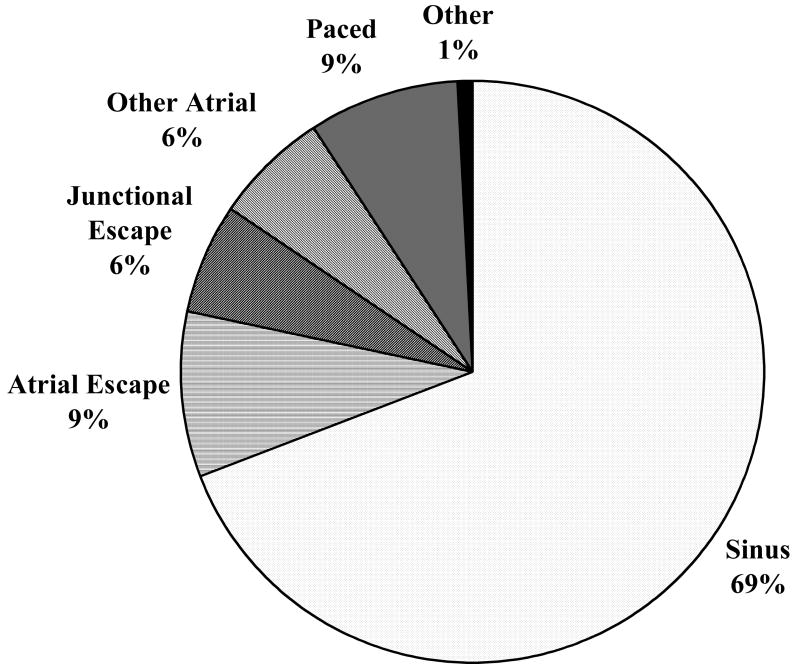
Sinus rhythm was the predominant rhythm on the resting supine ECG in only 69% of patients (Figure 1). Among 470 patients with a P wave on ECG, 20% had a low right atrial rhythm and 5% had a left atrial focus. Although 13% of patients had a pacemaker, during the resting supine ECG only 63% of these were paced in the following modes: AAI(R) (69%), DDD(R) (28%), or DDIR (3%).
Figure 1. Predominant Rhythm on Resting ECG in 509 Fontan procedure survivors aged 12±3 years.
Resting Heart Rate
After appropriate exclusions (see Methods), the average resting heart rate on ECG was 76±16 bpm. Resting heart rate decreased slightly with age (R = -0.15, 95% confidence interval -0.24 to -0.06, p=0.001). Over one-quarter (27%) of patients had a resting heart rate below the 5th percentile for age, but only 0.7% had resting heart rates above the 95th percentile for age. Patients with resting heart rates < 5th percentile for age were less likely to be in sinus rhythm and more likely to be in junctional escape rhythm than those patients with resting heart rates > 5th percentile for age (67% vs 79% in NSR and 16% vs 3% in junctional rhythm, respectively, p<0.0001).
Peak Heart Rate
The average peak heart rate during exercise testing in 371 patients was 157±21 bpm, and was not associated with age (R = 0.07, 95% confidence interval -0.04 to 0.17, p=0.211). Low peak heart rate, defined as less than 75% of predicted for age, was observed in 41% of patients. Mean change in heart rate (peak minus resting) was 83±26 bpm, and the mean chronotropic index (n=340) was 0.67±0.19 (median 0.70), with 73% having an abnormally low chronotropic index < 0.8.
Multiple Heart Rate and Rhythm Abnormalities
Many subjects had multiple heart rate and rhythm abnormalities. Nine percent had a resting heart rate below the 5th percentile for age and non-sinus rhythm on resting ECG, and 10.9% had a resting heart rate below the 5th percentile for age plus a peak heart rate below 75% of predicted. However, 61% of the 96 patients who had a resting heart rate below the 5th percentile for age had a peak heart rate ≥ 75% of predicted.
Functional Outcomes
Mean CHQ-p and CHQ-ps for the group were lower than historic healthy controls (CHQ-p was 45.4±11.8 (median 49.3) vs. 53.0±8.8 for historic controls and CHQ-ps was 47.3±10.9 (median 48.9) vs 51.2±9.1 for historic controls (18,19). Mean VAT was low at 18.8±6.4 ml/kg/min.
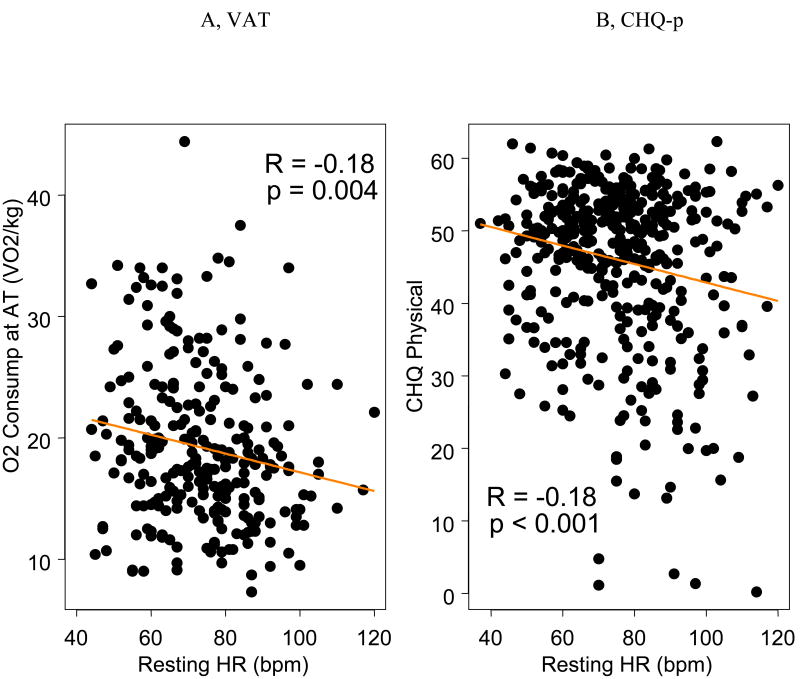
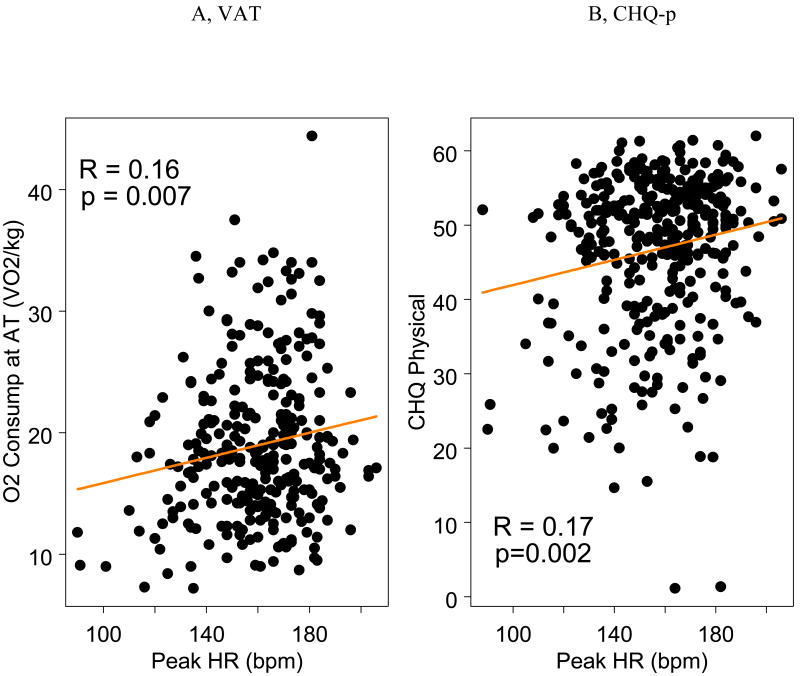
Associations with Oxygen Consumption at the Anaerobic Threshold (VAT)
VAT was measured in 311 subjects. Higher VAT was weakly associated with lower resting heart rate (R = -0.18, 95% confidence interval -0.27 to -0.09, p = 0.004, Figure 2A) and higher peak heart rate (R = 0.16, 95% confidence interval 0.04 to 0.27, p = 0.07, Figure 3A). When the association between continuous predicted peak heart rate and VAT was examined, the strength and significance of the association was similar to the association between raw peak heart rate and VAT.
Figure 2. Resting Heart Rate and Functional Outcome in Fontan Procedure Survivors. AT=Anaerobic Threshold; CHQ Physical=Child Health Questionnaire (Parent Report) Physical Summary Score; HR = Heart Rate.
Figure 3. Peak Heart Rate and Functional Outcome in Fontan Procedure Survivors. AT=Anaerobic Threshold; CHQ Physical=Child Health Questionnaire (Parent Report) Physical Summary Score; HR = Heart Rate.
VAT was not associated with bradycardia (resting heart rate below the 5th percentile for age) or the presence of an atrial pacemaker. (Table 2). Although patients with an abnormal P-axis had a higher VAT than those with a normal axis (20.7±6.8 vs. 18.4±6.2 ml/kg/min, p=0.02), VAT did not differ by predominant rhythm, including junctional rhythm, on resting ECG. VAT did not differ by history of atrial tachycardia status or by the use of anti-arrhythmic medication. A multivariate model for VAT (n=251) using age, rate and rhythm variables demonstrated that younger age (0.77 ml/kg/min increase per one year decrease in age, p<0.001), lower resting heart rate (0.91 ml/kg/min increase per 10 beats per minute decrease at rest, p <0.001), higher peak heart rate (0.44 ml/kg/min increase per 10 beats per minute increase during exercise, p = 0.03), and an abnormal P-axis (2.59 ml/kg/min decrease if P-axis is between 0 and 90 degrees, p = 0.004) were independent predictors of better performance and accounted for 20% of the variation in VAT. Furthermore, the association between age and resting and peak heart rate was observed at all ages, without a difference between age groups (interaction p-value 0.77 and 0.41, respectively)
Table 2. Heart Rate and Rhythm Associations with O2 consumption at the anaerobic threshold (VAT) and Parent Report Child Health Questionnaire Physical Summary Score (CHQ-p).
| n | VAT (ml/kg/min) | n | CHQ-p | ||
|---|---|---|---|---|---|
| Resting Heart Rate | |||||
| <5th percentile for age | 75 | 20.1±6.9 (median 19.2) | 117 | 48.1±8.4 (median 50.0) | |
| ≥5th percentile for age | 185 | 18.8±6.3 (median 17.6) | 302 | 45.2±12.0 (median(48.7) | |
| p | .137 | .154 | |||
|
| |||||
| Peak Heart Rate | |||||
| <75% of predicted for age | 98 | 18.5±6.2 (median 18.0) | 142 | 45.3±11.3 (median 18.0) | |
| ≥75% of predicted for age | 191 | 19.2±6.4 (median 17.9) | 210 | 47.8±9.7 (median 50.3) | |
| p | .539 | .082 | |||
|
| |||||
| Current pacemaker | 41 | 18.1±5.9 (median 17.0) | 61 | 40.8+14.1 (median 45.0) | |
| No current pacemaker | 270 | 18.9±6.5 (median 18.1) | 428 | 46.0±11.3 (median 49.5) | |
| p | 0.509 | 0.007 | |||
| History of AT | 30 | 17.2±6.7 (median 15.7) | 45 | 38.8±15.0 (median 45.2) | |
| No History of AT | 281 | 19.0±6.4 (median 18.1) | 444 | 46.0±11.3 (median 49.8) | |
| p | 0.081 | 0.0008 | |||
| Abnormal P-Axis | 64 | 20.7±6.8 (median 19.1) | 110 | 43.3±12.7 (median 46.4) | |
| Normal P-axis | 214 | 18.4±6.2 (median 17.4) | 334 | 46.0±11.1 (median 49.6) | |
| p | 0.015 | 0.071 | |||
| Non-Sinus Rhythn | 89 | 19.8±6.5 (median 18.0) | 146 | 44.1±12.9 (median 48.2) | |
| Sinus Rhythm | 210 | 18.6±6.4 (median 17.8) | 333 | 45.7±11.3 (median 49.5) | |
| p | 0.183 | 0.394 | |||
AT = atrial tachycardia.
Associations with Child Health Questionnaire, Physical Summary Score (CHQ-p)
Patients with lower resting heart rates had higher CHQ-p scores reflecting better functional outcome (R = -0.18, 95% confidence interval -0.27 to 0.09, p<0.001, Figure 2B). However, bradycardia was not specifically related to CHQ-p, since mean CHQ-p was similar for patients with a resting heart rate at or above vs. below the 5th percentile for age (Table 2). Patients with a higher peak heart rate had higher CHQ-p scores (R = 0.17, 95% confidence interval 0.06 to 0.27, p = 0.002, Figure 3B). When the association between continuous predicted peak heart and CHQ-p score was examined, the strength and significance of the association was similar to the association between raw peak heart rate and CHQ-p score. Greater changes in heart rate (peak heart rate minus resting heart rate) were associated with higher CHQ-p (R = 0.19, 95% confidence interval 0.08 to 0.29, p<0.001) scores. The presence of an atrial pacemaker was associated with a lower mean CHQ-p score as was a positive history of atrial tachycardia (Table 2). Patients who were treated with beta-blockers or class III antiarrhythmics had lower CHQ-p scores than those who were not treated with these medications (38.3±15.9 vs. 45.9±11.3, p = .005). Other than having a paced rhythm on resting ECG, predominant rhythm, including junctional rhythm, was not associated with a lower CHQ-p. A multivariate model for CHQ-p score (n=324) using age and rate and rhythm variables demonstrated that resting heart rate (8.1 point increase in CHQ-p score per 10 beats per minute decrease at rest, p = 0.02) and peak heart rate (7.0 point increase in CHQ-p score per 10 beats per minute increase during exercise, p = 0.01), were both independent predictors of CHQ-p. However, these variables accounted for only 4% of the variation in CHQ-p scores. Age, predominant rhythm, a history of atrial tachycardia, the presence of a pacemaker, and the change from resting to peak heart rate were not independently associated with CHQ-p after accounting for resting and peak heart rate.
Associations with Child Health Questionnaire, Psychosocial Summary Score (CHQ-ps)
None of the heart rate and rhythm variables were associated with CHQ-ps.
Discussion
This study provided a unique opportunity to analyze the associations of heart rate and rhythm with functional outcome in a large group of Fontan patients collected from 7 centers during a relatively uniform surgical era, offering new insight into the potential impact of these factors on the daily lives of Fontan patients. The specific new findings in this study are: 1) resting heart rate as a continuous measure was inversely related to functional outcome measured by VAT and CHQ-p, 2) bradycardia (resting heart rate < 5th percentile for age) was not related to poor functional outcome and 3) although lower than normal, peak heart rate during exercise was positively correlated with both VAT and CHQ-p. Additionally, this large sample, with its well-defined criteria for heart rate and rhythm abnormalities, provides a more accurate description of the prevalence of rate and rhythm abnormalities in Fontan patients than has been previously available.
Heart Rate and Functional Outcome
The most intriguing finding in this study is that, independent of age, lower resting heart rate was not associated with worsened functional outcome. Since heart rate normally falls with age and outcome usually worsens with age, the relationship between resting heart rate and outcome should be even stronger if age-adjusted heart rates were available for use or could be accurately derived from existing data. Further, despite a large number of patients with bradycardia, defined as a resting heart rate < 5th percentile for age, bradycardia was not associated with decreased functional status. On the surface, this finding appears to be at odds with previous studies that have associated sinus node dysfunction with lower physical performance. Sinus node dysfunction has often been broadly defined as various combinations of the following: non-sinus rhythm on resting ECG, low resting heart rate, low peak heart rate response to exercise, or long pauses (1-12;15;16; 23;24). However, these prior studies have typically not separately analyzed the individual components of sinus node dysfunction, perhaps accounting for the differences with the findings in the present study.
One possible explanation for the association between resting heart rate and functional outcome is that a high resting heart rate is an indicator of a poor functional state, perhaps due to low cardiac output and reflex sympathetic stimulation. Conversely, we speculate that a low resting heart rate may confer mechanical advantages to the Fontan ventricle. This may be related to longer diastolic filling times supporting the preload dependency of the Fontan circulation; or to improvement in load-independent diastolic mechanics. Of note, very few patients had a resting heart rate above the 95th percentile for age. The data in this study do not address whether a low resting heart rate is part of a compensatory mechanism; however, previous authors have proposed that resting bradycardia in Fontan patients may be more likely secondary to surgical or functional autonomic derangements, with selective reduction of cardiac sympathetic activation rather than sinus node dysfunction (25). Any link between autonomic function and the association between higher CHQ-p score and lower heart rate will need to be substantiated in further studies.
The role of peak heart rate in these patients may be more complex. It is clear the population had an abnormal heart rate response to exercise with 73% of subjects having an abnormally low chronotropic index. The chronotropic index may be a better representation of the expected peak heart rate response to exercise than the formula [peak heart rate = 220 – age(years)](22). It is less clear whether the abnormal chronotropy is secondary to intrinsic sinus node dysfunction, autonomic derangements or other mechanisms. Regardless of the etiology, a higher peak heart rate was associated with a higher VAT and a higher CHQ-p. Although this relationship was found to be weak in this group of Fontan patients, its existence is no different than in patients with normal hearts (26), where increasing heart rate is the most important mechanism for augmenting cardiac output during exercise.
Although other studies have demonstrated that pacing is indicated in Fontan patients with symptomatic bradycardia (1,3,4), the clinical message from this study might be that good functional outcomes in patients with low resting heart rates suggests that placement of a pacemaker for asymptomatic bradycardia might not improve clinical status and may warrant very careful reconsideration. Since a higher peak heart rate was also correlated with better functional outcome, failure to increase heart rate during exercise may be a better indicator of pacemaker necessity, but this needs to be evaluated in a prospective manner.
Heart Rate and Rhythm Abnormalities
Despite the more recent surgical era represented in the present study, the high incidence of heart rate and rhythm abnormalities in this Fontan population is consistent with that reported by previous authors (1-10). In the present study, 27% of patients had resting heart rates below the 5th percentile for age, 31% had a non-sinus rhythm on resting ECG, and 41% had a peak heart rate less than 75% predicted. Previous studies defined sinus node dysfunction as having any one of these abnormalities (1-3), with a prevalence of up to 44% in select series (4). Fishberger et al reported that 9.2% of Fontan patients had a pacemaker after a mean follow up of 6 years (7), similar to the 13% prevalence during a follow up of about 8.5 years in this study. Interestingly, the incidence of atrial tachycardia in the present study was lower than reported in prior studies despite a longer follow up period (9.6% at 8.5 years compared to 16-17% at 5 years (1;5)). Thus, the impact of the more recent era may have been greater on the development of atrial tachycardia than on other heart rate and rhythm abnormalities.
Limitations
Despite the important findings presented here, this study has several limitations. First, since the study was observational, causality cannot be inferred from the associations identified. Second, although this study suggests that lower resting and higher peak heart rates may be beneficial in Fontan patients, these variables accounted for only 8% of the variance in CHQ-p, indicating that other factors may be more important in determining CHQ-p than heart rate. Third, the associations found between heart rate and CHQ-p or VAT arose from a sub-sample of the study cohort, which excluded patients who were paced and those on anti-arrhythmic medication. Since the study design did not allow for the reprogramming of pacemakers so that underlying rhythm could be manifest when assessing heart rate, it is unknown whether the relationships between underlying heart rate and CHQ-p or VAT would have been different in those patients with a pacemaker. However, despite exclusion of paced patients in the heart rate analysis, a large number of patients without a pacemaker had bradycardia and were included in the analysis, indicating that the results are reasonably applicable to most Fontan patients. It is possible that the patients with pacemakers may have had more profound bradycardia than the bradycardic patients without pacemakers. Thus, excluding paced patients does not necessarily negate the relationship between resting heart rate and outcome for even the paced patients.
Fourth, there was not a core laboratory for the ECG or exercise testing interpretation, so that institutional variability could have influenced the results. Fifth, a definition of atrial tachycardia based upon chart review, study ECG, or exercise test may have underestimated the incidence of this problem compared to methods such as 24-hour electrocardiographic monitoring and electrophysiology study. Finally, associations with VAT have to be interpreted cautiously since only 311 patients had valid VATs reported. For subjects who underwent exercise testing, those with a VAT measurement had better physical functioning on CHQ than those without a VAT measurement. In general, the analyses of VAT as an outcome measure for Fontan subjects are based on an older and possibly somewhat healthier cohort than the other findings. Inability to reach VAT may be an important determinant of functional outcome by itself.
Conclusions
In pediatric patients (6-18 yrs) following the Fontan procedure, a lower resting heart rate and a higher peak heart rate during exercise are each independently associated with improved physical functional outcome as measured by the physical component of the Child Health Questionnaire and the oxygen consumption at the anaerobic threshold. However, these correlations are weak suggesting that other, non-rhythm and non-rate, factors may have a greater impact on the functional outcome of pediatric Fontan patients.
Acknowledgments
National Heart, Lung, and Blood Institute: Gail Pearson, Tracey Hoke, Carl Hunt, Mario Stylianou, Judith Massicot-Fisher, Marsha Mathis, Victoria Pemberton
Data Coordinating Center: New England Research Institutes, Lynn Sleeper, Steven Colan, Paul Mitchell, Gloria Klein, Dianne Gallagher, Patty Connell, Lisa Wruck
Network Chair: Lynn Mahony, University of Texas Southwestern Medical Center
Clinical Site Investigators: Children's Hospital Boston, Jane Newburger (PI), Stephen Roth, Roger Breitbart, Renee Margossian, Andrew Powell, Jonathan Rhodes, Jodi Elder, Ellen McGrath; Children's Hospital of New York, Welton M. Gersony (PI), Seema Mital, Beth Printz, Ashwin Prakash, Darlene Servedio; Children's Hospital of Philadelphia, Victoria Vetter (PI), Bernard J. Clark, Mark Fogel, Steven Paridon, Jack Rychik, Margaret Harkins, Jamie Koh; Duke University, Page A. W. Anderson (PI), Rene Herlong, Lynne Hurwitz, Jennifer S. Li, Ann Marie Nawrocki; Medical University of South Carolina, J. Philip Saul (PI), Andrew M. Atz, Andrew D. Blaufox, Girish Shirali, Jon Lucas, Amy Blevins; Primary Children's Medical Center, Salt Lake City, Utah, LuAnn Minich (PI), Richard Williams, Linda Lambert, Michael Puchalski; Hospital for Sick Children, Toronto, Brian McCrindle (PI), Timothy Bradley, Kevin Roman, Jennifer Russell, Shi-Joon Yoo, Elizabeth Radojewski, Nancy Slater
Core Laboratories: Cardiac MRI, Children's Hospital Boston: Tal Geva; Andrew J. Powell
Echocardiography, Children's Hospital Boston: Steven Colan (Director), Marcy Schwartz, Renee Margossian
Protocol Review Committee: Michael Artman, Chair; Judith Massicot-Fisher, Executive Secretary; Erle Austin, Daniel Bernstein, Timothy Feltes, Julie Johnson, Jeffrey Krischer, G. Paul Matherne, Anne Murphy, ad hoc, Anne Rowley, ad hoc.
Data and Safety Monitoring Board: John Kugler, Chair; Tracey R. Hoke, Executive Secretary; Kathryn Davis, David J. Driscoll, Mark Galantowicz, Sally A. Hunsberger, Thomas J. Knight, Catherine L. Webb, Lawrence Wissow.
Funding Sources: This work was supported by U01 HL068281, U01 HL068270, U01 HL068292, U01 HL068285, U01 HL068290, U01 HL068269, U01 HL068288, and U01 HL068279 from National Heart, Lung, and Blood Institute, NIH/DHHS
Abbreviations
- HR
Heart rate
- NHLBI
National Heart Lung and Blood Institute
- ECG
Electrocardiogram
- ET
Exercise test
- CHQ
Child Health Questionnaire
- VAT
Oxygen consumption at anaerobic threshold
- CHQ-p
Child Health Questionnaire-physical
- CHQ-ps
Child Health Questionnaire-psycho-social
- VO2
Oxygen consumption
- VCO2
Carbon dioxide production
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.Fishberger SB, Wernovsky G, Gentles TL, Gauvreau K, Burnett J, Mayer JE, Walsh EP. Factors that influence the development of atrial flutter after the fontan operation. J Thorac Cardiovasc Surg. 1997;113:80–86. doi: 10.1016/s0022-5223(97)70402-1. [DOI] [PubMed] [Google Scholar]
- 2.Cohen MI, Bridges ND, Gaynor J, Hoffman T, Wernovsky G, Vetter VL, Spray T, Rhodes LA. Modifications to the Cavopulmonary Anastomosis do not Eliminate Early Sinus Node Dysfunction. J Thorac Cardiovasc Surg. 2000 Jan 1;120:891–901. doi: 10.1067/mtc.2000.109708. [DOI] [PubMed] [Google Scholar]
- 3.Driscoll DJ, Offord KP, Feldt RH, Schaff HV, Puga FJ, Danielson GK. Five- to fifteen-year follow-up after Fontan operation. Circulation. 1992;85(2):469–496. doi: 10.1161/01.cir.85.2.469. [DOI] [PubMed] [Google Scholar]
- 4.Cohen MI, Wernovsky G, Vetter VL, Wieand TS, Gaynor J, Jacobs M, Spray T, Rhodes LA. Sinus Node Function After a Systematically Staged Fontan Procedure. Circulation. 1998;98:II-352–II-359. [PubMed] [Google Scholar]
- 5.Durongpisitkul K, Porter CJ, Cetta F, Offord KP, Slezak JM, Puga FJ, Schaff HV, Danielson GK, Driscoll DJ. Predictors of Early and Late-Onset Supraventricular Tachycarrhythmias After Fontan Operation. Circulation. 1998;98:1099–1107. doi: 10.1161/01.cir.98.11.1099. [DOI] [PubMed] [Google Scholar]
- 6.Cecchin F, Johnsrude CL, Perry JC, Friedman RA. Effect of age and surgical technique on symptomatic arrhythmias after the Fontan procedure. Am J Cardiol. 1995;76(5):386–391. doi: 10.1016/s0002-9149(99)80106-4. [DOI] [PubMed] [Google Scholar]
- 7.Fishberger SB, Wernovsky G, Gentles TL, Gamble WJ, Gauvreau K, Burnett J, Mayer JE, Walsh EP. Long-term outcome in patients with pacemakers following the Fontan operation. Am J Cardiol. 1996;77(10):887–889. doi: 10.1016/s0002-9149(97)89191-6. [DOI] [PubMed] [Google Scholar]
- 8.Bae E, Lee J, Noh CI, Kim W, Kim Y. Sinus node dysfunction after Fontan modifications-influence of surgical method. Int J Cardiol. 2003;88:285–291. doi: 10.1016/s0167-5273(02)00530-2. [DOI] [PubMed] [Google Scholar]
- 9.Dilawar M, Bradley SM, Saul JP, Stroud S, Balaji S. Sinus Node Dysfunction after Intraatrial Lateral Tunnel and Extracardiac Conduit Fontan Procedures: A Study of 24-Hour Holter Recordings. Pediatr Cardiol. 2003;24:284–288. doi: 10.1007/s00246-002-0238-9. [DOI] [PubMed] [Google Scholar]
- 10.Manning PB, Mayer JE, Jr, Wernovsky G, Fishberger SB, Walsh EP. Staged operation to Fontan increases the incidence of sinoatrial node dysfunction. J Thorac Cardiovasc Surg. 1996;111(4):833–839. doi: 10.1016/s0022-5223(96)70344-6. [DOI] [PubMed] [Google Scholar]
- 11.Triedman JK. Atrial Reentrant Tachycardias. In: Walsh EP, Saul JP, Triedman JK, editors. Cardiac Arrhythmias in Children and Young Adults with Conenital Heart Disease. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 137–160. [Google Scholar]
- 12.Rhodes LA, Saul JP, Gamble WJ, Walsh EP. Benefits and potential risks of atrial antitachycardia pacing after repair of congenital heart disease. J Am Coll Cardiol. 1993;21:107A. doi: 10.1111/j.1540-8159.1995.tb04741.x. [DOI] [PubMed] [Google Scholar]
- 13.Triedman JK, Alexander ME, Love BA, Collins KK, Berul CI, Bevilacqua LM, Walsh EP. Influence of Patient Factors and Ablative Technologies on Outcomes of Radiofrequency Ablation of Intra-Atrial Reentrant Tachycardia in Patients with Congenital Heart Disease. J Am Coll Cardiol. 2002;39:1827–1835. doi: 10.1016/s0735-1097(02)01858-2. [DOI] [PubMed] [Google Scholar]
- 14.Mavroudis C, Backer CL, Deal BJ, Johnsrude CL. Fontan conversion to cavopulmonary connection and arrhythmia circuit cryoblation. J Thorac Cardiovasc Surg. 1998;115(3):547–556. doi: 10.1016/s0022-5223(98)70316-2. [DOI] [PubMed] [Google Scholar]
- 15.Gentles TL, Mayer JE, Gauvreau K, Newburger JW, Lock JE, Kupferschmid JP, Burnett J, Jonas RA, Castaneda AR, Wernovsky G. Fontan operation in five hundred consecutive patients: factors influencing early and latge outcome. J Thorac Cardiovasc Surg. 1997;114:379–391. doi: 10.1016/s0022-5223(97)70183-1. [DOI] [PubMed] [Google Scholar]
- 16.Ghai A, Harris L, Harrison DA, Webb GD, Siu SC. Outcomes of Late Atrial Arrhythmias in Adults After the Fontan Operation. J Am Coll Cardiol. 2001;37:585–592. doi: 10.1016/s0735-1097(00)01141-4. [DOI] [PubMed] [Google Scholar]
- 17.McCrindle BW, Williams RV, Mitchell PD, Hsu DT, Paridon SM, Atz AM, Li JS, Newburger JW, Pediatric Heart Network Investigators Relationship of patient and medical characteristics to health status in children and adolescents after the Fontan procedure. Circulation. 2006 Feb 28;113(8):1123–9. doi: 10.1161/CIRCULATIONAHA.105.576660. [DOI] [PubMed] [Google Scholar]
- 18.Landgraf JM, Abetz L, Ware JE. The CHQ user's Manual. 1st. Boston: The Health Institute, New England Medical Center; 1996. [Google Scholar]
- 19.Schmidt L, Garratt A, Fitzpatrick R. Child/parent-assessed population health outcome measures: a structured review. Child Care Health Dev. 2002;28:227–237. doi: 10.1046/j.1365-2214.2002.00266.x. [DOI] [PubMed] [Google Scholar]
- 20.Davignon A, Rautaharju P, Boiselle E, Soumis F, Megelas M, Choquette A. Normal ECG standards for infants and children. Pediatric Card. 1979;1:123–131. [Google Scholar]
- 21.Cooper DM, Weiler-Ravell D. Gas exchange response to exercise in children. Am Rev Respir Dis. 1984;129(2 Pt 2):S47–8. doi: 10.1164/arrd.1984.129.2P2.S47. [DOI] [PubMed] [Google Scholar]
- 22.Gerhard-Paul D, Konstantinos D, Darlington O, et al. Heart rate response during exercise predicts survival in adults with congenital heart disease. Pediatr Cardiol. 2006;48:1250–1256. doi: 10.1016/j.jacc.2006.05.051. [DOI] [PubMed] [Google Scholar]
- 23.Gardiner HM, Dhillon R, Bull C, de Leval MR, Deanfield JE. Prospective study of the incidence and determinants of arrhythmia after total cavopulmonary connection. Circulation. 1996;94(9SupplSuppl):II17–21. [PubMed] [Google Scholar]
- 24.Gelatt M, Hamilton RM, McCrindle BW, Gow RM, Williams WG, Trusler GA, Freedom RM. Risk factors for atrial tachyarrhythmias after the Fontan operation. Journal of the American College of Cardiology. 1994;24(7):1735–1741. doi: 10.1016/0735-1097(94)90181-3. [DOI] [PubMed] [Google Scholar]
- 25.Davos CH, Francis DP, Leenarts MF, Yap SC, Li W, Davlouros PA, Wensel R, Coats AJ, Piepoli M, Sreeram N, Gatzoulis MA. Global impairment of cardiac autonomic nervous activity late after the Fontan operation. Circulation. 2003;108 1:II180–5. doi: 10.1161/01.cir.0000087946.47069.cb. [DOI] [PubMed] [Google Scholar]
- 26.Bauer R, Busch U, van de Flierdt E, Stettmeier H, Raab W, Langhammer HR, Pabst HW. Age-related heart function in patients with healthy hearts. Z Kardiol. 1988;77:632–41. [PubMed] [Google Scholar]