Abstract
We report a case of L4–L5 traumatic anterolisthesis. The patient was treated surgically 4 months after the injury. His radiological and operative findings showed L4 inferior facet tip fracture, L4–L5 anterior displacement and left L4–L5 foraminal disc protrusion. Decompression, reduction with L3, L4, L5 pedicular screw fixation, L4–L5 disc excision and interbody cage insertion with autologous bone grafts were done. Flexion type injury was thought to be the probable mechanism.
Keywords: Anterolisthesis, Traumatic spondylolisthesis, Spine fixation
Introduction
Traumatic spondylolisthesis is an uncommon entity reported in the literature. Watson-Jones described the first case in 1940 and about hundred cases reported since then [8]. All reported cases are traumatic lumbosacral dislocations, which represents a dislocation on L5–S1 level.
For the best of our knowledge, we present a unique case of L4–L5 traumatic anterolisthesis, and discuss the probable physiopathologic mechanism with surgical management.
Case report
A 44-year-old man was the driver of a tractor that has crashed to a tree and he was thrown to the ground. He was taken to a hospital and was diagnosed as traumatic spondylolisthesis of L4–L5 (Figs. 1, 2). He was then treated conservatively in another hospital for 4 months, as he did not want to be operated. The first 25 days was an absolute bed rest and then he was mobilized with a soft lumbosacral corset.
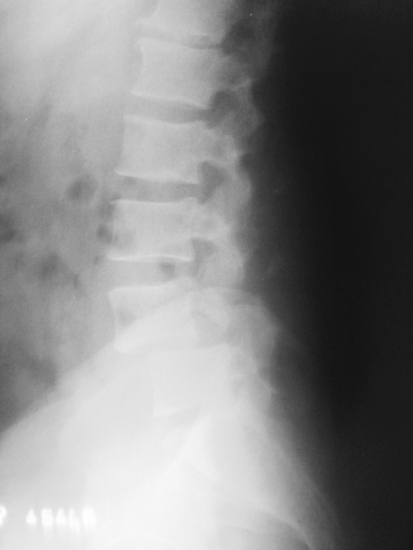
Fig. 1.
Lateral X-ray after trauma showing L4–L5 spondylolisthesis
Fig. 2.
Preoperative AP X-ray
The complaints of low back pain, numbness and weakness in both lower extremities by walking at about 50 m persisted and he decided to be operated after 4 months.
Additional preoperative computed tomography, plain radiography and magnetic resonance images showed L4 inferior facet tip fracture and dislocation, grade 2 L4–L5 spondylolisthesis and left L4–L5 foraminal disc herniation (Figs. 3, 4, 5) On neurological examination, hipoactivity of both Aschiles reflexes was found. He underwent surgery for L4–L5 dislocation. At operation bilateral facet dislocation and fractured tip of inferior L4 facets were confirmed. Decompression, including disc excision and open reduction, posterolateral fusion with autologous bone grafts taken from posterior iliac crest were done followed by internal fixation from L3–L5 vertebrae, using six pedicular screws and two rods. L4–L5 interbody cage was also inserted, with autologous corticocancellous bone grafts from the decompression material, in order to perform high degree of stability and fusion rate (Figs. 6, 7). The patient was mobilized on the second postoperative day without any neurological symptoms and discharged on the third day. Three months after surgery, he was symptom free.
Fig. 3.
Reconstructed sagittal CT showing L4–L5 spondylolisthesis, facet dislocation and L4 inferior facet tip fracture
Fig. 4.
T2 weighted MR image showing L4–L5 spondylolisthesis and L4–L5 disc disruption
Fig. 5.
Axial MR image showing L4–L5 left foraminal disc herniation
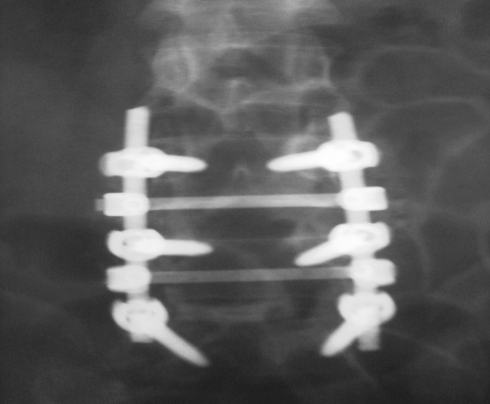
Fig. 6.
Postoperative AP X-ray
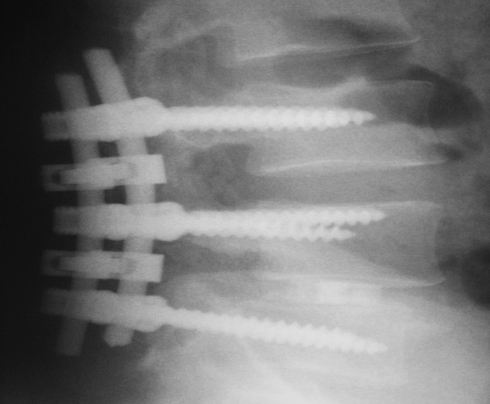
Fig. 7.
Postoperative lateral X-ray
Discussion
Spondylolisthesis was classified by Wiltse et al. into dysplastik, isthmic, degenerative, pathologic and traumatic types [9]. Acute traumatic type is very rare and should be distinguished from acute isthmic spondylolisthesis, in which acute pars interarticularis fracture occurs probably due to a predisposed spondylolysis. Magnetic resonance imaging is mandatory to evaluate the integrity of disc content, ligamentous structure injury and neural compression.
Different treatment modalities are proposed to treat the dislocation. Although there are some reports of successful conservative treatment, open decompression and to a certain site reduction with internal segmental fixation and fusion are the most accepted treatment modalities [5, 7]. There is no any neurological worsened case after the operation; they remained same or improved clinically at the reported cases. In the event of a traumatic disruption of the disc material, it should be excised for decompression, preferably with interbody fusion. Interbody fusion allows higher degree of stability and fusion rate. The anterior support reduces the risk of implant failure [4]. It may be performed anteriorly, especially if the disc height is needed to be restored, otherwise it may be done posteriorly. In grade 2 or more, listhesis reduction should be achieved before interbody placements. Autologous bone substitute is the gold standard with or without a cage insertion. If the disc material is intact, especially with ligamentous structures, at grade 1 or 2 spondylolisthesis, the necessity of the interbody fusion may be controversial, but it is mandatory to search neural canal and bilateral foraminal compression due to a disc protrusion especially after reduction.
Fracture dislocation of L5–S1 is a rare and severe lesion of the lumbosacral junction usually secondary to violent trauma of the lumbosacral area. Many physiopathologic hypotheses have been proposed concerning the mechanism. Watson-Jones pointed hyperextension stress as an efficient traumatic vector in the first reported case of lumbosacral dislocation [8]. Roaf suggested that hyperflexion axial rotation and compression forces were responsible for anterior lumbosacral dislocation [6]. Most of the authors considered that the main mechanism responsible for anterior or anterolateral lumbosacral dislocation is hyperflexion with compression [6, 7]. There are also reports of direct traumatic vectors that act as a tangential force applied to the L5–S1 apophyseal joints and cause the dislocation to occur and also hyperextension with compression and anterior translation is reported [5, 6].
Interestingly in our L4–L5 traumatic anterior dislocation case, different from most reported L5–S1 traumatic dislocations, there was no single transverse process fracture. Transverse process fracture is mostly attributed as a sign of the severity of the trauma and is thought to be a warning finding for physician to search for traumatic spondylolisthesis [1, 6, 7].
Although there was no significant progression of the displacement of the lesion, conservative treatment was insufficient in our patient and the patient was operated for his complaints, which the neurological claudication was the predominant symptom.
Facet dislocations occur frequently in the cervical region, less frequently in the upper thoracic region and rare in the lumbar region. Their more common occurrence in the cervical and thoracic spine is caused by the relatively coronal orientation of the facet joints in these regions. An exaggerated flexion is the mechanism of the injury in bilateral facet dislocation and a flexion moment combined with a rotational component most commonly results in unilateral facet dislocation. In facet dislocation, fracture, perching, or locking may occur. Also hyperextension type injury if combined with an axial load may result in facet fracture, laminar fracture may accompany to that kind of injury. In the lumbar region, the facet joints are able to slide past each other during extension, thus minimizing the chance for facet fracture by this mechanism [3]. In the lumbar region, the facet joints are oriented in a sagittal plane. Their ability to resist flexion or translation is minimal, whereas their ability to resist rotation is substantial. The facet joints do not support axial loads unless the spine is in an extension posture. Also at the lumbosacral junction, the angle of the sacrum in relation to the L5 vertebral body may substantially affect pathological processes. The greater the lumbosacral joint angle, the greater the applied translation forces are. The nearly coronal facet orientation at L5–S1 is a factor in the relatively decreased incidence of subluxation in the presence of intact facet joints; that is, in degenerative spondylolisthesis, subluxation is more common at L4–L5 than at L5–S1 despite the relative vertical orientation of the L5–S1 disc interspace [2].
The coronal facet orientation of L5–S1 and lumbosacral joint angle explains the reason why traumatic spondylolisthesis occurs mostly on L5–S1 level. It may be speculated that the weakness of the tip of this patient’s inferior articular process is the reason of L4–L5 traumatic spondylolisthesis.
We believe that traumatic spondylolisthesis with laminar fracture may probably be caused by an extension and axial load combination type injury, however, without laminar fracture hyperflexion type injury is the most likely cause, asymmetric lesions includes rotational component. But its occurrence mechanism in each particular case will be challenging to be exactly defined as both type of injury patterns with their subtypes, may cause to similar radiological findings. Biomechanical studies may help to understand the physiopathologic mechanisms.
Conclusions
As far as known, the first traumatic L4–L5 anterolisthesis is reported. The pathomechanism is thought to be a flexion type injury. Decompression, reduction with L3, L4, L5 pedicular screw fixation, L4–L5 disc excision and interbody cage insertion with autologous bone grafts were done.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Ahmed A, Mahesh BH, Shamshery PK, Jayaswal A. Traumatic retrolisthesis of the L4 vertebra. J Trauma. 2005;58:393–394. doi: 10.1097/01.TA.0000073998.94089.D1. [DOI] [PubMed] [Google Scholar]
- 2.Benzel EC. Biomechanics of spine stabilization. 1st edn. Illinois: Thieme; 2001. pp. 1–17. [Google Scholar]
- 3.Benzel EC. Biomechanics of spine stabilization. 1st edn. Illinois: Thieme; 2001. pp. 61–89. [Google Scholar]
- 4.Lamn M, Henriksen S-EH, Eiskjcer S. Acute traumatic L5–S1 spondylolisthesis. J Spinal Disord Tech. 2003;16:524–527. doi: 10.1097/00024720-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Reinhold M, Knop C, Blauth M. Acute traumatic L5–S1 spondylolisthesis: a case report. Arch Orthop Trauma Surg. 2006;126:624–630. doi: 10.1007/s00402-005-0078-1. [DOI] [PubMed] [Google Scholar]
- 6.Saiki K, Hirabayashi S, Sakai H, Inokuchi K. Traumatic anterior lumbosacral dislocation caused by hyperextension mechanism in preexisting L5 spondylolysis a case report and a review of literature. J Spinal Disord Tech. 2006;19:455–462. doi: 10.1097/00024720-200608000-00015. [DOI] [PubMed] [Google Scholar]
- 7.Tsirikos AI, Saifuddin A, Noordeen MH, Tucker SK. Traumatic lumbosacral dislocation. Spine. 2004;29:e164–e168. doi: 10.1097/00007632-200404150-00026. [DOI] [PubMed] [Google Scholar]
- 8.Watson-Jones R. Fractures and joint injuries. 1st edn. Baltimore: Williams & Wilkins; 1940. p. 641. [Google Scholar]
- 9.Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop. 1976;117:23–29. [PubMed] [Google Scholar]