Abstract
Symptomatic spinal epidural lipomatosis (SEL) is very rare and frequently associated to chronic exogenous steroid use, obesity and Cushing syndrome. The idiopathic cases where no identifiable association with SEL are found constitute only 17% of all cases. The usual clinical manifestations of this entity consist of dorsal or lumbar pain with paresthesias and weakness in lower limbs, but acute symptoms of myelopathy are exceptional. We report a case of acute paraparesis and urinary retention caused by thoracic SEL in a 55-year-old male who did not have any recognized predisposing factor for this condition. Urgent surgical decompression was performed in order to relieve the symptoms. Slow but progressive improvement was assessed after surgery. We consider this case to be exceptional due to the needing to perform an urgent decompressive laminectomy to treat a rapidly progressive myelopathy caused by idiopathic SEL.
Keywords: Epidural lipomatosis, Paraparesis, Spinal cord compression, Surgical decompression, Myelopathy
Introduction
Spinal epidural lipomatosis (SEL) consists of the overgrowth of epidural adipose tissue in the spinal canal causing spinal cord or nerve root compression. Symptomatic SEL is very rare and most frequently associated with exogenous steroid use. Obesity and Cushing syndrome can also be associated. The idiopathic cases in which no identifiable association with SEL is found constitute only 17% of all cases [4]. The usual clinical manifestations are chronic dorsal or lumbar pain with progressive paresthesia and weakness in the lower limbs. Acute neurological symptoms are uncommon. We report a rare case of acute sphincter dysfunction and paraparesis caused by thoracic SEL in a patient who did not have any recognized predisposing factor for this condition.
Materials and methods
A 55-year-old man presented with a 24-h history of progressive weakness of both lower limbs and urinary retention for 48 h. A urinary catheter was inserted in another hospital more than 24 h before admission. He had a past medical history of arterial hypertension treated with an angiotensin-converting enzyme inhibitor. Neurological examination revealed a 2/5 paraparesis with hyperactive deep tendon reflexes and bilateral extensor plantar responses. There was a sensory loss at and below T7 level and his body mass index was within normal limits.
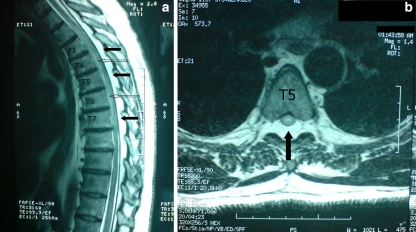
A whole spine magnetic resonance imaging was performed urgently and revealed an increased epidural fat tissue posterior to the spinal cord causing cord compression from T3 to T7 as well as a linear centromedullary cord area of high signal (in T2 weighted sequence) at the levels of compression (Fig. 1). The cerebrospinal fluid after lumbar puncture was normal.
Fig. 1.
Sagittal (a) and axial (b) T2-weighted MRI showing a hyperintense lesion, consistent with fat in the posterior aspect of the spinal canal (solid arrows) causing cord compression from T3 to T7 as well as a linear centromedullary cord area of high signal (open arrows) at the levels of compression
An urgent laminectomy was performed from T4 to T6 (the segment of maximum cord compression). Intraoperatively, the dura was found to be compressed by excessive adipose tissue that was removed. The histopathological examination confirmed normal adipose tissue.
Results
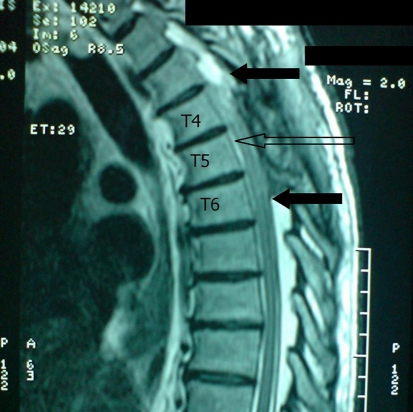
After surgery (Fig. 2), the patient received treatment with corticosteroids and bed rest for some days and was transferred to the spinal rehabilitation unit for further management. Slow but progressive improvement was assessed after surgery. The patient’s motor strength and tactile sensation returned to normal 7 weeks after surgery but sphincter disturbances and a mild deficit in thermoalgesic sensitivity were still present.
Fig. 2.
Postoperative sagittal T2-weighted MR. It shows the decompressive laminectomy (between solid arrows) and a high signal corresponding to the anterior subarachnoid space (open arrows)
Discussion
The excessive adipose tissue in SEL is typically found posterior to the cord and MR imaging is the procedure of choice for the diagnosis [6]. Quint et al. [10] measured MR images in six patients suffering from SEL and found a mean sagittal epidural fat thickness of 8 mm. In 28 normal control patients, the mean sagittal epidural fat thickness was 4.6 mm. Borre et al. [3] studied lumbosacral SEL and developed an MRI classification according to the percentage of the canal occupied by the adipose tissue: grade 0, <40%; grade I, <50%; grade II, 50–70%; grade III, >75%.
Spinal epidural lipomatosis is more frequent in men [11] and it is associated with exogenous steroid use in 55.3%. Obesity is the second-most common associated category with 24.5% and Cushing syndrome have been reported associated with SEL in 3.2% [4, 9]. Finally, the idiopathic cases where no identifiable association with SEL is found constitute 17% of all cases [4]. SEL is found in approximately the same number of cases in both the thoracic and the lumbosacral regions [4, 9].
The usual clinical manifestations consist of dorsal or lumbar pain with paresthesia and weakness in the lower limbs [1, 5, 10]. They could mimic the symptoms of a herniated disc or spinal stenosis. Weakness is the only symptom in 20% of SEL cases [9]. To our knowledge, few cases of SEL presented with acute sphincter dysfunction and paraparesis [7, 8].
The treatment of SEL depends on the severity of the symptoms, the evolution time and the cause suspected. It ranges from conservative management to surgical excision consisting of laminectomy and fat debulking. Surgical treatment is used in patients with severe and rapidly progressive symptoms. The success rate of surgical treatment in patients with SEL associated to exogenous steroids use is 77% [4, 9]. The medical treatment consisting on weight loss, steroid taper, analgesics, bed rest and observation also gets in this group of patients a success rate of 77% [4]. In the group of patients presenting SEL associated to obesity, the success rate of surgical treatment is 66.7 and 81.8% for medical treatment by weight loss [4]. Laminectomy is the treatment of choice for patients with idiopathic SEL with a success rate of 93.75% [4].
In the case we describe, it is very remarkable the rapidity of appearance of symptoms and the absence of associated factors such as obesity, exogenous steroid use or Cushing disease. Relationship between SEL diagnosed in this patient and clinical symptoms is clear: the level of sensory loss is concordant with the level of spinal cord compression and the extension of the presurgical linear centromedullary cord area of high signal fits to the levels of spinal cord compression and no vascular malformation or ischemic process was detected in MRI. A concomitant idiopathic transverse myelitis could, however, be possible in this patient but lumbar puncture did not demonstrate elevated protein or pleocytosis (cerebrospinal fluid analysis is normal in 38% of lumbar punctures in patients with idiopathic transverse myelitis [2]).
The severity of symptoms as well as the rapidly progressive myelopathy and the absence of other well-documented pathologies made us perform an urgent decompressive laminectomy and fat debulking. The patient’s recovery was slow and probably also associated with adjuvant medical treatment consisting of bed rest and steroids for some days.
To date, to the authors’ knowledge, there is no similar case published in which an urgent decompressive laminectomy had to be performed to treat a rapidly progressive myelopathy caused by idiopathic SEL.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Arroyo IL, Barron KS, Brewer EJ. Spinal cord compression by epidural lipomatosis simulating an acute herniated nucleus pulposus. J Neurosurg. 1982;57:559–562. doi: 10.3171/jns.1982.57.4.0559. [DOI] [PubMed] [Google Scholar]
- 2.Berman M, Feldman S, Alter M, Zilber N, Kahana E. Acute transverse myelitis: incidence and etiologic considerations. Neurology. 1981;31:966–971. doi: 10.1212/wnl.31.8.966. [DOI] [PubMed] [Google Scholar]
- 3.Borre DG, Borre GE, Aude F, Palmieri GN. Lumbosacral epidural lipomatosis: MRI grading. Eur Radiol. 2003;13:1709–1721. doi: 10.1007/s00330-002-1716-4. [DOI] [PubMed] [Google Scholar]
- 4.Fogel GR, Cunningham PY, Esses SI. Spinal epidural lipomatosis: case reports, literature review and meta-analysis. Spine J. 2005;5:202–211. doi: 10.1016/j.spinee.2004.05.252. [DOI] [PubMed] [Google Scholar]
- 5.George WE, Wilmot M, Greenhouse A, Hammeke M. Medical management of steroid-induced epidural lipomatosis. New Engl J Med. 1983;308:316–319. doi: 10.1056/NEJM198302103080605. [DOI] [PubMed] [Google Scholar]
- 6.Ishikawa Y, Shimada Y, Miyakoshi M N, Suzuki T, Hongo M, Kasukawa Y, Okada K, Itoi E. Decompression of idiopathic lumbar epidural lipomatosis: diagnostic magnetic resonance imaging evaluation and review of the literature. J Neurosurg Spine. 2006;4:24–30. doi: 10.3171/spi.2006.4.1.24. [DOI] [PubMed] [Google Scholar]
- 7.Jungreis CA, Cohen WA. Spinal cord compression induced by steroid therapy: CT findings. J Comput Assist Tomogr. 1987;11:245–247. doi: 10.1097/00004728-198703000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Kaplan JG, Barasch E, Hirschfeld A, Ross L, Einberg K, Gordon M. Spinal epidural lipomatosis: a serious complication on iatrogenic Cushing’s syndrome. Neurology. 1989;39:1031–1034. doi: 10.1212/wnl.39.8.1031. [DOI] [PubMed] [Google Scholar]
- 9.Porras-Estrada LF, Díaz-Pérez de Madrid J, Cabezudo-Artero JM, Lorenzana-Honrado L, Rodríguez-Sánchez JA, Ugarriza-Echebarrieta F. Spinal extradural lipomatosis. Revision of 108 cases. Case induced by exogenous contribution of ACTH. Neurocirugia. 2002;13:463–471. [PubMed] [Google Scholar]
- 10.Quint DJ, Boulos RS, Sanders WP, Mehta BA, Patel SC, Tiel RL. Epidural lipomatosis. Radiology. 1998;169:485–490. doi: 10.1148/radiology.169.2.3174998. [DOI] [PubMed] [Google Scholar]
- 11.Robertson SC, Traynelis VC, Foller KA, Menezes AH. Idiopathic spinal epidural lipomatosis. Neurosurgery. 1997;41:68–75. doi: 10.1097/00006123-199707000-00015. [DOI] [PubMed] [Google Scholar]