Abstract
Spinal epidural angiolipoma is a rare benign tumor containing vascular and mature adipose elements. A slow progressive clinical course was mostly presented and rarely a fluctuating course during pregnancy. The authors report the original case of spontaneous spinal epidural bleeding resulting from thoracic epidural angiolipoma who presented with hyperacute onset of paraplegia, simulating an extradural hematoma. The patient was admitted with sudden non-traumatic hyperacute paraplegia during a prolonged walk. Neurologic examination showed sensory loss below T6 and bladder disturbances. Spinal MRI revealed a non-enhanced heterogeneous thoracic epidural lesion, extending from T2 to T3. A bilateral T2–T4 laminectomy was performed to achieve resection of a lipomatous tumor containing area of spontaneous hemorrhage. The postoperative course was uneventful with complete neurologic recovery. Histologic examination revealed the tumor as an angiolipoma. Because the prognosis after rapid surgical management of this lesion is favorable, the diagnosis of spinal angiolipoma with bleeding should be considered in the differential diagnosis of hyperacute spinal cord compression.
Keywords: Angiolipoma, Epidural spinal tumor, Spinal cord compression, Spinal epidural hematoma
Introduction
Spinal epidural angiolipomas (SEA) are benign tumors containing mature adipose elements admixed with abnormal blood vessels [6, 8]. About a hundred cases were previously reported [1, 5, 7]. They generally produce a slow progressive spinal cord or radicular compression [1]. Acute myelopathy is exceedingly rare [2, 5]. To our knowledge, we present the first case of an intraspinal bleeding from an epidural angiolipoma producing hyperacute paraplegia and simulating an extradural hematoma.
Case Report
This 47-year-old-man, during a prolonged walk developed sudden back pain rapidly followed by paresthesia and complete neurologic palsy within a few-minutes period. He had no history of trauma or anticoagulation therapy. At admission, the patient was alert but unable to maintain the upright position; he had only mild dorsal–ventral flexion of the right foot. The deep tendon reflexes were absent and Babinski responses were negative. Sensory impairment was noted below the T6 level with urinary retention. Spinal MRI revealed a posterior epidural mass at T2–T3 level. The spinal cord was compressed and displaced anteriorly. The lower part of the mass showed a globular lesion that was isointense on T1–WI and slightly hyperintense on T2–WI. However, the upper part of the mass was isointense on T1–WI and hyperintense on T2–WI (Fig. 1). There was no gadolinium enhancement. A spinal epidural hematoma was suspected.
Fig. 1.
Spinal sagittal MRI using T1–WI (a) and T2–WI (b). The lower part of the mass was isointense on T1–WI and slightly hyperintense on T2–WI. The upper part of the mass was isointense on T1–WI and hyperintense on T2–WI
After a bilateral laminectomy from T2 to T4, we found a compressive hemorrhagic epidural lesion that present two portions: (1) In the lower part, a well circumscribed, globular soft mass, measuring about 20 × 12 × 8 mm in size. Numerous vessels that easily bled were adherent around the tumor; (2) At the superior pole of the tumor, we found an epidural hematoma measuring 10 mm in diameter. Both the hematoma and the tumor were easily removed completely without neurophysiological monitoring. At histopathologic examination, the tumor was diagnosed as angiolipoma (Fig. 2).
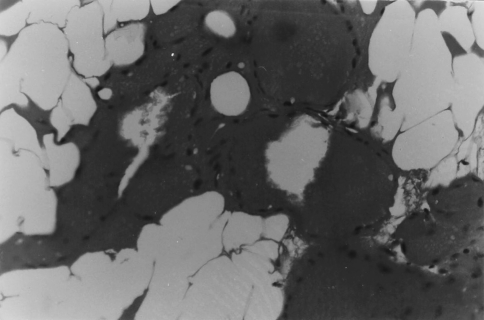
Fig. 2.
Histopathology. Typical features of angiolipoma. (hematoxylin and eosin, original magnification×250)
The postoperative course was uneventful, with rapid complete neurologic recovery. The patient was returned to his job, and has been well for more than 2 years of follow-up evaluation.
Discussion
SEA usually produce a progressive spinal cord or nerve root compression over many months, however, some cases may be present with remitting and relapsing course [1, 6, 8]. More rarely a subacute presentation related to venous thrombosis within the tumor SEA may be present[3].
Miscellaneous factors can contribute to the accelerated onset of symptoms. Such as rapid expansion of the tumoral volume caused by enlarging or degenerating blood vessels, or from hemorrhage within the lesion [6]. Von Hanwehr have speculated that the tumor can exert a local vasculature “steal” phenomenon that reduces blood supply and perfusion of neighboring neural tissue [8]. Other factors such as pregnancy, with blood volume and extracellular fluid volume changes, and alterations in fat mobilization patterns also may cause an increase in tumor mass. Finally, indirect compression of the anterior radiculomedullary artery can be responsible for neurological symptoms. Recently, Petrella reported a case with acute spontaneous intratumoral abscess [5].
In contrast to the previous descriptions, we believe that vigorous exercise in our patient contributed to augment blood flow size in the tumor to produce epidural bleeding, which in turn exerted a rapid compressive effect on the spinal cord. Although the exact source of blood has never been clear, an arterial source of clot seems to be more probable than venous because of the rapid onset and progression of symptoms. Only one case is remotely similar to that of our patient. In that an extradural clot was reported with an angiolipoma 48 h after the onset of an acute paraplegia [2].
Most MRI features of SEA have shown the tumor to be iso-hyperintense on T1–WI and usually inhomogeneous high-signal intensity on T2–WI [1, 3, 7]. However, differential diagnosis must include some epidural tumors and spinal epidural hematomas especially in the acute presentation [4]. Heterogeneous hyperintensity to spinal cord with focal hypointensity on T2–WI should suggest the diagnosis of acute/hyperacute spinal epidural hematoma [4]. The posterior localization of the tumor to spinal cord facilitates removal through a bilateral laminectomy [1]. The prognosis depends not only on the degree of neurologic loss at surgery but also on the time from symptom onset to surgical decompression [7].
Conclusions
Spinal epidural angiolipoma is an unusual benign tumor which generally produces a slow progressive spinal cord or radicular compression. Presentation may be atypical but MRI is usually diagnostic. Because the prognosis after rapid surgical management of this lesion is favourable, the diagnosis of spinal angiolipoma with bleeding should be considered in the differential diagnosis of hyperacute spinal cord compression.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Akhaddar A, Gazzaz M, Derraz S, Rifi L, Amarti A, Aghzadi A, et al. Spinal epidural angiolipomas: a rare case of spinal cord compression. A report of eight cases and review of the literature. Neurochirurgie. 2000;46:523–533. [PubMed] [Google Scholar]
- 2.Anson JA, Cybulsky GR, Reyes M. Spinal extradural angiolipoma: a report of two cases and review of the literature. Surg Neurol. 1990;34:173–178. doi: 10.1016/0090-3019(90)90069-2. [DOI] [PubMed] [Google Scholar]
- 3.Boockvar JA, Black K, Malik S, Stanek A, Tracey KJ. Subacute paraparesis induced by venous thrombosis of a spinal angiolipoma. Spine. 1997;22:2304–2308. doi: 10.1097/00007632-199710010-00022. [DOI] [PubMed] [Google Scholar]
- 4.Fukui MB, Swarnkar AS, Williams RL. Acute spontaneous spinal epidural hematomas. Am J Neuroradiol. 1999;20:1365–1372. [PMC free article] [PubMed] [Google Scholar]
- 5.Petrella G, Tamurrini G, Lauriola L, Di Rocco C. Spinal epidural angiolipoma complicated by an intratumoral abscess. J Neurosurg. 2005;103:166–169. doi: 10.3171/ped.2005.103.2.0166. [DOI] [PubMed] [Google Scholar]
- 6.Preul MC, Leblanc R, Tampieri D, Robitaille Y, Pokrupa R. Spinal angiolipomas. Report of three cases. J Neurosurg. 1993;78:280–286. doi: 10.3171/jns.1993.78.2.0280. [DOI] [PubMed] [Google Scholar]
- 7.Samdani AF, Garonzik IM, Jallo G, Eberhart CG, Zahos P. Spinal angiolipoma: case report and review of the literature. Acta Neurochir (Wien) 2004;146:299–302. doi: 10.1007/s00701-003-0196-x. [DOI] [PubMed] [Google Scholar]
- 8.Hanwehr R, Apuzzo MLJ, Ahmadi J, Chandrasoma P. Thoracic spinal angiolipoma: case report and literature review. Neurosurgery. 1985;16:406–411. doi: 10.1097/00006123-198503000-00023. [DOI] [PubMed] [Google Scholar]