Abstract
We present two cases in which the diagnosis was complicated by the presence of a weak muscle innervated by a compressed motor root in the intervertebral foramen (IVF) at an atypical level. The patients were 59- and 53-year-old men; they presented with marked atrophy and weakness predominantly in a unilateral deltoid. Neuroimaging revealed narrowing of the nerve root sleeve at the C5/6 IVF due to a herniated disk or osteophyte. Predominant atrophy and weakness of the deltoid were not consistent with radiculopathy at the C5/6 IVF, i.e. C6 radiculopathy. During an extended observation period to rule out motor neuron disease, their weakness did not spread and the patients underwent posterior medial facetectomy and anterior foraminotomy. This produced marked improvement of the deltoid weakness soon after the operation. We considered unexpectedly wide motor innervation of the C6 nerve root predominantly in the deltoid, anatomic variations in the C5 root such as the trunk of the C5 root entering into the C5/6 IVF, and descending anastomoses connecting the C5 and C6 rootlets as possible explanations. Awareness of this rare presentation may aid in the diagnosis and surgical management of these patients.
Keywords: Deltoid, Diagnosis, Innervation, Radiculopathy
Introduction
Decompression surgery for vertebral degenerative disorders is indicated when neurological findings of radiculopathy and/or myelopathy are consistent with the location of the lesion on neuroimages, and after motor neuron disease (MND) has been ruled out in patients with pure motor palsy [1, 2, 7, 13, 17]. However, in some cases the surgical indication is occult due to inconsistent findings.
We present two cases in which a segmental diagnosis was complicated by the sole presence of an atrophied deltoid innervated by a compressed motor root and/or rootlets at the C5/6 intervertebral foramen (IVF), a rare and atypical causative level [4, 14].
Case reports
Case 1
This 59-year-old man with a history of paroxysmal supraventricular tachycardia noticed difficulties when moving his right arm to wash his hair or write on a blackboard. The difficulties worsened over the next year and he was referred to our institute.
Neurological examination disclosed marked atrophy in the right deltoid (Fig. 1a) with sparing of the bulk of the ipsilateral biceps and brachioradialis. No fasciculation was observed. Manual muscle tests revealed 2/5 in the deltoid, 3/5 in the biceps and brachioradialis, 5/5 in the triceps, and 5/5 in the wrist and finger muscles. Deep tendon reflexes were diminished in the right biceps, brachioradialis, and triceps without pathological reflexes. His gait was normal and no sensory disturbances were detected. Electromyography revealed neurogenic patterns in the deltoid and biceps on the right side. Magnetic resonance imaging (MRI) showed slight cord compression at the C5/6 and C6/7 intervertebral space; there was no cord compression or intramedullary abnormality at C3/4 and C4/5, the levels of the anterior horn of the C5- and C6 root. Narrowing of the right root sleeve by a herniated disk was suspected at C5/6 (Fig. 1b). Indeed, computed tomography myelography (CTM) confirmed narrowing of the right root sleeve at the C5/6 IVF by a herniated disk (Fig. 1c). Among these radiological findings, right root sleeve compression at the C5/6 IVF was the most prominent, however, it did not coincide with isolated atrophy of the deltoid. Because we could not rule out early-stage MND and due to his poor cardiac function, spinal decompression surgery was contra-indicated. During an observation period of 3 years, his symptoms remained stable and the weakness did not spread. After informing the patient that the effectiveness of root decompression at the C5/6 IVF might be minimal, he underwent right posterior medial facetectomy at the C5/6 level (Fig. 1d). His symptoms were markedly improved on the morning following surgery and he was able to use his right arm as a pillow for his head. At 1 year after the operation, he had recovered right arm abduction and elevation; on manual muscle testing the result was 4/5.
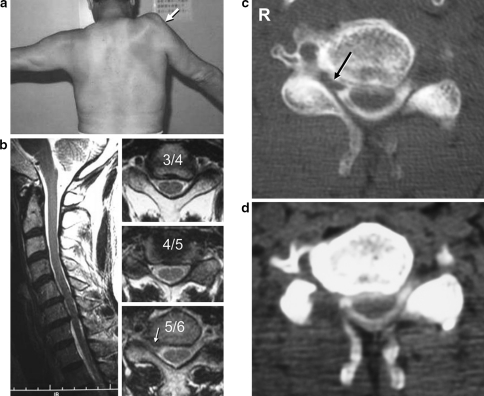
Fig. 1.
a Photograph showing marked atrophy of the right deltoid (arrow) and incomplete abduction of the right arm. b Magnetic resonance image showing slight ventral and dorsal compression of the cord at the C5/6 and C6/7 intervertebral space. There is no cord compression or intramedullary abnormality at C3/4 and C4/5. Narrowing of the right root sleeve by a herniated disk is suspected at C5/6 (arrow). c Pre- and d post-operative computed tomography myelogram at the C5/6 level. Narrowing of the right root sleeve by a herniated disk (arrow) was relieved by medial facetectomy
Electromyography and motor nerve conduction studies performed 2 years after the operation yielded evidence of an ongoing recovery process in the deltoid. This was confirmed by the appearance of a few normal units and marked improvement in the amplitude from a preoperative value of 0.7–10.9 mV.
Case 2
This 53-year-old man with no relevant medical history began noticing difficulties upon raising his left arm that progressed during the next 6 months and he was referred to our institute.
Neurological examination showed marked atrophy in the left deltoid with sparing of the ipsilateral bulk of the biceps and brachioradialis. No fasciculation was observed. Manual muscle testing revealed 2/5 in the deltoid, 3/5 in the biceps and brachioradialis, 5/5 in the triceps, and 5/5 in the wrist and finger muscles. Deep tendon reflexes were diminished in the left biceps and brachioradialis without pathological reflexes. His gait was normal and no sensory disturbances were observed. MRI showed bulging of the intervertebral disks at C4/5, C5/6, and C6/7. There was no evidence of cord compression or intramedullary abnormality at C3/4 and C4/5, the levels of the anterior horn of the C5- and C6 root. Suspected narrowing of the left root sleeve by a herniated disk at C5/6 (Fig. 2a) was confirmed by CTM that showed narrowing of the left root sleeve at the C5/6 IVF by an osteophyte and herniated disk (Fig. 2b).
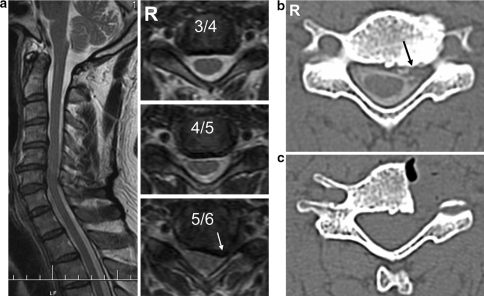
Fig. 2.
a Magnetic resonance image showing bulging of the intervertebral disk at C4/5, C5/6, and C6/7. There is no cord compression or intramedullary abnormality at C3/4 and C4/5. Narrowing of the left root sleeve by a herniated disk is suspected at C5/6 (arrow). b Pre- and c postoperative computed tomography myelogram at the C5/6 level. Narrowing of the left root sleeve by an osteophyte and herniated disk (arrow) was relieved by anterior foraminotomy
Although spinal root compression at the C5/6 IVF did not coincide with isolated atrophy of the deltoid, based on our experience with Case 1 we considered decompression surgery to be indicated. He underwent left anterior foraminotomy at C5/6 6 months post-onset (Fig. 2c) and his symptoms improved gradually. At 8 months after the operation he had fairly recovered left arm abduction and elevation; at manual muscle testing he scored 4/5.
Discussion
Diagnostic indices in our patients were a weakened deltoid predominantly innervated by a compressed nerve root at the C5/6 IVF. This was confirmed by our operative and electrophysiological results. Although the deltoid can be weakened by anterior horn impingement [14], the absence of cord compression or intramedullary abnormalities at C3/4 and C4/5, the levels of the anterior horn of the C5- and C6 root, precluded this pathology.
As the predominant innervation of each muscle in the shoulder and upper extremity is known, muscles with severe weakness suggest an affected nerve root. For example, if weakness is more severe in the deltoid than the biceps, this suggests disturbance of the C5 nerve root. Greater weakness of the biceps than the deltoid, on the other hand, is suggestive of C6 nerve root disturbance [3, 18]. Electrophysiological findings during neurotization of the brachial plexus support this anatomical rule. The evoked muscle amplitude potential in each muscle obtained by electric stimulation of nerve roots from C5 to T1 confirmed that the predominant innervating roots of the deltoid and biceps were the C5 and C6 nerve roots, respectively [5].
Our patients presented with more severe atrophy of the deltoid than biceps. We considered these findings incompatible with the typical presentation of nerve root compression at the C5/6 IVF as the C6 nerve root passes the C5/6 IVF. According to Shinomiya et al. [14], neuroradiologic and intraoperative electrophysiologic study of cervical spondylotic amyotrophy of the deltoid showed that radiculopathy at the C5/6 IVF, i.e. compression of the C6 nerve root as the sole lesion, is a rare causative lesion (20%) [14]. Another clinical study of monoradicular symptoms revealed no weakness of the deltoid in patients with C6 radiculopathy; weakness of the muscle, on the other hand, was associated with C5 radiculopathy [3].
The MND may initially present with focal weakness involving a single muscle group; this is also suggestive of radiculopathy. In addition, as no specific diagnostic procedure confirms or excludes the possibility of MND [1, 2, 15] and radiological studies commonly depict spinal degenerative disease in asymptomatic individuals older than 50 years, an age that coincides with the onset of MND [6, 11, 16], spinal decompression surgery for vertebral degenerative disease is sometimes erroneously performed in patients who are later diagnosed with MND [1, 2, 13, 17]. These considerations led us to postpone surgery and to place the patients under prolonged observation to rule out MND. As their muscle weakness failed to spread, and based on favorable outcomes obtained with decompression surgery in patients with deltoid paralysis due to radiculopathy at C5/6 [4, 14], we proceeded to perform decompression of the affected nerve root at the C5/6 IVF.
We considered unexpectedly wide motor innervation of the C6 nerve root predominantly in the deltoid, and anatomic variations of the C5 root to explain the atypical clinical manifestations in our patients. A possible anatomic variation, in which a narrow C5/6 IVF affects the C5 root, is entry of the trunk of the C5 root into the C5/6 IVF. This variation has been reported in a different segment, i.e. the C6 root entering into the C6/7 IVF [12]. Alternatively, there may be intradural prominent descending anastomoses connecting the C5 and C6 rootlets (Fig. 3). Adjacent ventral spinal rootlets may be interconnected by several types of anastomoses [10], i.e. a fiber from the lowermost rootlet uniting with the peripheral portion of the uppermost rootlet of the next lower segment, a fiber from the central portion of the uppermost rootlet connecting with the peripheral region of the lowermost rootlet of the nearest upper segment, a fiber between ventral roots exiting the cord at a point where the segmental border bifurcates and joins each rootlet of the upper and lower segments, and a fiber that interconnects neighboring rootlets and courses parallel to the cord. No anastomosis extends more than one level above or below. Among anastomoses in the ventral rootlets, those between C5 and C6 (the sites of interest in the present study) are the most frequent; they range from 9.3 to 81.3% [8–10]. In our patients, neither variation was documented on neuroimaging studies or at surgery and it remains unclear why isolated atrophy of the deltoid was caused in both cases by a compressed motor root and/or rootlets at the C5/6 IVF.
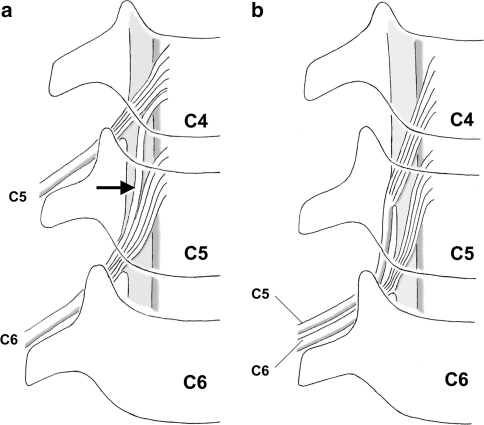
Fig. 3.
Diagram proposing anatomical features that may result in C5 nerve root radiculopathy originating at the C5/6 IVF. Note the prominent descending anastomosis connecting the C5 and C6 rootlets (arrow) that contain the main fiber of the C5 root (a), and the trunk of the C5 root entering the C5/6 IVF without entering the normal course of the C4/5 IVF (b)
In conclusion, awareness of the rare presentations we encountered may make it possible to reach a correct diagnosis early and may facilitate treatment planning. In the future, higher-resonance neuroimaging studies may depict the anatomic reason underlying this phenomenon.
Conflict of Interest
None of the authors has any potential conflict of interest.
References
- 1.Belsh JM, Schiffman PL. Misdiagnosis in patients with amyotrophic lateral sclerosis. Arch Intern Med. 1990;150:2301–2305. doi: 10.1001/archinte.150.11.2301. [DOI] [PubMed] [Google Scholar]
- 2.Belsh JM, Schiffman PL. The amyotrophic lateral sclerosis (ALS) patient. Perspective on misdiagnosis and its repercussions. J Neurol Sci. 1996;139(Suppl):110–116. doi: 10.1016/0022-510X(96)00088-3. [DOI] [PubMed] [Google Scholar]
- 3.Benini A. Clinical features of cervical root compression C5–C8 and their variations. Neuro Orthop. 1987;4:74–88. [Google Scholar]
- 4.Chang H, Park JB, Hwang JY, et al. Clinical analysis of cervical radiculopathy causing deltoid paralysis. Eur Spine J. 2003;12:517–521. doi: 10.1007/s00586-003-0541-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gu YD. Functional motor innervation of brachial plexus roots. An intraoperative electrophysiological study. J Hand Surg (Br) 1997;22:258–260. doi: 10.1016/s0266-7681(97)80076-9. [DOI] [PubMed] [Google Scholar]
- 6.Haverkamp LJ, Appel SH, Appel V. Natural history of ALS in a database population: validation of a scoring system and a model for survival prediction. Brain. 1995;118:707–719. doi: 10.1093/brain/118.3.707. [DOI] [PubMed] [Google Scholar]
- 7.Keegan JJ. The cause of dissociated motor loss in the upper extremity with cervical spondylosis. J Neurosurg. 1965;23:528–536. doi: 10.3171/jns.1965.23.5.0528. [DOI] [PubMed] [Google Scholar]
- 8.Kubo Y, Waga S, Kojima T, et al. Microsurgical anatomy of the lower cervical spine and cord. Neurosurgery. 1994;34:895–902. doi: 10.1097/00006123-199405000-00017. [DOI] [PubMed] [Google Scholar]
- 9.Marzo JM, Simmons EH, Kallen F. Intradural connections between adjacent cervical spinal roots. Spine. 1987;12:964–968. doi: 10.1097/00007632-198712000-00002. [DOI] [PubMed] [Google Scholar]
- 10.Moriishi J, Otani K, Tanaka K, et al. The intersegmental anastomoses between spinal nerve roots. Anat Rec. 1989;224:110–116. doi: 10.1002/ar.1092240114. [DOI] [PubMed] [Google Scholar]
- 11.Penning L, Wilmink JT, Woerden HH, et al. CT myelographic findings in degenerative disorders of the cervical spine: Clinical significance. AJR Am J Roentgenol. 1986;146:793–801. doi: 10.2214/ajr.146.4.793. [DOI] [PubMed] [Google Scholar]
- 12.Rosner MJ, Whaley R. Anomalous exit of the C-6 nerve root via the C-6, C-7 foramen. Neurosurgery. 1984;14:740–743. doi: 10.1097/00006123-198406000-00017. [DOI] [PubMed] [Google Scholar]
- 13.Rowland LP. Diagnosis of amyotrophic lateral sclerosis. J Neurol Sci. 1998;160(Suppl 1):S6–S24. doi: 10.1016/S0022-510X(98)00193-2. [DOI] [PubMed] [Google Scholar]
- 14.Shinomiya K, Komori H, Matsuoka T, et al. Neuroradiologic and electrophysiologic assessment of cervical spondylotic amyotrophy. Spine. 1994;19:21–25. doi: 10.1097/00007632-199401000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Swash M. The diagnosis of amyotrophic lateral sclerosis. A discussion. Adv Neurol. 1995;68:157–160. [PubMed] [Google Scholar]
- 16.Teresi LM, Lufkin RB, Reicher MA, et al. Asymptomatic degenerative disk disease and spondylosis of the cervical spine: MR imaging. Radiology. 1987;164:83–88. doi: 10.1148/radiology.164.1.3588931. [DOI] [PubMed] [Google Scholar]
- 17.Yoshor D, Klugh A, III, Appel SH, et al. Incidence and characteristics of spinal decompression surgery after the onset of symptoms of amyotrophic lateral sclerosis. Neurosurgery. 2005;57:984–989. doi: 10.1227/01.NEU.0000180028.64385.d3. [DOI] [PubMed] [Google Scholar]
- 18.Yoss RE, Corbin KB, MacCarty CS, et al. Significance of symptoms and signs in localization of involved root in cervical disk protrusion. Neurology. 1957;7:673–683. doi: 10.1212/wnl.7.10.673. [DOI] [PubMed] [Google Scholar]