Abstract
The authors report on a 14 years old female with intracranial hypotension who had a history of spinal instrumentation surgery for scoliosis 3 months prior to her admission. She had been diagnosed with migraine in a neurology clinic and was under medical therapy when presented. During the investigation process, a right thoracic pedicle screw, which was penetrating and transversing the dura mater at the T3–T4 level was identified. The diagnosis and management of such a case is discussed. Knowledge of this entity is of extreme importance to spine surgeons, in order to prevent delayed diagnosis and possible complications.
Keywords: Intracranial hypotension, Cerebrospinal fluid leak, Scoliosis surgery, Computerized tomography myelography, Radionuclide cisternography
Introduction
Intracranial hypotension (IH) secondary to cerebrospinal fluid (CSF) leakage is an increasingly recognized problem, characterized by orthostatic headaches, typically aggravated in the erect position and ameliorated by lying down. Other symptoms such as nausea, vomiting, tinnitus, vertigo and cranial nerve palsies may also be encountered during the clinical course [5]. IH may occur spontaneously or after a variety of interventions such as lumbar puncture, chiropractic manipulation or spinal surgery [3, 6]. There are limited numbers of reported IH cases following spinal surgery, which are mostly encountered after simple cervical or lumbar discectomies or surgery for degenerative spine [3]. We aim to report and discuss the management of a patient with symptomatic IH, resulting from a dorsal dural tear occurring after the medial penetration of a thoracic pedicle screw during scoliosis surgery.
Case report
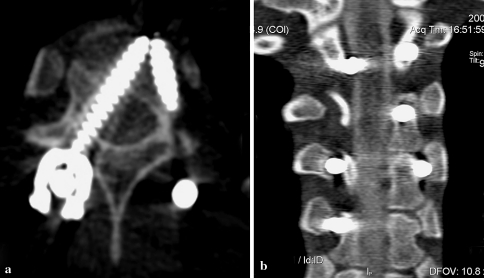
A 14-year-old female was referred to our clinic with a history of severe postural headache and vertigo starting in the morning and exacerbated in the afternoon, while relieved in the supine position. Her neurological examination was unremarkable. She had a history of posterior spinal instrumentation for scoliosis 3 months ago. She admitted that her symptoms started after she was discharged from the hospital on the postoperative 5th day. With these symptoms and additional tinnitus, she was diagnosed as having migraine by a neurologist and analgesic treatment was given, which did not relieve her symptoms. We initially performed a cranial magnetic resonance imaging (MRI) with and without gadolinium injection, which revealed nothing abnormal including pachymeningeal enhancement (Fig. 1). Due to the presence of a spinal instrumentation history and classical symptoms of IH, we performed a CT myelography, which demonstrated that the right pedicle screw at the same level has been penetrating and transversing the dura and embedding into the vertebral column (Fig. 2a, b). However, the point of leakage could not be visualized due to artefact. The opening pressure of the CSF was recorded as 3 cm H20. We further performed a radionucleoid cisternography (RC), which revealed the leakage of the radionucleoid material into the paravertebral area at the level of T3–T4 (Fig. 3a). She was then operated on and the right screw at the level of T3–T4 was repositioned. After partial laminectomy, the dural tear was closed with patches of allograft dura (Tutoplast®), reinforced with extradural application of a synthetic dural sealant (Duraseal®). The operation was terminated after the application of a lumbar drainage catheter. Postoperatively, there was significant improvement in clinical symptoms especially after the postoperative 2nd day. She was immobilized until day 4 and discharged from the hospital on the postoperative 8th day. The control RC at the postoperative 18th day revealed no leakage (Fig. 3b). The patient is on regular follow-up and on the 9th month of control she had no symptoms.
Fig. 1.
Axial T1-weighted cranial MR image with gadolinium injection shows no abnormality
Fig. 2.
Postcontrast axial (a) and coronal (b) CT and myelography scans reveal a right pedicle screw transversing and penetrating the dura mater at the T3–T4 level. However, the exact point of leakage cannot be demonstrated due to metal artefact
Fig. 3.
Preoperative RC (a) shows radionucleoid leakage to the paravertebral area at the T3–4 level. b RC study 18 days after the operation demonstrates no leakage
Discussion
Pedicle screw placement in the thoracic spine in scoliosis surgery requires meticulous caution and considerable experience in order to avoid the complications. In 4,369 scoliosis cases treated by posterior instrumentation and fusion, dural tear was reported in 8 cases (0.18%) [1]. Although rare, serious subsequent complications following dural tear such as cerebellar hemorrhage and pneumocephaly, which may be related to IH, have been reported [7]. A meticilous review by Inamasu and Guiot from 1966 to 2005 disclosed only nine IH cases with spinal pathology, of which six were after a posterior or thoracic discectomy and the remaining were after an anterior thoracic spine surgery [3].
The diagnosis of IH may not always be easy as it shares common signs and symptoms with more frequently observed conditions. For instance before being referred to our clinic, the patient was treated for migraine. Despite the improvements in diagnostic modalities, the early diagnosis still depends on the clinician’s foresight. Although it is reported that the majority of the IH cases show diffuse meningeal enhancement on cranial MRI [2], there are cases reported in which no enhancement is encountered and enhancement should not be regarded as an absolute finding of IH [6, 8]. In the present case, cranial MRI also revealed nothing abnormal, but the clinical picture and the past medical history forced us to think that this might be a secondary IH case.
Precise determination of the level of CSF leakage is crucial in planning the treatment approach. Currently diagnostic modalities such as CT myelography, MRI myelography and RC are the most commonly used methods [4, 9]. We performed CT myelography as the initial diagnostic modality, but failed to visualize the leakage point probably due to the artefact effect of rods and screws. The detection of the exact point of leakage at T3–T4 level was only possible with RC.
The treatment options for spontaneous IH such as conservative treatment with bed rest and administration of fluid and analgesics may apply to IH cases subsequent to spinal instrumentation. Although the symptoms may be improved, the relief is usually transient and a more aggressive treatment targeting the definite cause is required. For instance, surgical repositioning of the malpositioned screw and direct repair of the dural leakage point in the case described provided permanent relief of symptoms.
In conclusion, in patients with persistent postural headache after spinal surgery, IH must be ruled out and knowledge of this entity is essential to spine surgeons in order to prevent life threatening complications. Absence of dural enhancement on cranial MRI does not exclude IH diagnosis and further investigations must be carried out if the clinical symptoms and signs predominate. Due to the risk of artefact interference in other diagnostic modalities, RC can be initially performed for demonstrating the leakage site. The treatment must be directed towards the exact cause for obtaining sufficient results.
Conflict of interest statement
None of the authors has any potential conflict of interest.
References
- 1.Coe JD, Arlet V, Donaldson W, Berven S, Hanson DS, Mudiyam R, et al. Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine. 2006;31:345–349. doi: 10.1097/01.brs.0000197188.76369.13. [DOI] [PubMed] [Google Scholar]
- 2.Fishman RA, Dillon WP. Dural enhancement and cerebral displacement secondary to intracranial hypotension. Neurology. 1993;43:609–611. doi: 10.1212/wnl.43.3_part_1.609. [DOI] [PubMed] [Google Scholar]
- 3.Inamasu J, Guiot BH. Intracranial hypotension with spinal pathology. Spine J. 2006;6:591–599. doi: 10.1016/j.spinee.2005.12.026. [DOI] [PubMed] [Google Scholar]
- 4.Matsumura A, Anno I, Kimura H, Ishikawa E, Nose T. Diagnosis of spontaneous intracranial hypotension by using magnetic resonance myelography. Case report. J Neurosurg. 2000;92:873–876. doi: 10.3171/jns.2000.92.5.0873. [DOI] [PubMed] [Google Scholar]
- 5.Mokri B, Posner JB. Spontaneous intracranial hypotension: the broadening clinical and imaging spectrum of CSF leaks. Neurology. 2000;55:1771–1772. doi: 10.1212/wnl.55.12.1771. [DOI] [PubMed] [Google Scholar]
- 6.Mokri B. Low cerebrospinal fluid pressure syndromes. Neurol Clin. 2004;22:55–74. doi: 10.1016/S0733-8619(03)00089-6. [DOI] [PubMed] [Google Scholar]
- 7.Ozturk E, Kantarci M, Karaman K, Basekim CC, Kizilkaya E. Diffuse pneumocephalus associated with infratentorial and supratentorial hemorrhages as a complication of spinal surgery. Acta Radiol. 2006;47:497–500. doi: 10.1080/02841850600644766. [DOI] [PubMed] [Google Scholar]
- 8.Schievink WI, Tourje J. Intracranial hypotension without meningeal enhancement on magnetic resonance imaging: case report. J Neurosurg. 2000;92:475–477. doi: 10.3171/jns.2000.92.3.0475. [DOI] [PubMed] [Google Scholar]
- 9.Schievink WI. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. JAMA. 2006;295:2286–2296. doi: 10.1001/jama.295.19.2286. [DOI] [PubMed] [Google Scholar]