Abstract
Two cases of atlantoaxial (A-A) instability that showed different MRI findings between supine and upright positions are presented. The upright MRI represented the findings corresponding to their symptoms. In A-A lesions, conventional MR images taken in the supine position do not always explain the pathophysiological consequences. The MR images taken in the upright position disclose the actual spinal pathophysiology with gravitational effects.
Keywords: Dynamic study, Upright MRI, Atlantoaxial dislocation
Introduction
Atlantoaxial (A-A) joint has a unique structure compared with other cervical intervertebral joints. A-A joint, that lacks the intervertebral disc, has much larger range of motion and bears more weights than the other joints of cervical spine. When the anterior–posterior axis of A-A joint is parallel to the floor in upright position, the head weight forces the lateral mass of C1 to displace anteriorly in neck flexion and posteriorly in extension. This gravitational effect of head weight on C1 depending on neck position is characteristic to A-A joint. It is easily observed in X-rays taken in upright position.
In the conventional MRI taken in supine position, A-A joints are perpendicular to the floor with the head weight not loaded as in upright position. Because of lack of inclination of and physiological load on A-A joint, supine-MRI (s-MRI) does not always represent the actual dynamic pathology of the joint, even if it was taken in flexed and/or extended positions [2, 4].
Upright, weight-bearing dynamic-kinematic MRI (u-MRI) has been reported as a potential tool to enable optimal linkage of patient’s clinical symptom with the medical imaging [3, 5]. We experienced two patients who showed different MRI findings between upright and supine positions, and the u-MRI was thought to represent their pathophysiology more correctly.
MRI imaging
Imagings were acquired with a Signa Advantage 1.5-T MR system (General Electric Medical Systems, Milwaukee, WI, USA) for s-MRI. For u-MRI, patients sat on the chair in the gap of the two vertical magnet rings of SIGNA SP/i system (GE Medical Systems, Milwaukee, WI, USA). Sagittal T2 weighted images were acquired with following parameters: for s-MRI: TR 4000, TE 90, ETL 16, NEX 4, 256 × 256matrix and for u-MRI: TR 2000, TE 80, ETL 4, NEX 1, 256 × 128 matrix.
Case reports
Case 1: presentation and examination
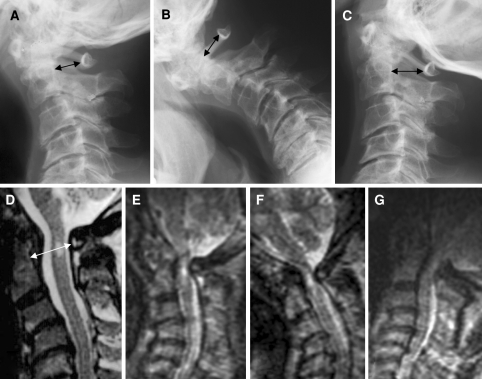
A 54-year-old man had mild torsion-neck-like involuntary movement for more than 40 years and presented with gradual worsening of bilateral upper-extremity dysesthesia and gait difficulty. He developed pain in the neck radiating down to the back on flexing the neck. Neurological examination revealed mild spastic tetraparesis and sensory disturbance in the hands and in the periphery of his face. Vibration sense was reduced in both feet. Plain X-ray films of cervical spine revealed the kyphotic changes in the lower cervical spine with compensatory extension in craniocervical junction, reducing the bony canal diameter consisted of C2 body and C1 posterior arch in neutral position (Fig. 1a). The anterior dislocation of atlas was strongest in flexed position and the bony canal was reduced as much as in neutral position (Fig. 1b). The dislocation was restored in extension and the bony canal was wider than the other neck positions (Fig. 1c). MRI in the supine position revealed the intramedullary signal change at the level of C1, but did not show any compression of the thecal sac (Fig. 1d). The s-MRI in neutral position did not show the anterior dislocation of C1 nor the compensatory extension of the upper cervical spine with reduction of the spinal canal. Then, u-MRI was taken using the vertically orientated open MRI system. Because of his mild involuntary movements, the images of dynamic u-MRI were not sharp, but clearly revealed cord compression irrespective of neck position at C1 where the intramedullary intensity change was observed in s-MRI (Fig. 1e–g).
Fig. 1.
Case 1. Dynamic cervical radiographs. In neutral position anterior dislocation of atlas is mild, but the inclination of atlas reduces the spinal canal diameter (a). The anterior dislocation is strongest in flexion (b) and restored in extension (c). Black arrows indicate the anteroposteiror diameter of the bony canal. MRI taken in supine position clearly shows a high intensity lesion in the spinal cord at C1, but does not show the dural/spinal cord compression (d, white arrow). Dynamic MRIs taken in upright position show that the spinal cord at C1 is compressed in any neck position: neutral (e), flexed (f) and extended (g) positions
Case 2: presentation and examination
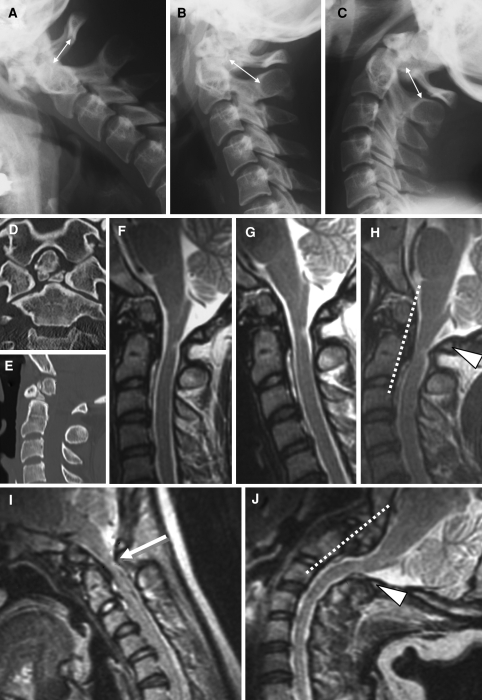
A 36-year-old woman presented with occipitocervical pain and mild dysesthsia in both hands after a minor traffic accident. The pain and hand dysesthesia were exaggerated by neck flexion but reduced in neck extension. Neurological examination revealed a mild sensory disturbance in the left C2 dermatome and bilateral upper and the right lower extremities. Plain X-ray films showed the dislocation of C1 anteriorly in flexion and posteriorly in extension (Fig. 2a–c). Although the dynamic change of bony canal was not easy to evaluate since the posterior surface of odontoid process was not clear, it seemed to be narrowest in flexion. Reconstructed images of CT showed a discontinuity of the dense to the body of axis probably due to the old fracture (Fig. 2d, e). The s-MRI in neutral position showed the intramedullary signal change in the dorsal part of the spinal cord at C1 level (Fig. 2f). Dynamic study in s-MRI showed mild compression of the spinal cord in extension (Fig. 2h) but not in flexion (Fig. 2g). Although the range of dynamic movement was different between u-MRI and s-MRI, u-MRI showed the spinal cord compression in flexion (Fig. 2i) but not in extension (Fig. 2j), that was completely different from the results of s-MRI. From the symptoms that the pain and dysesthesia were induced in neck extension, the results of u-MRI seemed to represent the actual pathophysiology rather than s-MRI.
Fig. 2.
Case 2. a–c Dynamic cervical radiographs. The bony canal diameter between the base of dens and the posterior arch of C1 in flexion is lesser than the diameter between dens and C2 lamina in neutral or extension (arrows). d, e Bone-window CT reconstructions show the discontinuity of dens to axis with small bone fragments between them. MRIs taken in supine position show the hyperintensity lesion in the dorsal part of spinal cord at C1 that is compressed in extension (h) but not in neutral (f) nor in flexion (g). Dynamic MRIs taken in upright position show the cord compression in flexion (i, white arrow) but not in extension (j)
Discussion
It is shown here that in patients with A-A dislocation the MR images taken in supine position do not always make clear the pathophysiology. In anterior A-A dislocation spinal cord is usually compressed in neck flexion but not in extension [4]. In Case 1, u-MRI clearly showed anterior dislocation and cord compression in neutral and extended position of the neck as well as in flexed position. In this case kyphotic deformity of the lower cervical spine made the long-axis of dens decline anteriorly in neutral position that resulted the anterior dislocation of C1 and also induced the compensatory extension of upper cervical spine with resultant narrowing of bony spinal canal. The anterior dislocation was exaggerated by neck flexion, resulting the narrowing of bony spinal canal. In extension, anterior dislocation was reduced and the bony canal was increased in plain X-ray filum but the interlaminal space was reduced in u-MRI, probably because the interlaminal ligament was made buckled into spinal canal. The localized extension in craniocervical junction was not reproduced in supine position probably because the nuchal muscle is relaxed without loading of the head weight. The vertical instability might also exaggerate the buckling of the ligament although it was not possible to evaluate by plain X-P.
In Case 2, neck position compressing the cord was different between s-MRI and u-MRI. Disconnection of dens from C2 body made the dislocation of the atlas not only anteriorly but also posteriorly depending on neck movement [2]. In r-MRI the head was hold by the pillow with resultant of the loss of gravitational effect, posterior dislocation of the atlas could not always be reproduced but the anterior dislocation might be induced by any neck position as in Case 2. Thus, by neck extension two pathophysiological events of cord compression, the anterior dislocation of the atlas and buckling of the yellow ligament, which are not always coupled, could be induced at the same time in supine position, resulting in compression of the spinal cord. In contrast, in upright position, atlas–odontoid complex dislocated posteriorly in extension similar to plain X-P but the buckling of the ligament was reduced, resulting less compression of the cord.
MRI can provide significant details regarding bony and/or soft tissue compressions in cervical spine, and the dynamic study might provide additional information in some cases. However MRI taken in supine position does not always represent the actual pathology as Case 1. And the dynamic movement in recumbent position does not always reproduce the real dynamic pathology as Case 2. Especially in craniocervical junction pathology, care must be taken to interpret the findings of MRI in recumbent position that cannot always represent the real pathology. For accurate understanding of A-A instability and planning the operative procedure, s-MRI should be evaluated by the actual dynamics, using the modality such as plain X-rays taken in the upright position, and by through neurological examination [1, 4]. The u-MRI represents the spinal cord compression in dynamic neck movement much more precisely than s-MRI that could be a powerful tool to reveal the real dynamic pathophysiology of A-A instability.
Conclusion
In A-A lesions, s-MRI does not always explain the pathophysiological consequences without the evaluation of dynamic study in upright position, such as plain X-rays. The dynamic u-MRI gives additonal informations of the actual pathophysiology with gravitational effects of the head.
Acknowledgments
Conflict of interest statement None of the authors has any potential conflict of interest.
References
- 1.Epstein NE, Hyman RA, Rosenthal AD. Technical note: “dynamic” MRI scanning of the cervical spine. Spine. 1988;13:937–938. doi: 10.1097/00007632-198808000-00015. [DOI] [PubMed] [Google Scholar]
- 2.Hughes TB, Richmen JD, Rothfus WE. Diagnosis of os odontoideum using kinematic magnetic resonance imaging. A case report. Spine. 1999;24:715–718. doi: 10.1097/00007632-199904010-00021. [DOI] [PubMed] [Google Scholar]
- 3.Jinkins JR, Dworkin JS, Damadian RV. Upright, weight-bearing, dynamic-kinetic MRI of the spine: initial results. Eur Radiol. 2005;15:815–1825. doi: 10.1007/s00330-005-2666-4. [DOI] [PubMed] [Google Scholar]
- 4.Laiho K, Sioini I, Kautiainen H, Kauppi M. Can we rely on magnetic resonance imaging when evaluating unstable atlantoaxial subluxation? Ann Rheum Dis. 2003;62:254–256. doi: 10.1136/ard.62.3.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vitaz TW, Shields CB, Raque GH, Hushek SG, Moser R, Hoerter N, Moriarty TM. Dynamic weight-bearing cervical magnetic resonance imaging: technical review and preliminary results. South Med J. 2004;97:456–461. doi: 10.1097/00007611-200405000-00008. [DOI] [PubMed] [Google Scholar]