Abstract
Objectives
Accidental finger injections with high-dose (1:1,000) epinephrine is a new and increasing phenomenon. The purpose of this study is to document the incidence of finger necrosis and the treatment for this type of injury. The necessity or type of treatment required for this type of injury has not been established.
Methods
The literature was reviewed from 1900 to 2005 by hand and by Internet to document all cases of high-dose (1:1,000) finger epinephrine injection. In addition, the authors added five additional cases.
Results
There are a total of 59 reported cases of finger injections with high-dose epinephrine, of which, 32 cases were untreated. There were no instances of necrosis or skin loss, but neuropraxia lasting as long as 10 weeks and reperfusion pain were carefully documented. Treatment was not uniform for those who received it, but phentolamine was the most commonly used agent.
Conclusions
There is not one case of finger necrosis in all of the 59 reported cases of finger injections with 1:1,000 epinephrine in the world literature. The necessity or type of treatment of high-dose epinephrine injection injuries remains conjecture, but phentolamine is the most commonly used agent in the reported cases, and the rationale and evidence for its use are discussed
Keywords: Accidental finger injection, High-dose epinephrine, Finger necrosis
Introduction
Although the myth that low-dose epinephrine (1:100,000) causes tissue necrosis in fingers has been dealt several serious blows [2, 5, 13, 14, 20, 25, 26, 29–31], many physicians continue to believe it as it was entrenched for so many years in medical schools worldwide. A careful review [5] of the world literature from 1880 to 2000 revealed that there were 48 case reports of digital gangrene and necrosis following local anesthesia in the digits, mostly dating before 1950. Much of the data were incomplete regarding the use and concentrations of epinephrine, hot soaks, tourniquets, tight dressings, or preexisting medical conditions. Only 21 out of the 48 cases involved the use of epinephrine, and only in four was the concentration of epinephrine recorded. None of the cases involved lidocaine with epinephrine. There is clear evidence [26] that denatured acidic procaine in those days before expiry dates may have contributed to the finger necrosis previously attributed to epinephrine. We also now know that there is considerable evidence that finger epinephrine is not only safe but a very useful adjunct in hand surgery [2, 13, 14, 20, 25, 29–31].
Since the introduction of the epinephrine autoinjector (Epi-Pen) in 1980 [16] for selftreatment of anaphylaxis, there have been several reports [1, 3, 4, 6–8, 10–12, 17–19, 21–24, 27, 28] of accidental injections of high-dose epinephrine (1:1,000) into fingers and thumbs. If low-dose (1:100,000) epinephrine injection into digits is a true common cause of finger ischemia, then there should undoubtedly be case reports of finger necrosis after accidental digital injection of high-dose (1:1,000) epinephrine. We therefore decided to perform a thorough literature search to find out if there are any such cases. We were also able to provide five additional case reports, in three of which we were able to carefully document all pertinent details. A second purpose of the study was to examine the treatment of accidental high-dose epinephrine injection.
Materials and Methods
A search by hand of Index Medicus from 1900–1950 was performed using the keywords anesthetic complications, local anesthesia complications, suprarenin solutions, gangrene, necrosis, and procaine. Electronic search through Pubmed, The National Library of Medicine, and Google was performed from 1950 to 2006. The keywords searched were Epi-Pen, Anakit, epinephrine digital injection, accidental Epi-Pen injection, finger necrosis, and epinephrine digit.
Five additional cases of high-dose epinephrine (1:1,000) were added by the authors of this paper. Three of those injection cases were by two of the authors who voluntarily had their own fingers injected with 1:1,000 epinephrine to carefully document the outcome.
Results
Table 1 summarizes the cases of high-dose epinephrine (1:1,000) finger injections that we were able to find in the world literature. Deshmukh [6], in 1989, reported a case of accidental injection of epinephrine 1:1,000 from an autoinjector into the right index finger of a 39-year-old nurse. She developed numbness, pallor, and coldness in the digit, which was treated with 1 mg of phentolamine. Thirty minutes later, the finger was pink, warm, and had normal sensation.
Table 1.
Reports of high-dose epinephrine injections (1:1,000) into fingers.
| Author | Year | Number of Cases | Treatment | Comments |
|---|---|---|---|---|
| Deshmukh N [6] | 1989 | 1 | Phentolamine 1 mg | No digital necrosis |
| Maguire WM. [17] | 1990 | 1 | Phentolamine 0.5 mg | No digital necrosis |
| McCauley WA. [18] | 1991 | 1 | Phentolamine 1.5 mg, nitropaste, warm compresses | No digital necrosis |
| Hinterberger JW. [10] | 1994 | 1 | Phentolamine 0.5 mg | No digital necrosis |
| Claudy FR. [4] | 1995 | 1 | Nitropaste and plastic wrap | Epithelial peeling, but no digital necrosis |
| Hardy SJ. [8] | 1995 | 1 | Phentolamine 2 mg, warm soaks | No digital necrosis |
| Ahearn MA. [1] | 1998 | 1 | Phentolamine 1 mg/kg | No digital necrosis |
| Kaspersen J. [11] | 1998 | 1 | Nitropaste, hot water | No digital necrosis |
| ElMaraghy MW [7] | 1998 | 6 | Phentolamine 0.5 mg | No digital necrosis |
| Nitropaste, hot compresses | No digital necrosis | |||
| Oral nifedipine | No digital necrosis | |||
| Phentolamine 1.5 mg | No digital necrosis | |||
| No treatment | No digital necrosis | |||
| Phentolamine 4.5 mg | No digital necrosis | |||
| Sellens C. [22] | 1999 | 1 | Nitropaste, phentolamine 0.5 mg | No digital necrosis |
| Stier PA. [24] | 1999 | 3 | Terbutaline 1 mg, nitropaste | No digital necrosis |
| Terbutaline 1 mg, nitropaste, warm compresses | No digital necrosis | |||
| Terbutaline 1 mg | No digital necrosis | |||
| Barkhordarian AR. [3] | 2000 | 1 | Iloprost | No digital necrosis |
| Khairalla E. [12] | 2001 | 1 | Phentolamine, calcium channel blocker | No digital necrosis |
| Mrvos R. [19] | 2002 | 28 | Phentolamine—two cases | No digital necrosis in any of the cases. |
| Terbutaline—one case | ||||
| Unknown—two cases | ||||
| No treatment—23 cases | ||||
| Velissariou I. [28] | 2004 | 3 | Nitropaste, warm compresses | No digital necrosis |
| No treatment | No digital necrosis | |||
| Phentolamine 1.5 mg | No digital necrosis | |||
| Turner MJ [27] | 2004 | 1 | Phentolamine 0.5 mg, warm soaks | No digital necrosis |
| Schintler MV [21] | 2005 | 1 | No treatment | No digital necrosis |
| Setnik L. [23] | 2005 | 1 | No treatment | No digital necrosis |
| Fitzcharles-Bowe (this paper) | 2005 | 5 | No treatment | No digital necrosis |
| Total cases | 59 | No digital necrosis |
In 1990, Maguire [17] reported a case of a 17-year-old boy who had injected his right index finger with 0.15 mg of epinephrine from an Epi-Pen injector. The finger became painful, pale, and cold. He was injected with 0.5 mg of phentolamine to each side of the digit, and 15 min later, color and warmth returned. There was no skin necrosis.
McCauley [18] reported a case in 1991 of a 28-year-old woman who accidentally injected her right index finger with 1:1,000 epinephrine from an autoinjector. Her digit became pale and cool with decreased capillary refill to the nail bed. She was treated with a digital block of lidocaine, topical nitropaste, and warm compresses with no change. She was then injected with 1.5 mg of phentolamine into the puncture site. Twenty minutes later, her digit was pink and warm with good capillary refill. No digital necrosis was seen at a 6-day follow up.
In 1994, Hinterberger [10] treated digital ischemia in a 17-year-old girl with an accidentally injected thumb with an adult epinephrine autoinjector. She received 0.5 mg of phentolamine at the puncture site with prompt resolution of ischemia. There was a loss of sensation, which started to return 5 min after the phentolamine injection. After 1 h, the sensation was back to normal.
In 1995, Claudy [4] published a case of a 35-year-old asthmatic who injected his right index finger with 0.3 cm3 of 1:1,000 epinephrine from an autoinjector. His digit was cool and white with decreased sensation. Topical nitropaste was applied and the finger was wrapped with plastic wrap. Twelve hours later, he regained color and sensation. At follow-up he had minimal epithelial peeling of the finger, which was normal at 1 month.
Also in 1995, Hardy [8] published a case of a police officer who accidentally injected his right thumb with 0.3 ml of 1:1,000 epinephrine from an Epi-Pen injector. The thumb became white and was treated with 2 mg of phentolamine and warm soaks. Thirty minutes later, warmth and color returned. The thumb was reported to have decreased sensation, which returned to normal 0.5 h after injection with the phentolamine.
In 1998, Ahearn [1] reported one episode of a 3-year-old girl who presented with a cold hand after accidental injection with an Epi-Pen injector. She was given local infiltration of phentolamine, and in 3 min, the color returned. There was no mention of sensory loss.
In 1998, Kaspersen [11] treated a case of accidental digital injection of 0.3 cm3 from an Epi-Pen injector with nitro paste and hot water. There was no report of digital necrosis.
In the same year, ElMaraghy [7] reported six cases of accidental injection of epinephrine 1:1,000 into digits. In three cases, phentolamine was used with rapid return of the digits to normal. In one of those three cases, there was mention of a loss of sensation, but the timing of its return was not documented. In the fourth case (no mention of sensory loss), oral nifedipine, 10 mg, was given with return of color after 9.5 h after treatment and 15.5 h after the initial injection. In the fifth case, in which sensory loss was documented, nitropaste and hot compresses were used with return to normal color and sensation 13.5 h after the injury. In the final case, no treatment was given and no sensory loss was reported. Within 10 h, the digit returned to normal. In none of the cases was there digital necrosis.
In 1999, Sellens [22] published a case of a 9-year-old girl who injected her right thumb with an adult epinephrine autoinjector. The digit was cold, painful, tingling, and blanching. When application of nitropaste did not improve the finger, phentolamine was infiltrated locally with return to normal in 5 min. No necrosis occurred.
The same year, Stier [24] also reported three cases of accidental injection of epinephrine into digits by autoinjectors. He treated these with terbutaline because phentolamine was not readily available. In no case was there digital necrosis. In the first case, there was normal sensation. In the second case, there was no mention of sensory deficit, and in the third, there was decreased sensation which returned to normal after 1 h of phentolamine injection. No dose was mentioned.
In 2000, Barkhordarian [3] had a case of a ward sister who injected her right thumb with 0.3 ml of 1:1,000 epinephrine. The thumb became acutely ischemic and numb. She was given iloprost and a stellate ganglion block. The thumb returned to normal color and sensation “within a few hours.”
In 2001, Khairalla [12] published a case of a radiologist who injected 1:1,000 epinephrine into her thumb. She was treated with phentolamine and a calcium channel blocker with return of the digit to normal. There was no specific information on sensation.
In 2002, Mrvos [19] published the largest series of case reports of accidental injection of epinephrine from autoinjectors in Maryland and Pittsburgh. She presented 28 cases that had been reported to the poison control center. Of these, only two patients received phentolamine, one got terbutaline, and in one, the treatment was unknown. All the other 23 cases received no treatment. There was no digital necrosis in any of the cases. Sensory loss occurred in one finger, which returned 3 h after injection with phentolamine; this was the only case in which sensory disturbance was described.
In 2004, Velissariou [28] reported three cases of accidental Epi-Pen injections into the digits of children. One child with sensory loss received nitropaste and warm compresses and sensation returned 6 h after treatment. A second child with no sensory loss was treated with 1.5 mg of phentolamine. The last child received no treatment and there was no mention of sensory disturbance.
Also in 2004, Turner [27] published a case of a 10-year-old boy who presented to the emergency department after injecting his left hand with his mother’s Epi-Pen. He was treated with 0.5 phentolamine and warm soaks, with a return to normal within 5 min. The child was reported to have reduced sensation, which was still reported to be present at the end of 6 weeks.
In 2005, Schintler [21] described a case of a 37-year-old woman who injected her index finger with an Epi-Pen. The injector penetrated the bone of the distal phalanx. She was treated with Augmentin and suffered no digital necrosis. Sensory loss was not mentioned.
In the same year, Setnik [23] published pictures of a case of accidental injection of epinephrine by an Epi-Pen in the thumb of a 16-year-old girl. She received no treatment and had no digital necrosis. There was no comment on sensory loss.
We were able to find one unusual 1953 report of non-finger skin loss that may have been attributable to high-dose epinephrine injection [15]. In 1953, Leslie and McPhee reported a case of an asthmatic who injected himself three to four times daily with epinephrine 1:1,000 to control attacks. Only after 2.5 years of injections did he develop his first episode of skin necrosis at the injection site. He continued to inject himself for another 2.5 years and developed multiple areas of skin necrosis at the injection sites. There is no mention of finger injections causing necrosis. At that time, the authors concluded that he had developed sensitivity to the epinephrine because he had used it for 2.5 years without any ill effects.
Additional Case Reports
Case #1
One of the authors of this paper (DL) had three of his own fingers injected with epinephrine on July 21, 2005, to carefully and accurately document the outcome. He had 0.5 cm3 of 1:1,000 epinephrine injected into the long finger, 0.5 cm3 of 1:10,000 epinephrine into the ring finger, and 0.5 cm3 of 1:100,000 epinephrine injected into the small finger of the left hand at one sitting. All injections were in the subcutaneous fat in the center of the finger just distal to the flexion crease of the proximal interphalangeal (PIP) joint on the volar side of the finger (see Fig. 1).
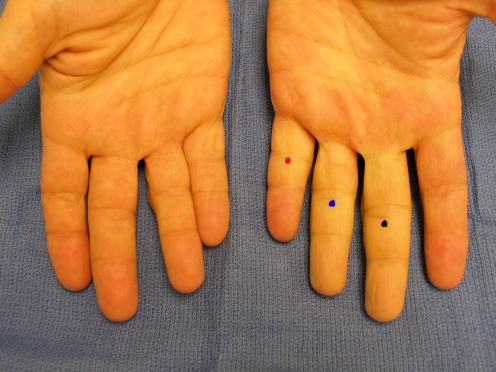
Figure 1.
Thirty minutes after 0.5 cm3 of 1:1,000 epinephrine injected into the long finger fat at the black dot, 0.5 cm3 of 1:10,000 epinephrine into the ring finger (blue dot), and 0.5 cm3 of 1:100,000 epinephrine injected into the small finger of the left hand (red dot). Note that the distal phalanx of the small finger is not pale, and that the long and ring fingers are completely white.
All three digits became very pale and cool from the finger PIP flexion crease distalward within 5 min, and all three digits became completely anesthetic, in spite of the fact that there was no lidocaine in the injectate. At 6 h and 15 min after the injection, the color and the feeling had completely returned in the small finger (1:100,000 epinephrine). At 10 h and 5 min after the injection, the color and feeling had completely returned to the ring finger (1:10,000 epinephrine). There was no significant ischemia reperfusion pain, nor was there any lasting numbness in either the small or ring fingers.
At 13 h after injection, the feeling and the color began to return to the long finger (1:1,000) epinephrine, and was accompanied by intense (7/10) reperfusion pain, which lasted approximately 4 h. At 14 h and 25 min after injection, the color had returned to normal in the long finger. At 31 h and 35 min after injection, the feeling started to return to the radial digital nerve distribution of the long finger. At 33 h and 30 min after injection, the feeling started to return to the ulnar digital nerve of the long finger. The long finger suffered a partial neuropraxia in both digital nerves, which completely resolved in the radial nerve by September 22, 2005, or 9 weeks after injection, and in the ulnar digital nerve by September 29, 2005, or 10 weeks after injection. The neuropraxia of both digital nerves of the long finger (1:1,000) resolved in the classic fashion described in the literature, with pain and temperature coming back first, followed by light touch, and finally by deep pressure. The very tip of the finger was the last part to return to normal sensibility. On a scale of 0–10, where 10 is full sensibility and 0 is complete anesthesia, the number of the feeling of light touch and deep pressure during the 10-week neuropraxic stage would be described as 8 by the author. There was no digital necrosis.
Case 2
A 35-year-old male paramedic in Saint John, Canada, suffered an accidental injection of 0.15 cm3 from an Epi-Pen in the right thumb in the middle of the middle phalanx. He was seen in the emergency department 1 h later with a very numb, white thumb. He received no treatment. He later reported that it took 2 h for sensation to return completely, and 5 h for the thumb to return to a normal color. He suffered no digital necrosis.
Case 3
A 42-year-old female from Nova Scotia, Canada, accidentally injected her right thumb with 0.15 cm3 of 1:1,000 epinephrine from her Epi-Pen. She was seen in the emergency department for numbness in the thumb but retained normal color. She received no treatment. She reported that 6 h after the injection, pain and temperature sensation returned. Twelve hours later, she had a return of light touch sensation. She suffered no digital necrosis.
Cases 4 and 5
Another author of this paper (KD) had 0.5 cm3 of 1:1,000 epinephrine injected into the little finger, 0.5 cm3 of 1:10,000 epinephrine into the ring finger, and 0.5 cm3 of 1:100,000 epinephrine into the middle finger of one hand at one sitting. In addition, all fingers had 0.5 cm3 of lidocaine plain injected concurrently with the epinephrine in the same syringe. The 1.0 cm3 total injections were subcutaneous, volar, and central, at the proximal crease of the PIP joint. All fingers very rapidly became locally ischemic and numb. Over a period of 6–12 h, complete sensation and color all returned, with the little finger being the last to recover.
On a separate occasion, 1 cm3 of pure 1:1,000 epinephrine was injected subcutaneously, volar, and centrally, at the proximal crease of the PIP joint of the little finger and 1 cm3 of pure 1:10,000 epinephrine into the ring finger without any local anesthetic (Figs. 2 and 3). The fingers became very white, numb, and ischemic. However, within 12 h, all the blanching and sensory loss had resolved. He suffered no neuropraxia or digital necrosis with any of the injections.
Figure 2.

Twenty minutes after injection of 1 cm3 of pure 1:1,000 epinephrine into the little finger.
Figure 3.

Same finger 6 h later.
Discussion
This paper reviewed all the reported cases of accidental high-dose (1:1,000) epinephrine injection in a finger from 1900 to 2005. We found 54 cases of injection of epinephrine 1:1,000 into a digit, and added five more for a total of 59 cases. Of these, 13 patients were treated with phentolamine [1, 6–8, 10, 12, 17, 19, 27, 28], four patients were treated with nitropaste [4, 7, 11, 28], two patients were treated with phentolamine and nitropaste [18, 22], two patients were treated with terbutaline [3, 24], two patients were treated with terbutaline and nitropaste [24], one patient was treated with iloprost [3], and one patient was treated with nifedipine [7] for ischemia. In two cases, the treatment was unknown [19]. In 32 cases, there was no treatment [7, 15, 19, 23, 28].
The types of treatment provided in 27 of the 59 cases that received treatment were variable. Although details in the reports were generally scarce, phentolamine was the most commonly used treatment, and this treatment appeared to have the most success at vasoconstriction reversal in those reports. Phentolamine is an α blocker that was introduced as a catecholamine vasoconstriction rescue agent in 1957 [32]. This drug has long been clinically recognized as the catecholamine extravasation vasoconstriction α receptor reversal agent of choice [9]. This is consistent with the experimental evidence, which has shown that 1 mg of phentolamine in 1 cm3 of saline reliably completely reverses epinephrine vasoconstriction in the human finger in an average of 1 h and 25 min after injection of the phentolamine where 1:100,000 epinephrine was injected, whereas it takes an average of 5 h and 19 min for the epinephrine-injected fingers to return to the same color as the other fingers after the injection of saline instead of phentolamine [20].
To treat or not to treat high-dose epinephrine injection injuries was far from uniform in the 59 reported cases. In the 32 nontreated cases, there were no permanent sequelae. Four of the reports [4, 7, 27] described a persistent sensory loss, the most carefully documented one being the case report described in this paper. In this case, the neuropraxia took 10 weeks to resolve. Ischemia reperfusion pain was also carefully documented in this case. It would be logical but pure conjecture to conclude that treatment of the injection injury may have prevented the neuropraxia or ischemia reperfusion pain. It would also be conjecture to assume that those 27 cases that received treatment did not suffer persistent injury because of successful treatment. The necessity to treat high-dose finger epinephrine injection therefore remains undetermined.
Nevertheless, because is has been well shown that phentolamine decreases the duration of epinephrine-induced vasoconstriction time in the human finger, it is the opinion of the authors that treatment of high-dose epinephrine injuries with 1 mg/kg of phentolamine may be of value to decrease ischemia reperfusion pain and possible neuropraxia, as well as possibly decreasing the possible risk of ischemic injury in patients with preexisting finger vascular insufficiency.
Not one of the reported 59 cases of high-dose (1:1,000) epinephrine injected into fingers developed tissue necrosis. We have therefore not been able to find a single case of high-dose (1:1,000) epinephrine-induced digital infarction in the literature. This finding makes the likelihood of low-dose epinephrine (1:100,000) finger injection causing finger infarction even less likely.
Conclusions
We describe the 59 cases of high-dose epinephrine (1:1,000) injection into the fingers in the literature, none of which suffered digital necrosis, in spite of the fact that 32 of them received no treatment. This paper has also carefully documented reperfusion pain and 10 weeks of neuropraxia caused by the injection 0.5 cm3 of high-dose epinephrine (1:1,000) into a finger. The necessity or type of treatment of high-dose epinephrine injection injuries remains conjecture, but phentolamine is the most commonly used agent in the reported cases, and the evidence for its use is discussed.
References
- 1.Ahearn MA. A pulseless hand. Accidental epinephrine injection. Am Fam Phys 1998;57(6):1238. [PubMed]
- 2.Andrades PR, Olguin FA, Calderon W. Digital blocks with or without epinephrine. Plast Reconstr Surg 2003;111:1769. [DOI] [PubMed]
- 3.Barkhorvarian AR, Wakelin SH, Paes TR. Accidental digital injection of adrenaline from an autoinjector device. Br J Dermatol 2000;143(6):1359. [DOI] [PubMed]
- 4.Claudy FR. Pertinent medical intelligence: accidental digital injection of epinephrine. Md Med J 1995;44(4):292–3. [PubMed]
- 5.Denkler K. A comprehensive review of epinephrine in the finger. To do or not to do. Plast Reconstr Surg 2001;108(1):114–24. [DOI] [PubMed]
- 6.Deshmukh N, Tolland JT. Treatment of accidental epinephrine injection in a finger. J Emerg Med 1989;7(4):408. [DOI] [PubMed]
- 7.ElMaraghy MW, ElMaraghy AW, Evans HB, et al. Digital adrenaline injection injuries: a case series and review. Can J Plast Surg 1998;6(4):196–200.
- 8.Hardy SJ, Agostini DE. Accidental epinephrine auto-injector induced digital ischemia reversed by phentolamine digital block. J Am Osteopath Assoc 1995;95(6):377–8. [PubMed]
- 9.Hill JM. Phentolamine mesylate: the antidote for vasopressor extravasation. Crit Care Nurse 1991;11(10):58–61. [PubMed]
- 10.Hinterberger JW, Kintzi HE. Phentolamine reversal of epinephrine-induced digital vasospasms. How to save an ischemic finger. Arch Fam Med 1994;3(2):193–5. [DOI] [PubMed]
- 11.Kaspersen J, Vedsted P. Accidental injection of adrenaline in a finger with EpiPen. Ugeskr Laeger 1998;160(45):6531–2. [PubMed]
- 12.Khairalla E. Epinephrine-induced digital ischemia relieved by phentolamine. Plast Reconstr Surg 2001;108(6):1831–2. [DOI] [PubMed]
- 13.Krunic AL, Wang LC, Soltani K, et al. Digital anesthesia with epinephrine: an old myth revisited. J Am Acad Dermatol 2004;51(5):755. [DOI] [PubMed]
- 14.Lalonde DH, Bell M, Benoit P, Sparkes G, et al. A multicenter prospective study of 3,110 consecutive cases of elective epinephrine use in the fingers and hand: the Dalhousie project clinical phase. J Hand Surg [Am] 2005;30(5):1061–7. [DOI] [PubMed]
- 15.Leslie G, McPhee D. Adrenaline necrosis. Br Med J 1953;1315–16. [DOI] [PMC free article] [PubMed]
- 16.Lockey SD. A new method of administering aqueous epinephrine: the Epipen, an automatic syringe. J Asthma Res 1980;17(4):153–5. [DOI] [PubMed]
- 17.Maguire WM, Reisdorff EJ, Smith D, et al. Epinephrine-induced vasospasms reversed by phentolamine digital block. Am J Emerg Med 1990;8(1):46–7. [DOI] [PubMed]
- 18.McCauley WA, Gerace RV, Scilley C. Treatment of accidental digital injection of epinephrine. Ann Emerg Med 1991;20(6):665–8. [DOI] [PubMed]
- 19.Mrvos R, Anderson BD, Krenzelok EP. Accidental injection of epinephrine from an autoinjector: invasive treatment not always required. South Med J 2002;95(3):318–20. [PubMed]
- 20.Nodwell T, Lalonde DH. How long does it take phentolamine to reverse adrenaline-induced vasoconstriction in the finger and hand? A prospective randomized blinded study: the Dalhousie project experimental phase. Can J Plast Surg 2003;11(4):187–90. [DOI] [PMC free article] [PubMed]
- 21.Schintler MV, Arbab E, Aberer W, et al. Accidental perforating bone injury using the EpiPen autoinjection device. Allergy 2005;60(2):259–60. [DOI] [PubMed]
- 22.Sellens C, Morrison L. Accidental injection of epinephrine by a child: a unique approach to treatment. Can J Emerg Med 1991;1(1):34–7. [DOI] [PubMed]
- 23.Setnik L. Treatment of accidental injection of epinephrine into a digit. Archives. www.emedhome.com May 22, 2002.
- 24.Stier PA, Bogner MP, Webster K, et al. Subcutaneous terbutaline to reverse peripheral ischemia. Am J Emerg Med 1999;17(1):91–4. [DOI] [PubMed]
- 25.Sylaidis P, Logan A. Digital blocks with adrenaline. An old dogma refuted. J Hand Surg [Br] 1998;23B(1):17. [DOI] [PubMed]
- 26.Thomson CJ, Lalonde DH, Denkler KA, et al. A critical look at the evidence for and against elective epinephrine use in the finger. Plast Reconstr Surg 2007;119. [DOI] [PubMed]
- 27.Turner MJ, Purushotham AD. Accidental EpiPen injection into a digit—the value of a google search. Ann R Coll Surg Engl 2004;86(3):218–9. [DOI] [PMC free article] [PubMed]
- 28.Velissariou I, Cottrell S, Berry K, et al. Management of adrenaline(epinephrine) induced digital ischemia in children after accidental injection from an EpiPen. Emerg Med J 2004;21(3):387–8 [DOI] [PMC free article] [PubMed]
- 29.Wilhelmi BJ, Blackwell SJ. Epinephrine in the finger. Plast Reconstr Surg 2002;110(3):999. [DOI] [PubMed]
- 30.Wilhelmi BJ, Blackwell SJ, Miller J, et al. Epinephrine in digital blocks: revisited. Ann Plast Surg 1998;41(4):410. [DOI] [PubMed]
- 31.Wilhelmi BJ, Blackwell SJ, Miller JH, et al. Do not use epinephrine in digital blocks: myth or truth? Plast Reconstr Surg 2001;107(2):393. [DOI] [PubMed]
- 32.Zucker G. Use of phentolamine to prevent necrosis due to levarterenol. JAMA 1957;163(16):1477–9. [DOI] [PubMed]