Abstract
The objective of this study was to examine the predictive validity of the remission criteria proposed by Andreasen et al in first-episode patients responding to antipsychotics. Antipsychotic responsive patients with first-episode schizophrenia showing symptom remission (n = 60) were compared with patients who did not fulfill the proposed criteria (n = 65). Outcome in terms of symptom severity, social functioning, and quality of life was assessed after 18 months. Patients in the remission group showed a significantly better outcome during follow-up on all Positive and Negative Syndrome Scale subscale scores (positive, negative, and general symptom subscales) and a significantly higher level of social functioning. Quality of life did not differ between groups. The proposed multidimensional criteria for symptomatic remission convey significant information when applied to first-episode patients who responded to antipsychotics, predicting outcome on the domains of both psychopathology and social functioning. The criteria represent a practicable benchmark with clinical relevance. Their implementation should be promoted in research settings, clinical practice, and routine outcome assessment procedures.
Keywords: remission, outcome, schizophrenia, first episode, criteria
Introduction
In schizophrenic research, general agreement on criteria of treatment outcome is currently lacking.1 An important and timely effort was made last year by Andreasen et al by proposing consensus criteria for symptomatic remission.2 These criteria are defined by thresholds of severity of selected symptoms, representing the 3-dimensional components of the disease process in schizophrenia: psychoticism (reality distortion), disorganization, and negative symptoms (psychomotor poverty). The proposed criteria are to provide a benchmark allowing the cross-trial comparison of treatment outcomes and to set a standard for the evaluation of the effectiveness of interventions. However, the predictive validity of the proposed criteria regarding symptomatic and functional outcomes has yet to be established. This article is a contribution to this issue using longitudinal data from a sample of first-episode schizophrenic patients.
Throughout the literature on schizophrenia a wide array of outcome criteria have been reported.3 First-episode studies defining criteria for remission mainly focused on positive symptoms.4–7 As modern therapy goals are extended to restore real-life functioning, aiming at recovery, we need a view less constrained by exclusively focusing on these symptoms.2 The elimination of positive symptoms alone does not adequately define symptomatic outcome. Andreasen et al acknowledged this view by also including negative and disorganization symptoms in their set of outcome criteria. The authors also made a distinction between symptomatic remission and the more demanding concept of recovery. Recovery implies a return to former, or even higher, levels of social and vocational functioning. According to their view, long-term multidimensional symptom remission may be a prerequisite for the achievement of these functional gains.2,8,9
These issues are particularly important in first-episode patients, in view of their greater potential for functional recovery and modern treatment perspectives. This study addresses the question whether the proposed multidimensional remission criteria predict symptomatic and functional outcomes in first-episode patients.
METHOD
Patient Sample
The patients included in the study sample were recruited as part of the Medication Strategies in First Onset Schizophrenia study. They were first-episode patients, aged 18–45 years, who had never been treated with antipsychotics before and who showed 6 months of positive symptom remission within their first year of treatment. A remission of positive symptoms was a formal criterion for participation in the study. Positive symptom remission implied a sustained response during the 6 months defined by Positive and Negative Syndrome Scale (PANSS) positive subscale item scores, allowing for up to 1 item score of 4 (moderate). Recruitment took place from October 2001 through December 2002 in a catchment area of 3.1 million inhabitants. The cohort was representative of first-episode patients who were willing to engage in treatment .10 Patients were asked to participate in the study as soon as they were able to understand the consequences of participation, usually around the time of first treatment response of positive symptoms. Soon after written informed consent was obtained, a research psychiatrist diagnosed the patient using a computerized version of the Schedules for Clinical Assessment in Neuropsychiatry (SCAN).11 The DSM-IV diagnosis had to match one of the following: schizophrenia, schizophreniform disorder, brief psychotic disorder, schizoaffective disorder, delusional disorder, or psychotic disorder not otherwise specified.
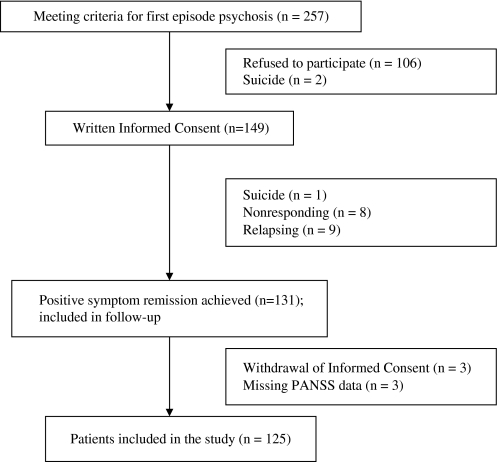
Of 257 treatment-naive first-episode patients who met the study criteria, 149 (58%) gave written informed consent. Two patients committed suicide and 106 patients refused participation. There were no differences between participants and nonparticipants regarding gender, age at first contact, marital status, living situation, and illicit drug use. An anonymous enquiry suggested that treatment response occurred less frequently in these patients and that most of the nonparticipants did not achieve remission of positive symptoms.
Of the 149 patients who were willing to participate, 131 (88%) showed a 6-month remission of positive symptoms within the first year of treatment and 18 did not: 1 patient committed suicide, 9 patients relapsed within 6 months after response, and 8 patients did not respond with adequate positive symptom reduction within 6 months of antipsychotic treatment. Three patients withdrew informed consent during follow-up (see figure 1). Of another 3 patients PANSS data at T0 or T6 were missing. This leaves 125 patients to be included in this study.
Fig. 1.
Flow Diagram.
Predictors of Outcome
In order to examine the association of conceivable predictors of outcome and the achievement of remission status, we recorded gender, age at onset of psychosis, duration of untreated psychosis (DUP), time to response (TTR) of positive symptoms, baseline social functioning (Groningen Social Disabilities Schedule [GSDS]), and living situation (living alone vs with others). DUP was assessed during the SCAN interview and defined by the time between the first manifestation of any positive psychotic symptom and the start of antipsychotic treatment. Sporadic psychotic symptoms were not included. TTR was defined by the time from the start of antipsychotic treatment until first treatment response.10
Operationalization of the Remission Status
In accordance with the proposal of Andreasen et al, selected items from the PANSS were used to determine the remission status of the patients included in the study. These criteria require sustained ratings of mild or lower severity (≤3) on all relevant items. For the dimension of reality distortion the selected PANSS items are P1 (delusions), P3 (hallucinatory behavior), and G9 (unusual thought content); for the dimension of disorganization they are P2 (conceptual disorganization) and G5 (mannerisms/posturing); and for the dimension of negative symptoms they are N1 (blunted affect), N4 (social withdrawal), and N6 (lack of spontaneity). Patients were monitored from the moment of response of positive symptoms for relapses of any symptoms, both by research nurses as well as clinicians. Patients who met the proposed criteria both at the time of response and 6 months later and who did not show a relapse of any symptoms between these assessments were considered to have achieved symptomatic remission status.
Outcome Assessment
Outcome was assessed after 18 months of follow-up and included psychopathology, social functioning, and quality of life. Psychopathology was assessed with the PANSS to measure observer-rated severity of positive, negative, and general symptoms during the preceding week.12 Social functioning was assessed with the GSDS, a semistructured interview with observer ratings of functioning over the 4 weeks preceding the interview. At baseline, GSDS was rated over the 4 weeks preceding treatment. Functional disabilities are rated on a 4-point scale, lower scores indicating less disability in 7 social role domains: work, community integration, social relationships, relationship with family, relationship with partner, household activities, and self-care. A total disability score ranging from 0 to 21 is calculated adding these 7 domains. The GSDS has good psychometric properties.13,14
Quality of life was assessed with the WHOQoL-Bref, a 26-item self-report questionnaire, comprising satisfaction with health, psychological functioning, social relationships, and environmental opportunities, as experienced over the last 2 weeks. Each item is scored on a 5-point scale, higher scores indicating better quality of life. We will present the total score, ranging from 26 to 130.15
In order to examine the possibility that remission status was related to a different antipsychotic dose regimen during follow-up, which might mediate outcome, we also checked the mean daily dose of antipsychotics during follow-up. We used existing conversion and dose range recommendation tables to convert prescribed doses of antipsychotics to haloperidol equivalents.16
Training and Reliability
Psychiatrists who were formally trained by the Groningen World Health Organization (WHO) Training Center administered the SCAN interview. Training for PANSS and GSDS was provided at investigator meetings, supplemented by written training materials. Training for the PANSS and GSDS included rating of a videotaped interview, followed by discussion and review of ratings. Regular booster meetings were organized to maintain interrater reliability. Reliability of the GSDS was established by 12 raters, all rating the same 11 subjects. We used another 12 subjects, all rated by 11 raters, to establish the reliability of the PANSS. We calculated weighted kappas for each GSDS item. The square weighted kappa scores ranged from .55 to .88 for each GSDS item, with a mean of .67. The 2-way mixed model intraclass correlation coefficient (ICC) was used to assess the reliability of the PANSS scales. The ICC for the PANSS subscale of positive symptoms was .84 and for the subscale of negative symptoms was .83.
Statistical Analysis
Analyses were carried out with the statistical package SPSS (version 12.0.2; SPSS Inc., Chicago, Ill). Differences between baseline characteristics of remitted and nonremitted patients were analyzed using the Student t tests for continuous variables and Pearson chi-square tests for categorical variables. Nonparametric analyses (Mann-Whitney U tests) were applied for DUP and TTR because of their positively skewed distribution. Binary logistic regression analysis was applied to find factors predicting remission status. Because of their skewed distribution, DUP and TTR were log transformed in this analysis. Outcome differences between the remitted and nonremitted groups after 18 months of follow-up were analyzed with analysis of variance, including PANSS positive, negative, and general symptoms subscale total scores, GSDS total scores, and World Health Organization Quality of Life Scaletotal scores. A general linear model (uni-anova) was used to examine the prediction of social functioning (GSDS total scores) after 18 months of follow-up by remission status adjusting for baseline GSDS scores.
Results
Baseline Characteristics
Of 125 patients in the study, 60 patients (48%) achieved remission status, while 65 (52%) did not. Baseline characteristics of the sample are given in table 1.
Table 1.
Baseline Characteristics of the Sample (N = 125)
| Characteristic | Statistic | Value |
| Male | n (%) | 86 (68.8) |
| Living alone | n (%) | 46 (36.8) |
| Married or cohabiting | n (%) | 19 (15.2) |
| Schizophrenia | n (%) | 57 (45.6) |
| Other nonaffective psychosis | n (%) | 68 (54.4) |
| Cannabis dependence/abuse | n (%) | 30 (24.0) |
| Age at onset psychosis | Mean (SD) | 25.7 (6.7) |
| Age at start of treatment | Mean (SD) | 26.4 (6.4) |
| Duration of untreated psychosis, d | Mean (SD) [median] | 265 (535) [31] |
| Time to response, d | Mean (SD) [median] | 75.9 (52.9) [61.0] |
| GSDS total score T0 | Mean (SD) | 8.5 (4.3) |
| WHOQoL total score T0 | Mean (SD) | 91.7 (12.3) |
Note: GSDS, Groningen Social Disability Schedule; WHOQoL, World Health Organization Quality of Life Scale.
Bivariate analyses showed that patients achieving remission status already differed at baseline from nonremitted patients (table 2).
Table 2.
Differences Between Remitted and Not-Remitted Patients at Baseline
| Variable | Remitted | Not Remitted | Statistic | P Value (2-sided) | |
| n (%) of males | 36 (60.0) | 50 (76.9) | Pearson χ2 | 4.163 | .041 |
| Age at onset psychosis, mean (SD), y | 27.0 (6.6) | 24.5 (6.6) | t test | −2.065 | .041 |
| DUP, mean (SD) [median], d | 181 (377) [31] | 343 (640) [61] | M-W Z score | −2.019 | .043 |
| TTR, mean (SD) [median], d | 67 (50) [59] | 84 (54) [90] | M-W Z score | −2.033 | .042 |
| PANSS positive symptoms subscale, mean (SD) | 9.1 (2.3) | 11.4 (3.1) | t test | 4.581 | .000 |
| PANSS negative symptoms subscale, mean (SD) | 11.2 (3.6) | 15.8 (5.4) | t test | 5.599 | .000 |
| PANSS general symptoms subscale, mean (SD) | 23.0 (5.6) | 28.7 (6.4) | t test | 5.245 | .000 |
| GSDS total score, mean (SD) | 7.3 (3.7) | 9.7 (4.5) | t test | 3.185 | .002 |
| WHOQoL total score, mean (SD) | 92.7 (12.0) | 90.7 (12.6) | t test | −0.875 | .383 |
Note: SD, standard deviation; DUP, duration of untreated psychosis; TTR, time to response; M-W, Mann-Whitney statistic; PANSS, Positive and Negative Syndrome Scale; GSDS, Groningen Social Disability Schedule; WHOQoL, World Health Organization Quality of Life Scale.
As expected, the PANSS subscale scores at baseline of remitted and nonremitted patients also differed significantly, but they are not independent from the remission criteria.
To examine the relative contribution of the baseline factors to remission status, excluding the PANSS subscale scores, we tested a logistic regression model. The GSDS total score at baseline remained as the only significant predictor of remission status (odds ratio = 0.89, P = .032). Because higher scores imply worse social functioning, the odds ratio demonstrates that worse baseline social functioning predicts a lower probability of remission status.
The predictive validity of the proposed remission status was tested on a range of outcome criteria after 18 months of follow-up (see table 3).
Table 3.
Predictive Validity of Proposed Remission Criteria. Analysis of Variance With Outcome Measures After 18 Months of Follow-up
| Outcome Measure | Remitted, Mean (SD) | Not Remitted, Mean (SD) | F | P |
| PANSS positive subscale | 10.0 (3.5) | 11.7 (4.4) | 5.329 | .023 |
| PANSS negative subscale | 11.5 (5.9) | 13.8 (5.3) | 5.225 | .024 |
| PANSS general subscale | 22.9 (6.4) | 26.5 (7.0) | 8.497 | .004 |
| GSDS total scorea | 4.8 (4.2) | 7.1 (4.0) | 4.787 | .031 |
| WHOQoL total score | 98.4 (13.2) | 96.5 (12.7) | 0.713 | .400 |
Note: SD, standard deviation; PANSS, Positive and Negative Syndrome Scale; GSDS, Groningen Social Disability Schedule; WHOQoL, World Health Organization Quality of Life Scale.
Adjusted for GSDS at baseline.
Remission status predicted a better outcome after 18 months on all 3 PANSS subscales and the GSDS social functioning score adjusted for social functioning at baseline. Quality of life did not differ between the remitted and nonremitted groups.
The mean daily dose of antipsychotics during follow-up did not differ between remitted and nonremitted patients (F = 1.4, P = .238).
Discussion
We studied a sample of first-episode schizophrenic patients who met the traditional 1-dimensional criteria for remission, limited to positive psychotic symptoms. The reader should be aware that the selection of this sample (about 50% of all incident cases) limits the generalizibility of the results to patients with positive symptom remission only. These symptoms were usually the reason for seeking treatment. They generally showed a better response to treatment compared with negative and disorganization symptoms. Recently, the focus of treatment shifted toward functional outcome, making other symptom dimensions at least equally important as the positive dimension.
Applying the multidimensional remission criteria proposed by Andreasen et al to our sample results in 2 groups of almost equal size. One half still suffered from negative and/or disorganization symptoms while the other half had reached a true symptomatic remission on all 3 dimensions.
The question has to be answered whether these criteria are informative regarding symptomatic and functional outcomes. Our results show that remission according to the Andreasen criteria predicted lower psychopathology scores on all 3 symptom dimensions after 18 months of follow-up, but more interestingly, also better outcome in the domain of social functioning. Thus, the proposed remission criteria convey clinically and functionally significant information and offer a valid and relevant benchmark for symptomatic convalescence and functional recovery.
However, remission did not lead to higher self-reported quality of life. Appraisal by clinicians in terms of PANSS and GSDS scores did not seem to be reflected by the patients’ own reports of their well-being. This might be explained by the broad scope of the quality of life instrument which covers satisfaction with physical and mental health, social interactions, as well as environmental conditions. It is unlikely that remission alone will affect all these dimensions in a relatively short period of time.
Another limitation of our study is the relatively short period of observation. Long-term follow-up studies have shown that a subgroup of patients recover after many years of illness.17,18 Patients who do not respond favorably in the beginning may do so later on. For example, Harrow et al showed that 10% recovered after 2 years of follow-up but about 20% after 4.5 years or later.19
So far, we have studied early symptom remission. The question has yet to be answered whether the predictive validity of remission status is preserved if it is achieved after longer periods of treatment and/or multiple episodes.
Finally, an important next step will be the definition of criteria for functional recovery, which have to include measures of social functioning.
Acknowledgments
We acknowledge Zorgonderzoek Nederland Medische Wetenschappen (DO945-01-001), Stichting Steun V.C.V.G.Z (Arnhem), Stichting Dienstbetoon (Soesterberg), Eli Lilly Nederland B.V.
References
- 1.Boshes RA, Manschreck TC. Review of antipsychotic medication administration: a proposal of intermittent dosing. Schizophr Bull. 2002;28:203–222. doi: 10.1093/oxfordjournals.schbul.a006932. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen NC, Carpenter WT, Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162:441–449. doi: 10.1176/appi.ajp.162.3.441. [DOI] [PubMed] [Google Scholar]
- 3.Hegarty JD, Baldessarini RJ, Tohen M, Waternaux C, Oepen G. One hundred years of schizophrenia: a meta-analysis of the outcome literature. Am J Psychiatry. 1994;151:1409–1416. doi: 10.1176/ajp.151.10.1409. [DOI] [PubMed] [Google Scholar]
- 4.Amminger GP, Resch F, Mutschlechner R, Friedrich MH, Ernst E. Premorbid adjustment and remission of positive symptoms in first-episode psychosis. Eur Child Adolesc Psychiatry. 1997;6:212–218. doi: 10.1007/BF00539928. [DOI] [PubMed] [Google Scholar]
- 5.Ho BC, Andreasen NC, Flaum M, Nopoulos P, Miller D. Untreated initial psychosis: its relation to quality of life and symptom remission in first-episode schizophrenia. Am J Psychiatry. 2000;157:808–815. doi: 10.1176/appi.ajp.157.5.808. [DOI] [PubMed] [Google Scholar]
- 6.Eaton WW, Thara R, Federman E, Tien A. Remission and relapse in schizophrenia: the Madras Longitudinal Study. J Nerv Ment Dis. 1998;186:357–363. doi: 10.1097/00005053-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Lieberman J, Jody D, Geisler S, et al. Time course and biologic correlates of treatment response in first-episode schizophrenia. Arch Gen Psychiatry. 1993;50:369–376. doi: 10.1001/archpsyc.1993.01820170047006. [DOI] [PubMed] [Google Scholar]
- 8.van Os J, Burns T, Cavallaro R, et al. Standardized remission criteria in schizophrenia. Acta Psychiatr Scand. 2006;113:91–95. doi: 10.1111/j.1600-0447.2005.00659.x. [DOI] [PubMed] [Google Scholar]
- 9.Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 2004;161:473–479. doi: 10.1176/appi.ajp.161.3.473. [DOI] [PubMed] [Google Scholar]
- 10.Wunderink A, Nienhuis FJ, Sytema S, Wiersma D. Treatment delay and response rate in first episode psychosis. Acta Psychiatr Scand. 2006;113:332–339. doi: 10.1111/j.1600-0447.2005.00685.x. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organisation. Schedules for Clinical Assessment in Neuropsychiatry. Version2.1. Geneva, Switzerland: Author; 1992. [Google Scholar]
- 12.Kay S, Fishbein A, Opler L. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–275. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 13.Wiersma D, de Jong A, Kraaijkamp HJM, Ormel J. GSDS II, The Groningen Social Disabilities Schedule. Version 2. Groningen, Netherlands: Department of Psychiatry, Rijksuniversiteit Groningen; 1990. [Google Scholar]
- 14.Wiersma D, Jong Ad, Ormel J. The Groningen Social Disabilities Schedule: development, relationship with the ICIDH and psychometric properties. Int J Rehabil Res. 1988;11:213–224. [PubMed] [Google Scholar]
- 15.O'Carroll RE, Smith K, Couston M, Cossar JA, Hayes PC. A comparison of the WHOQOL-100 and the WHOQOL-BREF in detecting change in quality of life following liver transplantation. Qual Life Res. 2000;9:121–124. doi: 10.1023/a:1008901320492. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Practice Guideline for the Treatment of Patients with Schizophrenia. 2nd ed. Washington, DC: 2004. [Google Scholar]
- 17.Harrison G, Hopper K, Craig T, et al. Recovery from psychotic illness: a 15-and 25-year international follow-up study. Br J Psychiatry. 2001;178:506–517. doi: 10.1192/bjp.178.6.506. [DOI] [PubMed] [Google Scholar]
- 18.Harding CM. Course types in schizophrenia: an analysis of European and American studies. Schizophr Bull. 1988;14:633–643. doi: 10.1093/schbul/14.4.633. [DOI] [PubMed] [Google Scholar]
- 19.Harrow M, Grossman LS, Jobe TH, Herbener ES. Do patients with schizophrenia ever show periods of recovery? A 15-year multi-follow-up study. Schizophr Bull. 2005;31:723–734. doi: 10.1093/schbul/sbi026. [DOI] [PubMed] [Google Scholar]