Abstract
This article presents the rationale, design, and preliminary findings of the North American Prodrome Longitudinal Study (NAPLS), a collaborative, multisite investigation into the earliest phase of psychotic illness. We describe how 8 independently conceived research projects were integrated methodologically, how diagnostic reliability was achieved across sites on the Structured Interview for Prodromal Syndromes, and how baseline and follow-up data were aggregated for 888 at risk and comparison subjects. Data are presented describing the demographic, academic/work, and diagnostic characteristics of 3 relevant subgroups: persons at heightened clinical risk for psychosis, help-seeking comparison subjects, and nonpsychiatric controls. The NAPLS data set will be used to explore a series of questions related to prodromal psychosis, including the descriptive phenomenology of currently accepted diagnostic criteria, conversion rates over a 30-month period, predictors of psychosis onset and functional disability, and the impact of early treatment on the course of prodromal symptoms.
Keywords: psychosis, prodrome, schizophrenia, consortium, early detection, prevention, NAPLS
Introduction
There has been increasing interest in the potential for early detection and intervention during the prodromal phase of a psychotic disorder, ie, the period of functional decline before full-blown psychotic symptoms first appear.1 Interceding here, when psychological and interpersonal resources may be relatively intact, may offer the greatest opportunity to redirect the illness' negative trajectory.2,3 In the United States, research into the schizophrenia prodrome was spurred by the 1999 program announcement issued by the National Institute of Mental Health (NIMH), “Prevention and Early Intervention in Psychotic Disorders.” 7 projects subsequently funded by NIMH between 2000 and 2003 focused on refining prodromal diagnostic criteria, characterizing prodromal stages in greater detail and improving the accuracy of risk prediction models.
Experience with these projects revealed several challenges to conducting prospective research with at risk individuals.4 Sample size is the principal obstacle to achieving rapid progress in prodromal research because, first, the annual incidence of new cases is presumed to be low (ie, no more than 1 case per 10 000 persons per year in the general population) and, second, these individuals are hard to find. Annual recruitment has averaged 18 at risk subjects per year in the single-site prodromal schizophrenia research studies funded by NIMH since 2000. Without a dramatic improvement in recruitment, we estimate that it will take nearly a decade for a single-site study to accrue a sample of at risk subjects adequately powered to test hypotheses related to psychosis onset, illness progression, short-term outcome, and discriminating true from false-positive prodromal cases.
Collaborative multisite projects represent 1 alternative to the typical single-site, single Principal Investigators (PI) approach to early schizophrenia research. Spreading recruitment responsibilities across multiple sites will produce larger samples of at risk individuals over shorter periods, thereby solving the sample size/time frame dilemma.4 Going forward, large samples of at risk subjects will be necessary to detect the subtle neurobiological processes that may drive progression to active illness.5 In the short term, more robust samples are critical for addressing fundamental questions about the psychosis prodrome, including the validity of current diagnostic criteria, the precision of risk prediction methods, and the impact of early treatment on the course of prodromal symptoms and disorder.
The purpose of this article is to describe a recently established consortium of prodromal psychosis research centers known collectively as the North American Prodrome Longitudinal Study (NAPLS). Our goal is to recount how a collection of independently conceived projects were integrated retrospectively, how reliability was established on key diagnostic measures, and how descriptive, clinical, and functional outcome variables were selected and aggregated into a federated, longitudinal database. Characteristics of the integrated database are presented, including selected demographic and clinical variables for 888 at risk and comparison subjects. We then discuss how the cross-site data set will be utilized to address a series of scientific questions about the nature of the prodromal syndrome. Finally, we speculate on future prospects for collaborative, large-scale research approaches to early schizophrenia. First we describe the current NAPLS sites, as well as the organization and management of the research consortium.
NAPLS Sites, Organization, and Management
The 8 NAPLS research programs are presented in Table 1. 7 of the investigations focus on characterizing the schizophrenia prodrome and improving the accuracy of prospective prediction of initial psychosis; Harvard University (HU) was added to the NAPLS consortium in order to include a sample of well-characterized genetic high-risk subjects in the analysis of psychosis risk factors.
Table 1.
Research Centers Participating in the North American Prodrome Longitudinal Study
| Research Center | Principal Investigators | Initial NIMH Funding Date | Project Title |
| ZHH | Barbara Cornblatt | April 27, 2000 | Characterization of Prodromal Schizophrenia |
| UCSD | Kristin Cadenhead | May 7, 2000 | Vulnerability Markers in Prodromal Schizophrenia |
| EU | Elaine Walker | March 19, 2002 | Prediction of Psychosis in Schizotypal Adolescents |
| UCLA | Tyrone Cannon | January 16, 2003 | Working Memory and Social Functioning in Schizophrenia |
| UNC | Diana Perkins | May 08, 2003 | Enhancing the Prospective Prediction of Psychosis |
| YU | Scott Woods | May 08, 2003 | Enhancing the Prospective Prediction of Psychosis |
| Thomas McGlashan | |||
| UT | Jean Addington | May 08, 2003 | Enhancing the Prospective Prediction of Psychosis |
| HU | Larry Seidman | July 01, 2005 | Schizophrenia—Psychopathology and Heterogeneity |
| Ming Tsuang |
Note: NIMH, National Institute of Mental Health; ZHH, Zucker Hillside Hospital; UCSD, University of California San Diego; EU, Emory University; UCLA, University California Los Angeles; UNC, University of North Carolina; YU, Yale University; UT, University of Toronto; HU, Harvard University.
Methodological similarities among the NAPLS sites include identical procedures for identifying at risk subjects (described below), inclusion of nonprodromal, help-seeking, and normal comparison subjects, clinical monitoring of subjects for at least 2 years following initial evaluation, and conversion to psychosis as the principal outcome of interest. Although clinical, behavioral, and neuropsychological assessment methods differ across the projects, there is considerable overlap in constructs measured at baseline and follow-up evaluations.
Organizing the Research Consortium
Between January 2004 and July 2006, NAPLS PIs designed the multisite collaboration with active participation from NIMH program staff. Guidance for organizing and managing consortium activities came from a recent Institute of Medicine report on large-scale approaches to biomedical research.6 Governance principles are summarized in a memorandum of understanding, as are agreements regarding access to the federated database and the publication of results.
Consortium members agreed early on that 4 major tasks had to be accomplished: (1) obtaining Institutional Review Board (IRB) approval, (2) determining cross-site consistency in diagnosis, (3) determining the core set of variables, and (4) developing a common platform for electronic data and procedures for data management. Regarding IRB approval, each NAPLS site obtained permission to contribute anonymous data to the consortium database before data were merged. Methods for establishing diagnostic reliability, selecting key variables for the combined database, and recoding and combining data are as follows.
METHOD
Establishing Diagnostic Reliability
The NAPLS projects employ similar ascertainment and longitudinal assessment methods. Specifically, each site utilizes the Structured Interview for Prodromal Syndromes (SIPS) to evaluate and monitor prodromal symptoms for all at risk and comparison subjects. Detailed descriptions of SIPS symptom severity scales, prodromal diagnostic criteria, and psychometric properties are available.7–9
To justify the pooling of data for at risk and comparison subjects across research programs, it was necessary to demonstrate that sites applied SIPS prodromal syndrome criteria equivalently. Data supporting cross-site consistency in diagnostic methods come from a rater-training program developed at Yale University that teaches clinical researchers to identify features of the prodromal syndrome with good reliability.8–10 The kappa statistic11 is used to compare trainee agreement with the “gold standard” diagnosis of presence or absence of a prodromal syndrome.
Rater-training workshops were conducted at different times at 7 NAPLS sites with 40 raters. The majority of the sites completed the workshop prior to recruiting clinical at risk subjects (Emory University [EU], Harvard University [HU], University of California Los Angeles [UCLA], University of California San Diego [UCSD], University of North Carolina [UNC])9. 2 other sites (University of Toronto [UT] and Zucker Hillside Hospital (ZHH)) had received training from the Yale group previously but completed the rater-training workshop as part of the NAPLS project. Table 2 shows diagnostic agreement before and after training at each site. Post-training data within sites demonstrate that agreement with gold standard diagnoses was in the excellent range at each of the 7 centers. This bolsters confidence that SIPS diagnostic criteria were applied uniformly across NAPLS sites and justifies the decision to aggregate data for independently acquired at risk and comparison subjects.
Table 2.
Agreement between Trainees and Expert Trainer on SIPS Diagnosis before and after a 2 Day Rater-Training Workshopa
| Site |
||||||||
| Rating Session | EU | HU | UCLA | UCSD | UNC | UT | ZHH | All Sites |
| Before Training | 0.25 | 0.60 | 0.43 | 0.40 | 0.50 | 0.80 | 1.00 | 0.52 |
| After Training | 1.00 | 1.00 | 0.86 | 0.80 | 0.83 | 1.00 | 1.00 | 0.90 |
Note: SIPS, Structured Interview for Prodromal Syndromes; EU, Emory University; HU, Harvard University; UCLA, University California Los Angeles; UCSD, University of California San Diego; UNC, University of North Carolina; UT, University of Toronto; ZHH, Zucker Hillside Hospital.
Agreement expressed as kappa values23 < 0.40, poor; 0.40–0.59, fair; 0.60–0.74, good; ≥ 0.75, excellent.
Developing an Omnibus Assessment Protocol
Because the individual projects were originally designed as independent investigations, baseline evaluation and follow-up procedures differed among the studies. The diversity of variables and instruments required PIs to establish an omnibus assessment protocol for NAPLS, and then to map already acquired data onto the new assessment scheme. Eighteen variable domains were identified: 5 classes of demographic and developmental history variables, 6 classes of baseline functioning variables, and 7 classes of longitudinal outcome variables (see Tables 3 and 4). PIs compared the range of assessment instruments for all variable domains to identify commonalities in measurement procedures, or when differences were observed, to suggest options for harmonizing already collected data. There were 3 levels of methodological consistency within the 18 variable domains. In 6 instances, measurement strategies were nearly identical across NAPLS sites. Standardized scoring procedures, with acceptable methods for training and establishing interrater reliability, were the norm for the SIPS, Structured Clinical Interview for DSM, and Kiddie-Schedule for Affective Disorders and Schizophrenia (SADS) diagnostic interviews and for the Cannon-Spoor Premorbid Adjustment Scale.12–14 The highly structured nature of these instruments minimizes the likelihood of measurement error related to site differences and increases confidence that these data can be aggregated.
Table 3.
Methodological Consistency in 11 Baseline Variables and Percent of Missing Data at Baseline
|
Demographic/Historical Variables |
Baseline Functioning Variables |
||||||||||
| Age, Sex, Race, etc. (n = 7) | Family History (n = 8) | Life Events (n = 26) | Premorbid Adjustment (n = 4) | Lifetime Psychiatric Treatment (n = 72) | Prodromal Symptoms (n = 73) | DSM-IV Diagnoses (n = 18) | Alcohol/Substance Abuse (n = 10) | Current Psychiatric Treatment (n = 18) | Social/School/Work Functioning (n = 24) | Cognitive Performance (n = 13) | |
| Methodological consistency across sites at baseline | |||||||||||
| Nearly identical methods | ✓ | ✓ | ✓ | ||||||||
| Consistency across ≥4 sites | ✓ | ✓ | ✓ | ||||||||
| Inconsistency across sites | ✓ | ✓ | ✓ | ✓ | |||||||
| Percentage of missing data in the 11 classes of variables assessed at baseline | |||||||||||
| % Missing data | 4 | 14 | 13 | 23 | Medication: 3 | 13 | Psychosis: 0 | 12 | Medication: 14 | 11 | 21a |
| Other axis I: 25 | Psychosocial: 23 | ||||||||||
| Psychosocial: 18 | Axis II: 35 | ||||||||||
Note: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Missing data rate is based on number of subjects with missing IQ data.
Table 4.
Methodological Consistency Across Sites for 7 Classes of Variables Assessed Longitudinally
| Longitudinal Outcome Variables |
|||||||
| Methodological Consistency Across Sites | Intervening Life events (n = 26) | Alcohol/ Substance Abuse (n = 10) | Intervening Psychiatric Treatment (n = 18) | Social/School/Work Functioning (n = 24) | Prodromal Symptoms (n = 73) | DSM-IV Diagnoses (n = 18) | Cognitive Performance (n = 13) |
| Nearly identical methods | ✓ | ✓ | |||||
| Consistency across ≥4 sites | ✓ | ✓ | |||||
| Inconsistency across sites | ✓ | ✓ | ✓ | ||||
Note: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Methodological consistency was high, but not perfect, for another 5 variable domains. Data collection was identical in at least half of NAPLS sites for lifetime psychiatric treatment, substance abuse, and current treatments. For these domains, centers that differed in data collection methods agreed to recode already collected data onto the majority instruments. PIs performed item-by-item comparisons between majority and minority measures in order to develop valid algorithms for recoding data. When the wording of items or scoring differences prohibited direct substitution of items, sites consulted informants' original interview responses to complete the majority assessment instrument. Missing data are infrequent for these variables in the combined NAPLS data set (see Table 3), suggesting that the data translation strategy was largely successful.
Assessment procedures differed widely for the remaining variable domains. Within 5 of these categories (family history of mental illness; stressful life events before and after baseline; social, school, and work functioning), it was necessary to generate new measures that could be applied retrospectively across sites. For family history, sites recorded whether psychotic or nonpsychotic illnesses had been reported for subjects' first- and second-degree relatives. For stressful life events, the sites had used a range of published measures.15–17 PIs compared all scales and drew upon common elements to create a 25-item measure of life events in the areas of school/work, family disruption, personal and relationship problems, and traumatic events or natural disasters. In addition, each site reviewed all original documentation and consulted with relevant clinical and research staff to determine whether events occurred in childhood, early adolescence, late adolescence, or adulthood.
Measures of social and instrumental role functioning were particularly variable across sites and it became apparent that most established measures of functioning were not particularly suited to this population. The article by Cornblatt and Cannon in this issue18 illustrates how global measures of social functioning and instrumental role performance were developed to overcome these limitations of existing instruments for the NAPLS project and how raters were trained to apply these scales to source materials.
Cognitive performance variables presented unique challenges to the omnibus assessment protocol. A total of 68 different neurocognitive measures derived from 40 separate tests were used in the individual NAPLS projects, with varying degrees of overlap observed between the sites. Decisions regarding which tests, or components of tests, to include in the omnibus protocol were made on the basis of (1) representation across 4 or more sites, (2) comparability of test versions, administration procedures, and scoring, and/or (3) coverage of presumed areas of separable cognitive impairment in schizophrenia.19 In all, 13 cognitive variables derived from 8 tests were selected for the cross-site assessment battery, representing the domains of IQ, estimated academic achievement, attention/vigilance, speed of processing, working memory, verbal learning and memory, visual learning and memory, reasoning and problem solving, and motor functioning.
In sum, 273 variables within 11 baseline domains and 182 variables within 7 follow-up domains are included in the omnibus assessment protocol. Each variable is summarized in the comprehensive NAPLS assessment codebook, assuring a standardized approach to NAPLS data recoding and aggregation. Table 3 summarizes missing data for each baseline variable domain.
Translating Data to the Omnibus Assessment Protocol
A versatile data integration program with appropriate safeguards for error was created by UCLA to convert site-specific data to the omnibus format. Data recoding and translation began in July 2005 and was completed in February 2006 for baseline and November 2006 for follow-up data. Site-specific data sets were combined at UCLA for baseline data and at Toronto for follow-up data. Appropriate cleaning and checking procedures were subsequently conducted.20 The cleaned and checked baseline database was distributed to PIs in October 2006 and the follow-up data set in March 2007.
Eligible Subjects
Inclusion criteria are intentionally broad for the NAPLS project as our goal is to maximize the number of subjects eligible for the collaborative project. Consequently, any subject with a valid SIPS diagnosis at initial assessment can be admitted into the baseline database. Among these individuals, any subject who has also completed at least 1 subsequent clinical evaluation (6, 12, 18, 24, or 30 months) is included in follow-up analyses. Beyond these minimal requirements, there are no restrictions on which individuals can be included in the federated NAPLS database.
Results
A total of 888 subjects enrolled in North American prodromal schizophrenia research projects between the years 1998 and 2005 are included in the baseline database. Among this group, 651 subjects have sufficient data for planned outcome analyses. The majority of subjects (n = 801) had been recruited into longitudinal assessment studies with naturalistic designs; approximately 10% (n = 87) had participated in medication trials, with random assignment to either placebo or active treatment. For the purpose of this article, the NAPLS sample is organized into 6 nonoverlapping groups that reflect varying degrees of psychosis vulnerability (see Table 5). Group assignments are made on the basis of subjects' SIPS responses during the initial diagnostic interview, information about family history of psychotic disorders, and the presence or absence of Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) schizotypal personality disorder at the time of index evaluation.
Table 5.
Criteria for Subjects' Group Assignment
| Study Group | N | Assignment Criteria |
| CHR | 370 | Subject meets severity, onset, and duration threshold of COPS |
| GHR | 65 | Subject does not meet criteria for CHR |
| Subject does not display psychotic symptoms | ||
| One or more first-degree relatives with a diagnosis of schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, brief psychotic disorder, psychotic disorder not otherwise specified, major depressive disorder with psychotic features, or bipolar disorder with psychotic features | ||
| SPD | 56 | Subject does not meet criteria for CHR or GHR |
| Subject does not display psychotic symptoms | ||
| Subject meets DSM-IV criteria for schizotypal personality disorder | ||
| POPS | 28 | Subject meets criteria for the presence of psychotic symptoms24 |
| HSC | 174 | Subject presented for help at a prodromal psychosis research clinic |
| Subject does not meet criteria for CHR, GHR, SPD, or POPS | ||
| NPC | 195 | Subject was recruited as a normal control subject |
| Subject does not meet criteria for CHR, GHR, SPD, POPS, or HSC |
Note: CHR, clinical high risk; COPS, Criteria of Prodromal Symptoms; GHR, genetic high risk; SPD, schizotypal personality disorder; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition;POPS, psychotic symptoms; HSC, help-seeking controls; NPC, nonpsychiatric controls.
Individuals believed to be at heightened clinical risk for psychosis make up the largest subgroup in the database (n = 370). These were all help-seeking individuals who presented for evaluation and treatment at established clinical and psychiatric settings. The Criteria of Prodromal Syndromes (COPS; see Table 6) describe 3 pathways to a SIPS prodromal syndrome diagnosis: (1) presence of attenuated positive symptoms such as perceptual abnormalities, suspiciousness, and unusual ideas (Attenuated Positive Symptom Syndrome [APSS]), (2) genetic risk for psychosis coupled with deterioration in global functioning (Genetic Risk and Deterioration Syndrome [GRDS]), and (3) intermittent psychotic symptoms that are recent, brief in duration, and not seriously disorganizing or dangerous (Brief Intermittent Psychotic Syndrome [BIPS]). Most subjects in the NAPLS clinical high-risk (CHR) group reported APSS only (349; 94.3%). BIPS and GRDS diagnoses were far less common (2.9 and 0.6%, respectively), and multiple prodromal diagnoses were equally rare (2.2%).
Table 6.
| 1. Attenuated Positive Symptom Syndrome |
| 1.1. Severity rating of moderate (3), moderately severe (4), or severe but not psychotic (5) on any one of the 5 SIPS positive symptoms |
| 1.2. Symptom occurs at above severity level at an average frequency of at least once per week in the past month |
| 1.3. Symptom must have begun in the past year or currently rates at least one scale point higher than rated 12 mo previously |
| 2. Genetic Risk and Deterioration Syndrome |
| 2.1. First-degree relative with psychosis or patient with schizotypal personality disorder |
| 2.2. 30% drop in Global Assessment of Functioning score compared with that 1 y ago, sustained over the past month |
| 3. Brief Intermittent Psychotic Syndrome |
| 3.1. Severity rating of psychotic intensity (6) on any one of the 5 SIPS positive symptoms |
| 3.2. Symptom is present at least several minutes per day at a frequency of at least once per month |
| 3.3. Symptom must have reached a psychotic intensity in the past 3 mo |
| 3.4. Symptom is not seriously disorganizing or dangerous |
| 3.5. Symptom does not last for more than 1 h/d at an average frequency of 4 d/wk over 1 mo |
Note: SIPS, Structured Interview for Prodromal Syndrome; BIPS, Brief Intermittent Psychotic Syndrome.
Other at risk groups include individuals with 1 or more first-degree relatives who are diagnosed with any form of psychotic illness (n = 65), persons who meet DSM-IV criteria for schizotypal personality disorder (n = 56), and patients with recently developed psychotic symptoms (n = 28). Additional comparison groups include help seekers who fail to meet criteria for elevated clinical risk by COPS (n = 174) and nonpsychiatric controls (NPCs) (n = 195). Because help seekers report a plethora of worrisome clinical symptoms, they are included to test the sensitivity and specificity of current prodromal diagnostic criteria. NPC subjects provide benchmark information regarding normal developmental processes in adolescents and young adults.
Table 7 compares subjects in the 3 largest NAPLS subgroups on selected demographic, instrumental functioning, and diagnostic variables. The CHR and help-seeking control (HSC) samples are similar in gender and race but differ in age and schooling. Compared with other subjects, members of the HSC group are significantly younger, have completed fewer years of education, and are more likely to be enrolled in school at the time of initial assessment. NPCs are more diverse in terms of gender and race and have completed more years of formal education. The 3 groups are similar in socioeconomic background (measured by level of parental education) and competitive employment at baseline.
Table 7.
Group Comparisons on Selected Demographic, Instrumental Functioning, and Diagnostic Variables
| Dependent Measures | Comparison Groups |
|||
| Clinical High Risk, N = 370 | Help-Seeking Controls, N = 174 | Nonpsychiatric Controls, N = 195 | Overall F and χ2 Values | |
| Males (%) | 61.9† | 64.7† | 45.9‡ | χ2(2, 739) = 17.28** |
| Mean age (SD) | 18.2 (4.7)† | 16.1 (3.5)‡ | 18.7 (4.5)† | F(2, 736) = 18.56** |
| Race (%) | χ2(4, 723) = 19.70* | |||
| White | 79.8† | 72.1†‡ | 64.4‡ | |
| African American | 9.5† | 16.9†‡ | 15.5‡ | |
| Multiracial/other | 10.6† | 11.0†‡ | 20.1‡ | |
| Parental education (%) | NS | |||
| ≥ College degree | 66.3 | 67.1 | 74.6 | |
| High school graduate | 27.9 | 29.7 | 20.4 | |
| < High school graduate | 5.7 | 3.2 | 5.0 | |
| Mean highest grade (SD) | 10.3 (3.0)† | 8.8 (2.5)‡ | 11.3 (3.4)§ | F(2, 725) = 30.96** |
| School/work status (%) | ||||
| Current school enrollment | 69.3† | 87.8‡ | 70.8† | χ2(2, 735) = 22.30** |
| Current Full-time or Part-time work | 21.8 | 13.8 | 15.5 | NS |
| DSM-IV diagnosis (%) | ||||
| Psychotic disordera | 0 | 0 | 0 | NS |
| Mood disorderb | 34.9† | 20.4† | 0.0‡ | χ2(2, 496) = 56.93** |
| Anxiety disorderc | 30.4† | 24.8† | 0.0‡ | χ2(2, 477) = 45.01** |
| Alcohol abuse/dependence | 15.3† | 16.1† | 3.5‡ | χ2(2, 660) = 16.93** |
| Drug abuse/dependence | 19.5† | 12.2† | 0.6‡ | χ2(2, 660) = 35.85** |
Note: NS, not signicifcant; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Schizophrenia, schizoaffective disorder, schizophreniform disorder, delusional disorder, brief psychotic disorder, psychotic disorder not otherwise specified, major depressive disorder with psychotic features, or bipolar disorder with psychotic features.
Major depression, dysthymia, or bipolar disorder.
Panic disorder, agoraphobia, social phobia, simple phobia, obsessive compulsive disorder, or generalized anxiety disorder.
*P < .001, **P < .0001 for all group comparisons; means and percentages not sharing the same subscript differ significantly from one another (Bonferroni analysis, P < .002).
DSM-IV psychotic disorders were not observed among CHR, HSC, and NPC subjects. Mood and anxiety disorders were prevalent in both clinical samples but were absent among NPC subjects. Alcohol-related diagnoses were equivalent in the CHR and HSC groups, but substance abuse/dependence was somewhat more likely among CHR subjects (χ2 = 3.969, [1, 490], P < 0.05). In general, alcohol and drug problems were rare among NPC subjects.
Discussion
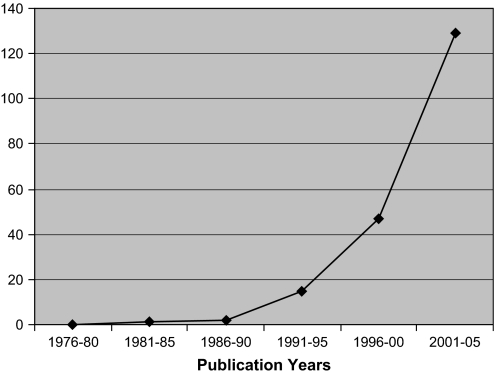
The scientific literature regarding the prodrome to psychosis is expanding rapidly, with 176 of 193 peer-reviewed articles on the topic published since 1995 (see Figure 1). Most empirical studies from this literature reflect a single-site, single-investigator approach to science that is well suited for studying high-prevalence disorders but are less effective in CHR research, in which subjects are more difficult to locate and recruit. A different investigative strategy may be required to accelerate scientific progress in understanding the earliest stages of psychotic illness. Integrated multisite research programs represent 1 alternative model for acquiring large samples of at risk individuals and following them over time. Interest in this approach is growing, as evidenced by both the NAPLS project and a recent article describing the multisite European Prediction of Psychosis Study (EPOS).21
Fig. 1.
Number of peer-reviewed articles published on the prodrome to psychosis, 1976–2005.
The present article focuses on the mechanics of establishing a viable consortium among research projects originally conceived as independent scientific investigations. The existence of the federated NAPLS database proves that effective cross-site collaboration is possible. Success ultimately depended on a number of structural and procedural factors, including early administrative oversight by NIMH program staff, a consistent schedule of contact between PIs, action plans and timelines for completing tasks, and a consensus building approach to decision making. NIMH leadership served as an early catalyst for cooperation by smoothing over preexisting differences among PIs, highlighting commonalities in research goals and methods, and fostering teamwork. A democratic governing structure emerged during the second year of operation and continues to the present. NAPLS is now a self-governing enterprise, with minimal Federal involvement in managing the project.
While a retrospectively integrated data set such as NAPLS can provide valuable data on common and reliably collected measures, there are limitations to this approach. For example, neurocognitive measures may lack standard administration across sites, with a consequent penalty in error variance. Other limitations include the exclusion of subjects who meet CHR criteria but are not help seeking, such as those identified in epidemiological studies who report psychotic like experiences.22
To our knowledge, the NAPLS longitudinal database represents the largest sample of prospectively followed at risk subjects worldwide. The database presents opportunities to explore many fundamental questions related to prodromal psychosis, including the descriptive phenomenology of currently accepted diagnostic criteria, conversion rates over a 30-month period, predictors of psychosis onset and functional disability, and the impact of early treatment on the course of prodromal symptoms. Articles on each of these topics are forthcoming. The EPOS project21 is designed to address similar questions using comparable methods for ascertaining at risk subjects and following them longitudinally. We anticipate that findings from these 2 large-scale investigations will rapidly advance our knowledge regarding the symptomatic, behavioral, neurocognitive, and environmental events proximal to the onset of psychosis and taken together and will set the direction for the next generation of prodromal research studies.
Acknowledgments
The authors acknowledge the substantial contributions of Jennifer Johnson (UCLA), Diane Kirsopp (UT), Anthony Giuliano (HU), and Roy Money (Yale) to the creation of the federated NAPLS database described in this article. The views expressed are those of the authors and do not necessarily reflect the official views of the NIMH, the National Institutes of Health, or any other branch of the U.S. Department of Health and Human Services.
Appendix
NAPLS Group
Jean Addington, Diane Kirsopp, Ivana Furimsky, Irvine Epstein, and Robert Zipursky (Toronto, Canada); Donald Addington and Anna Gresko (Calgary, Canada); Kristin Cadenhead, Kathleen Shafer, Iliana Marks, Katherine Seeber, Nasra Harou, and Karin Kristensen (UCSD); Tyrone Cannon, Jennifer Johnson, Carrie Bearden, Mary O'Brien, Melita Daley, Tara Niendam, and Jamie Zinburg (UCLA); Barbara Cornblatt, Christopher Smith, Andrea Auther, Pradeep Nagachandran, and Joshua Biener (ZHH); Diana Perkins, Johanna Boobas, Jennifer Nieri, and Karen Graham (UNC); Larry Seidman, Ming Tsuang, Anthony Giuliano, Eric Meyer, and Lynda Tucker (HU); Elaine Walker and Shivali Dhruv (EU); Scott Woods, Thomas McGlashan, Tandy Miller, Roy Money, and Philip Markovich (Yale University); and Robert Heinssen, (NIMH).
References
- 1.Tan HY, Ang YG. First-episode psychosis in the military: a comparative study of prodromal symptoms. Aust N Z J Psychiatry. 2001;35:512–519. doi: 10.1046/j.1440-1614.2001.00912.x. [DOI] [PubMed] [Google Scholar]
- 2.McGlashan TH. A selective review of recent North American long-term followup studies of schizophrenia. Schizophr Bull. 1988;14:515–542. doi: 10.1093/schbul/14.4.515. [DOI] [PubMed] [Google Scholar]
- 3.McGlashan TH. Early Detection and Intervention of Schizophrenia: Rationale and Research. Br J Psychiatry. 1998;172:3–6. [PubMed] [Google Scholar]
- 4.Heinssen RK, Cuthbert BN, Breiling J, Colpe L, Dolan-Sewell R. Overcoming barriers to research in early serious mental illness: Issues for future collaboration. Schizophr Bull. 2003;29:737–746. doi: 10.1093/oxfordjournals.schbul.a007043. [DOI] [PubMed] [Google Scholar]
- 5.Cannon TD, van Erp TG, Bearden CE, et al. Early and late neurodevelopmental influences in the prodrome to schizophrenia: contributions of genes, environment, and their interactions. Schizophr Bull. 2003;29:653–669. doi: 10.1093/oxfordjournals.schbul.a007037. [DOI] [PubMed] [Google Scholar]
- 6.Nass SJ, Stillman BW. Large Scale Biomedical Science:Exploring Strategies for Exploring Future Research. Washington, D.C.: National Acadamies Press; 2003. [Google Scholar]
- 7.McGlashan TH, Miller TJ, Woods SW. Pre-onset detection and intervention research in schizophrenia psychoses: current estimates of benefit and risk. Schizophr Bull. 2001;27:563–570. doi: 10.1093/oxfordjournals.schbul.a006896. [DOI] [PubMed] [Google Scholar]
- 8.Miller TJ, McGlashan TH, Rosen JL, et al. Prospective diagnosis of the initial prodrome for schizophrenia based on the structured interview for prodromal syndromes: preliminary evidence of interrater reliability and predictive validity. Am J Psychiatry. 2002;159:863–865. doi: 10.1176/appi.ajp.159.5.863. [DOI] [PubMed] [Google Scholar]
- 9.Miller TJ, McGlashan TH, Rosen JL, et al. Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophr Bull. 2003;29:703–715. doi: 10.1093/oxfordjournals.schbul.a007040. [DOI] [PubMed] [Google Scholar]
- 10.Miller TJ, Zipursky R, Perkins DO, et al. A randomized double blind clinical trial of olanzapine vs placebo in patients at risk for being prodromally symptomatic for psychosis: II recruitment and baseline characteristics of the “prodromal” sample. Schizophr Res. 2003 doi: 10.1016/s0920-9964(02)00440-1. [DOI] [PubMed] [Google Scholar]
- 11.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Measur. 1960;20:37–46. [Google Scholar]
- 12.Cannon-Spoor H, Potkin S, Wyatt R. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 13.Orvaschel HP-AJ. Schedule for Affective Disorders and Schizophrenia for School-Aged Children- Epidemiologic Version. Fort Lauderdale, FL: Centre for Psychological Studies, Nova Southeastern University; 1994. [Google Scholar]
- 14.Williams J, Gibbon M, First M, Spitzer R, Davies M, et al. The structured clinical interview for DSM-III-R (SCID): multisite test-retest reliability. Arch Gen Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- 15.Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the Peri Life Events Scale. J Health Soc Behav. 1978;19:205–229. [PubMed] [Google Scholar]
- 16.Goodman LA, Corcoran C, Turner K, Yuan N, Green BL. Assessing traumatic event exposure: general issues and preliminary findings for the Stressful Life Events Screening Questionnaire. J Trauma Stress. 1998;11:521–542. doi: 10.1023/A:1024456713321. [DOI] [PubMed] [Google Scholar]
- 17.Gray MJ, Litz BT, Hsu JL, Lombardo TW. Psychometric properties of the life events checklist. Assessment. 2004;11:330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 18.Cornblatt B, Neindam T, Auther A, Smith C, Johnson JCT. Validation of two new measures of functional outcome in the schizophrenia prodrome. Schizophr Bull. 2007 [Google Scholar]
- 19.Nuechterlein KH, Barch DM, Gold JM, Goldberg TE, Green MF, Heaton RK. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72:29–39. doi: 10.1016/j.schres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Wisniewski SR, Leon AC, Otto MW, Trivedi MH. Prevention of missing data in clinical research studies. Biol Psychiatry. 2006;59:997–1000. doi: 10.1016/j.biopsych.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 21.Klosterkotter J, Ruhrmann S, Schultze-Lutter F, et al. The European Prediction of Psychosis Study (EPOS): integrating early recognition and intervention in Europe. World Psychiatry. 2005;4:161–167. [PMC free article] [PubMed] [Google Scholar]
- 22.van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss 1969 Revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 23.Cicchetti D, Sparrow SA. Developing criteria for establishing interrater reliability of specific items: applications to assessment of adatptive behavior. Am J Ment Defic. 1981;86:127–137. [PubMed] [Google Scholar]
- 24.McGlashan TH, Zipursky R, Perkins DO, et al. The PRIME North America randomized double blind clinical trial of olanzapine vs placebo in patients at risk for being prodromally symptomatic for psychosis: I study rationale and design. Schizophr Res. 2003;61:7–18. doi: 10.1016/s0920-9964(02)00439-5. [DOI] [PubMed] [Google Scholar]