Abstract
AIM
To describe nation-wide secular trends in statin use.
METHODS
Reimbursed prescriptions for lipid lowering drugs between 1995 and 2005 in Finland were retrieved from the nation-wide Prescription Register. The 1 year prevalence and incidence of statin use stratified by gender and age of users were measured for each calendar year. The relative changes (RR) in the incidence and the prevalence were calculated by using the year 1995 as a reference.
RESULTS
The 1 year prevalence increased 11-fold (95% confidence interval 11.2, 11.5), i.e. from 7.8 per 1000 inhabitants in 1995 to 88.9 in 2005. The incidence increased five-fold (95% CI 4.9, 5.1) from 355 per 100 000 inhabitants to 1772 during the respective years. The prevalence and incidence were the highest among persons aged 65−74 years. The largest relative increase in incidence was found among those aged ≥ 75 years, in both females (RR 14.1, 95% CI 13.0, 15.3) and males (RR 14.0, 95% CI 12.5, 15.7). Since 2002 the prevalence has been higher among females (P < 0.05).
CONCLUSIONS
As statin use has increased particularly among the elderly, further studies on the benefits in real life situation are needed in this age group.
WHAT IS ALREADY KNOWN
Statin use has increased in western societies since the 1990s.
Efficacy of statins in the prevention of coronary heart diseases has been clearly documented in the general population but only recently in elderly persons.
WHAT THIS STUDY ADDS
Since 1995 the use of statins has clearly shifted towards the elderly in Finland.
At the beginning of the 11 year follow-up the prevalence of statin use was higher among males than females but since 2002 the prevalence has been higher among females.
Keywords: hydroxymethylglutaryl-CoA reductase inhibitors, incidence, prevalence, statins, utilization
Introduction
The use of lipid-lowering drugs (LLDs), mainly 3-hydroxy-3-methylglutaryl coentzyme A reductase inhibitors (statins) has increased exponentially in western societies [1, 2] since the publication of the Scandinavian Simvastatin Survival Study (4S) in 1994 [3]. Publication of other benchmarking trials in the late 1990s [4–6] further stimulated the use. The increase has been seen in pharmacy based registers [7–9], surveys [10, 11] and administrative databases [8, 12–16] including drug consumption statistics [17]. Despite the increase in statin use, data on its prevalence, and especially on new users categorized by the demographic characteristics are scarce in general population [2, 9, 13–15]. Furthermore, the generalizability of previous utilization studies is limited due to the small size or restrictions of the study populations, or the time windows included in the studies: most of them describe statin use during the 1990s.
As in other western societies, statin use in Finland has also increased exponentially [17]. In 2005 the total consumption was 94.9 defined daily doses (DDD) per 1000 inhabitants a day [18]. Simvastatin has been the most used statin since 1997; in 2005 it accounted for 40% of statin consumption [18]. The use of atorvastatin has steadily increased since its introduction in 1998, and atorvastatin accounted for 34% of statin consumption in 2005. Rosuvastatin, pravastatin, fluvastatin and lovastatin are clearly smaller players in the market, each of them accounting for less than 10% of the consumption [18].
The comprehensive nation-wide drug reimbursement registers make Finland suitable for studies on drug utilization patterns. The aim of the present study was to evaluate the use of statin therapy in the Finnish population between the years 1995 and 2005. We analyzed trends of prevalence and incidence of statin use separately for both genders in various age categories.
Methods
Data source
The data were based on the national Prescription Register managed by the Social Insurance Institution. All permanent residents living in community are included in the Register. In 2003, 94.6% of the consumption for lipid lowering drugs (consisting mainly statins) outside institutions was covered by the Register (Martikainen J, the Social Insurance Institution, personal information). In this study a prescription refers to the amount of reimbursable medicine which consists of one preparation purchased during one transaction from a pharmacy. Reimbursed medicines can be supplied to a patient for no longer than 3 months per purchase. Consequently, a 1 year therapy issued by a physician contributes at least four prescriptions. The reimbursement register covers purchases that meet the minimum deductible limit, i.e. 8.41 euros until 2002 and 10 euros thereafter until 2006. All statins are available on prescription only. During the study period all statin prescriptions were reimbursable, and with a minor exception their purchases were also registered. After the introduction of generic substitution in 2003 a limited number of low-price simvastatin packages remained below the deductible limit in 2004–2005 and were registered only if the patient purchased other reimbursable medicines at the same transaction.
The data on the population were collected by the Social Insurance Institution. During the study period the population increased from 5.1 to 5.3 million.
Prescriptions
The following LLD prescriptions were retrieved using the corresponding Anatomical Therapeutic Chemical code (ATC) presented by the WHO [19]: simvastatin (C10AA01), lovastatin (C10AA02), pravastatin (C10AA03), fluvastatin (C10AA04), atorvastatin (C10AA05), cerivastatin (C10AA06), rosuvastatin (C10AA07), clofibrate (C10AB01), bezafibrate (C10AB02), gemfibrozil (C10AB04), fenofibrate (C10AB05), cholestyramine (C10AC01), colestipol (C10AC02) and ezetimibe (C10AX09). These ATC codes were applied for the years between 1996 and 2005 [19]. For the years 1994 and 1995 respective ATC codes valid for that time were used [20]. The LLD users were identified by a unique social security number linked to each prescription in the register. Reimbursed LLD prescriptions were further linked with the date of the purchase, the gender and the age of the patient in years at the end of each calendar year.
Definitions
The 1 year period prevalence of statin use was calculated from the number of persons who redeemed at least one reimbursed statin prescription during a calendar year divided by the number of inhabitants in Finland at the end of the respective year. The 1 year incidence of statin use was defined as the number of initiators, new users in the respective year divided by the number of inhabitants excluding those who had redeemed at least one statin prescription during the previous year. The prescription data in 1994 were used to ensure that new users of statins in 1995 had not redeemed any statins during the previous year.
The genders were analyzed separately. Both the prevalence and the incidence were calculated for patients aged 44 years or less, for those aged 45−54, 55−64, 65−74 and 75 years or more. The age and gender specific population was used in the denominator where appropriate.
Statistical analysis
To analyze the relative changes in statin use, the rate ratios (RR) of the 1 year prevalence in each year in relation to the reference year 1995 and the respective RRs of incidences and their 95% confidence intervals were calculated using the Poisson regression. A two-tailed P value < 0.05 was regarded as statistically significant. The crude prevalence and incidence in each year were standardized according to the age and gender specific population in 2000. The statistical analyses were performed using SAS version 9.1 (SAS Institute Inc., Cary, NC).
Results
After the exclusion of persons with incomplete data (n = 106) a total of 603 866 persons who had received at least one prescription for a LLD were identified. Among these, 590 907 persons received at least one prescription for a statin. The number of statin users increased from 40 089 (0.8% of the population) in 1995 to 467 168 (8.9%) in 2005. The number of users of other LLDs than statins decreased slightly from 8046 to 7314 during the respective years. In the following only data on statins are presented.
The median age of the users increased from 62 to 66 years during the 11 year observation period (Table 1). Among the users in 2005 (467 168 persons) the largest group was males younger than 65 years who accounted for 33.3% of the users, and the second largest group was females ≥ 65 years of age with the 26.5% share.
Table 1.
1 year prevalence of statin use (at least one reimbursed statin prescription per year); users per 1000 inhabitants in Finland and the median age of all users in respective years
| Both genders | Males* | Females* | Median age, year (interquartile range) | ||
|---|---|---|---|---|---|
| 1995 | 7.8 | 8.8 | 6.9 | 62 | (54–68) |
| 1996 | 12.8 | 13.9 | 11.7 | 63 | (55–69) |
| 1997 | 18.4 | 19.4 | 17.4 | 63 | (56–70) |
| 1998 | 24.3 | 25.2 | 23.4 | 64 | (56–70) |
| 1999 | 32.4 | 33.1 | 31.7 | 64 | (56–71) |
| 2000 | 41.7 | 41.8 | 41.6 | 65 | (56–72) |
| 2001 | 50.4 | 50.2 | 50.6 | 65 | (56–72) |
| 2002 | 58.6 | 58.3 | 58.8 | 65 | (57–73) |
| 2003 | 67.6 | 67.3 | 68.0 | 65 | (57–73) |
| 2004 | 79.2 | 78.5 | 80.0 | 65 | (57–73) |
| 2005 | 88.9 | 88.5 | 89.3 | 66 | (57–74) |
The difference between males and females P < 0.05 in all other years but in 2000 and 2001.
Prevalence
The 1 year prevalence of statin use increased from 7.8 per 1000 inhabitants in 1995 to 88.9 in 2005 (RR 11.3, 95% CI 11.2, 11.5). Among females, the prevalence increased from 6.9 per 1000 female inhabitants to 89.3, and among males from 8.8 to 88.5 per 1000 male inhabitants during the respective years (Table 1). From 1995 to 1999 the prevalence of statin use was significantly higher among males than among females (P < 0.05) but since 2002 the situation has reversed: the prevalence was higher among females (P < 0.05).
The direct standardization procedure according to the population in 2000 did not affect the results and hence the crude period prevalence is presented (Table 1, Figure 1).
Figure 1.
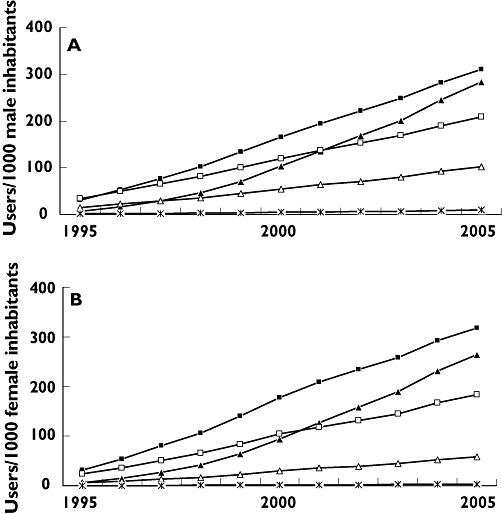
1 year prevalence of statin use stratified by age among males (A) and females (B) in Finland. >75 years (▴); 65–74 years (▪); 55–64 years (□); 45–54 years (▵); <44 years ( )
)
Among both genders the prevalence increased in all age categories during the 11 year follow-up (Figure 1). The relative increase was most prominent among those aged at least 75 years (RR 40.6, 95% CI 37.5, 43.9 for males and RR 40.2, 95% CI 38.1, 42.4 for females). The gender specific 1 year prevalence in this age category increased from 7.0 per 1000 male inhabitants in 1995 to 283.3 in 2005 and from 6.7 per 1000 female inhabitants to 264.4, respectively.
Incidence
The overall incidence of statin use increased from 355 per 100 000 inhabitants in 1995 to 1772 in 2005 (RR 5.0, 95% CI 4.9, 5.1). Among females, the incidence increased from 312 per 100 000 female inhabitants to 1732, and among males from 399 to 1815 per 100 000 male inhabitants. In 1995 the 1 year incidence was higher among males than females (RR 1.3, 95% CI 1.2, 1.3) but since 1996 no significant difference was observed. Persons aged between 65 and 74 years showed the highest incidence in both genders over the whole observation period (Figure 2). Direct standardization to the year 2000 population did not significantly affect the incidence figures either.
Figure 2.
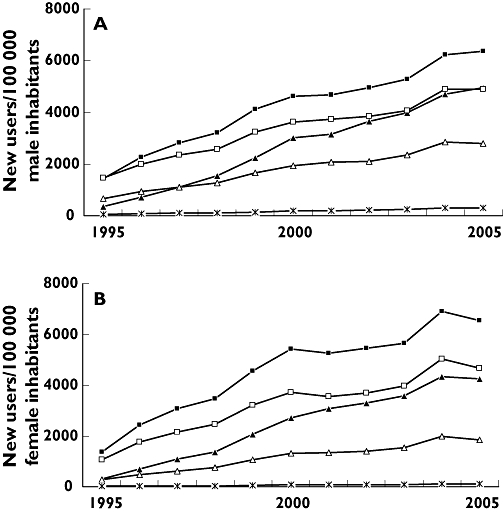
1 year incidence of statin use stratified by age among males (A) and females (B) in Finland. >75 years (▴); 65–74 years (▪); 55–64 years (□); 45–54 years (▵); <44 years ( )
)
In concordance with prevalence, the relative increase in the number of new users was the highest among persons aged at least 75 years (RR 14.0, 95% CI 12.5, 15.7 for male users and RR 14.1, 95% CI 13.0, 15.3 for female users). The increase in the incidence among the oldest persons was from 353 per 100 000 male inhabitants in 1995 to 4948 in 2005, and from 301 per 100 000 female inhabitants to 4 252, respectively.
All values for prevalence and incidence for both genders in various age categories are presented in the electronic supplementary data online.
Discussion
Among the whole population of Finland the relative increase of the prevalence of statin use was 11-fold between 1995 and 2005. The most evident, 40-fold, increase was observed among persons aged at least 75 years. The relative increase of the incidence was five-fold among the whole population. In accordance with the highest relative change of the prevalence, the largest (14-fold) increase of the incidence was observed among the oldest persons. In absolute terms, both the highest prevalence and incidence of statin use were found among persons aged between 65 and 74 years; 31% of the persons in this age category had used statins in 2005. Only small differences in the statin use between the genders were found.
The Prescription Register covers every permanent resident of Finland receiving statin treatment in open care. The further strength of our study was the low turnover of the population. However, persons staying permanently in public institutional care are not entitled to drug reimbursement, and were thus not included in our study. Therefore, we may have underestimated statin use especially among the elderly. Furthermore, the Prescription Register does not cover non-reimbursed medicines of low-price packages. During 1994−2003 all statin prescriptions were registered, but after the introduction of generic substitution in 2003 prices of a limited number of simvastatin packages fell below the reimbursement level in 2004−2005. Thus, the plateau observed in the incidence level in 2005 may be more of a reflection of the decreased coverage of statins in the Register than a real decrease in the number of new users.
The observed increase in prevalence among those aged at least 75 years partly reflects a continuum of statin therapy initiated at earlier ages. However, the relative increase in the number of new users among the oldest population, already observed during the 1990s, is concordant with the transition of coronary heart disease (CHD) prevalence towards the oldest group. In Finland the prevalence of CHD has decreased among persons younger than 65 years, and increased during the past 20 years among those aged more than 75 years [21]. Consequently, in 2000 the most dominant group of patients with CHD was females aged ≥ 75 years [21].
The increase in the prevalence of statin use also reflects the increase in the morbidity of CHD. The ageing of the Finnish population has promoted the increase in the total estimated number of persons with established CHD by 18% during the past 20 years [21] although the incidence of first myocardial infarction (MI) decreased between 1991 and 2001 [22]. The reduction in MI incidence and the shift of CHD morbidity towards those aged over 75 years suggests successful primary prevention among the younger population.
Large statin trials conducted during the 1990s showed clear evidence on statin efficacy in the prevention of CHD events [3–6]. These trials were not specifically conducted among the elderly though data from sub-analyses revealed efficacy of statin treatment also among those aged up to 75 years [3, 5]. The first trials showing efficacy among persons aged over 75 years were not published until 2002 [23, 24] and the respective recommendations were incorporated into the Finnish evidence-based clinical guidelines on dyslipidaemia 2 years later [25]. Thus, the clinical trial evidence on the younger population present in the 1990s may have already been extrapolated to elderly patients by physicians before 2002.
A cross-sectional survey conducted among Finns in 2000 showed that the percentage of males with CHD or with low density lipoprotein values higher than 3.0 mmol l–1 (116 mg dl–1) was significantly higher than that for females [26]. Hence, we assumed that males would use statins more frequently than females, but after 1999 no remarkable gender differences in prevalence existed (Table 1).
The slopes of the incidence curves were steepest in 1998/1999 and 2003/2004 (Figure 2). These coincide with, and may be explained by, the launching of atorvastatin in 1998 onto the Finnish market and the introduction of generic substitution in 2003. The intensive marketing of atorvastatin may have targeted therapy to persons not previously considered eligible for statins. On the other hand, the substantial price reductions of generic simvastatin and other generic statin preparations may have boosted their use.
The direct comparison of our results with other studies is difficult since only a few studies have used similar methodology to describe the demographics of statin users. In Norway, the 1 year prevalence of statin use among males was 7.5% and among females 6.3% in 2004/2005 [27]. Furthermore, national statistics on drug use in other Nordic countries offer relevant comparison data [28, 29]. In Sweden the intensity of statin use among females counted by DDDs was 27% lower than among males, and in Denmark 46% of the users were females. The use was the most intensive among persons aged 65−74 years in Sweden. In Denmark the median age of the users was 2 years lower than in Finland, 64 years (interquartile range 57−72) in 2005 [29]. The prevalence and incidence figures on statin use in our study corresponded to the highest prevalence and incidence of the use of all lipid lowering drugs among populations aged 60−69 years in some previous studies [14, 15]. A previous report from Finland [8], as well as reports from Sweden [12], Denmark [2, 13, 15] and the Netherlands [14] have shown increasing LLD use in the 1990s to be dominated by males.
In conclusion, in Finland the use of statins had already shifted to elderly persons some years before rigorous evidence from clinical trials was available. The shift was in accordance with the change in the age-specific prevalence of CHD. However, current targeting of statin therapy may be partly suboptimal as reflected by the missing difference in the utilization pattern between the genders. Considering the large number of the elderly, a fragile population, continuously on statins studies on benefits and harms in a real-life setting among elderly are needed.
Disclosures: Päivi Ruokoniemi: No conflict of interests. Arja Helin-Salmivaara: No conflict of interests. Timo Klaukka: No conflict of interests. Pertti J. Neuvonen: No conflict of interests. Risto Huupponen: No conflict of interests.
We thank Hilkka Ruuska and Kristiina Tyrkkö, from the Social Insurance Institution, for their data management skills and biostatistician Tero Vahlberg, Department of Biostatistics, University of Turku, for his valuable instructions and comments on statistical analysis.
This study was partly funded by the research grant from the Social Insurance Institution (10/26/2007). The sponsor had no role in the design, conduct, analysis, interpretation of the data, or in the preparation, review, or approval of the manuscript.
Supporting information
Additional supporting information may be found in the online version of this article:
1 year prevalence of statin use, both genders (per 1000)
1 year prevalence of statin use among males (per 1000)
1 year prevalence of statin use among females (per 1000)
1 year incidence of statin use, both genders (per 100 000)
1 year incidence of statin use among males (per 100 000)
1 year incidence of statin use among females (per 100 000)
Please note: Blackwell Publishing is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- 1.Baxter C, Jones R, Corr L. Time trend analysis and variations in prescribing lipid lowering drugs in general practice. BMJ. 1998;317:1134–5. doi: 10.1136/bmj.317.7166.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larsen J, Andersen M, Kragstrup J, Gram LF. Changes in the utilisation of lipid-lowering drugs over a 6-year period (1993–1998) in a Danish population. Eur J Clin Pharmacol. 2001;57:343–8. doi: 10.1007/s002280100307. [DOI] [PubMed] [Google Scholar]
- 3.Scandinavian Simvastatin Survival Study Group. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S) Lancet. 1994;344:1383–9. [PubMed] [Google Scholar]
- 4.Shepherd J, Cobbe SM, Ford I, Isles CG, Lorimer AR, MacFarlane PW, McKillop JH, Packard CJ. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–7. doi: 10.1056/NEJM199511163332001. [DOI] [PubMed] [Google Scholar]
- 5.Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E for the Cholesterol and Recurrent Events Trial investigators. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. N Engl J Med. 1996;335:1001–9. doi: 10.1056/NEJM199610033351401. [DOI] [PubMed] [Google Scholar]
- 6.The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med. 1998;339:1349–57. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 7.Siegel D, Lopez J, Meier J. Use of cholesterol-lowering medications in the United States from 1991 to 1997. Am J Med. 2000;108:496–9. doi: 10.1016/s0002-9343(00)00319-3. [DOI] [PubMed] [Google Scholar]
- 8.Martikainen J, Klaukka T, Reunanen A, Peura S, Wahlroos H. Recent trends in the consumption of lipid-lowering drugs in Finland. J Clin Epidemiol. 1996;49:1453–7. doi: 10.1016/s0895-4356(96)00267-3. [DOI] [PubMed] [Google Scholar]
- 9.Deambrosis P, Saramin C, Terrazzani G, Scaldaferri L, Debetto P, Giusti P, Chinellato A. Evaluation of the prescription and utilization patterns of statins in an Italian local health unit during the period 1994–2003. Eur J Clin Pharmacol. 2007;63:197–203. doi: 10.1007/s00228-006-0239-3. [DOI] [PubMed] [Google Scholar]
- 10.Wang TJ, Stafford RS, Ausiello JC, Chaisson CE. Randomized clinical trials and recent patterns in the use of statins. Am Heart J. 2001;141:957–63. doi: 10.1067/mhj.2001.115587. [DOI] [PubMed] [Google Scholar]
- 11.EUROASPIRE I and II Group. European Action on Secondary Prevention by Intervention to Reduce Events. Clinical reality of coronary prevention guidelines: a comparison of EUROASPIRE I and II in nine countries. Lancet. 2001;357:995–1001. doi: 10.1016/s0140-6736(00)04235-5. [DOI] [PubMed] [Google Scholar]
- 12.Magrini N, Einarson T, Vaccheri A, McManus P, Montanaro N, Bergman U. Use of lipid-lowering drugs from 1990 to 1994: an international comparison among Australia, Finland, Italy (Emilia Romagna Region), Norway and Sweden. Eur J Clin Pharmacol. 1997;53:185–9. doi: 10.1007/s002280050360. [DOI] [PubMed] [Google Scholar]
- 13.Larsen J, Vaccheri A, Andersen M, Montanaro N, Bergman U. Lack of adherence to lipid-lowering drug treatment. A comparison of utilization patterns in defined populations in Funen, Denmark and Bologna, Italy. Br J Clin Pharmacol. 2000;49:463–71. doi: 10.1046/j.1365-2125.2000.00192.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mantel-Teeuwisse AK, Klungel OH, Verschuren WM, Porsius AJ, de Boer A. Time trends in lipid lowering drug use in The Netherlands. Has the backlog of candidates for treatment been eliminated? Br J Clin Pharmacol. 2002;53:379–85. doi: 10.1046/j.1365-2125.2002.01562.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Riahi S, Fonager K, Toft E, Hvilsted-Rasmussen L, Bendsen J, Paaske Johnsen S, Sorensen HT. Use of lipid-lowering drugs during 1991–98 in Northern Jutland, Denmark. Br J Clin Pharmacol. 2001;52:307–11. doi: 10.1046/j.0306-5251.2001.01439.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walley T, Folino-Gallo P, Stephens P, Van Ganse E. Trends in prescribing and utilization of statins and other lipid lowering drugs across Europe 1997–2003. Br J Clin Pharmacol. 2005;60:543–51. doi: 10.1111/j.1365-2125.2005.02478.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nordic Medico Statistical Committee (Nomesco) Medicines Consumption in the Nordic Countries 1999–2003. Copenhagen, Denmark: Nomesco; 2004. [Google Scholar]
- 18.The National Agency for Medicines and the Social Insurance Institution. Finnish Statistics on Medicines 2005. Helsinki, Finland: National Agency for Medicines and the Social Insurance Institution; 2006. [Google Scholar]
- 19.The National Agency for Medicines. Classification of Medicines and the Defined Daily Doses 2005. Helsinki, Finland: National Agencies for Medicines; 2005. [Google Scholar]
- 20.The National Agency for Medicines. Classification of Medicines and the Defined Daily Doses 1995. Helsinki, Finland: National Agencies for Medicines; 1995. [Google Scholar]
- 21.Kattainen A, Salomaa V, Härkänen T, Jula A, Kaaja R, Kesäniemi YA, Kähönen M, Moilanen L, Nieminen MS, Aromaa A, Reunanen A. Coronary heart disease: from a disease of middle-aged men in the late 1970s to a disease of elderly women in the 2000s. Eur Heart J. 2006;27:296–301. doi: 10.1093/eurheartj/ehi630. [DOI] [PubMed] [Google Scholar]
- 22.Pajunen P, Pääkkönen R, Juolevi A, Hämäläinen H, Keskimäki I, Laatikainen T, Moltchanov V, Niemi M, Rintanen H, Salomaa V. Trends in fatal and non-fatal coronary heart disease events in Finland during 1991–2001. Scand Cardiovasc J. 2004;38:340–4. doi: 10.1080/14017430410010996. [DOI] [PubMed] [Google Scholar]
- 23.Shepherd J, Blauw GJ, Murphy MB, Bollen ELEM, Buckley BM, Cobbe SM, Ford I, Gaw A, Hyland M, Jukema JW, Kamper AM, Macfarlane PW, Meinders AE, Norrie J, Packard CJ, Perry IJ, Stott DJ, Sweeney BJ, Twomey C, Westendorp RGJ. Pravastatin in elderly individuals at risk of vascular disease (PROSPER): a randomised controlled trial. Lancet. 2002;360:1623–30. doi: 10.1016/s0140-6736(02)11600-x. [DOI] [PubMed] [Google Scholar]
- 24.Heart protection Study Collaborative Group. MRC/BHF heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–21. doi: 10.1016/S0140-6736(11)61125-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suomen Sisätautilääkärien yhdistyksen asettama työryhmä. Dyslipidemiat. Duodecim. 2004;120:1794–1816. in Finnish. [Google Scholar]
- 26.Aromaa A, Koskinen S. Health and functional capacity in Finland. Baseline results of the Health 2000 health examination survey. Publications of the National Public Health Institute. B.
- 27.Sakshaug S, Furu K, Karlstad Ø, Rønnig M, Skurtveit S. Switching statins in Norway after new reimbursement policy – a nationwide prescription study. Br J Clin Pharmacol. 2007;64:476–81. doi: 10.1111/j.1365-2125.2007.02907.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Försäljningsstatistik. Statistics on medicinal product sales. [3 August 2007]. Available at http://www2.apoteket.se/Apoteket/om/VadViGor/Forsalj/default.htm.
- 29.Danish Medicines Agency. Medicinal Product Statistics 2001–2005. Danish Medicines Agency, Denmark: Legemiddelstyrelsen; 2006. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
1 year prevalence of statin use, both genders (per 1000)
1 year prevalence of statin use among males (per 1000)
1 year prevalence of statin use among females (per 1000)
1 year incidence of statin use, both genders (per 100 000)
1 year incidence of statin use among males (per 100 000)
1 year incidence of statin use among females (per 100 000)


