Abstract
For evaluation of the prevalence of Cryptosporidium sp. infection in diarrheic and non-diarrheic humans in Iran, fecal specimens from diarrheic (n = 129) and non-diarrheic humans (n = 271) were collected and examined for the presence of Cryptosporidium sp. oocysts. The presence of Cryptosporidium sp. oocysts was determined by Ziehl-Neelsen acid-fast staining. Humans were grouped according to their age as follows: younger than 15, 16-25, 26-35, 36-50, and over 51 years. The results showed that the overall prevalence of infection in all 400 samples was 10.8%, but the prevalence (25.6%) in diarrheic humans was higher than that (3.7%) in non-diarrheic humans. Oocysts of Cryptosporidium sp. were detected in the feces of 21.4%, 9.3%, 8.8%, 6.7% and 5.7% of different age groups, respectively. The intensity of oocysts was significantly higher in diarrheic humans than in non-diarrheic ones. There was a significant association between Cryptosporidium sp. infection and occurrence of diarrhea (P < 0.05). The results indicate that Cryptosporidium sp. infection is prevalent in diarrheic humans in Iran.
Keywords: Cryptosporidium sp., cryptosporidiosis, prevalence, diarrhea, Iran
INTRODUCTION
Cryptosporidium sp. is an intestinal protozoan parasite that has been recognized as a human pathogen since 1976 (Fayer and Ungar, 1986). This parasite is well known to cause severe life-threatening illness in immunocompromised individuals. This parasite invades epithelial cells of the intestinal tract and respiratory tree of vertebrate hosts (O'Donoghue, 1995; Sturdee et al., 1999). Cryptosporidium sp. is a primary pathogen causing acute diarrhea and the most evident symptom of cryptosporidiosis is diarrhea. Non-specific signs, such as dehydration, fever, anorexia, weakness, and progressive loss of conditions may be accompanied. Diarrhea is usually self-limiting in immunocompetent humans, however, it can be life-threatening in children and immunocompromised humans. There are a variety of methods, including microscopy, immunological and molecular techniques, for the detection of Cryptosporidium oocysts. Microscopic methods include concentration techniques and staining of fecal smears. There are difficulties in distinguishing Cryptosporidium oocysts from other small particles, such as yeasts, moulds, algae, and plant debris by routine fecal examination techniques in fecal and environmental specimens (Fayer et al., 2000). The modified acid-fast staining technique is useful and the oocysts appear as pink to red, spherical to ovoid, bodies on a blue or purple background. The stained smears are permanent and can be stored for a long time before examination when the samples are high numbers (Sevinc et al., 2003).
The purpose of this study was to determine the prevalence of Cryptosporidium sp. infection in different age groups of diarrheic and non-diarrheic humans in Iran by the conventional microscopy method using the modified acid-fast staining.
MATERIALS AND METHODS
Subjects and fecal examination
Fecal samples (400 in total number) were collected in sterile plastic bottles from the inhabitants residing in the City of Shiraz, Fars Province, Iran, who presented with diarrhea (n = 129) and non-diarrhea (n = 271) during the period from July 1 to September 30, 2002. Humans were grouped according to their age as follows: under 15, 16-25, 26-35, 36-50, and over 51 years. Fecal smears were prepared by formalin-ether sedimentation, and examined after modified acid-fast staining (Casemore et al., 1985). The intensity of infection was estimated semi-quantitatively according to the average number of oocysts in 20 randomly selected fields at 1,000 x magnification. The categories established were; negative (absence of oocysts); slight (1-5 oocysts); moderate (6-10 oocysts); and severe (> 10 oocysts) (Sevinc et al., 2003).
Statistical analysis
The results of the study were analyzed using the SPSS software Version 10.1. The chi-square test was used to determine the relationship between the presence of Cryptosporidium oocysts in the patients who provided the stool samples, and other parameters, such as diarrhea symptoms, and age. The differences were considered significant, when the P-value was less than 0.05.
RESULTS
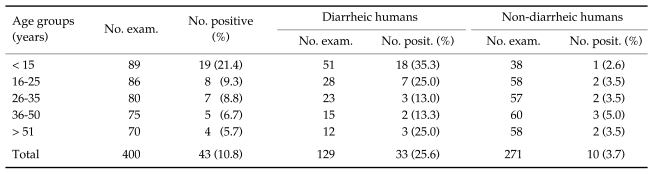
The total number of Cryptosporidium oocyst positive specimens was 43, and the prevalence was 10.8%. Cryptosporidium sp. oocysts appeared as pink to red and spherical to ovoid bodies in modified acid-fast staining. Cryptosporidium oocysts were detected in 33 (25.6%) of 129 diarrheic humans, and in 10 (3.7%) of 271 non-diarrheic humans. The age-dependent prevalence was 21.4%, 9.3%, 8.8%, 6.7% and 5.7% in the age groups of younger than 15 years old, 16-25, 26-35, 36-50, and over 51 years, respectively (Table 1). The intensity of infection in the oocyst numbers was significantly higher in diarrheic humans than in non-diarrheic ones (data not shown). There was a significant association between Cryptosporidium sp. infection and occurrence of diarrhea (P < 0.05). Also the prevalence of Cryptosporidium sp. infection was significantly higher in children under 15 years old than other age groups (P < 0.05).
Table 1.
The prevalence of Cryptosporidium sp. infection in different age groups of diarrheic and non-diarrheic humans in Iran
DISCUSSION
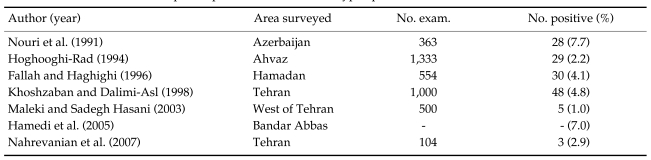
The objective of this study was to determine the prevalence of Cryptosporidium sp. infection in diarrheic and non-diarrheic humans in Iran. In this study, the total number of positive specimens was 43 and the prevalence of Cryptosporidium sp. in all specimens was 10.8%. There are discrepancies in the prevalence between different surveys, which were done on human cryptosporidiosis. In the Republic of Korea, the prevalence of cryptosporidiosis varied according to the localities. For example, Lee et al. (2005) reported a prevalence of 1% (among non-HIV patients), whereas Yu et al. (2004) reported a prevalence of 3.3% among the villagers in several rural areas. Also Park et al. (2006), Seo et al. (2001), and Chai et al. (1996) reported 1.5%, 1.9% and 7.9% positive rates of human cryptosporidiosis, respectively. In Tanzania, Houpt et al. (2005) described a prevalence of 17.3% amongst HIV patients. In Guinea Bissau, Cryptosporidium sp. had a prevalence of 7.7% and was the second most common parasite with a marked seasonal variation, with peak prevalence found consistently at the beginning of or just before the rainy seasons, i.e., from May to July (Perch et al., 2001). The bovine genotype of Cryptosporidium parvum accounts for most cases of human cryptosporidiosis in Iran (Meamar et al., 2006). There were also discrepancies in different surveys which were done in Iran, about the prevalence rate of Cryptosporidium sp. (Table 2). For example, Hamedi et al. (2005) reported a prevalence of 7% in children in southeastern Iran, but in the present study, the prevalence of Cryptosporidium infection was 21.4% in children, who are under 15 years old.
Table 2.
A brief review of the reported prevalences of human cryptosporidiosis in Iran
Intestinal parasites are very common in developing countries and Cryptosporidium has been revealed as one of the most common parasites, which causes diarrhea, and diarrhea is the most pronounced clinical feature of cryptosporidiosis. Cryptosporidium parasitizes the small intestinal epithelium, therefore, the infection results in an accelerated loss of villous enterocytes, leading to severe villous atrophy and a malabsorptive and secretory diarrhea. Other symptoms include dehydration, weight loss, stomach cramp, or pain, fever, nausea, and vomiting (Abdel-Messih et al., 2005).
Several studies have observed higher prevalences of Cryptosporidium sp. infections among diarrheic calves as compared with non-diarrheic calves (Naciri, 1999; De la Fuente et al., 1999; Lefay et al., 2000; Uga et al., 2000; Castro-Hermid et al., 2002). Also in the present study, Cryptosporidium sp. was detected in 33 (25.6%) and 10 (3.7%) of diarrheic and non-diarrheic humans, respectively. The majority of the diarrheic humans (39.5%) were younger than 15 years and 18 (35.3%) of them were positive for Cryptosporidium sp. infection. The infection was detected in 19 (21.4%), 8 (9.3%), 7 (8.8%), 5 (6.7%) and 4 (5.7%) of humans in the age groups < 15, 16-25, 26-35, 36-50 and over 51 years, respectively.
Though humans seem to be susceptible at any time in their lives (Fayer and Ungar, 1986), results of this research showed that the prevalence of Cryptosporidium sp. was higher in children under 15 years old. The high prevalence of Cryptosporidium sp. in children is similar to previous reports (Bezerra et al., 2001; Yu et al., 2004). Also previous studies in tropical countries have shown the highest prevalence of cryptosporidiosis in children younger than 2 years. However, recent studies in Kuwait (Sulaiman et al., 2005) have indicated that children infected with Cryptosporidium were significantly older. The occurrence of high infection rates in children less than 15 years old might be attributed to their weak immune responses. However, more studies need to be done in order to confirm this hypothesis. From prevalence studies, oocyst excretion rates are known to vary between 1% and 3% in industrialized countries and around 10% in less industrialized nations. Cryptosporidium sp. infection generally occurs in 10-15% of children with diarrhea in the developing world, but in this study Cryptosporidium sp. infection was found in 35.3% of the children with diarrhea. The most common clinical manifestation of cryptosporidiosis is diarrhea, characteristically profuse and watery, and often containing mucus, but rarely blood or leucocytes (Fayer and Ungar, 1986). The diarrhea is watery, and stool frequency can be up to 10 times a day with a mean volume of 1 liter (Chen and LaRusso, 1999).
The results of the present study showed that the prevalence of Cryptosporidium sp. in diarrheic humans was higher than that in non-diarrheic humans in Iran, and children under 15 years old are more susceptible to Cryptosporidium sp. infection.
ACKNOWLEDGMENTS
The author wish to thank Mrs. Diane Simpson for editing this article.
References
- 1.Abdel-Messih IA, Wierzba TF, Abu-Elyazeed R, Ibrahim AF, Ahmed SF, Kamal K, Sanders J, French R. Diarrhea associated with Cryptosporidium parvum among young children of the Nile River Delta in Egypt. J Trop Pediatr. 2005;51:154–159. doi: 10.1093/tropej/fmh105. [DOI] [PubMed] [Google Scholar]
- 2.Bezerra FSM, Troiani RM, Parente TML, Paiva ARA, Queiroz RMP, Coelho JR, Oliveira MF. Incidência de criptosporidiose em crianças com desnutrição de moderada à grave internas no IPREDE (Instituto de Prevenção à Desnutrição e à Excepcionalidade) em Fortaleza-CE. Revista da Sociedade Brasileira de Medicina Tropical. 2001;34:300. [Google Scholar]
- 3.Casemore DP, Armstrong M, Sands RL. Laboratory diagnosis of cryptosporidiosis. J Clin Pathol. 1985;38:1337–1341. doi: 10.1136/jcp.38.12.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castro-Hermida JA, Gonzalez-Losada YA, Ares-mazas E. Prevalence of and risk factors involved in the spread of neonatal bovine cryptosporidiosis in Galicia (NW Spain) Vet Parasitol. 2002;106:1–10. doi: 10.1016/S0304-4017(02)00036-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chai JY, Lee SH, Guk SM, Lee SH. An epidemiological survey of Cryptosporidium parvum infection in randomly selected inhabitants of Seoul and Jeollanam-do. Korean J Parasitol. 1996;34:113–119. doi: 10.3347/kjp.1996.34.2.113. [DOI] [PubMed] [Google Scholar]
- 6.Chen XM, LaRusso NF. Human intestinal and biliary cryptosporidiosis. World J Gastroenterol. 1999;5:424–429. doi: 10.3748/wjg.v5.i5.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De la Fuente R, Luzon M, Ruiz-Santa-Quiteria JA, Garcia A, Cid D, Orden JA, Garcia S, Sanz R, Gomez-Bautista M. Cryptosporidium and concurrent infections with other major enteropathogens in 1 to 30-day-old diarrheic dairy calves in central Spain. Vet Parasitol. 1999;80:179–185. doi: 10.1016/S0304-4017(98)00218-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fallah M, Haghighi A. Cryptosporidiosis in children with diarrhea submitted to health centers in the west of Iran (Hamadan) Med J Islam Repub Iran. 1996;4:315–317. [Google Scholar]
- 9.Fayer R, Morgan U, Upton SJ. Epidemiology of Cryptosporidium: transmission, detection and identification. Int J Parasitol. 2000;30:1305–1322. doi: 10.1016/s0020-7519(00)00135-1. [DOI] [PubMed] [Google Scholar]
- 10.Fayer R, Ungar BLP. Cryptosporidium spp. and cryptosporidiosis. Microbiol Rev. 1986;50:458–483. doi: 10.1128/mr.50.4.458-483.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hamedi Y, Safa? O, Haidari? M. Cryptosporidium infection in diarrheic children in southeastern Iran. Pediatr Infect Dis J. 2005;24:86–88. doi: 10.1097/01.inf.0000148932.68982.ec. [DOI] [PubMed] [Google Scholar]
- 12.Hoghooghi-Rad N. Some epidemiological aspects of cryptosporidiosis in Ahvaz, Capital of Khoozestan province, Islamic Republic of Iran. Med J Islam Repub Iran. 1994;1:17–22. [Google Scholar]
- 13.Houpt E, Bushen OY, Sam NE, Kohli A, Asgharpour A, Ng CT, Calfee DP, Guerrant RL, Maro V, Ole-Nguyaine S, Shao JF. Short report: asymptomatic Cryptosporidium hominis infection among human immunodeficiency virus-infected patients in Tanzania. Am J Trop Med Hyg. 2005;73:520–522. [PubMed] [Google Scholar]
- 14.Khoshzaban F, Dalimi-Asl A. Epidemiological study on Cryptosporidiosis in diarrheatic children. Sci Res J Shahed Univ (Iran) 1998;19:26–21. [Google Scholar]
- 15.Lee JK, Song HJ, Yu JR. Prevalence of diarrhea caused by Cryptosporidium parvum in non-HIV patients in Jeollanam-do, Korea. Korean J Parasitology. 2005;43:111–114. doi: 10.3347/kjp.2005.43.3.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lefay D, Naciri M, Poirier P, Chermette R. Prevalence of Cryptosporidium infection in calves in France. Vet Parasitol. 2000;89:1–9. doi: 10.1016/S0304-4017(99)00230-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maleki F, Sadegh-Hasani S. Prevalence of cryptosporidiosis in students of elementary schools in the west Tehran-Iran from 1999-2001. J Iran Univ Med Sci. 2003;33:110–105. [Google Scholar]
- 18.Meamar AR, Rezaian M, Rezaie S, Mohraz M, Mohebali M, Mohammad K, Golestan B, Guyot K, Dei-Cas E. SSU- rRNA Gene Analysis of Cryptosporidium spp. in HIV Positive and Negative Patients. Iranian J Publ Hlth. 2006;35:1–7. [Google Scholar]
- 19.Naciri M, Lefay MP, Mancassola R, Poirier P, Chermette R. Role of Cryptosporidium parvum as a pathogen in neonatal diarrhea complex in suckling and dairy calves in France. Vet Parasitol. 1999;85:245–257. doi: 10.1016/S0304-4017(99)00111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nahrevanian H, Assmar M, Samin MG. Cryptosporidiosis among immunocompetent patients with gastroenteritis in Iran: a comparison with other enteropathogenic parasites. J Microbiol Immunol Infect. 2007;40:154–156. [PubMed] [Google Scholar]
- 21.Nouri M, Moghadam A, Haghighatnia H. Cryptosporidium infection in human diarrhea patients in West Azerbaijan, Iran. Med J Islam Repub Iran. 1991;2:35–38. [Google Scholar]
- 22.O'Donoghue PJ. Cryptosporidium and cryptosporidiosis in man and animals. Int J Parasitol. 1995;25:139–195. doi: 10.1016/0020-7519(94)e0059-v. [DOI] [PubMed] [Google Scholar]
- 23.Park JH, Kim HJ, Guk SM, Shin EH, Kim JL, Rim HJ, Lee SH, Chai JY. A survey of cryptosporidiosis among 2,541 residents of 25 coastal islands in Jeollanam-Do (Province), Republic of Korea. Korean J Parasitol. 2006;44:367–372. doi: 10.3347/kjp.2006.44.4.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Perch M, Sodemann M, Jakobsen MS, Valentiner-Branth P, Steinsland H, Fischer TK, Lopes DD, Aaby P, Molbak K. Seven years' experience with Cryptosporidium parvum in Guinea-Bissau, West Africa. Ann Trop Paediatr. 2001;21:313–318. doi: 10.1080/07430170120093490. [DOI] [PubMed] [Google Scholar]
- 25.Seo M, Huh S, Chai JY, Yu JR. An epidemiological survey on Cryptosporidium parvum infection of inhabitants in Chorwon-gun, Kangwon-do. Korean J Parasitol. 2001;39:201–203. doi: 10.3347/kjp.2001.39.2.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sevinc F, Irmak K, Sevinc M. The prevalence of Cryptosporidium parvum infection in the diarrhoiec and non-diarrheic calves. Revue Méd Vét. 2003;154:357–361. [Google Scholar]
- 27.Sturdee AP, Chalmers RM, Bull SA. Detection of Cryptosporidium oocysts in wild mammals of mainland Britain. Vet Parasitol. 1999;80:273–280. doi: 10.1016/s0304-4017(98)00226-x. [DOI] [PubMed] [Google Scholar]
- 28.Sulaiman IM, Hira PR, Zhou L, Al-Ali FM, Al-Shelahi FA, Shweiki HM, Iqbal J, Khalid N, Xiao L. Unique endemicity of cryptosporidiosis in children in Kuwait. J Clin Microbiol. 2005;43:2805–2809. doi: 10.1128/JCM.43.6.2805-2809.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Uga S, Matsuo J, Kono E, Kimura K, Inoue M, Rai SK, Ono K. Prevalence of Cryptosporidium parvum infection and pattern of oocyst shedding in calves in Japan. Vet Parasitol. 2000;94:27–32. doi: 10.1016/s0304-4017(00)00338-1. [DOI] [PubMed] [Google Scholar]
- 30.Yu JR, Lee JK, Seo M, Kim SI, Sohn WM, Huh S, Choi HY, Kim TS. Prevalence of cryptosporidiosis among the villagers and domestic animals in several rural areas of Korea. Korean J Parasitol. 2004;42:1–6. doi: 10.3347/kjp.2004.42.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]