Abstract
The prevalence of liver and intestinal fluke infections was surveyed on residents of Savannakhet Province, Laos. Fecal specimens were collected from a total of 981 residents in 4 Mekong riverside villages and examined by the Kato-Katz thick smear technique. The results revealed that the overall helminth egg positive rate was 84.2%, and the positive rate for small trematode eggs, including Opisthorchis viverrini, heterophyids, or lecithodendriids, was 67.1%. To obtain adult flukes, 38 small trematode egg positive cases were treated with a 20-30 mg/kg single dose of praziquantel and purged. Diarrheic stools were then collected from 29 people and searched for helminth parasites using stereomicroscopes. Mixed infections with O. viverrini and 6 kinds of intestinal flukes were found, namely, Haplorchis taichui, Haplorchis pumilio, Haplorchis yokogawai, Prosthodendrium molenkampi, Phaneropsolus bonnei, and echinostomes. The total number of flukes collected was 7,693 specimens (av. no. per treated person; 265.3). The most common species was O. viverrini, followed by H. taichui, P. molenkampi, echinostomes, H. pumilio, P. bonnei, and H. yokogawai. The results indicate that foodborne liver and intestinal fluke infections are prevalent among residents of Savannakhet Province, Laos.
Keywords: Opisthorchis viverrini, Haplorchis taichui, Prosthodendrium molenkampi, Phaneropsolus bonnei, prevalence, Savannakhet Province, Laos
INTRODUCTION
The liver, lung and intestinal flukes are recognized as an important group of emerging and reemerging foodborne zoonotic parasites (Chai and Lee, 2002; Chai et al., 2005a). In Southeast Asia, Clonorchis sinensis, Opisthorchis viverrini, and Paragonimus westermani have been recognized as the 3 major foodborne trematode species. However, more than 50 species of intestinal flukes, including Heterophyes nocens, Metagonimus yokogawai, Haplorchis spp., Centrocestus spp., Prosthodendrium molenkampi, Phaneropsolus bonnei, and Echinostoma spp., are also included in the list of foodborne trematodes of public health importance (Yu and Mott, 1994; Chai and Lee, 2002; Chai et al., 2005a).
Laos is located in the middle of South Asia, and the Mekong River runs through Laos, from north to south. High prevalences of O. viverrini infection have been recorded among residents or schoolchildren in different localities of Laos (Sornmani et al., 1974; Pholsena et al., 1991; Chai and Hongvanthong, 1998; Kobayashi et al., 2000; Rim et al., 2003). However, with regard to intestinal flukes, only a small number of studies have been available (Ditrich et al., 1990; Giboda et al., 1991; Chai et al., 2005b). It is of note that mixed-infections with O. viverrini, heterophyids (Haplorchis spp.), and lecithodendriids (P. molenkampi and P. bonnei) are common, and the intensity of infection with each fluke species varies by locality along the Mekong River basin (Chai et al., 2005b). However, this tendency has been verified only in Vientiane Municipality and Saravane Province.
Therefore, the present study was performed to determine the status of O. viverrini, H. taichui, and other foodborne trematode infections among the residents of Savannakhet Province (Mekong riverside), which is located some distance between Vientiane Municipality and Saravane Province.
MATERIALS AND METHODS
Areas surveyed
Four villages (Bane Xok, Bane Phonsoun, Bane Houay, and Ban Nhangsoung) in Savannakhet Province were included in the present study (Fig. 1). These villages are located near the tributaries of the Mekong River. Most residents are agricultural workers, and some residents catch freshwater fish and aquatic insect larvae, such as the naiads of dragonflies from small streams and ponds, and consume them raw or under improperly cooked conditions.
Fig. 1.
Map showing the surveyed area (arrow: Savannakhet City) of Laos.
Fecal examinations
A total of 981 fecal samples, one sample from each person, were collected from residents (494 men and 487 women; aged 3-76 years) of Savannakhet Province, in July 2002. Samples were transported to the Malaria Station in Savannakhet City within 2-3 days of collection and stored at 4℃ until examined. The Kato-Katz thick smear technique was used to detect helminth eggs. It was difficult to differentiate eggs of O. viverrini from those of heterophyids, such as H. taichui, and lecithodendriids, like P. molenkampi and P. bonnei (Tesana et al., 1991; Kaewkes et al., 1991; Ditrich et al., 1992). Therefore, these eggs were recorded collectively as small trematode eggs.
Worm collection
A total of 38 people who discharged small trematode eggs (opisthorchiid, heterophyid, or lecithoden driid eggs) were selected for adult fluke collection. After obtaining informed consent, these people who visited the Malaria Station were treated with a single dose (20-30 mg/kg) of praziquantel (Shinpoong Pharmaceutical Co., Seoul, Republic of Korea) and then purged with magnesium salt. Whole diarrheic stools passed successively 4-5 times were collected and pooled. Further processing of the diarrheic stools was done as previously described (Chai et al., 2005b). From the final sediment, worms were collected using a glass pipette and washed several times in water. The number of worms collected was counted, and some were fixed with 10% formalin under cover slip pressure, acetocarmine-stained, and morphologically identified using a light microscope. Fecal examination and worm collection from residents were approved by the Ministry of Public Health, Laos, under the terms of the Korea-Laos agreement on Parasite Control in Laos (1999-2004).
Statistical analysis
Fecal examination results for trematode eggs were analyzed with respect to age and sex of subjects using the Student's t-test and the chi-square test. P-values < 0.05 were considered significant.
RESULTS
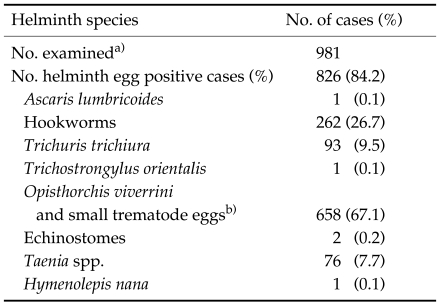
Helminth egg positive rates
The overall helminth egg positive rate was 84.2% (Table 1). Small trematode eggs, including those of O. viverrini, heterophyids and lecithodendriids, were the most frequently encountered, with an egg positive rate of 67.1% (Table 1). Eggs of other parasites included those of hookworms (26.7%), Trichuris trichiura (9.5%), Taenia spp. (7.7%), echinostomes (0.2%), Ascaris lumbricoides (0.1%), Trichostrongylus orientalis (0.1%), and Hymenolepis nana (0.1%). Egg positive rates were not significantly (P > 0.05) different between men and women (data not shown), and the age-dependent prevalence was unremarkable (data not shown).
Table 1.
Helminth egg positive rates in the feces of residents in Savannakhet Province, Laos (July 2002)
a)Fecal examination was performed by the Kato-Katz thick smear technique. One smear was examined for each person.
b)Including the eggs of heterophyids (Heterophyidae) and lecithodendriids (Lecithodendriidae).
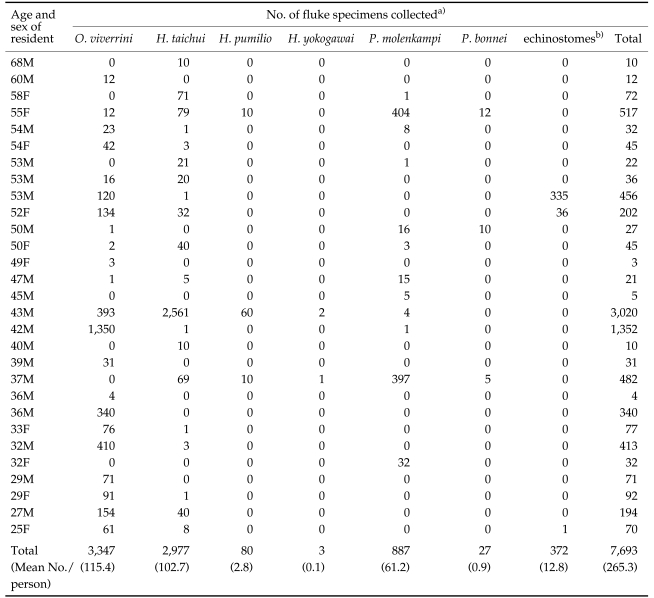
Worm collection results
Worm collection was completed successfully in 29 persons (19 men and 10 women; age range 25-68 years) (Table 2). A total of 3,347 O. viverrini specimens (0-1,350 individually; av. 115.4 per person) and a total of 4,346 intestinal flukes (0-2,561; av. 149.9 per person) were collected (Table 2). O. viverrini comprised 43.5% of flukes collected and intestinal flukes 56.5%. Of the intestinal flukes, H. taichui was the dominant species, followed by P. molenkampi, echinostomes (species undetermined), H. pumilio, P. bonnei and H. yokogawai (Table 2). The highest number of H. taichui collected from a single person was 2,561, with an average number of collected worms per person of 102.7. The number of H. pumilio collected per person ranged from 0 to 60, with an average of 2.8 worms, which was much smaller than the number of H. taichui. The number of H. yokogawai was only 3. With regard to lecithodendriid flukes, the number of P. molenkampi ranged from 0 to 404 worms per person (av. 61.2 worms), and the number of P. bonnei ranged from 5 to 12 (av. 0.9 worms). Data on echinostomes will be published separately.
Table 2.
Results of adult fluke collection from residents in Savannakhet Province, Laos (July 2002)
a)O. viverrini, Opisthorchis viverrini; H. taichui, Haplorchis taichui; H. pumilio, Haplorchis pumilio; H. yokogawai, Haplorchis yokogawai; P. molenkampi, Prosthodendrium molenkampi; P. bonnei, Phaneropsolus bonnei.
b)Species not determined.
DISCUSSION
The results of the present study indicate that the liver fluke O. viverrini and intestinal flukes, including H. taichui, H. pumilio, H. yokogawai, P. molenkampi, P. bonnei, and echinostomes, are mixed-infected among the residents of Savannakhet Province, Laos. O. viverrini and H. taichui appeared to be the 2 most common species. Mixed infections with various fluke species were similar to our previous study performed in Vientiane Municipality and Saravane Province, Laos (Chai et al., 2005b). However, the intensity of infection with each fluke species varied by locality surveyed, i.e., in Vientiane, O. viverrini composed 62.9% of all flukes recovered, whereas, in Saravane, intestinal flukes accounted for over 99.0% of all recovered flukes (Chai et al., 2005b). In the present study, 43.5% of flukes collected were O. viverrini and 56.5% were intestinal flukes. Therefore, Savannakhet Province was intermediate between Vientiane Municipality and Saravane Province with respect to the predominance of O. viverrini and intestinal flukes infected among the riverside residents.
However, the intensity of O. viverrini infection was the highest in Savannakhet Province (av. 115.4 worms per treated person), followed by Vientiane Municipality (av. 57.8) and Saravane Province (av. 21.9) (Chai et al., 2005b). In the case of H. taichui, the average number of worms recovered per person was remarkably high (8,514) in Saravane Province, whereas it was comparatively low in Savannakhet Province (102.7) and Vientiane Municipality (26.9) (Chai et al., 2005b). In the case of lecithodendriid flukes, the highest average number of worms was found in Savannakhet Province (61.2 for P. molenkampi and 0.9 for P. bonnei), followed by Saravane Province (24.5 and 20.4, respectively), and Vientiane Municipality (3.4 and 0.0) (Chai et al., 2005b). These results together indicate that the relative predominance of trematode species vary by locality in Laos. However, Savannakhet Province was found to be generally more endemic for O. viverrini, H. taichui, and lecithodendriids than Vientiane Municipality, and less endemic for H. taichui than Saravane Province.
Human O. viverrini infection has been reported to be prevalent in northeast Thailand (Kaewkes, 2003), Mekong riverside areas of Laos (Sornmani et al., 1974; Chai and Hongvanthong, 1998), and southern areas of Vietnam (De et al., 2003). In Thailand, the infection sources of O. viverrini are various species of freshwater fish, including Cyclocheilichthys siaja, Hampala dispar, Puntius orphoides, Puntius gonionotus, Puntius proctozysron, Puntius viehoever, Labiobarbus lineatus, Esomus metalicus, and Osteochilus sp. (Rim, 1982; Kaewkes, 2003). In Laos, freshwater fish species, including Hampala macrolepidota, H. dispar, Puntius brevis, P. gonionotus, Barbodes gonionotus, and Cyclocheilichthys repasson (Scholz et al., 1990; Ditrich et al., 1990) were verified to be the second intermediate hosts. Dishes containing raw freshwater fish, such as 'Koi pla', 'Pla som', and 'Som fak', are popular foods among the residents of Savannakhet Province, Laos and considered to be the main sources of infection.
Human H. taichui, H. pumilio and H. yokogawai infections have been reported in Southeast Asia, including the Philippines, Thailand, Laos, Taiwan, and South China (Giboda et al., 1991; Yu and Mott, 1994, Chai et al., 2005b; Belizario et al., 2005). Various species of freshwater fish, including Cyprinus spp. and Puntius spp., have been reported to be the second intermediate hosts (Velasquez, 1982). In Laos, H. macrolepidota, H. dispar, P. gonionotus, Mystacoleucus marginatus and Esomus longimana were verified to be the fish hosts for H. taichui and H. pumilio (Scholz et al., 1990; Ditrich et al., 1990).
Human P. molenkampi and P. bonnei infections were first discovered at autopsy of 24 people who resided in Udornthani and Nonkhai Provinces, Thailand, which are geographically close to Laos (Manning et al., 1971), and now known to prevalent in Thailand (Radomyos et al., 1994) and Laos (Chai et al., 2005b). In Thailand, the infection sources with these flukes were verified to be naiads, i.e., the juvenile form in aquatic environments, of dragon- and damselflies (Manning and Lertprasert, 1973). Also in Laos, people found to be infected with P. molenkampi and P. bonnei admitted that they had eaten dragonfly naiads (Chai et al., 2005b). However, in Laos, no larval stages of these flukes have been demonstrated in naiads of dragonflies. Studies are required on this point.
ACKNOWLEDGMENTS
We thank Dr. Sithat Insisiengmay and the staff of the Center for Laboratory and Epidemiology, Department of Hygiene and Prevention, Ministry of Public Health, Vientiane, and staffs of the Savannakhet Provincial Health Department, Savannakhet, Lao PDR, for their help during the collection of fecal samples from residents and for the preparation of Kato-Katz smears. We also thank the staff of the Korea Association of Health Promotion, Seoul, Republic of Korea, who participated in the Korea-Laos Cooperation Project on Parasite Control in Lao PDR (1999-2004).
References
- 1.Belizario VY, Jr, de Leon WU, Bersabe MJJ, Purnomo, Baird JK, Bangs MJ. A focus of human infection by Haplorchis taichui (Trematoda: Heterophyidae) in the Southern Philippines. J Parasitol. 2005;90:1165–1169. doi: 10.1645/GE-3304RN. [DOI] [PubMed] [Google Scholar]
- 2.Chai JY, Hongvanthong B. A small-scale survey of intestinal helminthic infections among the residents near Pakse, Laos. Korean J Parasitol. 1998;36:55–58. doi: 10.3347/kjp.1998.36.1.55. [DOI] [PubMed] [Google Scholar]
- 3.Chai JY, Lee SH. Food-borne intestinal trematode infections in the Republic of Korea. Parasitol Int. 2002;51:129–154. doi: 10.1016/s1383-5769(02)00008-9. [DOI] [PubMed] [Google Scholar]
- 4.Chai JY, Murrell KD, Lymbry A. Fishborne parasitic zoonoses: status and issues. Int J Parasitol. 2005a;35:1233–1254. doi: 10.1016/j.ijpara.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 5.Chai JY, Park JH, Han ET, Guk SM, Shin EH, Lin A, Kim JL, Sohn WM, Yong TS, Eom KS, Min DY, Hwang EH, Phommasack B, Insisiengmai B, Rim HJ. Mixed infections with Opisthorchis viverrini and intestinal flukes in residents of Vientiane Municipality and Saravane Province in Laos. J Helminthol. 2005b;79:283–289. doi: 10.1079/joh2005302. [DOI] [PubMed] [Google Scholar]
- 6.De NV, Murrell KD, Cong LD, Cam PD, Chau LV, Toan ND, Dalsgaard A. The food-borne trematode zoonoses of Vietnam. Southeast Asian J Trop Med Public Health. 2003;34:12–34. [PubMed] [Google Scholar]
- 7.Ditrich O, Giboda M, Scholz T, Beer SA. Comparative morphology of eggs of the Haplorchiinae (Trematoda: Heterophyidae) and some other medically important heterophyid and opisthorchiid flukes. Folia Parasitol. 1992;39:123–132. [PubMed] [Google Scholar]
- 8.Ditrich O, Scholz T, Giboda M. Occurrence of some medically important flukes (Trematoda: Opisthorchiidae and Heterophyidae) in Nam Ngum water reservoir. Southeast Asian J Trop Med Public Health. 1990;21:482–488. [PubMed] [Google Scholar]
- 9.Giboda M, Ditrich O, Scholz T, Viengsay T, Bouaphanh S. Human Opisthorchis and Haplorchis infections in Laos. Trans Royal Soc Trop Med Hyg. 1991;85:538–540. doi: 10.1016/0035-9203(91)90248-w. [DOI] [PubMed] [Google Scholar]
- 10.Kaewkes S. Taxonomy and biology of liver flukes. Acta Trop. 2003;88:177–186. doi: 10.1016/j.actatropica.2003.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Kaewkes S, Elkins DB, Sithithaworn P, Haswell-Elkins MR. Comparative studies on the morphology of the eggs of Opisthorchis viverrini and lecithodendriid trematodes. Southeast Asian J Trop Med Public Health. 1991;22:623–630. [PubMed] [Google Scholar]
- 12.Kobayashi J, Vannachone B, Sato Y, Manivong K, Nambanya S, Inthakone S. An epidemiological study on Opisthorchis viverrini infection in Lao villages. Southeast Asian J Trop Med Public Health. 2000;31:128–132. [PubMed] [Google Scholar]
- 13.Manning GS, Lertprasert P. Studies on the life cycle of Phaneropsolus bonnei and Prosthodendrium molenkampi in Thailand. Ann Trop Med Parasitol. 1973;67:361–365. doi: 10.1080/00034983.1973.11686899. [DOI] [PubMed] [Google Scholar]
- 14.Manning GS, Lertprasert P, Watanasirmkit K, Chetty C. A description of newly discovered intestinal parasites endemic to northeastern Thailand. J Med Ass Thailand. 1971;54:466–474. [PubMed] [Google Scholar]
- 15.Pholsena K, Sayaseng B, Hongvanthong B, Vanisaveth V. The prevalence of helminth infection in Ban Nanin, Laos. Southeast Asian Journal of Tropical Medicine and Public Health. 1991;22:137–138. [PubMed] [Google Scholar]
- 16.Radomyos P, Radomyos B, Tungtrongchitr A. Multi-infection with helminthes in adults from northeast Thailand as determined by post-treatment fecal examination of adult worms. Trop Med Parasitol. 1994;45:133–135. [PubMed] [Google Scholar]
- 17.Rim HJ. Opisthorchiasis. In: Steele JH, editor. CRC Handbook Series in Zoonoses, Section C: Parasitic Zoonoses. Vol. III (Trematode Zoonoses) Boca Raton, Florida, USA: CRC Press; 1982. pp. 109–121. [Google Scholar]
- 18.Rim HJ, Chai JY, Min DY, Cho SY, Eom KS, Hong SJ, Sohn WM, Yong TS, Deodato G., Standgaard H, Phommasack B, Yun CY, Hoang EH. Prevalence of intestinal parasite infections on a national scale among primary schoolchildren in Laos. Parasitol Res. 2003;91:267–272. doi: 10.1007/s00436-003-0963-x. [DOI] [PubMed] [Google Scholar]
- 19.Scholz T, Ditrich O, Giboda M. Larval stages of medically important flukes (Trematoda) from Vientiane Province, Laos. Part I. Metacercariae. Ann Parasitol Hum Comp. 1990;65:238–243. doi: 10.1051/parasite/199267375. [DOI] [PubMed] [Google Scholar]
- 20.Sornmani S, Pathammavong O, Bunnag T, Impand P, Intarakhao C, Thirachantra S. An epidemiological survey of human intestinal parasites in Vientiane, Laos. Southeast Asian J Trop Med Public Health. 1974;5:541–546. [PubMed] [Google Scholar]
- 21.Tesana S, Srisawangwonk T, Kaewkes S, Sithithaworn P, Kanla P, Arunyanart C. Eggshell morphology of the small eggs of human trematodes in Thailand. Southeast Asian J Trop Med Public Health. 1991;22:631–636. [PubMed] [Google Scholar]
- 22.Velasquez CC. Heterophyidiasis. In: Steele JH, editor. CRC Handbook Series in Zoonoses, Section C: Parasitic Zoonoses. Vol. III (Trematode Zoonoses) Boca Raton, Florida, USA: CRC Press; 1982. pp. 99–107. [Google Scholar]
- 23.Yu SH, Mott KE. Epidemiology and morbidity of food-borne intestinal trematode infections. Trop Dis Bull. 1994;91:R125–R152. [Google Scholar]