Abstract
A common technique to aid in implant fixation into surrounding bone is to inject bone cement into the space between the implant and surrounding bone. The most common bone cement material used clinically today is poly(methyl methacrylate), or PMMA. Although promising, there are numerous disadvantages of using PMMA in bone fixation applications which has limited its wide spread use. Specifically, the PMMA polymerization reaction is highly exothermic in situ, thus, damaging surrounding bone tissue while curing. In addition, PMMA by itself is not visible using typical medical imaging techniques (such as X-rays required to assess new bone formation surrounding the implant). Lastly, although PMMA does support new bone growth, studies have highlighted decreased osteoblast (bone forming cell) functions on PMMA compared to other common orthopedic coating materials, such as calcium phosphates and hydroxyapatite. For these reasons, the goal of this study was to begin to investigate novel additives to PMMA which can enhance its cytocompatibility properties with osteoblasts, decrease its exothermic reaction when curing, and increase its radiopacity. Results of this study demonstrated that compared to conventional (or micron) equivalents, PMMA with nanoparticles of MgO and BaSO4 reduced harmful exothermic reactions of PMMA during solidification and increased radiopacity, respectively. Moreover, osteoblast adhesion increased on PMMA with nanoparticles of MgO and BaSO4 compared with PMMA alone. This study, thus, suggests that nanoparticles of MgO and BaSO4 should be further studied for improving properties of PMMA for orthopedic applications.
Keywords: bone cement, PMMA, Poly(methyl methacrylate), osteoblast, nanoparticles
Introduction
The long-term success of total joint replacements is largely dependent upon the incorporation of the implant with healthy surrounding bone tissue (ie, osseointegration). A common technique to aid in implant fixation into surrounding bone is to inject bone cement into the space between the implant and surrounding bone (Kuhn 2000). Such bone cements have been developed to be injected in liquid form and then solidify to mediate the attachment of the implant to bone.
The most common bone cement material used clinically today is poly(methyl methacrylate), or PMMA (Li et al 1995; Scripitz and Aspenberg 1999; Kuhn 2000). It is prepared at the clinical bed side by mixing PMMA powder, an initiator, and a monomer liquid, methyl methacrylate (MMA). Creating PMMA bone cement is analogous to mixing epoxy for daily use. Once mixed, the cement is liquid and, thus, can easily cover the implant after injection. PMMA continues to polymerize and cures in the empty space between the implant and bone providing stability to the implant.
Although promising, there are numerous disadvantages of using traditional PMMA in bone fixation applications which has limited its wide spread use. Specifically, the PMMA polymerization reaction is highly exothermic (as high as 80 °C in some cases) in situ, thus, damaging surrounding bone tissue (Biehl et al 1974; Fukushima et al 2002). In addition, PMMA is not visible using typical medical imaging techniques (such as X-rays required to assess new bone formation surrounding the implant). Thus, to monitor new bone growth surrounding PMMA after insertion, the radiopacity of PMMA can be increased by adding a common contrast agent (such as barium sulfate [BaSO4]) (Ginebra et al 2002). However, there are limitations on the amount of BaSO4 that can be added to PMMA since BaSO4 has been shown to adversely affect the mechanical and biocompatibility properties of PMMA at high concentrations (Bhambri et al 1995; Ginebra et al 2002). Lastly, although PMMA does support new bone growth, studies have highlighted decreased osteoblast (bone forming cell) functions on PMMA compared with other common orthopedic coating materials, such as calcium phosphates and hydroxyapatite (Glimcher 1987; Gauthier et al 1999; Barralet et al 2004; Gbureck et al 2004; Lilley et al 2005).
The goal of this study was to begin to investigate novel additives to PMMA which can enhance its cytocompatibility properties with osteoblasts, decrease its exothermic reaction when curing, and increase its radiopacity. Due to increased surface area, it is theorized here that nanoparticles of MgO may reduce exothermic reactions of polymers compared to micron particles of MgO and other chemistries. Moreover, while micron particles of BaSO4 are common additives to PMMA, researchers have hypothesized that due to increased surface area, nanoparticles of BaSO4 can improved X-ray contrast properties of PMMA (Wei and Ma 2004). Lastly, numerous studies have emerged demonstrating greater in vitro and in vivo bone growth on polymer composites containing nanoparticles (summarized in Liu et al 2005 and Liu and Webster 2007). Thus, PMMA with nanoparticles of MgO and BaSO4 may not only reduce heat released during PMMA solidification and enhance X-ray radiopacity, respectively, but they both may also simultaneously enhance osteoblast functions. For these reasons, the present study separately added MgO and BaSO4 nanoparticles to PMMA in an effort to improve its properties for orthopedic applications.
Materials and methods
PMMA cement preparation
Methyl methacrylate (MMA) was purchased from Polysciences (Warrington, PA). In order to create bone cement samples without any additives, five grams of MMA beads were added to an initiator (benzoyl peroxide; Sigma). For some of the samples, 10 percent (w/w) of the selected additives in conventional (or micron) and nanometer particulate form were added into the dissolved PMMA (Table 1). These additives, MgO and BaSO4, were purchased from Sigma-Aldrich (St. Louis, MO) and Reade Materials (Providence, RI), respectively (Table 2). Once the MMA beads were added to an initiator, they were allowed to solidify for 1 day. Prior to testing, all PMMA cements were sterilized by soaking in ethanol (5 minutes).
Table 1.
Chemical composition of the PMMA bone cements of interest to the present study
| Groups | PMMA | Conventional MgO | Nanoscale MgO | Conventional BaSO4 | Nanoscale BaSO4 |
|---|---|---|---|---|---|
| Group 1 | 5 g | – | – | – | – |
| Group 2 | 4.5 g | 0.5 g | – | – | – |
| Group 3 | 4.5 g | – | 0.5 g | – | – |
| Group 4 | 4.5 g | – | – | 0.5 g | – |
| Group 5 | 4.5 g | – | – | – | 0.5 g |
Abbreviation: PMMA, poly(methyl methacrylate).
Table 2.
Particulate size of PMMA additives
| Bone cement additive | Particulate size (Diameter) |
|---|---|
| Conventional MgO | 12 μm |
| Nanoscale MgO | 12.8 nm |
| Conventional BaSO4 | 2 μm |
| Nanoscale BaSO4 | 80–500 nm |
Abbreviation: PMMA, poly(methyl methacrylate).
PMMA characterization
Scanning electron microscopy and atomic force microscopy
To visualize the micron and nanoparticles of MgO and BaSO4 in the various PMMA samples, scanning electron microscopy (SEM) and atomic force microscopy (AFM) were used. Samples were mounted on stubs and sputter-coated with gold prior to examination using a Leo 1530-VP scanning electron microscope. To provide quantitative evidence of the difference in surface roughness, the substrates were also examined by AFM (Nanoscope IIIa, Veeco, CA) with scan areas of 1 μm × 1 μm. Commercially available AFM tips (radius of tip curvature was less than 10 nm, NSC15/ALBS, Micro-Masch, OR) were used in tapping mode. All roughness values (RMS or root mean square) were measured at least three times on each substrate and were repeated three times using installed software (Nanoscope 4.42, Veeco, CA).
Exothermic measurement
The change in temperature of the PMMA samples during solidification was determined by using a 4-channel DI-1000 thermocouple (DATAQ Instruments). Type T thermocouple leads (copper/constantan, 0.1 °C accuracy) were placed into the PMMA samples and the temperature change was recorded over various periods of time until the PMMA completely hardened. The temperature of pure PMMA cement at time zero was used as background recording. This temperature was subtracted from recorded temperatures for each type of PMMA cement at 1 second, 1 minute, 2 minutes, 10 minutes and at the end of recording (1 hour and 47 minutes).
Radiopacity
X-ray images of the various PMMA cement samples were taken after they solidified with an X-ray machine (General Electric) using a digital detector (40 kV, 63 mA, in air). X-rays were then analyzed using Image Pro software for pixel intensity.
Cell experiments
Cell cultures
Human osteoblasts (CRL-11372) were obtained from the American Type Culture Collection (ATCC) and were used at population numbers up to 3. Osteoblasts were cultured according to ATCC instructions in Dulbecco’s modified Eagle medium (DMEM; Gibco) supplemented with 10% fetal bovine serum (FBS; Hyclone) and 1% penicillin/streptomycin (P/S; Hyclone) under standard cell culture conditions (37 °C, humidified, 5% CO2/95% air environment).
Adhesion assay and fluorescence microscopy
Osteoblasts were seeded (3500 cells/cm2) in DMEM supplemented with 10% FBS and 1% P/S onto the substrates of interest to the present study and were placed in standard cell culture conditions for 4 hours. After 4 hours, nonadhered cells were removed by rinsing several times with phosphate-buffered saline (PBS). Adherent cells were then fixed with 4% formalin in PBS and their nuclei were stained with DAPI (Sigma). Cells were counted in five random fields per substrate and images were taken using a Zeiss Axiovert 200M light microscope (10 X objective) with image analysis software (Axiovision). The adhesion experiments were run in triplicate and repeated at least three different times per substrate.
Statistical analysis
Cell density (cells/mm2) on the substrates of interest were analyzed statistically using standard analysis of variance (ANOVA) techniques; statistical significance was considered at p < 0.05.
Results
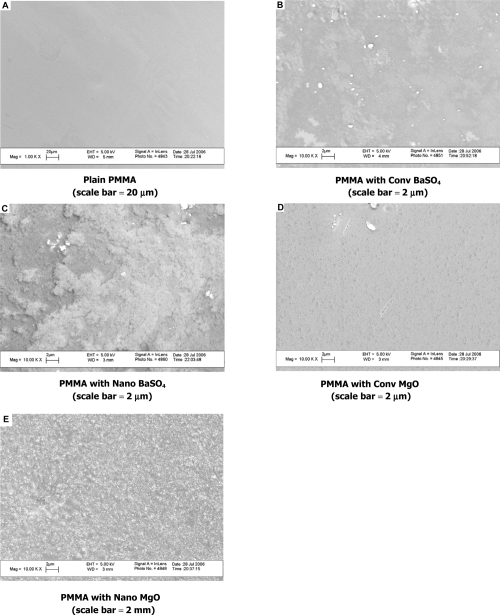
Scanning electron microscope images and atomic force microscopy data of PMMA cements
SEM images and AFM data provided evidence that pure PMMA possessed a very smooth surface with little to no micron and nanometer roughness (Figure 1 and Table 3). In contrast, the PMMA samples which contained either BaSO4 or MgO exhibited increased surface roughness. PMMA that contained nanophase particles possessed greater micron and nanometer roughness as compared to those with conventional particles.
Figure 1.
SEM images of PMMA with nano BaSO4 or nano MgO.
Table 3.
AFM surface roughness of PMMA cements
| PMMA bone cement sample | AFM RMS (nm) obtained through 1 by 1 μm AFM scans |
|---|---|
| Plain PMMA | 0 |
| PMMA with conventional MgO | 1.2 |
| PMMA with nanoscale MgO | 25.9 |
| PMMA with conventional BaSO4 | 4.2 |
| PMMA with nanoscale BaSO4 | 42.1 |
Abbreviations: AFM, atomic force microscopy; PMMA, poly(methyl methacrylate).
Reduced exothermic reaction for PMMA with nano MgO
Results of the present study demonstrated that PMMA samples which contained either BaSO4 or MgO (conventional or nanophase) exhibited lower increases in temperatures compared with pure PMMA while curing (Table 4). The drop in temperature was the most dramatic during the first 10 minutes of recording. More importantly, the PMMA sample which contained nanoparticles of MgO had the smallest temperature increase compared to any of the samples in this study. Specifically, compared to plain PMMA, PMMA with nanoparticles of MgO had −5.31 °C, −5.46 °C, −4.01 °C, −3.65 °C, and −2.95 °C temperature changes after 1 second, 1 minute, 2 minutes, 10 minutes, and 1 hour and 47 minutes of mixing, respectively. The temperature of PMMA after 1 second, 1 minute, 2 minutes, 10 minutes, and 1 hour and 47 minutes of mixing was 44.98 °C, 45.82 °C, 50.1 °C, 52.5 °C, and 47.85 °C, respectively.
Table 4.
Decreased PMMA exothermic reaction with nano MgO (ΔT °C compared to time after curing of PMMA alone)
| Sample | 1 sec | 1 min | 2 min | 10 min | 1hr 47 min |
|---|---|---|---|---|---|
| PMMA + 10 wt% conventional MgO | −1.65 °C** | −1.96 °C** | −1.81 °C** | −1.50 °C** | −0.45 °C** |
| PMMA + 10 wt% nanophase MgO | −5.31 °C*,** | −5.46 °C*,** | −4.01 °C*,** | −3.65 °C*,** | −2.95 °C*,** |
| PMMA + 10 wt% conventional BaSO4 | 0 °C | −0.60 °C | −0.45 °C | −0.15 °C | −0.15 °C |
| PMMA + 10 wt% nanophase BaSO4 | −0.15 °C* | −1.20 °C*,** | −1.05 °C*,** | −0.30 °C* | −0.15 °C |
Notes: p < 0.01 (compared with respective conventional additive) and
p < 0.01 (compared with PMMA alone).
Abbreviation: PMMA, poly(methyl methacrylate).
Increased radiopacity of PMMA cements with nano BaSO4
Results of this study further demonstrated that PMMA with nanoparticles of BaSO4 were more radiopaque than those with microparticles (Table 5). As expected, PMMA with either nanometer or micron particles of BaSO4 possessed increased X-ray intensity compared to PMMA alone. X-ray images showed that the order of the X-ray intensities of the samples were (first being the highest intensity): nanophase BaSO4 > conventional BaSO4 ≫ nanophase MgO > conventional MgO > pure PMMA.
Table 5.
Increased radiopacity of PMMA with nano BaSO4
| Sample | X-ray intensity (%) |
|---|---|
| PMMA + 10 wt% conventional MgO | 0.4 |
| PMMA + 10 wt% nanophase MgO | 0.5 |
| PMMA + 10 wt% conventional BaSO4 | 12.5** |
| PMMA + 10 wt% nanophase BaSO4 | 35.9*,** |
Notes: p < 0.01 (compared with respective conventional additive) and
p < 0.01 (compared with PMMA alone). X-rays taken with a digital detector (40 kV, 63 mA, in air).
Abbreviation: PMMA, poly(methyl methacrylate).
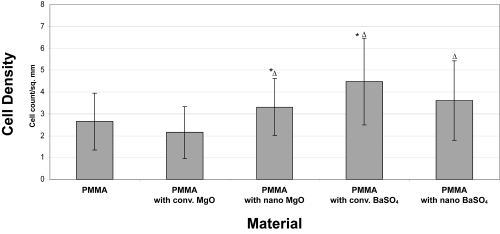
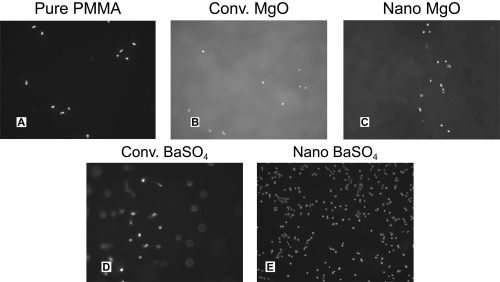
Increased osteoblast adhesion on PMMA with nano MgO and BaSO4
Lastly, results of this study demonstrated that the PMMA cement samples with nanophase MgO and nanophase BaSO4 had higher cell densities than the pure PMMA cement samples (p < 0.1) (Figures 2 and 3). Interestingly, while osteoblast adhesion was greater on PMMA with nanophase compared to conventional MgO, it was similar on PMMA with nanophase compared to conventional BaSO4. Moreover, the PMMA cement samples with conventional BaSO4 had a significantly higher cell density than those with conventional MgO.
Figure 2.
Increased osteoblast adhesion on PMMA with either nano MgO or conventional/nano BaSO4. Data = mean ± SEM; n = 3; Δ p < 0.1 (compared to PMMA alone and PMMA with conventional MgO); *p < 0.01 (compared to PMMA with conventional MgO).
Figure 3.
Increased osteoblast adhesion on PMMA with either nano MgO or conventional/nano BaSO4 (mag. = 100X).
Discussion
PMMA possesses attractive properties for orthopedic applications, but it has three major drawbacks. The first shortcoming of PMMA is its strong exothermic properties from its monomer methyl methacrylate (MMA). A significant amount of heat is produced when MMA polymerizes. In vitro testing of pure MMA demonstrated that the temperature can reach up to 100 °C. Because of this tremendous heat release, the composition of commercial bone cement has been modified to have polymer/monomer ratios of 2/1 (w/w) which ensures less heat release and a smaller volume change (Kuhn 2000). However, the temperature at the bone-cement interface is still above the physiological range (43 ~ 46 °C), which could cause surrounding tissue death (Kuhn 2000).
Magnesium oxide (MgO) is a ceramic that has seldom been used in the orthopedic industry due to its poor mechanical properties possesses. However, nanoparticles of MgO could potentially reduce heat generation since the overall surface area and dispersion of such nanoparticles is much higher than that of micron-sized particles. That is, by exposing more surface area, nanoparticles in general can decrease exothermic reactions of bone cements. This was confirmed in the current study where it was found that PMMA cement samples which contained either MgO (or BaSO4) dramatically decreased temperature increases during PMMA solidification. Importantly, the temperature drops were significantly larger when nanoparticles were present instead of conventional (or micron-sized) particles.
Another disadvantage of PMMA as an orthopedic material is its radiolucency (Bhambri et al 1995; Ginebra et al 2002). Since X-rays are used to monitor the bone healing process, identifying osteolytic lesions around an implant, and detecting fractures in the bone cement after surgery, radiolucent PMMA cements presents a challenge. Conventionally, two heavy metal ion salts (barium sulfate or zirconium dioxide (ZrO2) have been added to bone cements to increase its X-ray contrast; both in micron particle form (Bhambri et al 1995; Ginebra et al 2002). However, adding micron sized metal ions adversely affects the biological and mechanical properties of PMMA (Bhambri et al 1995; Ginebra et al 2002). For example, micron-sized particles of BaSO4 decreased the tensile strength of bone cements from 45 MPa to 36 MPa (Ginebra et al 2002). BaSO4 micron agglomerates serve as initiation sites for fatigue cracks. It has also been found that PMMA wear particles that contain micron-sized BaSO4 and ZrO2 particles cause more bone resorption than pure PMMA wear particles; this has lead to increased osteolysis when micron-sized BaSO4 and ZrO2 particles are used in PMMA (Liu-Synder and Webster 2007). In addition, although more testing is needed, recent studies have demonstrated less adverse reactions of ceramic nanoparticulate compared to micron wear debris (Liu-Synder and Webster 2007). Therefore, the present study investigated the possibility of replacing micron with nanoparticles of BaSO4. X-ray images of PMMA cement samples showed that the highest radiopacity was obtained when using nanoparticles compared to micron particles of BaSO4. Any improvements in X-ray image contrast will not only shorten hospital stay but also reduce a patients’ exposure to X-rays. X-ray exposure has been linked to increased risk of cancer (Liu-Synder and Webster 2007), thus, increased radiopacity of bone cements will allow for a reduced patients’ exposure to X-rays and consequently lead to a lower incidence of cancer.
Lastly, the most challenging issue associated with commercially available PMMA cements is their poor osseointegration (Glimcher 1987; Gauthier et al 1999; Barralet et al 2004; Gbureck et al 2004; Lilley et al 2005). PMMA additives (such as antibiotics and radiopacifiers) have been shown in the past to adversely affect osseointegration (Liu-Synder and Webster 2007). Therefore, whenever a new material is added into PMMA, the resulting PMMA cements should be tested for cytocompatibility properties. Results of the present study demonstrated that osteoblast adhesion was higher on PMMA cements with either nanophase MgO or conventional and nanophase BaSO4 than pure PMMA cement. Results of improved osteoblast adhesion on PMMA with nanometer compared to micron particles of MgO confirms that of other studies which have shown greater osteoblast functions on nanometer compared with conventional ceramics, metals, polymers, and composites (Liu-Synder and Webster 2007). However, future investigations will be needed to elucidate why greater osteoblast adhesion was not observed on nanometer compared with micron BaSO4 added to PMMA. Perhaps sonication or other processing conditions will have to be modified to amplify the degree of nanometer roughness when using nanoparticles of BaSO4 in PMMA. Previous studies have shown greater dispersion of nanoparticles in polymers promotes osteoblast functions (Liu-Synder and Webster 2007). Furthermore, although osteoblast adhesion is a prerequisite for mineral deposition, longer-term functions of osteoblasts will have to be determined on the PMMA samples of interest to this study.
In the current study, the additives (MgO an BaSO4) were used at 10% (w/w) per total PMMA cement. Little information is known about the optimal composition for both MgO and BaSO4 in PMMA and this needs to be further investigated. In addition, the current study was performed when MgO and BaSO4 were added separately to PMMA. It is intriguing to ponder whether PMMA cement with both nano MgO and nano BaSO4 would combine the benefits of reduced exothermic reaction, increased radiopacity, and greater osteoblast functions.
Importantly, there are also other examples in the literature of using nanoparticles in PMMA to improve bone cement properties. For example, nano sized alumina and titania powder filled PMMA cements have improved mechanical properties compared to commercial PMMA cements (Liu-Snyder and Webster 2007). In addition, (5 % wt) nanophase alumina-PMMA composites (alumina nanoparticles were coated with a layer of (3-acryloxypropyl) dimethylmethoxysilane (Gelest Inc.) before they were mixed and sonicated with MMA) exhibited a 28% increased tensile strength over pure PMMA (Liu-Snyder and Webster 2007). Also, the thermal conductivity of polymer-carbon nanotube (CNT) composites increased 2.5-fold with the presence of a small amount of CNTs (1% v/v) (Liu-Snyder and Webster 2007). CNT fillers can also help PMMA cements achieve better mechanical properties and promote bone cell growth and functions (Liu-Snyder and Webster 2007).
In summary, Lee and colleagues claimed in 1977 that “for the immediate future, refinements in the technical use of [bone] cements are likely to prove more fruitful than changes in the cement itself” (Liu-Synder and Webster 2007). Over the last few decades, many modifications have been made to bone cements. But as our knowledge of nanotechnology expands exponentially, we envision a breakthrough in bone cement properties which will ensure long-term survival of joint implants in the body.
Acknowledgments
The authors would like to thank Mr Geoffrey Williams for his assistance with fluorescence microscopy imaging as well as Dr Karen Haberstroh and the Undergraduate Translational Research Program at Brown University.
References
- Barralet JE, Lilley KJ, Grover LM, et al. Cements from nanocrystalline hydroxyapatite. J Mater Sci Mater Med. 2004;15:407. doi: 10.1023/b:jmsm.0000021111.48592.ab. [DOI] [PubMed] [Google Scholar]
- Bhambri SK, Gilbertson LN. Micromechanisms of fatigue crack initiation and propagation in bone cements. J Biomed Mater Res. 1995;29:233–7. doi: 10.1002/jbm.820290214. [DOI] [PubMed] [Google Scholar]
- Biehl G, Harms J, Hanser U. Experimentelle untersuchungen über die wärmeentwicklung im knochen bei der polymerisation von knochenzement. Arch Orthop Unfallchir. 1974;78:62. doi: 10.1007/BF00417083. [DOI] [PubMed] [Google Scholar]
- Gauthier O, Bouler JM, Weiss P, et al. Kinetic study of bone ingrowth and ceramic resorption associated with the implantation of different injectable calcium-phosphate bone substitutes. J Biomed Mater Res. 1999;47:28. doi: 10.1002/(sici)1097-4636(199910)47:1<28::aid-jbm4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Gbureck U, Barralet JE, Hofmann MP, et al. Nanocrystalline tetracalcium phosphate cement. J Dent Res. 2004;83:425. doi: 10.1177/154405910408300514. [DOI] [PubMed] [Google Scholar]
- Ginebra MP, Albuixech L, Fernandez-Barragan E, et al. Mechanical performance of acrylic bone cements containing different radiopacifying agents. Biomaterials. 2002;23:1873–82. doi: 10.1016/s0142-9612(01)00314-3. [DOI] [PubMed] [Google Scholar]
- Glimcher MJ. PMMA. Instr Course Lect. 1987;36:49. [PubMed] [Google Scholar]
- Fukushima H, Hashimoto Y, Yoshiya S, et al. Conduction analysis of cement interface temperature in total knee arthroplasty. Kobe J Med Sci. 2002;48:63. [PubMed] [Google Scholar]
- Kühn K-D. Bone Cements, Up-to-Date Comparison of Physical and Chemical Properties of Commercial Materials. Berlin: Springer Verlag; 2000. pp. 12–20. [Google Scholar]
- Li J, Fartash B, Hermansson L. Hydroxyapatite – alumina composites and bone-bonding. Biomaterials. 1995;16:417. doi: 10.1016/0142-9612(95)98860-g. [DOI] [PubMed] [Google Scholar]
- Lilley KJ, Gbureck U, Knowles JC, et al. Alkali ion substituted calcium phosphate cement formation from mechanically activated reactants. J Mater Sci Mater Med. 2005;16:455. doi: 10.1007/s10856-005-6982-7. [DOI] [PubMed] [Google Scholar]
- Liu H, Slamovich EB, Webster TJ. Increased osteoblast functions on poly-lactic-co-glycolic acid with highly dispersed nanophase titania. J Biomed Nanotech. 2005;1:83–9. doi: 10.1088/0957-4484/16/7/038. [DOI] [PubMed] [Google Scholar]
- Liu H, Webster TJ. Nanomedicine for implants: A review of studies and necessary experimental tools. Biomaterials. 2007;28:354–69. doi: 10.1016/j.biomaterials.2006.08.049. [DOI] [PubMed] [Google Scholar]
- Liu-Synder P, Webster TJ. Developing a new generation of bone cements with nanotechnology. Clin Trend Nanotech. 2007 in press. [Google Scholar]
- Skripitz R, Aspenberg P. Attachment of PMMA cement to bone: force measurements in rats. Biomaterials. 1999;20:351. doi: 10.1016/s0142-9612(98)00175-6. [DOI] [PubMed] [Google Scholar]
- Wei G, Ma PX. Structure and properties of nano-hydroxyapatite/polymer composite scaffolds for bone tissue engineering. Biomaterials. 2004;25:4749. doi: 10.1016/j.biomaterials.2003.12.005. [DOI] [PubMed] [Google Scholar]