Abstract
Lipomas are the most common benign tumors of soft tissues. However, conventional lipomas have been reported only rarely as presenting in the vulva. We present a case of vulvar lipoma in a 17-yr-old woman, possibly caused by chronic intermittent irritation.
Keywords: Lipoma, Vulvar Neoplasms, Vulva, Adolescent
INTRODUCTION
Benign tumors of the vulva are normally classified according to their origin as epithelial cell tumors (e.g., keratinocytic, adnexal and ectopic tumors), or mesenchymal cell tumors (e.g., vascular, fibrous, muscular, neural, adipose and melanocytic tumors) (1). Although lipomas are the most common benign tumors in soft tissues derived from mesenchymal cells, for the vulva they are so rare that there are very few reports. Here we document a case of such a rare large vulvar lipoma in an adolescent with a review of the literature.
CASE REPORT
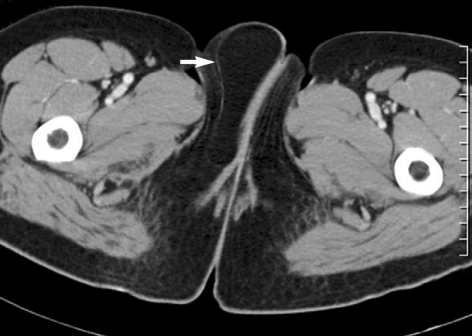
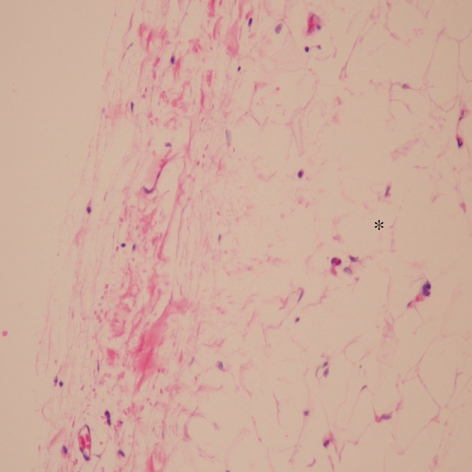
A 17-yr-old woman, a Tae Kwon Do practitioner, presented to our hospital complaining of a soft, movable mass in the right labia majora (Fig. 1). She reported that it caused discomfort when she exercised. The mass had grown gradually over one year. There was no family history or abnormality in the laboratory tests that could serve as a good reference. Using ultrasonography and computed tomography (CT) scans (Fig. 2), an encapsulated fatty mass was detected on the right labia majora. Tumorectomy was carried out under general anesthesia. Incision was made along the lateral margin of mucosa on the right vulva longitudinally as to conceal the scar from being visible. Mass including 1-cm width of skin strap on the lateral area from the incision line was extracted carefully. There was no difficulty in surgery because the mass was well-encapsulated. After the removal, an evacuator Barovac® (closed suction drainage system) was applied and secure suturing was followed by compressive dressing. The excised specimen measured 8.2 × 5.5 × 3.8 cm and it was surrounded by a fibrous capsule. Serial histological sections showed lobulated and homogeneous mature adipose tissue (Fig. 3), and the histopathologic diagnosis was of a lipoma.
Fig. 1.
Mass on the right labia majora.
Fig. 2.
CT scan in the level of external genitalia reveals a lipomatous mass (arrow).
Fig. 3.
The tumor consisted of mature adipocytes (*). Hematoxylin and Eosin staining, ×200.
DISCUSSION
The most common areas for lipomas, the most common benign tumor in soft tissues, are the upper back, neck, shoulder and abdomen. Lipomas have been identified in all age groups, but usually first appear between 40 and 60 yr of age. Whereas solitary lipomas are more common in women, the presence of multiple lipomas (lipomatosis) is more common in men. Variants seen include spindle cell lipomas, pleomorphic lipomas, angiolipomas and adenolipomas.
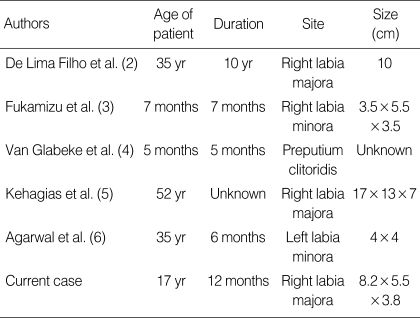
There are very few reports on conventional lipomas in the vulva (Table 1). In 1969, De Lima Filho et al. (2) reported a case of a 35-yr-old woman. In 1982, Fukamizu et al. (3) reported a case of a large pedunculated vulvar lipoma in an infant, which had been present since birth. In 1999, Van Glabeke et al. (4) reported a case of a neonate with a vulvar lipoma observed in the preputium clitoridis. Kehagias et al. (5) described CT findings for a large pedunculated vulvar lipoma measuring 17 × 13 × 7 cm in a 35-yr-old woman and concluded that ultrasound, CT and magnetic resonance imaging (MRI) were useful tools to reveal the lipomatous consistency of these tumors and to differentiate them from vulvar cysts. The most recent report by Agarwal et al. in 2004 (6) described a 35-yr-old woman with a lipoma arising from the left labia minora.
Table 1.
Cases of conventional vulvar lipomas reported in the literature
Most reported cases of vulvar lipomas involved adults were tumors that had presented since birth. However, our case here was of a conventional lipoma in the vulva of an adolescent 17-yr-old Tae Kwon Do practitioner. Although lipomas are well-known fatty tumors both clinically and pathologically, their precise etiology is unknown. However, one of the most commonly implicated etiologic factors is trauma (7). Copcu (8) reported that chronic minor traumas might trigger the formation and enlargement of lipomas, and described two cases of sport-induced scapular lipomas in a volleyball player and a table tennis player. Our patient mentioned discomforts when kicking due to the mass of the vulva. This may be regarded to show the relationship between the formation or enlargement of lipomas and chronic irritation caused by activities such as kicking. We speculate that the lipoma in this patient arose from chronic intermittent irritation of the soft tissue in the vulva caused by kicking.
Vulvar lipomas need to be differentiated from liposarcomas, which develop rarely but are very similar to lipomas clinically (9). Recently, CT and MRI have been used with some success to differentiate the two (10). To exclude the possibility of malignant tumors, biopsy should be performed by surgical excision. To our knowledge, this is the first case of a conventional vulvar lipoma reported in an adolescent.
References
- 1.Haley JC, Mirowski GW, Hood AF. Benign vulvar tumors. Semin Cutan Med Surg. 1998;17:196–204. doi: 10.1016/s1085-5629(98)80014-x. [DOI] [PubMed] [Google Scholar]
- 2.De Lima Filho OA, Cogliati AO, Reitzfeld G. Lipoma of the vulva. Rev Paul Med. 1969;75:165–176. [PubMed] [Google Scholar]
- 3.Fukamizu H, Matsumoto K, Inoue K, Moriguchi T. Large vulvar lipoma. Arch Dermatol. 1982;118:447. [PubMed] [Google Scholar]
- 4.Van Glabeke E, Audry G, Hervet F, Josset P, Gruner M. Lipoma of the preputium clitoridis in neonate: an exceptional abnormality different from ambiguous genitalia. Pediatr Surg Int. 1999;15:147–148. doi: 10.1007/s003830050541. [DOI] [PubMed] [Google Scholar]
- 5.Kehagias DT, Smyrniotis VE, Karvounis EE, Gouliamos AD, Creatsas G. Large lipoma of the vulva. Eur J Obstet Gynecol Reprod Biol. 1999;84:5–6. doi: 10.1016/s0301-2115(98)00247-4. [DOI] [PubMed] [Google Scholar]
- 6.Agarwal U, Dahiya P, Sangwan K. Vulval lipoma: a rare occurrence. Arch Gynecol Obstet. 2004;270:59–60. doi: 10.1007/s00404-002-0452-y. [DOI] [PubMed] [Google Scholar]
- 7.Signorini M, Campiglio GL. Posttraumatic lipomas: where do they really come from? Plast Reconstr Surg. 1998;101:699–705. doi: 10.1097/00006534-199803000-00017. [DOI] [PubMed] [Google Scholar]
- 8.Copcu E. Sport-induced lipoma. Int J Sports Med. 2004;25:182–185. doi: 10.1055/s-2003-45254. [DOI] [PubMed] [Google Scholar]
- 9.Nucci MR, Fletcher CD. Liposarcoma (atypical lipomatous tumors) of the vulva: a clinicopathologic study of six cases. Int J Gynecol Pathol. 1998;17:17–23. doi: 10.1097/00004347-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Einarsdottir H, Söderlund V, Larsson O, Mandahl N, Bauer HC. 110 subfascial lipomatous tumors: MR and CT findings versus histopathological diagnosis and cytogenetic analysis. Acta Radiol. 1999;40:603–609. doi: 10.3109/02841859909175595. [DOI] [PubMed] [Google Scholar]