Abstract
Although enhanced appetite and weight gain are potential side effects of treatment with antipsychotic agents, particularly olanzapine and clozapine, the mechanisms underlying these side effects are poorly understood. Leptin and ghrelin were recently identified as hormones that play crucial roles in the regulation of energy balance and glucose metabolism. To elucidate relationships between weight change and plasma levels of ghrelin and leptin, we investigated the circulating ghrelin and leptin levels and body weight during olanzapine treatment. Twenty-four patients with schizophrenia were examined during 6-month administration of olanzapine. Ghrelin, leptin, weight and body mass index (BMI) were measured before and after 2, 4, 8, 12, 16, and 24 weeks of olanzapine treatment. The concentration of glucose and various lipid metabolic parameters were measured at baseline and at 24 weeks. Significant increases in weight, BMI and leptin were observed at week 24. On the other hand, the serum levels of ghrelin decreased significantly after olanzapine treatment. In addition, the level of ghrelin was negatively correlated with the leptin level, BMI and weight. The leptin level was positively correlated with both BMI and weight. Ghrelin is associated with metabolic changes, in combination with leptin, during olanzapine treatment. However, further large-scale and longitudinal studies are warranted to elucidate the metabolic changes involving ghrelin, leptin and insulin during treatment with antipsychotics.
Keywords: Olanzapine, Weight Gain, Ghrelin, Leptin, Schizophrenia
INTRODUCTION
Schizophrenia is a devastating emotional, physical and mental disorder. One percent of the US population is afflicted with schizophrenia, and antipsychotics have become the first-line treatment for schizophrenia as well as for other psychotic disorders (1). Recently developed antipsychotics generally possess a similar efficacy compared to older antipsychotics, but they have a better side-effect profile, especially with regard to extrapyramidal symptoms and tardive dyskinesia (2). The increased use of second-generation antipsychotics over the last decade has raised concerns about their metabolic side effects, such as weight gain, diabetes and dyslipidemia (3, 4).
Obesity, dyslipidemia and diabetes have serious implications for overall health and survival because they are associated with an increased risk for cardiovascular and malignant disorders (5). In addition, medication-induced weight gain has been associated with a lower quality of life (6) and non-compliance (7), which increases the risk for relapse (8). Among the atypical antipsychotics, significantly more weight gain occurred during treatment with olanzapine than with other antipsychotics (9). However, the mechanisms of weight gain and dyslipidemia are poorly understood, and various parts of the endocrine system are presumably involved in these side effects.
The hypothalamus has been recognized as a major site of energy homeostasis in the central nervous system (10). Recent studies have shown that the hormones leptin and ghrelin are crucial elements of the hypothalamic neurocircuitry. Leptin is one of a number of cytokine-like molecules synthesized in adipose tissue. It is actively transported into the hypothalamus, where it acts to limit food intake (11). It also directly influences insulin secretion (12). Thus, leptin has been intensively investigated with respect to its association with changes in weight and glucose metabolism during treatment with various antipsychotics (13). Ghrelin is a recently discovered orexigenic hormone that is primarily secreted by the stomach and duodenum, and it has been implicated in both meal-time hunger and the long-term regulation of body weight (14). Ghrelin is currently recognized as the main endogenous ligand for growth hormone secretagogue receptors, as well as other regulatory factors in growth hormone (GH) secretion and energy balance (15). The levels of circulating ghrelin are increased under conditions of starvation and in anorexia nervosa, but decreased under conditions of feeding and in obesity (16, 17). Ghrelin has been shown to play crucial roles in the regulation of energy balance and glucose metabolism in combination with leptin. Ghrelin and leptin may have opposite actions in the regulation of body weight (18).
This study was designed to investigate the relationships between weight gain and plasma levels of ghrelin and leptin because the correlation between olanzapine-induced weight gain and changes in plasma levels of ghrelin and leptin was not fully described in previous studies.
MATERIALS AND METHODS
Subjects
The subjects of this study were 24 male in-patients in the Department of Psychiatry at Hadong Wooridle Hospital in Korea who fulfilled the DSM-IV diagnostic criteria for schizophrenia. We chose to study only males because gender differences in the effects of antipsychotic drugs on weight have not been fully investigated. The exclusion criteria were: 1) patients who had a substance-related disorder or other physical illness, including hypertension or hyperlipidemia, that might affect their appetite or glucose metabolism; 2) significant weight loss/gain ±1 kg in the past 8 weeks. The patients underwent a screening evaluation followed by a washout period of up to 2 weeks if they had received any antipsychotic medication. Each subject was informed of the purpose, procedures, and potential risks of participation in the study before signing an informed consent form.
Procedure
Olanzapine was initially administered at a dose of 5-20 mg once daily. The dose was increased at weekly intervals based on clinical improvement. Benzodiazepines were permitted to control nonpsychotic symptoms like anxiety. Body weight, body mass index (BMI) and plasma levels of ghrelin and leptin were assessed at baseline and after 2, 4, 8, 12, 16, and 24 weeks. Glucose, total cholesterol, high density lipoprotein (HDL)-cholesterol, low density lipoprotein (LDL)-cholesterol and triglyceride levels were assessed at baseline and at 24 weeks. All meals were prepared and provided by the kitchen staff at Wooridle Hospital.
Blood samples
The author collected 10-12 mL venous blood samples between 7:00 am and 8:00 am after overnight fasting. The samples were immediately analyzed for glucose, total cholesterol, HDL-cholesterol, LDL-cholesterol, and triglycerides. The samples to be analyzed for ghrelin and leptin were immediately centrifuged and stored at -80℃ until thawing for analysis. Plasma concentrations of ghrelin and leptin were determined using a commercially available radioimmunoassay system at Gyeongsang National University (ghrelin: LINCO Research Inc., Mo, U.S.A.; Leptin: LINCO Research, Mo, U.S.A.).
Statistics
Analysis of variance (ANOVA) with repeated measure was used to evaluate ghrelin, leptin, weight and BMI at the medication-free stage and after treatment in those subjects who had data for all of the time points. Differences in glucose, total cholesterol, HDL-cholesterol, LDL-cholesterol and triglyceride levels before and after olanzapine treatment were compared using the paired t-test. Pearson correlation coefficient analyses were used to examine the correlation between changes in weight, BMI, ghrelin and leptin levels following treatment with olanzapine. p<0.05 was considered statistically significant in all analyses. All statistical analyses were performed using SPSS software (version 11.0).
RESULTS
A total of 24 patients with schizophrenia met our inclusion criteria. Most of the patients were diagnosed with paranoid schizophrenia according to DSM-IV diagnostic criteria for subtypes of schizophrenia. The only other subtype observed in our patients was undifferentiated schizophrenia. All patients completed the full 24-week study. The mean age of the patients treated with olanzapine was 34.3±6.5 yr. The mean daily dose used by the patients at week 24 was 11.7±3.1 mg.
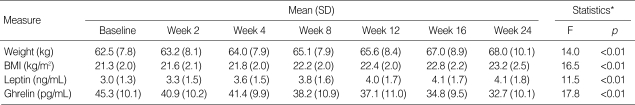
The changes in ghrelin, leptin, weight and BMI are shown in Table 1. The BMI (F=16.5, p<0.001) and weight (F=14.0, p<0.001) of the patients increased significantly during the period of treatment with olanzapine. The patients were an average 5.5 kg heavier at week 24 than they were at baseline. Plasma leptin levels also increased significantly during olanzapine treatment (F=11.5, p<0.001). However, plasma ghrelin levels decreased significantly (F=17.8, p<0.001).
Table 1.
Body weight, body mass index (BMI), plasma leptin levels and ghrelin levels in patients with schizophrenia during olanzapine treatment
*, ANOVA with repeated measures. BMI, body mass index.
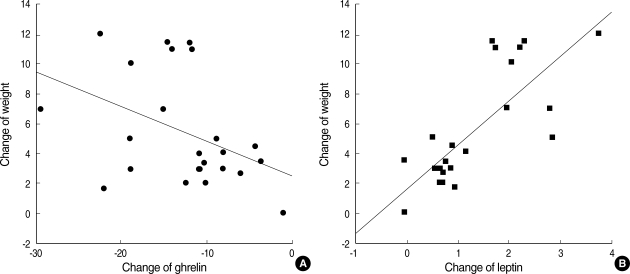
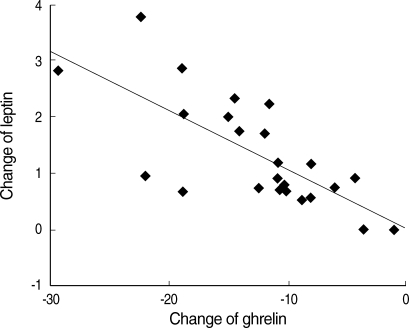
The change in plasma ghrelin levels was significantly correlated with the changes in BMI (r=-0.481, p=0.017) and weight (r=-0.411, p=0.046) (Fig. 1A), while the change in plasma leptin levels was significantly correlated with the changes in BMI (r=0.784, p<0.001) and weight (r=0.773, p<0.001) (Fig. 1B). The level of ghrelin (r=-0.724, p<0.001) correlated negatively with the level of leptin (Fig. 2).
Fig. 1.
Correlation between changes in the plasma levels of ghrelin (pg/mL) and leptin (ng/mL) and body weight (kg) in patients with schizophrenia during 24 weeks of treatment with olanzapine. Ghrelin and body weight (A), leptin and body weight (B). The change in weight was significantly correlated with the change in the plasma levels of ghrelin (r=-0.411, p=0.046) and the plasma levels of leptin (r=0.773, p<0.001).
Fig. 2.
Correlation between the changes in the circulating plasma levels of ghrelin (pg/mL) and leptin levels (ng/mL) in patients with schizophrenia during 24 weeks of treatment with olanzapine. The change in plasma levels of leptin was significantly correlated with the change in plasma levels of ghrelin (r=-0.724, p<0.001).
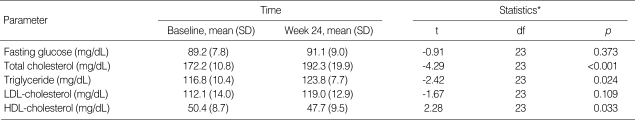
The level of glucose and lipid metabolic parameters in patients with schizophrenia during olanzapine treatment are shown in Table 2. The concentrations of glucose (t=-0.91, df=23, p=0.373) and LDL-cholesterol (t=-1.67, df=23, p=0.109) did not change significantly from the baseline values after 24 weeks. However, the concentrations of total cholesterol (t=-4.293, df=23, p<0.001), HDL-cholesterol (t=2.28, df=23, p=0.033) and triglycerides (t=-2.42, df=23, p=0.024) changed significantly.
Table 2.
The levels of glucose and lipid metabolic parameters in patients with schizophrenia during olanzapine treatment
*, paired t-test.
LDL, low density lipoprotein; HDL, high density lipoprotein; SD, standard deviation.
DISCUSSION
Many reports have suggested that olanzapine induces weight gain (19). However, the mechanism behind this weight gain remains unclear. It was recently found that appetite and body weight are controlled by complex hypothalamic neurocircuitry, and that the hormones leptin and ghrelin are crucial elements of this control system. The circulating concentration of leptin is directly proportional to adiposity and functions within the hypothalamus to limit food intake, while ghrelin is synthesized in the stomach and functions within the hypothalamus to stimulate food intake (20-22). A few studies investigated the association of leptin and ghrelin with weight changes and glucose metabolism during treatment with antipsychotics. Previous studies have reported an increase in circulating leptin in patients treated with olanzapine (23, 24). However, Hosojima et al. reported that ghrelin levels decreased after the initiation of olanzapine therapy and suggested that ghrelin is associated with metabolic changes in combination with leptin, during treatment with olanzapine (25). Potential limitations of previous studies include the relatively short duration of exposure and the evaluation of a relatively small number of subjects. Thus, we conducted a prospective study using the changes in plasma levels of ghrelin, leptin and body weight to elucidate the relations with each other behind the weight gain observed in 24 patients with schizophrenia after 24 weeks of treatment with therapeutic doses of olanzapine.
In the present study, we demonstrated that plasma ghrelin levels decreased significantly during olanzapine treatment, while plasma leptin levels and BMI increased significantly during treatment with olanzapine. Leptin has been intensively investigated with respect to association with obesity induced antipsychotics. Previous studies have reported an increase in leptin in subjects treated with olanzapine (23). And this was corroborated by our results. Results of the present study correspond with the results of earlier studies which reported that ghrelin was reduced in obesity and weight gain. Tschop et al. reported that, in humans, fasting plasma ghrelin was reduced in obese subjects in comparison to lean subjects (26). In rodents, subcutaneous, intracerebroventricular and intraperitoneal administration of ghrelin stimulates feeding, reduces fat utilization and increases body weight (27, 28). Furthermore, Hansen et al. reported that ghrelin is suppressed in most cases of obesity and is not a causal factor in the pathogenesis of obesity (29). These data seem to indicate that ghrelin is downregulated as a consequence of excess energy in obese subjects. Therefore, we suggest that ghrelin may be downregulated as a consequence of obesity induced by olanzapine, showing a normalizing effect on energy homeostasis and metabolic change induced by olanzapine.
Another finding is that the level of ghrelin is negatively correlated with the level of leptin, BMI, and weight. Ghrelin and leptin secretions are apparently regulated by disparate mechanisms because no temporal synchrony was observed in the episodic discharge of these hormones in sated rats (30). However, Kalra et al. reported that fasting increased ghrelin secretion by triggering high-amplitude pulses at a greater frequency in synchrony with leptin pulses of markedly reduced amplitude (31). In addition, Ueno et al. found that the increased ghrelin expression in ob/ob mice was downregulated by leptin administration and suggested that leptin is an upstream regulator of gastric ghrelin (32). These studies support our result that ghrelin levels are negatively correlated with the leptin levels. Our results are consistent with previous studies, suggesting that ghrelin is downregulated by increased leptin following weight gain induced by olanzapine.
In this study, no significant changes in the levels of glucose and LDL-cholesterol were observed. However, serum levels of HDL-cholesterol, total cholesterol and triglycerides changed significantly. In a previous study, Huang et al. reported that triglyceride levels increased significantly 3 weeks after treatment with olanzapine (33). Furthermore, Brown and Estoup reported that olanzapine-treated patients showed adverse changes in all measured metabolic parameters, with increases in total cholesterol and triglycerides reaching a statistical significance (34). In addition, several previous studies have emphasized that individuals most at risk for the development of coronary heart disease are those with combined dyslipidemia (35). The results of our study and previous studies indicate that regular health screenings are needed in patients with schizophrenia. These findings also suggest that psychiatrists should discuss the potentially serious side effects of olanzapine with patients prior to initiating treatment and provide psychoeducation concerning the management of the metabolic side effects of olanzapine.
A possible first limitation of this study is that only male patients were included. Second limitation of this study is that all of the subjects in this study were within the normal weight range, although the patients with schizophrenia patients tended to have higher body weights than the healthy individuals. Therefore, the generalization of these results to all schizophrenia is limited. Third limitation is that Benzodiazepines were permitted to control the nonpsychotic symptoms. Even though these are not known to affect appetite and glucose metabolism definitely, There are some possibility of risk to increase appetite (36) and might affect the result of this study. Additionally, feeding behavior is extremely complicated because it involves many factors, including emotion, memory, learning, and various cognitive factors. However, in this study, the possible existence of many physiological and behavioral factors that modulate weight gain was not considered. Therefore, further long-term studies must be conducted taking these factors into consideration.
In summary, treatment with olanzapine is associated with weight gain and increases in BMI. Ghrelin correlates negatively with weight gain and BMI during olanzapine treatment. Leptin, on the other hand, shows a positive correlation with weight gain and BMI during olanzapine treatment. However, the generalization of the study results to all patients with schizophrenia is limited because various parts of the endocrine system and genetic factors are presumably involved in the effect of antipsychotics on weight gain. Therefore, further large-scale and longitudinal studies are warranted to evaluate the many processes involving ghrelin and leptin during treatment with olanzapine and other antipsychotics.
References
- 1.De Oliveira IR, Juruena MF. Treatment of psychosis: 30 years of progress. J Clin Pharm Ther. 2006;31:523–534. doi: 10.1111/j.1365-2710.2006.00784.x. [DOI] [PubMed] [Google Scholar]
- 2.Markowitz JS, Brown CS, Moore TR. Atypical antipsychotics. Part I: Pharmacology, pharmacokinetics, and efficacy. Ann Pharmacother. 1999;33:73–85. doi: 10.1345/aph.17215. [DOI] [PubMed] [Google Scholar]
- 3.Casey DE, Zorn SH. The pharmacology of weight gain with antipsychotics. J Clin Psychiatry. 2001;62(Suppl 7):4–10. [PubMed] [Google Scholar]
- 4.Kinon BJ, Basson BR, Gilmore JA, Tollefson GD. Long-term olanzapine treatment: weight change and weight-related health factors in schizophrenia. J Clin Psychiatry. 2001;62:92–100. [PubMed] [Google Scholar]
- 5.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348:1625–1638. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 6.Allison DB, Mackell JA, McDonnell DD. The impact of weight gain on quality of life among persons with schizophrenia. Psychiatr Serv. 2003;54:565–567. doi: 10.1176/appi.ps.54.4.565. [DOI] [PubMed] [Google Scholar]
- 7.Weiden PJ, Mackell JA, McDonnell DD. Obesity as a risk factor for antipsychotic noncompliance. Schizophr Res. 2004;66:51–57. doi: 10.1016/s0920-9964(02)00498-x. [DOI] [PubMed] [Google Scholar]
- 8.Robinson DG, Woerner MG, Alvir JM, Geisler S, Koreen A, Sheitman B, Chakos M, Mayerhoff D, Bilder R, Goldman R, Lieberman JA. Predictors of treatment response from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatry. 1999;156:544–549. doi: 10.1176/ajp.156.4.544. [DOI] [PubMed] [Google Scholar]
- 9.Simpson MM, Goetz RR, Devlin MJ, Goetz SA, Walsh BT. Weight gain and antipsychotic medication: differences between antipsychotic-free and treatment periods. J Clin Psychiatry. 2001;62:694–700. doi: 10.4088/jcp.v62n0906. [DOI] [PubMed] [Google Scholar]
- 10.Kalra SP, Dube MG, Pu S, Xu B, Horvath TL, Kalra PS. Interacting appetite-regulating pathways in the hypothalamic regulation of body weight. Endocr Rev. 1999;20:68–100. doi: 10.1210/edrv.20.1.0357. [DOI] [PubMed] [Google Scholar]
- 11.Prolo P, Wong ML, Licinio J. Leptin. Int J Biochem Cell Biol. 1998;30:1285–1290. doi: 10.1016/s1357-2725(98)00094-6. [DOI] [PubMed] [Google Scholar]
- 12.Janeckova R. The role of leptin in human physiology and pathophysiology. Physiol Res. 2001;50:443–459. [PubMed] [Google Scholar]
- 13.Monteleone P, Fabrazzo M, Tortorella A, La Pia S, Maj M. Pronounced early increase in circulating leptin predicts a lower weight gain during clozapine treatment. J Clin Psychopharmacol. 2002;22:424–426. doi: 10.1097/00004714-200208000-00015. [DOI] [PubMed] [Google Scholar]
- 14.De Ambrogi M, Volpe S, Tamanini C. Ghrelin: central and peripheral effects of a novel peptydil hormone. Med Sci Monit. 2003;9:RA217–RA224. [PubMed] [Google Scholar]
- 15.Nogueiras R, Perez-Tilve D, Wortley KE, Tschop M. Growth hormone secretagogue (ghrelin-) receptors--a complex drug target for the regulation of body weight. CNS Neurol Disord Drug Targets. 2006;5:335–343. doi: 10.2174/187152706777452227. [DOI] [PubMed] [Google Scholar]
- 16.Ariyasu H, Takaya K, Tagami T, Ogawa Y, Hosoda K, Akamizu T, Suda M, Koh T, Natsui K, Toyooka S, Shirakami G, Usui T, Shimatsu A, Doi K, Hosoda H, Kojima M, Kangawa K, Nakao K. Stomach is a major source of circulating ghrelin, and feeding state determines plasma ghrelin-like immunoreactivity levels in humans. J Clin Endocrinol Metab. 2001;86:4753–4758. doi: 10.1210/jcem.86.10.7885. [DOI] [PubMed] [Google Scholar]
- 17.Muccioli G, Tschöp M, Papotti M, Deghenghi R, Heiman M, Ghigo E. Neuroendocrine and peripheral activities of ghrelin: implications in metabolism and obesity. Eur J Pharmacol. 2002;440:235–254. doi: 10.1016/s0014-2999(02)01432-2. [DOI] [PubMed] [Google Scholar]
- 18.Shintani M, Ogawa Y, Ebihara K, Aizawa-Abe M, Miyanaga F, Takaya K, Hayashi T, Inoue G, Hosoda K, Kojima M, Kangawa K, Nakao K. Ghrelin, an endogenous growth hormone secretagogue, is a novel orexigenic peptide that antagonizes leptin action through the activation of hypothalamic neuropeptide Y/Y1 receptor pathway. Diabetes. 2001;50:227–232. doi: 10.2337/diabetes.50.2.227. [DOI] [PubMed] [Google Scholar]
- 19.Taylor DM, McAskill R. Atypical antipsychotics and weight gain-a systematic review. Acta Psychiatr Scand. 2000;101:416–432. doi: 10.1034/j.1600-0447.2000.101006416.x. [DOI] [PubMed] [Google Scholar]
- 20.Togo T, Hasegawa K, Miura S, Hosojima H, Kojima K, Shoji M, Kase A, Uchikado H, Iseki E, Kosaka K. Serum ghrelin concentration in patients receiving olanzapine or risperidone. Psychopharmacology (Berl) 2004;172:230–232. doi: 10.1007/s00213-003-1642-4. [DOI] [PubMed] [Google Scholar]
- 21.Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K. Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature. 1999;402:656–660. doi: 10.1038/45230. [DOI] [PubMed] [Google Scholar]
- 22.Nakazato M, Murakami N, Date Y, Kojima M, Matsuo H, Kangawa K, Matsukura S. A role for ghrelin in the central regulation of feeding. Nature. 2001;409:194–198. doi: 10.1038/35051587. [DOI] [PubMed] [Google Scholar]
- 23.Kraus T, Haack M, Schuld A, Hinze-Selch D, Kuhn M, Uhr M, Pollmacher T. Body weight and leptin plasma levels during treatment with antipsychotic drugs. Am J Psychiatry. 1999;156:312–314. doi: 10.1176/ajp.156.2.312. [DOI] [PubMed] [Google Scholar]
- 24.Murashita M, Kusumi I, Inoue T, Takahashi Y, Hosoda H, Kangawa K, Koyama T. Olanzapine increases plasma ghrelin level in patients with schizophrenia. Psychoneuroendocrinology. 2005;30:106–110. doi: 10.1016/j.psyneuen.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 25.Hosojima H, Togo T, Odawara T, Hasegawa K, Miura S, Kato Y, Kanai A, Kase A, Uchikado H, Hirayasu Y. Early effects of olanzapine on serum levels of ghrelin, adiponectin and leptin in patients with schizophrenia. J Psychopharmacol. 2006;20:75–79. doi: 10.1177/0269881105056647. [DOI] [PubMed] [Google Scholar]
- 26.Tschop M, Weyer C, Tataranni PA, Devanarayan V, Ravussin E, Heiman ML. Circulating ghrelin levels are decreased in human obesity. Diabetes. 2001;50:707–709. doi: 10.2337/diabetes.50.4.707. [DOI] [PubMed] [Google Scholar]
- 27.Tschop M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407:908–913. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- 28.Wren AM, Small CJ, Ward HL, Murphy KG, Dakin CL, Taheri S, Kennedy AR, Roberts GH, Morgan DG, Ghatei MA, Bloom SR. The novel hypothalamic peptide ghrelin stimulated food intake and growth hormone secretion. Endocrinology. 2000;141:4325–4328. doi: 10.1210/endo.141.11.7873. [DOI] [PubMed] [Google Scholar]
- 29.Hansen TK, Dall R, Hosoda H, Kojima M, Kangawa K, Christiansen JS, Jorgensen JO. Weight loss increases circulating levels of ghrelin in human obesity. Clin Endocrinol (Oxf) 2002;56:203–206. doi: 10.1046/j.0300-0664.2001.01456.x. [DOI] [PubMed] [Google Scholar]
- 30.Bagnasco M, Kalra PS, Kalra SP. Ghrelin and leptin pulse discharge in fed and fasted rats. Endocrinology. 2002;143:726–729. doi: 10.1210/endo.143.2.8743. [DOI] [PubMed] [Google Scholar]
- 31.Kalra SP, Bagnasco M, Otukonyong EE, Dube MG, Kalra PS. Rhythmic, reciprocal ghrelin and leptin signaling: new insight in the development of obesity. Regul Pept. 2003;111:1–11. doi: 10.1016/s0167-0115(02)00305-1. [DOI] [PubMed] [Google Scholar]
- 32.Ueno H, Yamaguchi H, Kangawa K, Nakazato M. Ghrelin: a gastric peptide that regulates food intake and energy homeostasis. Regul Pept. 2005;126:11–19. doi: 10.1016/j.regpep.2004.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Huang TL, Chen JF. Serum lipid profiles and schizophrenia: effects of conventional or atypical antipsychotic drugs in Taiwan. Schizophr Res. 2005;80:55–59. doi: 10.1016/j.schres.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 34.Brown RR, Estoup MW. Comparison of the metabolic effects observed in patients treated with ziprasidone versus olanzapine. Int Clin Psychopharmacol. 2005;20:105–112. doi: 10.1097/00004850-200503000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Expert panel on detection, evaluation, and treatment of high blood cholesterol in adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 36.Cooper SJ. Palateability-dependent appetite and benzodiazepines: new directions from the pharmacology of GABA(A) receptor subtypes. Appetite. 2005;44:133–150. doi: 10.1016/j.appet.2005.01.003. [DOI] [PubMed] [Google Scholar]