Abstract
This study was performed to identify the chronological changes of the knee angle or the tibiofemoral angles in normal healthy Korean children. Full-length anteroposterior view standing radiographs of 818 limbs of 452 Korean children were analyzed. The overall patterns of the chronological changes in the knee angle were similar to those described previously in western or Asian children, but the knee angle development was delayed, i.e., genu varum before 1 yr, neutral at 1.5 yr, increasing genu valgum with maximum a value of 7.8° at 4 yr, followed by a gradual decrease to approximately 5-6° of genu valgum of the adult level at 7 to 8 yr of age. These normative data on chronological changes of knee angles should be taken into consideration when evaluating lower limb alignment in children.
Keywords: Axial Alignment of Lower Extremity, Knee Joint Orientation, Tibiofemoral Knee Angle, Child, Korea
INTRODUCTION
The bowleggedness and knock-knees are frequently encountered in pediatric orthopaedic clinics. Although benign and self-limiting in most cases, these deformities sometimes cause a great concern to the parents and the relatives (1-6), and such anxieties frequently lead physicians to conduct physical or radiological examinations (4, 7-9). However, even after these examinations have been conducted, misunderstandings of physiologic ranges and changes in knee alignment might initiate costly and time-consuming therapeutic measures, such as, bracing, which may be entirely unnecessary and in certain instances may prove harmful (8).
It has been well established by previous studies involving radiological analysis and clinical measurements that children undergo sequential physiologic changes in axial alignment, i.e., genu varum, neutral, and genu valgum, during normal development (4, 5, 7, 8, 10). Moreover, the physiologic changes in knee angle have been investigated with respect to gait, joint range of motion, and torsional deformities (4, 5), and have been found to correct spontaneously in time (3, 4, 10). However, the absence of values defining normal ranges in different ethnic groups limits the application of this information.
The purposes of the present study were to provide normative data on the axial alignment or the anatomical tibiofemoral angle (aTFA) of the lower extremity in normal Korean children, and to compare its trend with those reported by previous studies.
MATERIALS AND METHODS
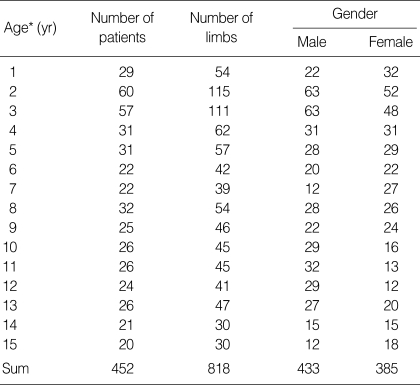
We retrospectively reviewed the teleradiographs of the lower limbs taken in children younger than 16 yr old from July 2001 to March 2004. In total 818 limbs (433 boys and 385 girls) in 452 children (243 boys and 209 girls) were enrolled in this study. Ninety-seven patients underwent repeat radiographic examinations by at least at one-year intervals, and were considered independent cases. The chronological age of the subjects was rounded off to the nearest integer, and the ones from 2-yr-7-month to 3-yr-6 month old were grouped into age 3 group (Table 1).
Table 1.
The demographics of the subjects
*, Age was rounded off to the nearest interger, and the age 3 group includes ones from 2-yr-7-month to 3-yr-6-month old.
To prevent any selection bias in a retrospective design study, strict inclusion and exclusion criteria were implemented, all the more because the radiographs had probably been taken owing to any discomfort of the leg. The children who were brought to orthopedic clinic for the parents' concern of malalignment, and only to get negative result constituted most of the subjects. Those with growing pain or Osgood-Schlatter disease were included, and so does the children who had been admitted to pediatric or urological department owing to diseases unrelated to the musculoskeletal system, and happened to have a leg discomfort. Those with skeletal or extra-skeletal disorders that might have affected the alignment of the lower extremity were excluded from the study including orthopaedic disorders such as developmental dislocations of the hip, various skeletal dysplasias, cerebral palsy, neuromuscular disorders, foot deformities, and metabolic diseases influencing the musculoskeletal system. Children who underwent operations on the legs were omitted. Those with a leg length discrepancy over 2 cm, angular deformity of a lower limb over 10°, or those with a height deviated more than 2 standard deviation from the age and gender matched norm were also left out.
Weight-bearing anteroposterior radiographs of the entire lower extremities, or teleradiographs, were taken in a standing position when the subject was compliant, or in a supine position, if not. Extreme caution was needed to ensure that the patella was positioned facing forward, indicating a neutral rotational position of the lower extremity, and inadequate films for measurement were abandoned. Both of the legs were not included in all the subjects, and only available radiographs were included. The radiographs were taken with radiography beams centered at the knee, and projected from 101.6 cm onto a 35.6 × 43.2 cm cassette and from 182.9 cm onto a 35.6 × 91.4 cm cassette. The acquisition and storage of the digitalized images were conducted using a picture archiving and communication system (PACS) (Marosys™, Marotec, Seoul; or IMPAX™, AGFA, Antwerp, Belgium). The aTFA was defined as the angle between the anatomical axes of femur and tibia, being given a positive value for varus and a negative value for valgus (Fig. 1). The means, standard deviations, and 95% confidence intervals were calculated for each age and gender group. The mean aTFA gender differences were tested using the t-test, and the significance level was set at p<0.05.
Fig. 1.

The teleradiograph of the lower extremity. The radiographs were obtained in standing position, if the subject is compliant, including hip, knee, and ankle joints in a single exposure. The anatomical tibiofemoral angle (aTFA) was defined as the angle (α) between the anatomical axes of femur and tibia.
In order to assess the reliability of the measurement, 2 orthopedic surgeons performed the measurement twice at an interval of 1 week in 5 randomly selected limbs of each age group. The reliability of the measurement was attested by the intraclass correlation (ICC) (11).
RESULTS
The ICCs for intra- and inter-rater agreement ranged from 0.79-0.86. A typical interpretation of an ICC value is as follows: 0.00-0.20, poor; 0.21-0.40, fair; 0.41-0.60, moderate; 0.61-0.80, substantial; 0.81-1.00, perfect agreement. These findings led the authors to rely on the validity of the measurement, and the measurement of a single investigator was utilized in the following analysis.
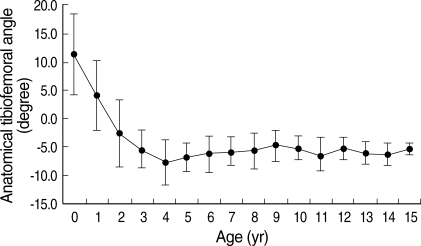
Knee alignment or aTFA was in varus alignment in infancy, and became neutral at an average age of 1.5 yr. Development into valgus alignment continued until age 4 yr when it peaked at 7.8°. It then decreased slowly to plateau at 5-6° at age 7 to 8 yr, and remained at this level thereafter (Table 2, Fig. 2). This pattern of knee alignment change is similar to that found previously in other ethnic groups, except that the valgus peak occurred later.
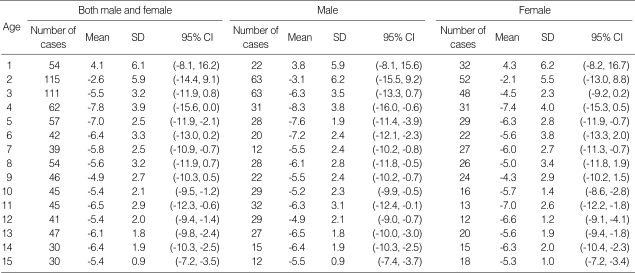
Table 2.
The descriptive statistics and confidence intervals of knee angles (aTFA) by age
aTFA, anatomical tibiofemoral angle; SD, standard deviation, CI, confidence interval.
Fig. 2.
The chronological change of anatomical tibiofemoral angles (aTFA) in Korean children. Error bars denote ± 1 standard deviations.
Chronological aTFA changes can be divided into 3 phases: phase I (0-4 yr), during which knee alignment changes from an infantile physiologic varus to maximum valgus; phase II (5-8 yr) when valgus knee alignment decreases in amount; and phase III (9-15 yr) during which knee alignment remains stationary, i.e., the adult pattern of genu valgum.
Overall patterns of aTFA chronological changes were similar for males and females. Females showed a larger peak valgus alignment at age 4 yr, but this did not differ significantly from that of males. However, at 3 yr of age, the differences became significantly different. In addition, a significant difference was observed between males and females at age 12 yr, but knee alignment change trends seemed similar in both sexes at this time of age.
DISCUSSION
The establishment of a normal range of the knee alignment in children is of paramount clinical importance, as such knowledge would allow physicians to determine whether the knee alignment in a specific patient represents physiologic development or not. Moreover, a relevant and correct understanding of the development of the knee angle and limb alignment would prevent unreasonable apprehension by parents and relatives, and unnecessary diagnostic measurements, such as repeated exposure to radiation, and the inappropriate application of orthotics or bracing, which are not often cost-effective and might even hinder natural development (6-8). In addition, this understanding would help diagnose, evaluate, and treat pathologic conditions, such as, infantile tibia vara or Blount's disease (1, 3, 6).
Several authors, based upon clinical measurements and radiological analysis, have reported on the development of knee angle in children. Engel and Staheli (4) investigated lower extremity axial alignment with respect to the mid-longitudinal axis of the thigh and lower leg in 160 normal Caucasian elementary school children, in pre-school children, and in infants and neonates. It was found that children of less than one year displayed genu varum, and that this spontaneously corrects during the second year of life, and further that the greatest mean values of genu valgum occurred in 2 or 3 yr of age. Cheng et al. (8) studied 2,630 Chinese children attending nurseries, kindergartens, and schools, and Heath and Staheli (7) studied 392 limbs of 196 Caucasian children from daycare centers, day camps, and local elementary schools. These three studies were based upon clinical or photographic measurements.
However, we consider that radiological analysis is more suitable for determining axial alignment of the lower extremity because the clinical or photography-based measurements cannot exclude the soft tissue over bone, which hinders accurate measurement. Salenius and Vankka (10) were the first to investigate the development of the knee angle in children radiologically. They conducted a study on 1,480 patients in a hospital for a variety of reasons and whose knees and legs were radiographically examined for the reasons unrelated to their illnesses. They found that the knee angles underwent serial changes, i.e., genu varum before 1 yr, neutral at 1 yr and 6 month, increasing genu valgum at 2-3 yr, reaching a maximum value at 3 yr 6 months, and followed by a subsequent slight decrease to adopt the adult knee angle pattern at 5-6 yr.
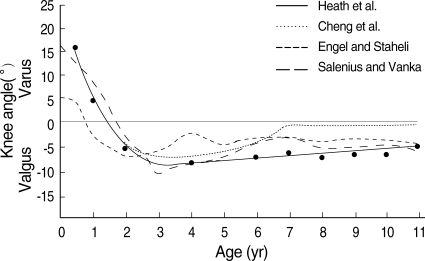
One should be cautious when describing what is 'normal', because of the possibilities of individual and ethnic variations. Although Cheng et al. (8) concluded that trends in the Chinese were nearly identical to those shown by other races in this context. Heath et al. (7) suggested that there are racial differences. Whereas Cheng et al. (8) concluded that soon after 3 yr of age the tibiofemoral angel of Chinese children approaches 0°, which indicates that normal Chinese children aged between 3 and 11 yr exhibit a significant amount of varus, Heath et al. (7) observed preservation of valgus with a mean of 2.8° at 11 yr, and normal limits of these ages did not include any amount of varus, hence more varus in Chinese children than in white children (Fig. 3). Korean children in our study showed patterns of sequential physiologic knee angle changes that are similar to those reported in other races (4, 5, 7, 8, 10), although the valgus peak occurred later and the overall development of alignment more prolonged.
Fig. 3.
The changes of the knee angle from the previously published reports (Reprinted with permission from reference 7).
The weakness of this study lies is its cross-sectional nature. A cohort study would have been more meaningful and reliable, but it would have required unnecessary repeated radiation exposure in growing children. Moreover, if emphasis is placed on the representation of knee angle in different age groups rather than on sequential changes in a specific cohort group, then the current study design has a seat at the table. Second, the wide range of data and the large standard deviation encountered hinders the establishment of a 'cut-off' value. Although general trends in knee angle changes were detected by the study, the determination as to whether a specific limb is mal-aligned or not is difficult. The authors recommend that alignment testing, including the determination of mechanical axis deviation, is clinically more appropriate in children over 10 yr. Third, as with most of the study depending on measuring of radiographs, the reproducibility and reliability of the measurement deserve attention. The characteristics of the children's bone including wide metaphysis, short diaphysis, and occasional bowing hinder exact measurements. The acceptable reliability of the measurement of the current study probably arose in that all the rater shared the basic notion and measurement tips through discussion. Although exact reproducibility might be doubted, the general trends of the development of the tibiofemoral angle might well be represented nonetheless.
In summary, we provided the data of the chronological changes of the lower limb alignment for the Korean children by radiographic measurement. The overall pattern of chronological changes in the knee angle or the anatomical tibiofemoral angle was similar to those found in other ethnic groups, but the development of the knee angle was slightly delayed, i.e., genu varum before 1 yr, neutral at 1.5 yr, increasing genu valgum with a maximum value of 7.8° by 4 yr followed by a gradual decrease to 5-6° of genu valgum to the adult pattern at 7 to 8 yr of age. These normative data should be taken into consideration when evaluating lower limb alignment in children.
ACKNOWLEDGMENTS
The authors are thankful to Sung Ju Kim at the Korean Center for Disease Control and Prevention for his statistical assistance.
References
- 1.McDade W. Bow legs and knock knees. Pediatr Clin North Am. 1977;24:825–839. doi: 10.1016/s0031-3955(16)33501-5. [DOI] [PubMed] [Google Scholar]
- 2.Morley AJ. Knock-knee in children. Br Med J. 1957;2:976–979. doi: 10.1136/bmj.2.5051.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sherman M. Physiologic bowing of the legs. South Med J. 1960;53:830–836. doi: 10.1097/00007611-196007000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Engel GM, Staheli LT. The natural history of torsion and other factors influencing gait in childhood. A study of the angle of gait, tibial torsion, knee angle, hip rotation, and development of the arch in normal children. Clin Orthop Relat Res. 1974;99:12–17. doi: 10.1097/00003086-197403000-00002. [DOI] [PubMed] [Google Scholar]
- 5.Hachiya M. A roentgenographical study on chronological changes in genu varum and valgum in children (author's transl) Nippon Seikeigeka Gakkai Zasshi. 1981;55:31–43. [PubMed] [Google Scholar]
- 6.Levine AM, Drennan JC. Physiological bowing and tibia vara. The metaphyseal-diaphyseal angle in the measurement of bowleg deformities. J Bone Joint Surg Am. 1982;64:1158–1163. [PubMed] [Google Scholar]
- 7.Heath CH, Staheli LT. Normal limits of knee angle in white children--genu varum and genu valgum. J Pediatr Orthop. 1993;13:259–262. [PubMed] [Google Scholar]
- 8.Cheng JC, Chan PS, Chiang SC, Hui PW. Angular and rotational profile of the lower limb in 2,630 Chinese children. J Pediatr Orthop. 1991;11:154–161. doi: 10.1097/01241398-199103000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 10.Salenius P, Vankka E. The development of the tibiofemoral angle in children. J Bone Joint Surg Am. 1975;57:259–261. [PubMed] [Google Scholar]
- 11.Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychol Bull. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]