Abstract
With recent progress in treatment modalities, mortality from upper gastrointestinal (UGI) bleeding has decreased appreciably. The aim of this study was to establish how UGI bleeds are managed in Korean patients with cirrhosis and to evaluate treatment outcomes. A total of 479 episodes of acute UGI bleeding in 464 patients with cirrhosis were included during a six-month period at nine tertiary medical centers. Treatment outcomes were assessed by failure to control bleeding, rebleeding and mortality. The source of bleeding was esophagogastric varices in 77.7% of patients, nonvariceal lesions in 15.9%, and undefined in 6.5%. For control of bleeding, endoscopic and pharmacologic treatments were used in 74.7% and 81.9% of patients, respectively. Variceal ligation was a major technique for endoscopic treatment (90%), and terlipressin and somatostatin were the main pharmacologic agents used (96.4%). Initial hemostasis was achieved in 86.8% of cases, but rebleeding occurred in 3.8% and 16.8% of cases within five days and six weeks of hemorrhage, respectively. Five-day and six-week mortality were 11.3% and 25.9%, respectively. Survival of patients with variceal bleeding seems to be remarkably improved than previous reports, which may suggest the advances in hemostatic methods for control of variceal hemorrhage.
Keywords: Liver Cirrhosis, Varicose Veins, Hemorrhage, Hemostasis, Prevention and Control, Prognosis
INTRODUCTION
Variceal bleeding is one of the life-threatening complications in patients with cirrhosis and reportedly accounted for a 40-60% mortality rate in these patients 30 to 40 yr ago (1-5). During recent decades, however, there has been significant progress in and diversification of hemostatic modalities for variceal bleeding, including pharmacologic, endoscopic, surgical, and radiological therapies. Several recent studies have suggested that mortality of patients with cirrhosis and acute variceal bleeding has significantly decreased over the past two decades (5-9).
In addition to the improvement in initial hemostatic management, several other factors might play a role in improved survival after variceal hemorrhage. Rebleeding may occur in as high as 70% of patients with cirrhosis who experience a variceal bleed and is associated with a very high mortality (2). Currently recommended practice is secondary prophylaxis with a nonselective beta-blocker (10) and endoscopic variceal eradication (11, 12) to prevent rebleeding and increase the survival rate. Indeed, several recent studies have reported that such secondary prevention considerably reduced the incidence of rebleeding (5, 8, 9). Likewise, bacterial infection is a common phenomenon after variceal bleeding in patients with cirrhosis and appears to be associated with failure to control bleeding as well as with septic complications (13). Because bleeding might be provoked by microbial endotoxins, which increase portal pressure and prophylactic antibiotics reportedly substantially reduce mortality in patients with variceal hemorrhage, antibiotic prophylaxis is now a recommended practice on admission (14).
We previously reported improved survival in Korean patients with cirrhosis and variceal bleeding in a cohort within a single institution (15). However, there has been no nationwide survey to assess the prognosis of upper gastrointestinal (UGI) bleeding in cirrhotic patients and to assess whether they are appropriately managed in accordance with general standard guidelines for initial hemostasis, prevention of rebleeding, and antibiotic prophylaxis. Therefore, we conducted a multicenter cohort study to identify how UGI bleeds are managed in Korean patients with cirrhosis and to identify treatment outcomes.
MATERIALS AND METHODS
Patients and data collection
This multicenter, retrospective study included a total of 479 episodes of acute UGI bleeding in 464 patients with cirrhosis. Subjects were all patients with cirrhosis, consecutively admitted for hematemesis and/or melena between May and October 2005 at nine tertiary medical centers distributed throughout Korea. The medical records of enrolled patients were reviewed to obtain necessary demographic, clinical, laboratory, treatment, and follow-up data. Gender, age at diagnosis, etiology of cirrhosis, presence of ascites, portal vein thrombosis, hepatocellular carcinoma, and laboratory results at presentation (hemoglobin, leukocyte and platelet count, albumin, bilirubin, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, hepatitis serological tests) were also identified. Further identified from the medical records were acute therapy for hemostasis, prophylactic therapy, and the amount of blood transfused. Diagnosis of cirrhosis was based on a previous liver biopsy or on compatible clinical, laboratory and imaging findings. Source of bleeding was classified with endoscopic findings as variceal (esophageal or gastric varices), nonvariceal (portal hypertensive gastropathy; esophageal, gastric or duodenal ulcers; Mallory-Weiss syndrome; sclerotherapy/banding-induced ulcerations), or undefined (that is, unidentified source of bleeding or no endoscopy). In addition, time intervals from start of bleeding to hospital admission, from admission to endoscopy, and from start of bleeding to endoscopy were reviewed. All patients were followed up to the time of death or 42 days from admission. For patients who had multiple hospitalizations for UGI bleeding during the study period, rebleeding after 42 days of index bleed was considered as a new episode. The size of esophageal varices was classified according to the criteria of Beppu et al. (16). The classification of gastric varices was based on criteria by Sarin et al. (17). The hepatic function of patients at admission was graded according to the Child-Pugh classification (4).
Definitions
The following definitions were based on recommendations from the Baveno II, III and IV consensus workshops (14, 18, 19). 1) Time zero of the bleeding episode: the time of admission to the first hospital to which the patient was taken, 2) source of bleeding: a lesion actively bleeding or with adherent clot, white nipple, or presence of a single lesion without other potential sources of bleeding, 3) type of bleeding: bleeding was defined as active if a spurting or oozing lesion was seen on endoscopy, or if fresh blood was regurgitated via the gastric tube when endoscopy was not allowed, 4) control of bleeding: the acute bleeding episode was considered finished at the beginning of the first 24-hr interval with no hematemesis, stable hemoglobin concentration without blood transfusions, and stable hemodynamic conditions (absence of systolic blood pressure or reduction of 20 mmHg or more, and increase of heart rate of 20/min or more), and 5) rebleeding: any occurrence of hematemesis or hemoglobin drop with fresh melena after initial control of bleeding.
Treatment outcomes were assessed in accordance with the failure to control index bleeding, rebleeding and death within 42 days from time 0 of index bleed. Five-day failure was defined as failure to control bleeding, rebleeding, or death within 5 days of admission.
The presence of infectious diseases at admission and their development during hospitalization were investigated with appropriate diagnostic methods and cultures. Patients with a fever >38℃ that lasted more than 24 hr and leukocytosis with a shift to the left, but without any other evidence of infection, were considered as having "possible infections" (20).
Statistical analysis
Qualitative variables were expressed as percentages and compared using Pearson's chi-square test. Quantitative variables were expressed as mean±standard deviation and compared using Student's t-test. Cumulative rates of survival were estimated by the Kaplan-Meier method and comparisons between patient subgroups were made with the use of logrank tests. All tests were two-tailed, and p values below 0.05 were considered to indicate statistical significance. All the statistical analyses were performed using SPSS version 10.0.
RESULTS
Characteristics of cohorts
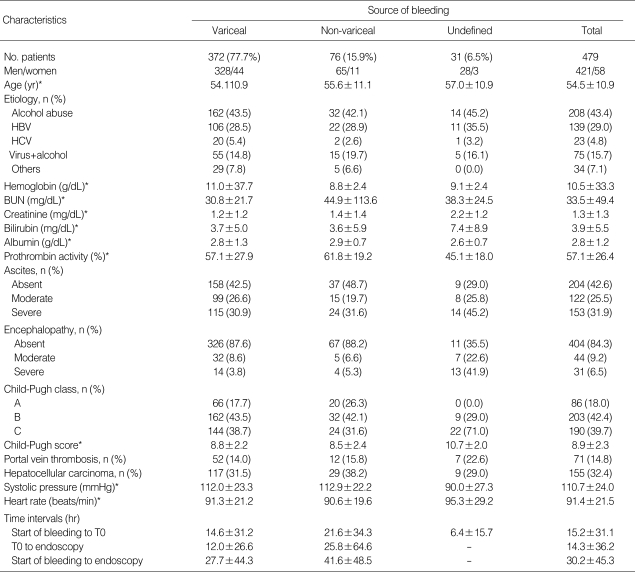
Demographic, clinical, and laboratory data at admission are presented in Table 1. In the whole series, 421 (87.9%) out of 479 episodes of UGI bleeds occurred in males and the mean age was 54.5 yr. Liver cirrhosis was related to heavy alcohol intake in 43.4% of patients, to hepatitis B virus in 29%, to hepatitis C virus in 4.8%, and to both alcohol and virus in 15.7%. The mean systolic blood pressure was 111 mmHg and the mean heart rate was 91/min. Hemoglobin concentration averaged 10.5 g/dL. Ascites and hepatic encephalopathy were found in 57.4% and 15.7% of patients, respectively. According to the Child-Pugh classification, 86 (18%) patients were included in grade A, 203 (42.4%) in grade B, and 190 (39.7%) in grade C. Portal vein thrombosis and hepatocellular carcinoma were combined in 14.8% and 32.4% of patients, respectively.
Table 1.
Demographic and clinical characteristics of the cohort on admission
*Mean±standard deviation; variceal, patients with variceal bleeding; nonvariceal, patients with bleeding from other sources than varices; undefined, patients with bleeding from undefined sources. T0, the time of admission to the hospital to which the patient was taken; HBV, hepatitis B virus; HCV, hepatitis C virus.
When included in this study, 220 (45.9%) patients had a history of at least one episode of previous bleeding, mainly caused by variceal rupture (185 of 220 cases, 84.1%), and 144 (77.8%) of them had received preventive measures against rebleeding. In contrast, among 259 patients without previous bleeds, only 24 (9.3%) were receiving prophylaxes.
Source and type of bleeding
The median time from initial sign of bleeding to hospital admission was 17 hr (range 0-96 hr) and from admission to endoscopy was six hours (range 0-158 hr). Endoscopy revealed the source of bleeding in 448 (93.5%) of 479 episodes as follows: esophageal varices in 273 patients (57%), gastric varices in 99 (20.7%), gastric ulcer in 48 (10%), duodenal ulcer in 16 (3.3%), and other lesions in 12 (2.5%). The size of varices in 273 patients who bled from esophageal varices was F1 in 16 patients (5.9%), F2 in 118 (43.2%), and F3 in 139 (50.9%). Red color sign was noted in 243 patients (89%). The types of gastric varices were GOV1 in 56 patients (56.6%), GOV2 in 38 (38.4%), and IGV1 in 5 (5%). In 31 patients, however, the source of bleeding remained undefined because endoscopy was unsatisfactory. In one patient, it was due to hemodynamic instability, and endoscopic evaluation could not be performed in 30 patients for the following reasons: massive bleeding with encephalopathy in six, massive bleeding with hemodynamic instability in 21, and refusal of endoscopy in three. Active bleeding was found in 184 (38.4%) of 479 episodes either by endoscopy or by gastric aspirate. Among the patients with bleeding from identified sources, there were no significant differences in type of bleeding according to the source of bleeding (p=0.627). On the other hand, the patient group who bled from undefined sources exhibited active bleedings in all cases and contained more patients with encephalopathy and severe hepatic dysfunction, and thus included in Child-Pugh grade C, as compared with other groups (p<0.001).
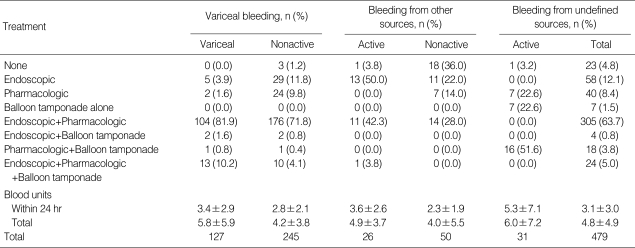
Treatment
Types of treatments employed for initial hemostasis are represented in Table 2. In the whole series, pharmacologic treatments were performed in 81.9% of patients, endoscopic treatment in 74.7%, and balloon tamponade in 10.9%. In one case, a transjugular intrahepatic portosystemic shunt was inserted. The treatment modalities were applied in combination in most cases (69.3%) but alone in some cases. The most frequent type of combination was pharmacologic plus endoscopic treatment (287 cases, 59.9%). There were no significant differences in types of treatment for initial hemostasis between patients with HCC and portal vein invasion and the others (p=0.374).
Table 2.
Types of initial treatment for hemostasis in all patients according to the source of bleeding
The pharmacologic agents used for initial hemostasis were terlipressin in 42.4% of episodes, somatostatin in 35.5%, and octreotide in 2.9%. They were administered in advance of diagnostic endoscopy in 84.8% of cases. The median (range) dose and duration of each drug was 4 (3-6) mg/day for 3 (1-8) days for terlipressin, 6 (6) mg/day for 3 (1-8) days for somatostatin, and 0.6 (0.6) mg/day for 4 (2-8) days for octreotide.
Endoscopic treatment for initial hemostasis was carried out during initial diagnostic endoscopy in 252 of 310 patients (81.3%), or otherwise on an elective basis and in stable hemodynamic conditions at the median time of nine hours after admission. The major endoscopic techniques for treating variceal and nonvariceal hemorrhage were banding ligation (279 of 310 patients, 90%) and electrocoagulation (20 of 48 patients, 41.7%), respectively. To control the bleeding from esophageal varices, banding ligation and endoscopic injection sclerotherapy were used in 242 cases (88.6%) and 15 cases (5.5%), respectively. In patients who bled from gastric varices, banding ligation and endoscopic variceal obturation with N-butyl-2-cyanoacrylate (Histoacryl) were most frequently used (32.3% and 30.3%, respectively).
Outcomes after acute UGI bleeding
Initial control of bleeding was achieved in 416 (86.8%) of 479 episodes (Table 3). The median time from admission to hemostasis was eight hours (range 0-504 hr). In the 63 cases (13.2%) where control of bleeding failed, the source of bleeding was esophageal varices in 26 cases (41.3%), gastric varices in nine (14.3%), and undefined in 27 (42.9%). The rate of failure in initial hemostasis was significantly higher in patients with variceal bleeding (35 of 372 patients, 9.4%) than in those with nonvariceal bleeding (1 of 76, 1.3%; p=0.011 between two groups).
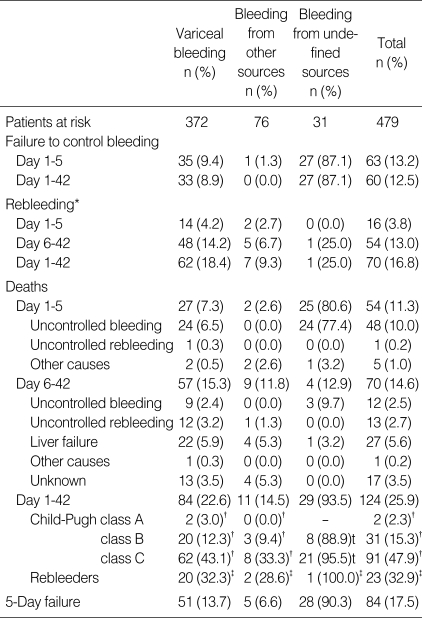
Table 3.
Treatment outcomes according to the source of bleeding
*, Patients with uncontrolled bleeding were not included in this analysis; †, Proportion of patients dying in each subgroup according to the source of bleeding and Child-Pugh class; ‡, Proportion of patients dying in the group of patients with rebleeding according to the source of bleeding.
Five-day failure took place in 84 of the whole 479 (17.5%) episodes as shown in Table 3, comprising 54 deaths and 15 cases of rebleeding and 15 failures in initial hemostasis of patients who were still alive on day 5. The five-day failure rate was not significantly different between patients with variceal bleeding and patients with nonvariceal bleeding (13.7% vs. 6.6%, p=0.09). The five-day failure rate was high in patients with bleeding of undefined sources (28 of 31 cases, 90.3%), 27 of whom failed to control bleeds and 25 died.
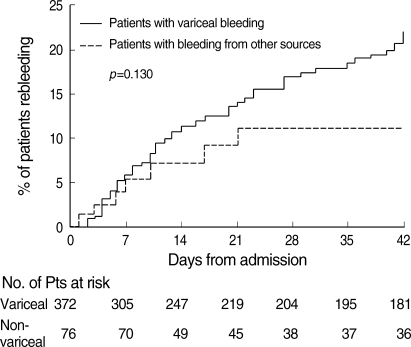
On the whole, 70 of 414 patients (16.9%) rebled within six weeks of index bleeds, 16 (3.9%) within five days, 54 (13.4%) during days 6 to 42 (Table 3). The six-week rebleeding rate was 18.4% (62 of 337 cases) for patients with variceal bleedings, 9.3% (7 of 75) for patients with nonvariceal bleedings and 25% (1 of 4) for patients with bleedings of undefined source. There was no significant difference between patients with variceal bleeding and patients with nonvariceal bleeding (p=0.130, Fig. 1). Rebleeding was uncontrollable in 14 of 70 patients (20%), including 13 of 62 variceal bleeds and one of seven nonvariceal bleeds.
Fig. 1.
Cumulative incidence of rebleeding after hemostasis according to the source of initial bleeding in 448 patients with known source of bleeding. Thirty-one patients with bleeding from undefined sources were excluded in this analysis. The p value was obtained from the log-rank test.
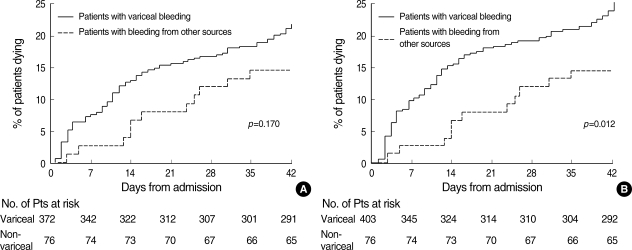
Overall, 124 of 479 patients (25.9%) died within six weeks of index bleeds, 54 (11.3%) within five days, and 70 (14.6%) during days 6 to 42 (Table 3). The six-week mortality rate was 22.6% in patients with variceal bleeding, which was not significantly different from that in patients with nonvariceal bleeding (14.5%, p=0.107, Fig. 2A).
Fig. 2.
(A) Cumulative mortality according to the source of initial bleeding in 448 patients with known source of bleeding. Thirty-one patients with bleeding from undefined sources were excluded in this analysis. (B) In this figure, patients with bleeding from undefined sources were included in patients with variceal bleeding. The p value was obtained from the log-rank test.
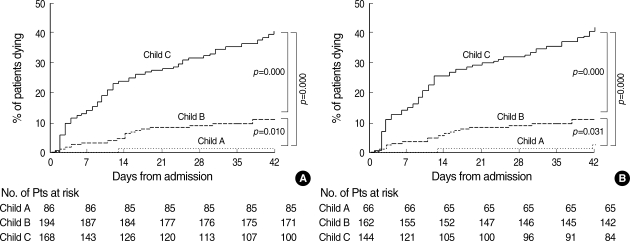
The mortality increased with the degree of hepatic dysfunction in patients with all known sources of bleeding (Table 3, Fig. 3A) as well as in cases with variceal bleeding (Fig. 3B). In the whole series (Table 3), failure to control initial or recurrent bleeding was a main cause of death within six weeks of hemorrhage and responsible for 74 of all 124 casualties (59.7%), including 46 of 84 deaths due to variceal bleeds (54.8%), for one of 11 deaths due to nonvariceal bleeds (9.1%), and for 27 of 29 deaths due to bleeds of undefined source (93.1%). In particular, the failure to control initial bleeding was responsible for 88.9% (24 of 27 cases) and 96% (24 of 25 cases) of all deaths within five days of bleeds from varices and undefined sources, respectively, whereas it was not related to early deaths due to nonvariceal bleeds. In contrast, the failure to control rebleeding accounted for 21.1% (12 of 57 cases) and 11.1% (one of nine cases) of late deaths that occurred after five days of variceal and nonvariceal bleeding, respectively.
Fig. 3.
Cumulative mortalities according to the Child-Pugh class of (A) 448 patients with known sources of bleeding and (B) 372 patients with variceal bleeding. Thirty-one patients with bleeding from undefined sources were excluded in this analysis. The p values were obtained from the log-rank test. Child A, patients with Child-Pugh class A; Child B, patients with Child-Pugh class B; Child C, patients with Child-Pugh class C.
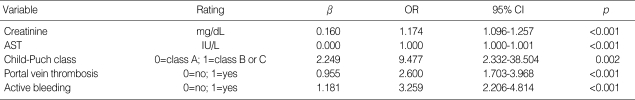
In multivariate analysis for 6-week mortality in patients with variceal bleeding, baseline creatinine and AST level, Child-Pugh class, portal vein thrombosis and active bleeding from varices were the independent predictive factors for survival (Table 4).
Table 4.
Prognostic factors for the 6-week mortality in patients with variceal bleeding by multivariate analysis
AST, aspartate aminotransferase; OR, odds ratio; CI, confidence interval.
Prophylactic therapy for variceal rebleeding
Of 343 patients with successfully controlled variceal bleeding, 321 (93.6%) received pharmacologic or endoscopic treatments to prevent recurrent bleeding. In 22 patients, no prophylactic therapy was performed. Pharmacologic prophylaxis was given to 194 patients (56.6%), commencing at median four days (0-20 days) from admission. The main drug prescribed was propranolol (184 of 194 cases, 95.4%), and the median daily dose was 40 mg (10-240 mg).
Endoscopic prophylaxis was performed in 294 of 343 cases (85.7%) with a total of 427 sessions. Endoscopic band ligation was the most common technique applied (350 of 427 sessions, 82%), and at each session, median 4.2 bands were used. Twenty-six sessions (6.1%) of endoscopic sclerotherapy were performed in 23 cases using median 14.8 cc of ethanolamine olate per session. For gastric varices, 51 sessions of Histoacryl injection were performed in 45 cases. At each session, 2.7 cc of Histoacryl was injected. Variceal eradication was achieved in 67 of 294 cases (22.8%) at 29±41 days from the commencement of endoscopic prophylaxis.
Infectious complications
On admission, infections were proven in 64 of 479 patients (13.4%); spontaneous bacterial peritonitis in 19 (4%), sepsis in six (1.3%), pneumonia in four (0.8%), urinary tract infection in three (0.6%), cellulites in one (0.2%), and possible infection in 31 (6.5%). Of 415 patients without signs of infection at admission, 199 (48%) were given prophylactic antibiotics. The most common agents prescribed were third-generation cephalosporins (79.9%), followed by quinolone (10.9%).
During hospitalization, a total of 37 patients (37 of 479, 7.7%) who had not shown signs of infection at admission, were infected, including spontaneous bacterial peritonitis in three (0.6%), sepsis in seven (1.5%), pneumonia in eight (1.7%), urinary tract infection in two (0.4%), cholangitis and renal abscess in one (0.2%), and possible infection in 16 (3.3%) cases. The incidence of infections during hospitalization was not significantly different whether prophylactic antibiotics were given or not (10.1% vs. 7.4%, respectively; p=0.385).
Causative organisms were identified in 10 of 64 (15.6%) patients with infections on admission and in 19 of 37 (51.4%) patients with infections during hospitalization. Eight of 10 infections at admission (80%) were caused by Gram-negative bacilli. In contrast, 11 of 19 infections during hospitalization were caused by Gram-positive cocci, of which Staphylococcus species were the most common organism (36.8%).
The incidence of infection was more frequent in patients with Child-Pugh class C (58 of 190 cases, 30.5%) than those with Child-Pugh class A or B (42 of 289, 14.5%; p<0.001).
DISCUSSION
This study included nine tertiary medical centers in different regions in Korea and enrolled all consecutive patients with cirrhosis who had been admitted during a six-month period for hematemesis and/or melena. Thus, the study, despite being retrospective, can provide recent, representative data about clinical features and treatment outcomes of cirrhotic patients admitted for UGI bleeding in this country.
Several clinical features of the study are noteworthy. First, esophagogastric variceal bleedings accounted for most (78%) UGI bleeds in our cohort, a result somewhat higher than but comparable with the proportions reported in some recent studies (5, 9). Second, cirrhosis was related to alcohol abuse in 60% of patients, including 40% with alcoholic cirrhosis, which is appreciably higher than the usual proportion of alcohol abuse among the etiologies of cirrhosis in Korea (about 26%) (21). This result might be supported by several studies suggesting that ethanol consumption increases the risk of variceal bleeding in patients with cirrhosis by increasing hepatic vascular resistance, portal pressure, and variceal blood flow (22, 23). Third, hepatocellular carcinoma was found in as much as one-third of all patients, which was twice the proportion of patients with hepatocellular carcinoma in the recent study reported by D'Amico et al. (9). This might reflect the geographic characteristics of the endemic area of hepatitis B virus infection in Korea and be related to a relatively higher rate of failure to control bleeding in our series. Although chronic hepatitis B virus carriers accounted for only 29% (139 of 479) of all patients, they accounted for 71.6% (111 of 155) of patients with hepatocellular carcinoma.
This study showed a remarkable reduction in six-week mortality after variceal hemorrhages when compared to that in a pioneering study reported in 1981 by Graham et al. (2) (from 42% to 23%), a result consistent with several recent studies (5-9, 15). Actually, the proportion of patients with Child-Pugh class C was significantly lower in this study (38.7%) than in the study by Graham et al. (69.9%). However, this remarkable reduction in the mortality could be noted when compared with other studies (mortality, 32-49%) that included similar proportions of patients with Child-Pugh class C (21-39%) with this study (3, 5). The most prominent change was the reduction in five-day mortality, which was 7.3% in the present study, whereas it was 23.5% in the study by Graham et al. (2). By contrast, the mortality after five days to six weeks of hemorrhage was similar between the two studies (15.3% vs. 17.7%, respectively). This suggests that a significant improvement in survival after variceal bleeding in recent years is mainly attributable to the reduction in mortality during the early period of bleeding. This has been achieved by the notable improvement in initial hemostasis and prevention of early rebleeding with the development of effective endoscopic and pharmacologic therapies for controlling variceal bleeding. Indeed, in this study, initial hemostasis was achieved in 86.8% of cases in our series, and rebleeding occurred in only 3.9% of patients within five days of hemorrhage. However, if the cases with bleeding of undefined source were counted as patients with variceal bleedings, the five-day mortality and 6-week mortality in patients with variceal bleeding increased to 12.9% and 28%, respectively. Most previous studies included patients with variceal bleeding that was identified by endoscopy. In our study, endoscopy could not be performed in many patients with cirrhosis and UGI bleeding because of hemodynamic instability. Most of these patients with bleeding from undefined sources might bleed from varices. Therefore, the actual mortality rate in patients with cirrhosis variceal bleeding might be higher than previously reported.
The rate of failure to control initial bleedings in this study was higher for variceal than for nonvariceal hemorrhages (9.4% vs. 1.3%), and this hemostatic failure eventually caused more than 90% of casualties occurring within five days of the variceal bleeds. Moreover, the early mortality of variceal bleeding would be further increased if the hemorrhages from undefined sources were included together, considering the high proportion of variceal bleeding among all UGI bleeds in our cohort. In this study, 87.1% of patients with undefined source of bleeding failed in initial hemostasis and 80.6% died within five days, which was prominently higher compared with the five-day failure rate of 20% in a recent report by D'Amico et al. (9). This big difference between the two studies might be partly explained by a far higher proportion of patients with massive bleeding, liver failure or advanced hepatocellular carcinoma in our series.
Because variceal bleeding contributes to the considerable mortality in patients with cirrhosis, a recent guideline recommends all patients with cirrhosis be screened for varices and primary prophylaxis be given for those patients with large varices (14). In the present study, only 8.9% of patients without previous bleeding received primary prophylaxis. This calls for much more efforts in providing primary prophylaxis for variceal bleeding in the high-risk group.
Also, this study indicates that more effective secondary prophylaxis is needed to prevent rebleeding. In the study, 11.3% of patients encountered rebleeding after five days of initial bleeding and this is similar to the rebleeding rate of 10.6% in the Graham study 25 yr ago, which raises a question about the effectiveness of current preventative measures. In the present study, pharmacologic or endoscopic prophylaxis was executed in 94% of patients after achieving successful initial hemostasis. In particular, endoscopic prophylaxis was commenced in 88% of cases, mainly using endoscopic variceal ligation (EVL); however, it was only in 22.8% of cases that endoscopy was followed up until all varices were eradicated. Although several studies reported that EVL was effective for the prevention of rebleeding and could improve survival (12, 24), it should be noted that the eradication of varices was a prerequisite for achieving the goal in those clinical trials. In this respect, the secondary endoscopic prophylaxis performed in the present study seems insufficient for preventing rebleeding. Among 355 patients who survived 42 days from admission, the duration of follow-up was less than 1 month in 93.8% of patients (333 of 355) and 60% of these lost patients were alcoholics. The high rate of loss of follow-up could be one reason for the low endoscopic eradication rate in our study. Similarly, nonselective beta-blockers have been reported to reduce the incidence of rebleeding and mortality in patients with prior variceal bleeding (25-27), and in our series, they were prescribed in 57.9% of patients after successful initial hemostasis. Usually, doses of beta-blocker sufficient to diminish hepatic venous pressure gradient (HVPG) to 12 mmHg or below, or to decrease heart rate by more than 20% from baseline, are necessary to prevent rebleeding effectively. Although it was not identified whether a sufficient reduction in HVPG or heart rate was achieved after the treatment with beta-blockers, the median maintenance dose in our series was relatively lower than the dose in other clinical trials (28, 29) and this might suggest an inadequacy of secondary pharmacologic prophylaxis in our series.
Several studies have suggested that the use of prophylactic antibiotics decreased the incidence of infections and improved the survival of cirrhotic patients with gastrointestinal bleeding (13). Nowadays, it is recommended that antibiotic prophylaxis be instituted in patients presenting with variceal bleeding at the time of admission (14). In this study, prophylactic antibiotics were prescribed in 48% of 415 patients without signs of infection on admission, and infections occurred in 8.7% of these patients. When considering the incidence of infection was 25-50% in the preprophylactic antibiotics era (5), the infection rate in our series appears to be significantly decreased. Contrary to expectation, however, the antibiotic prophylaxis in the present study did not substantially decrease the incidence of infection or the mortality of patients. This result could possibly be explained by selection bias: prophylactic antibiotics might have been prescribed more frequently for patients with more serious clinical conditions. The fact that this study was performed retrospectively and many cases of minor infectious events might be missed during data collection could be another explanation for this result.
Despite these limitations, some interesting results were found. The types of cultured organisms from the patients who were infected during hospitalization significantly differed from those from the patients with infection at admission. Most infections that existed at admission were caused by Gram-negative organisms, possibly derived from enteric flora. In contrast, most infections that developed during hospitalization were caused by Gram-positive organisms. This difference might be accounted for by the fact that third-generation cephalosporins, most frequently used as prophylactic antibiotics in this study, have a more powerful antibiotic potency for Gram-negative organisms than for Gram-positive ones, and many invasive procedures such as endoscopic therapy, intravenous puncture, or urinary catheter insertion were performed during hospitalization.
In conclusion, the survival of patients with cirrhosis admitted for UGI bleeding seems to be significantly improved in recent years and this might be related to a striking reduction in five-day mortality, owing to the development of endoscopic and pharmacologic treatments for controlling variceal hemorrhage. However, considering patients of undefined sources, the actual mortality of patients with variceal bleeding may be somewhat higher than previously reported data. Although secondary prophylaxis for variceal rebleeding was performed in most patients, it seems insufficient to prevent rebleeding effectively and more meticulous prophylactic treatment is needed.
Footnotes
This study was supported by a grant from the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (No. A050021).
References
- 1.Nachlas MM, O'Neil JE, Campbell AJ. The life history of patients with cirrhosis of the liver and bleeding esophageal varices. Ann Surg. 1955;141:10–23. doi: 10.1097/00000658-195501000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Graham DY, Smith JL. The course of patients after variceal hemorrhage. Gastroenterology. 1981;80:800–809. [PubMed] [Google Scholar]
- 3.Pinto HC, Abrantes A, Esteves AV, Almeida H, Correia JP. Long-term prognosis of patients with cirrhosis of the liver and upper gastrointestinal bleeding. Am J Gastroenterol. 1989;84:1239–1243. [PubMed] [Google Scholar]
- 4.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60:646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 5.Carbonell N, Pauwels A, Serfaty L, Fourdan O, Levy VG, Poupon R. Improved survival after variceal bleeding in patients with cirrhosis over the past two decades. Hepatology. 2004;40:652–659. doi: 10.1002/hep.20339. [DOI] [PubMed] [Google Scholar]
- 6.El-Serag HB, Everhart JE. Improved survival after variceal hemorrhage over an 11-year period in the Department of Veterans Affairs. Am J Gastroenterol. 2000;95:3566–3573. doi: 10.1111/j.1572-0241.2000.03376.x. [DOI] [PubMed] [Google Scholar]
- 7.McCormick PA, O'Keefe C. Improving prognosis following a first variceal haemorrhage over four decades. Gut. 2001;49:682–685. doi: 10.1136/gut.49.5.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chalasani N, Kahi C, Francois F, Pinto A, Marathe A, Bini EJ, Pandya P, Sitaraman S, Shen J. Improved patient survival after acute variceal bleeding: a multicenter, cohort study. Am J Gastroenterol. 2003;98:653–659. doi: 10.1111/j.1572-0241.2003.07294.x. [DOI] [PubMed] [Google Scholar]
- 9.D'Amico G, De Franchis R. Upper digestive bleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology. 2003;38:599–612. doi: 10.1053/jhep.2003.50385. [DOI] [PubMed] [Google Scholar]
- 10.Lebrec D, Poynard T, Hillon P, Benhamou JP. Propranolol for prevention of recurrent gastrointestinal bleeding in patients with cirrhosis: a controlled study. N Engl J Med. 1981;305:1371–1374. doi: 10.1056/NEJM198112033052302. [DOI] [PubMed] [Google Scholar]
- 11.D'Amico G, Pagliaro L, Bosch J. The treatment of portal hypertension: a meta-analytic review. Hepatology. 1995;22:332–354. doi: 10.1002/hep.1840220145. [DOI] [PubMed] [Google Scholar]
- 12.Laine L, Cook D. Endoscopic ligation compared with sclerotherapy for treatment of esophageal variceal bleeding. A meta-analysis. Ann Intern Med. 1995;123:280–287. doi: 10.7326/0003-4819-123-4-199508150-00007. [DOI] [PubMed] [Google Scholar]
- 13.Goulis J, Armonis A, Patch D, Sabin C, Greenslade L, Burroughs AK. Bacterial infection is independently associated with failure to control bleeding in cirrhotic patients with gastrointestinal hemorrhage. Hepatology. 1998;27:1207–1212. doi: 10.1002/hep.510270504. [DOI] [PubMed] [Google Scholar]
- 14.de Franchis R. Evolving consensus in portal hypertension. Report of the Baveno IV consensus workshop on methodology of diagnosis and therapy in portal hypertension. J Hepatol. 2005;43:167–176. doi: 10.1016/j.jhep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 15.Park DK, Um SH, Lee JW, Lee JB, Kim YS, Park CH, Jin YT, Chun HJ, Lee HS, Lee SW, Choi JH, Kim CD, Ryu HS, Hyun JH. Clinical significance of variceal hemorrhage in recent years in patients with liver cirrhosis and esophageal varices. J Gastroenterol Hepatol. 2004;19:1042–1051. doi: 10.1111/j.1440-1746.2004.03383.x. [DOI] [PubMed] [Google Scholar]
- 16.Beppu K, Inokuchi K, Koyanagi N, Nakayama S, Sakata H, Kitano S, Kobayashi M. Prediction of variceal hemorrhage by esophageal endoscopy. Gastrointest Endosc. 1981;27:213–218. doi: 10.1016/s0016-5107(81)73224-3. [DOI] [PubMed] [Google Scholar]
- 17.Sarin SK, Lahoti D, Saxena SP, Murthy NS, Makwana UK. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992;16:1343–1349. doi: 10.1002/hep.1840160607. [DOI] [PubMed] [Google Scholar]
- 18.de Franchis R. Developing consensus in portal hypertension. J Hepatol. 1996;25:390–394. doi: 10.1016/s0168-8278(96)80127-9. [DOI] [PubMed] [Google Scholar]
- 19.de Franchis R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol. 2000;33:846–852. doi: 10.1016/s0168-8278(00)80320-7. [DOI] [PubMed] [Google Scholar]
- 20.Pauwels A, Mostefa-Kara N, Debenes B, Degoutte E, Levy VG. Systemic antibiotic prophylaxis after gastrointestinal hemorrhage in cirrhotic patients with a high risk of infection. Hepatology. 1996;24:802–806. doi: 10.1002/hep.510240408. [DOI] [PubMed] [Google Scholar]
- 21.Kim YS, Um SH, Ryu HS, Lee JB, Lee JW, Park DK, Kim YS, Jin YT, Chun HJ, Lee HS, Lee SW, Choi JH, Kim CD, Hyun JH. The prognosis of liver cirrhosis in recent years in Korea. J Korean Med Sci. 2003;18:833–841. doi: 10.3346/jkms.2003.18.6.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luca A, Garcia-Pagan JC, Bosch J, Feu F, Caballeria J, Groszmann RJ, Rodes J. Effects of ethanol consumption on hepatic hemodynamics in patients with alcoholic cirrhosis. Gastroenterology. 1997;112:1284–1289. doi: 10.1016/s0016-5085(97)70142-2. [DOI] [PubMed] [Google Scholar]
- 23.Oshita M, Takei Y, Kawano S, Yoshihara H, Hijioka T, Fukui H, Goto M, Masuda E, Nishimura Y, Fusamoto H, Kamada T. Roles of endothelin-1 and nitric oxide in the mechanism for ethanol-induced vasoconstriction in rat liver. J Clin Invest. 1993;91:1337–1342. doi: 10.1172/JCI116334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heresbach D, Jacquelinet C, Nouel O, Chaperon J, Bretagne JF, Gosselin M. Sclerotherapy versus ligation in hemorrhage caused by rupture of esophageal varices. Direct meta-analysis of randomized trials. Gastroenterol Clin Biol. 1995;19:914–920. [PubMed] [Google Scholar]
- 25.Burroughs AK, Jenkins WJ, Sherlock S, Dunk A, Walt RP, Osuafor TO, Mackie S, Dick R. Controlled trial of propranolol for the prevention of recurrent variceal hemorrhage in patients with cirrhosis. N Engl J Med. 1983;309:1539–1542. doi: 10.1056/NEJM198312223092502. [DOI] [PubMed] [Google Scholar]
- 26.Garden OJ, Mills PR, Birnie GG, Murray GD, Carter DC. Propranolol in the prevention of recurrent variceal hemorrhage in cirrhotic patients. A controlled trial. Gastroenterology. 1990;98:185–190. doi: 10.1016/0016-5085(90)91308-s. [DOI] [PubMed] [Google Scholar]
- 27.Bernard B, Lebrec D, Mathurin P, Opolon P, Poynard T. Beta-adrenergic antagonists in the prevention of gastrointestinal rebleeding in patients with cirrhosis: a meta-analysis. Hepatology. 1997;25:63–70. doi: 10.1053/jhep.1997.v25.pm0008985266. [DOI] [PubMed] [Google Scholar]
- 28.Sarin SK, Wadhawan M, Gupta R, Shahi H. Evaluation of endoscopic variceal ligation (EVL) versus propanolol plus isosorbide mononitrate/nadolol (ISMN) in the prevention of variceal rebleeding: comparison of cirrhotic and noncirrhotic patients. Dig Dis Sci. 2005;50:1538–1547. doi: 10.1007/s10620-005-2877-1. [DOI] [PubMed] [Google Scholar]
- 29.Poynard T, Cales P, Pasta L, Ideo G, Pascal JP, Pagliaro L, Lebrec D. Beta-adrenergic-antagonist drugs in the prevention of gastrointestinal bleeding in patients with cirrhosis and esophageal varices. An analysis of data and prognostic factors in 589 patients from four randomized clinical trials. Franco-Italian Multicenter Study Group. N Engl J Med. 1991;324:1532–1538. doi: 10.1056/NEJM199105303242202. [DOI] [PubMed] [Google Scholar]