Abstract
The aim of this study was to identify factors that predict morbidity and mortality in patients with traumatic pancreatic injuries. A retrospective review was performed on 75 consecutive patients with traumatic pancreatic injuries admitted to the Emergency Medical Center at Masan Samsung Hospital and subsequently underwent laparotomy during the period January 2000 to December 2005. Overall mortality and morbidity rates were 13.3% and 49.3%, respectively. A multivariate regression analysis revealed that greater than 12 blood transfusions and an initial base deficit of less than -11 mM/L were the most important predictors of mortality (p<0.05). On the other hand, the most important predictors of morbidity were surgical complexity and an initial base deficit of less than -5.8 mM/L (p<0.01). These data suggests that early efforts to prevent shock and rapidly control of bleeding are most likely to improve the outcome in patients with traumatic pancreatic injuries. The severity of pancreatic injury per se influenced only morbidity.
Keywords: Pancreas, Injuries, Morbidity, Mortality
INTRODUCTION
Despite the increase in the incidence of abdominal trauma caused by traffic accidents, traumatic pancreatic injury is relatively uncommon. Pancreatic injuries occur in only 0.2% to 4% of all abdominal injuries (1-5). However, morbidity and mortality rates associated with injuries to the pancreas approach 40% and 19%, respectively (2), and these high rates are attributed to difficulties with initial assessment, establishment of diagnosis, and occasionally treatment. The spectrum of pancreatic injury is broad and ranges from simple contusion, fracture, and laceration to complete disruption of the pancreatic duct and parenchyma. Moreover, the diagnosis of blunt abdominal injuries, especially in cases of isolated pancreatic injury, can be extremely difficult, because retroperitoneal lesions do not have any specific symptoms. Another cause of elevated morbidity and mortality is the missing or underestimation of pancreatic lesions during exploration of the abdomen. The purpose of this study was to identify predictors of morbidity and mortality in patients with traumatic pancreatic injuries.
MATERIALS AND METHODS
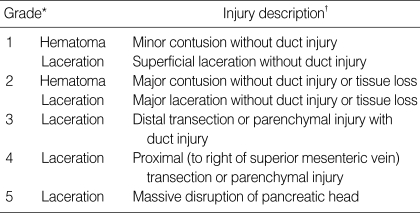
This was a retrospective study of the medical records of 75 consecutive patients with a pancreatic injury who underwent laparotomy at the Emergency Medical Center, Masan Samsung Hospital from January 2000 to December 2005. Medical records were reviewed for the following parameters: demographic data, mechanism of injury, accident to surgical operation time, initial systolic blood pressure (SBP), initial heart rate, initial base deficit, initial amylase, initial Glasgow Coma Scale (GCS), revised trauma score (RTS), number of abbreviated injury scales (AIS), injury severity score (ISS), number of associated injuries (head, colon, stomach, small bowel, abdominal vessel, etc.), grade of pancreatic injury, method of surgical operation, amount of blood transfusion, mortality, morbidity, and others. Pancreatic injuries were graded according to the pancreatic organ injury scale proposed by the Organ Injury Scaling Committee of the American Association for the Surgery of Trauma (AAST), as shown in Table 1 (6). For the purpose of data analysis, postoperative morbidity was subdivided into three groups, i.e., pancreatic complications, non-pancreatic abdominal complications, and intensive care unit (ICU) complications. Pancreatic complications included pancreatic fistula, pseudocyst, and pancreatitis. Abdominal complications included intra-abdominal abscess, enterocutaneous fistulas, and wound infections. ICU complications included acute respiratory distress syndrome, pneumonia, renal failure, and multiple organ failure.
Table 1.
Pancreatic organ injury scale by the American Association for the Surgery of Trauma
*Advance one grade for multiple injuries to the same organ; †based on most accurate assessment at autopsy, laparotomy, or radiologic study from J Trauma 30: 1427, 1990.
Data were analyzed using SPSS (SPSS 11.5 version, SPSS Inc., Chicago, IL, U.S.A.) and MedCalc (MedCalc 7.2 version, MedCalc Inc., Mariakerke, Belgium). A univariate analysis was performed using the Student's t test or by one-way analysis of variance for continuous variables, or by using the χ2 test for categorical variables. Using receiver operating characteristic curve analysis, the cut-off point that best divided each significant continuous or polychotomous variable into two subgroups was determined to minimize false negative and false positive results. This variable was transformed into a dichotomous variable based on the cut-off point. All variables found to be significant by the univariate analysis were then analyzed by a multivariate logistic regression analysis. Statistical significance was accepted at the p<0.05 level.
RESULTS
The demographic data revealed a male predominance (72.0%) and a young age (37.9±15.8). Blunt trauma was the predominant mechanism of injury and accounted for 92.0% of injuries. Traffic accident wounds were the most common injuries and accounted for 65.3%, fall-down wounds accounted for 14.7%, and compression wounds for 4.0%. The remaining patients (8.0%) suffered from stab injury. Mechanisms of injury were not associated with mortality or morbidity by univariate analysis (Table 2).
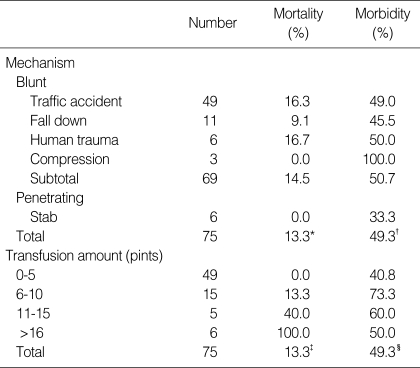
Table 2.
Outcomes by mechanism of injury and transfusion requirement
Data are expressed as numbers or percentiles.
*,†,§Non-significant. ‡p< 0.001.
The most frequent site of pancreatic injury was the head (including neck) in 21 patients (28.0%). Both pancreatic body and tail were injured equally in 18 cases (24.0%). Multiple sites were injured in 18 patients (24.0%). Sites of pancreatic injury were not found to be associated with mortality or morbidity by univariate analysis.
Grade 2 pancreatic injuries were most frequent and accounted for 42.7%. Grade 3 accounted for 36.0%, grade 4 for 10.7%, grade 1 for 8.0%, and grade 5 for 2.7% of patients, and higher grades of pancreatic injury were associated with poorer outcomes (p<0.05, Table 3). Based on only main pancreatic duct status, grades of pancreatic injury were divided into two groups: injury grades 1 and 2 were allocated to group 1, and grades 3 to 5 to group 2. The mortality rates of these two groups were 7.9% and 18.9%, respectively, which were not significantly different, but morbidity rates in these two groups were 34.2% and 64.9%, respectively, and these were significantly different (p=0.008). Another grouping was performed based on both site and ductal status of injured pancreas. One of these groups included injury grades 1 to 3, and the other grades 4 and 5. Mortality rates in these two groups were 9.2% and 40.0%, respectively, and these were significantly different (p=0.008). However, morbidity rates in these two groups were 46.2% and 70.0%, respectively, which were not significantly different.
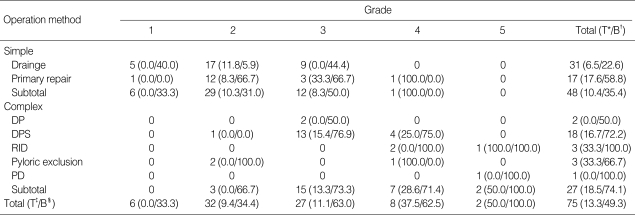
Table 3.
Outcomes by grade and operation method of pancreatic injury
Data are expressed as frequencies or percentiles. Numbers in parentheses indicate mortality/morbidity. χ2 test for trend to compare grade and operation method of pancreatic injury reveals significant (p<0.01).
*Non-significant; †p<0.01; ‡,§p<0.05; ‡,§analyzed by χ2 test for trend.
T, mortality; B, morbidity; DP, distal pancreatectomy; DPS, distal pancreatectomy with splenectomy; RID, resection with internal drainage; PD, pancreaticoduodenectomy.
Simple surgical operations such as drainage and primary repair were performed more often for pancreatic injuries than more complex surgical operations, such as pancreatectomy, resection with internal drainage, pyloric exclusion, and pancreaticoduodenectomy. Forty-eight patients (64.0%) underwent drainage and primary repair, and 20 patients (26.7%) underwent distal pancreatectomy. Of the remaining seven patients, resection with internal drainage or pyloric exclusion was performed equally, i.e., both in 4.0% of patients. Pancreaticoduodenectomy was performed only in one patient, and this patient survived. The majority (72.9%) of patients who had undergone simple surgical operations had a low grade (1 or 2) pancreatic injury, and 88.9% of patients who had undergone complex surgical operations had a high grade (3 to 5). The method of initial surgical management was found to be associated with the grade of pancreatic injury (p<0.001), but the correlation was not strong (r=0.566, p< 0.001). There was no association between the surgical method and mortality, but there was an association with morbidity (p<0.01, Table 3).
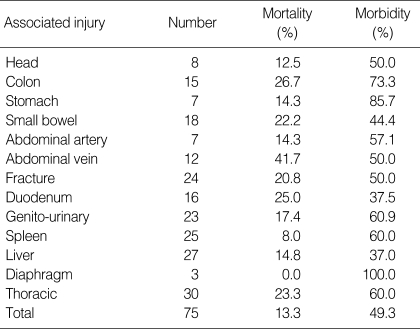
Associated injuries were common, with a mean of 3.7±2.1 organs injured, ranging from isolated pancreatic wounds to nine organs injured. The liver was the most commonly injured organ, seen in 36% of patients. Other commonly injured organs included spleen (33.3%), bone (32.0%), genitourinary organ (30.7%), small bowel (24.0%), and duodenum (21.3%). Associated major abdominal venous injuries were observed in 16% of patients (Table 4). The superior mesenteric veins, portal vein, and inferior vena cava accounted for most of these injuries.
Table 4.
Outcomes by associated injury
Data are expressed as numbers or percentiles.
Blood transfusions were frequently required in the 62 patients (82.7%). Only 13 patients (17.3%) did not require a blood transfusion. Thirty-six patients (48.0%) required five or less units of packed red blood cells, and the others (34.7%) required six or more units of packed red blood cells; sixteen or more units of packed red blood cells were required in 8% of patients (Table 2). Higher blood transfusion quantities were related to higher mortality rates (p<0.001).
The mean base deficit was -7.0±5.4 mM/L in all patients, and mean base deficits in patients who survived or succumbed were -5.8±4.3 mM/L and -15.3±4.4 mM/L, respectively, and the mean base deficits of patients with or without a complication were -8.4±5.3 mM/L or -5.7±5.2 mM/L, respectively. Mean base deficits of patients who survived or did not have a complication were higher than those who died or had a complication, respectively (p<0.05).
Mean ISS in all patients was 27.2±15.1, and mean ISS in patients who succumbed (50.8±15.7) was higher than in patients who survived (23.6±11.3, p<0.001), and mean ISS in patients with one or more complications (31.8±13.3) was higher than in patients without a complication (22.7± 15.5, p<0.01).
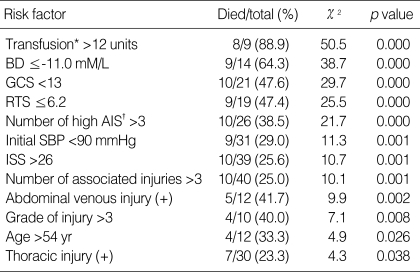
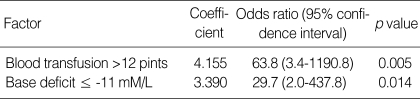
The overall mortality rate in our patient population was 13.3%. Thirty-eight independent factors were evaluated for an association with mortality. Of these, twelve were revealed to be significantly associated with mortality by univariate analysis (Table 5). These factors were a blood transfusion of >12 units, a base deficit of ≤-11.0 mM/L, GCS <13, RTS ≤6.2, four or more number with high AIS (4 or 5) , an initial SBP of <90 mmHg, an ISS of >26, four or more associated injuries, abdominal venous injury, high grade pancreatic injury, old age, and thoracic injury. Multivariate analysis revealed that a blood transfusion of >12 units and a base deficit of ≤-11.0 mM/L were most significantly correlated with mortality (Table 6).
Table 5.
Univariate analyses of factors associated with mortality
*Blood transfusion only; †number of all AIS more than three (4 or 5).
BD, base deficit; GCS, Glasgow coma scale; RTS, revised trauma score; AIS, abbreviated injury scale; SBP, systolic blood pressure; ISS, injury severity score.
Table 6.
Multivariate analysis of factors associated with mortality
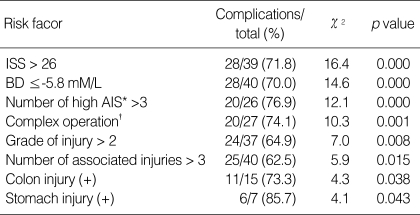
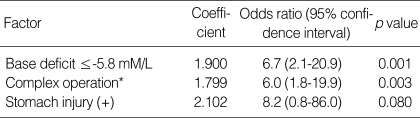
The overall morbidity rate of the 75 patients was 49.3%. Fourteen patients (18.7%) had a pancreatic complication, and intra-abdominal and ICU complications both accounted for 18 patients (24.0%). Univariate analysis revealed that eight factors were significantly associated with morbidity, namely, an ISS of >26, a base deficit of ≤-5.8 mM/L, four or more number with high AIS (4 or 5), surgical complexity, high-grade pancreatic injury, four or more associated injuries, colon injury, and stomach injury (Table 7). However, multivariate analysis revealed that a base deficit of ≤-5.8 mM/L and surgical complexity were most significantly correlated with morbidity (Table 8).
Table 7.
Univariate analyses of factors associated with morbidity
*Number of all AIS more than three (4 or 5); †included distal pancreatectomy with or without splenectomy, resection with internal drainage, pyloric exclusion, and pancreaticoduodenectomy, but excluded drainage and primary repair.
ISS, injury severity score; BD, base deficit; AIS, abbreviated injury scale.
Table 8.
Multivariate analysis of factors associated with morbidity
*Included distal pancreatectomy with or without splenectomy, resection with internal drainage, pyloric exclusion, and pancreaticoduodenectomy, but excluded drainage and primary repair.
DISCUSSION
Although the pancreas remains one of the least frequently injured organs in cases of abdominal trauma, its location and the fact that it is surrounded by vital structures means that pancreatic injuries often present complicated diagnostic and treatment problems. Frequencies of pancreatic injuries are related to the geographic settings of the traumatic incidents (i.e., urban or rural). In the U.S.A., penetrating trauma accounts for 70% of all pancreatic injuries, and blunt trauma accounts for the remaining 30% (3, 7, 8). However, in our series, 92% of all pancreatic injuries were caused by blunt trauma and the remaining 8% by penetrating trauma. The mechanism of wounding in cases of penetrating trauma is simple violation by a sharp object (i.e., a knife blade). However, the kinematics are considerably more complex for blunt injury. The pancreas has a relatively fixed retroperitoneal position anterior to the spine, and thus, forcible compression of the pancreas against the vertebral column resulting from blunt trauma is the most common mechanism of blunt pancreatic injury.
By multivariate analysis, the grade of pancreatic injury was not associated with morbidity or mortality in our patient population. Generally, the status of the main pancreatic duct is an important predictor of outcome, and knowledge of its status is essential for establishing a basis for treatment decisions in cases of pancreatic injury (1-3, 8-10). Bradley et al. (9) reported a significant association between main pancreatic ductal injury and an increased incidence of pancreas-related complications, particularly, with an increased incidence of pancreatic fistula. Kao et al. (1) reported that the grade of pancreatic injury was an independent predictor of both pancreatic complications and mortality. However, their study did not include the important factors of the patients' outcome, such as, amount of blood transfusion, base deficit, GCS, and RTS. In this study, univariate analysis revealed these parameters were strong significant predictors of mortality. In the present study, grade 1 and 2 pancreatic injuries (no ductal injuries) were usually treated by closed drainage with or without local debridement and pancreatorrhaphy, which is the most commonly adopted procedure, and this approach proved to be safe and effective (11, 12). Fabian et al. (11) reported on the superiority of closed-suction drainage for the treatment of pancreatic trauma in a randomized prospective study, and we also prefer and widely use this modality. Grade 3 injuries in the present series were treated commonly by distal pancreatectomy. The integrity of the pancreatic duct has been suggested to be an important factor for determining the method of treatment (13), whereas for grade 4 injuries, multiple procedures, such as closed suction drainage and distal resection, could be selected, depending on the clinical condition. Moreover, when resecting more than 80% of pancreatic parenchyma with associated diabetes mellitus, one should consider preservation of the distal pancreas and internal drainage by Roux-en-Y jejunal anastomosis. Pyloric exclusion has been suggested as a valuable means of treating severe duodenal injuries, and of reducing the postoperative leakage rate, and pyloric exclusion has also been considered as a viable option for grade 4-5 pancreatic injuries associated with duodenal injuries (14). Grade 5 injuries characterized by massive devascularization of the pancreatic head and adjacent duodenum are infrequent and usually require pancreaticoduodenectomy. As mentioned above, the selection of the surgical method depends primarily on the grade of pancreatic injury. However, other clinical conditions such as the site of the pancreatic injury, the characteristics and severity of the associated injuries, and the physiological status of the patient can also affect the decision. Therefore, the surgical method appears to better reflect the general pathophysiological condition of the patient than the grade of pancreatic injury. This explains why univariate analysis revealed both the grade of pancreatic injury and the surgical complexity were associated with morbidity. However, multivariate analysis revealed only the surgical complexity was a better predictor for morbidity.
In the present study, associated injuries were very common, with a mean of 3.7±2.1 organs injured per patient. The liver was most frequently injured, and this was observed in 36% of our patients, which is consistent with the findings of other authors (2-5). Moreover, associated major abdominal venous injuries were found to correlate with mortality by univariate analysis, but were not found to significantly predict mortality by multivariate analysis. Likewise, associated colon and stomach injuries were found to correlate with increased morbidity by univariate analysis, but this relation was not substantiated by multivariate analysis.
Base deficit has been shown to be an excellent predictor of transfusion requirement, shock-related complications, and mortality (15, 16). As base deficit reduced, both mortality and morbidity increased in our study, whereas transfusion requirement was associated with mortality only. The present report is the first to show that base deficit and transfusion requirement are predictors of mortality in patients with a traumatic pancreatic injury. This finding demonstrates that not only is the physiologic presentation of a patient important, but that efforts to rapidly control ongoing hemorrhage may also significantly improve the patient outcome.
Although the small number of subjects limits our conclusions, the data suggest that early efforts to prevent shock and rapidly control of bleeding are most likely to reduce the mortality rates in patients with a traumatic pancreatic injury.
Footnotes
This study was supported by Hyoseok Research fund.
References
- 1.Kao LS, Bulger EM, Parks DL, Byrd GF, Jurkovich GJ. Predictors of morbidity after traumatic pancreatic injury. J Trauma. 2003;55:898–905. doi: 10.1097/01.TA.0000090755.07769.4C. [DOI] [PubMed] [Google Scholar]
- 2.Mayer JM, Tomczak R, Rau B, Gebhard F, Beger HG. Pancreatic injury in severe trauma: early diagnosis and therapy improve the outcome. Dig Surg. 2002;19:291–297. doi: 10.1159/000064576. [DOI] [PubMed] [Google Scholar]
- 3.Asensio JA, Demetriades D, Hanpeter DE, Gambaro E, Chahwan S. Management of pancreatic injuries. Curr Probl Surg. 1999;36:325–419. doi: 10.1016/s0011-3840(99)80003-3. [DOI] [PubMed] [Google Scholar]
- 4.Akhrass R, Yaffe MB, Brandt CP, Reigle M, Fallon WF, Malangoni MA. Pancreatic trauma: a ten-year multi-institutional experience. Am Surg. 1997;63:598–604. [PubMed] [Google Scholar]
- 5.Timberlake GA. Blunt pancreatic trauma: experience at a rural referral center. Am Surg. 1997;63:282–286. [PubMed] [Google Scholar]
- 6.Moore EE, Cogbill TH, Malangoni MA, Jurkovich GJ, Champion HR, Gennarelli TA, Mcaninch JW, Pachter HL, Shackford SR, Trafton PG. Organ injury scaling, II: pancreas, duodenum, small bowel, colon, and rectum. J Trauma. 1990;30:1427–1429. [PubMed] [Google Scholar]
- 7.Farrell RJ, Krige JE, Bornman PC, Knottenbelt JD, Terblanche J. Operative strategies in pancreatic trauma. Br J Surg. 1996;83:934–937. doi: 10.1002/bjs.1800830715. [DOI] [PubMed] [Google Scholar]
- 8.Patton JH, Jr, Lyden SP, Croce MA, Pritchard FE, Minard G, Kudsk KA, Fabian TC. Pancreatic trauma: a simplified management guideline. J Trauma. 1997;43:234–239. doi: 10.1097/00005373-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Bradley EL, 3rd, Young PR, Jr, Chang MC, Allen JE, Baker CC, Meredith W, Reed L, Thomason M. Diagnosis and initial management of blunt pancreatic trauma: guidelines from a multiinstitutional review. Ann Surg. 1998;227:861–869. doi: 10.1097/00000658-199806000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lin BC, Chen RJ, Fang JF, Hsu YP, Kao YC, Kao JL. Management of blunt major pancreatic injury. J Trauma. 2004;56:774–778. doi: 10.1097/01.ta.0000087644.90727.df. [DOI] [PubMed] [Google Scholar]
- 11.Fabian TC, Kudsk KA, Croce MA, Payne LW, Mangiante E, Voeller GR, Britt LG. Superiority of closed suction drainage for pancreatic trauma. Ann Surg. 1990;211:724–728. doi: 10.1097/00000658-199006000-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Madiba TE, Mokoena TR. Favourable prognosis after surgical drainage of gunshot, stab or blunt trauma of the pancreas. Br J Surg. 1995;82:1236–1239. doi: 10.1002/bjs.1800820926. [DOI] [PubMed] [Google Scholar]
- 13.Smego DR, Richardson JD, Flint LM. Determinants of outcome in pancreatic trauma. J Trauma. 1985;25:771–776. doi: 10.1097/00005373-198508000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Degiannis E, Krawczykowski D, Velmahos GC, Levy RD, Souter I, Saadia R. Pyloric exclusion in severe penetrating injuries of the duodenum. World J Surg. 1993;17:751–754. doi: 10.1007/BF01659085. [DOI] [PubMed] [Google Scholar]
- 15.Davis JW, Parks SN, Kaups KL, Gladen HE, O'Donnell-Nicol S. Admission base deficit predicts transfusion requirements and risk of complications. J Trauma. 1996;41:769–774. doi: 10.1097/00005373-199611000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Davis JW, Kaups KL, Parks SN. Base deficit is superior to pH in evaluating clearance of acidosis after traumatic shock. J Trauma. 1998;44:114–118. doi: 10.1097/00005373-199801000-00014. [DOI] [PubMed] [Google Scholar]