Abstract
Elevated intraocular pressure (IOP) is one of the major risk factors for glaucomatous visual field defects. Each individual systemic risk factor of coronary heart disease (CHD) is associated with elevated IOP, although no reports have argued for a correlation between the risk factors for CHD and IOP after a comprehensive or collective analysis. The National Cholesterol Education Program Adult Treatment Panel III presented the Framingham projection, which can predict the risk of CHD quantitatively. We investigated the association between IOP and the Framingham projection in 16,383 Korean subjects. The Framingham projection was applied using the indicated risk factors. The associations between the Framingham projection and IOP and the influences of the risk factors on the IOP were examined. The Framingham projection was correlated with the mean IOP in women (p<0.05). The relationship between IOP and systemic variables other than smoking was significant (p<0.05). The mean IOP was significantly higher in the high-risk CHD group than in the low-risk group based on the Framingham projection (p<0.05). Because an elevated IOP was associated with cardiovascular risk factors, subjects with a high CHD risk based on the Framingham projection need continuous monitoring for IOP to prevent glaucomatous visual field defects.
Keywords: Coronary Disease, Intraocular Pressure, Koreans, Cholesterol, Low-Density Lipoprotein
INTRODUCTION
Elevated intraocular pressure (IOP) is one of the major risk nfactors for glaucomatous visual field defects. In addition, it is associated with various systemic diseases and indices (1-6). Each systemic risk factor of coronary heart disease (CHD) has been associated with an elevated IOP, including hypertension, male gender, a high body mass index (BMI), and hyperlipidemia (7, 8). However, no reports have argued for a correlation between the risk factors for CHD including smoking, low-density lipoprotein (LDL)-cholesterol, and triglyceride and IOP after a comprehensive or collective analysis. The National Cholesterol Education Program Adult Treatment Panel III (NCEP ATP III) developed the Framingham projection, which can predict the risk of CHD quantitatively. The Framingham projection is an index that predicts the probability of having a CHD event within 10 yr. No reports have analyzed the relationship between IOP and the Framingham projection, which incorporates all the risk factors for CHD (2, 5, 7, 9). Therefore, we investigated the association between IOP and cardiovascular risk factors and between IOP and the Framingham projection in 16,383 Korean subjects.
MATERIALS AND METHODS
The study subjects were 16,383 adults from 20 to 79 yr old who visited the Health Promotion Center of Asan Medical Center from July to December of 2001. There were 9,795 men and 6,588 women. The mean age of the men and women was 46.5 and 46.1 yr, respectively. Sixty-five percent of the subjects lived in Seoul and had regular check-ups and subsequent consultations concerning diet and exercise if needed. The body mass index (BMI=weight divided by the height squared), blood pressure, smoking history, total cholesterol, triglycerides, high-density lipoprotein (HDL)-cholesterol, LDL-cholesterol, and high sensitive C-reactive protein (hs-CRP) were measured. Blood samples were taken in the morning after fasting for more than 9 hr. The serum total cholesterol, triglyceride, and HDL-cholesterol concentrations were measured using enzymatic methods on a Hitachi 747-200 (Hitachi, Tokyo, Japan). The serum LDL-cholesterol concentration was calculated using the Friedewald formula (10). The hs-CRP concentration was measured using immunoturbidimetry on a Cobas Integra 800 (Roche Diagnostic System, Basel, Switzerland). Applying the Framingham projection, the 10-yr absolute CHD risk (i.e., the percent probability of having a CHD event within 10 yr) was calculated using age, total cholesterol, cigarette smoking, HDL-cholesterol, and systolic blood pressure. The IOP was determined as the mean value of the readings for both eyes using a non-contact tonometer (T-2, Canon, Tokyo, Japan) between 9 and 11 a.m.
Statistics
Student's t-test was used to determine the statistical difference between men and women in the mean of each factor. Parametric correlation analyses were used to analyze the statistical significance between the Framingham projection and IOP and between each risk factor and IOP in both men and women. After correcting for the other risk factors, stepwise multiple linear regressions were performed to determine if each risk factor affected the mean IOP independently. The mean IOP was compared between the high- (10-yr risk > 20%) and low-risk (10-yr risk ≤ 20%) CHD groups based on the Framingham projection. The software SPSS (version 11.0, SPSS Inc., Chicago, IL, U.S.A.) was used for the statistical analyses.
RESULTS
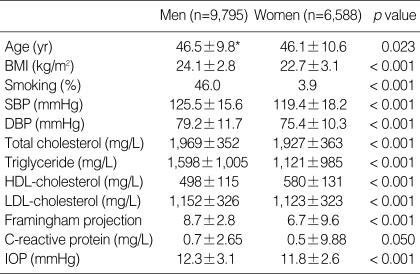
Comparison of IOP and the Framingham projection between men and women
The mean IOP (men 12.3±3.1 mmHg, women 11.8±2.6 mmHg) and the Framingham projection (men 8.7±4.8, women 6.7±6.6) were significantly higher in men than in women (p < 0.05). Men were significantly older, smoked more, and had higher systolic blood pressure, triglycerides, LDL-cholesterol, total cholesterol, and hs-CRP than women, and significantly lower HDL-cholesterol (p < 0.05; Table 1).
Table 1.
The mean and standard deviation of risk factors in men and women
*Mean±standard deviation.
BMI, body mass index (weight divided by height squared); SBP, systolic blood pressure; DBP, diastolic blood pressure; HDL-cholesterol, high-density lipoprotein cholesterol; LDL-cholesterol, low-density lipoprotein cholesterol; IOP, intraocular pressure.
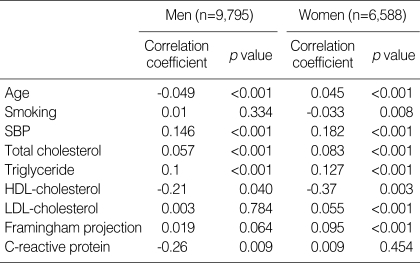
Correlation between IOP and other parameters
In men, the mean IOP had significant negative correlations with age, HDL-cholesterol, and hs-CRP and positive correlations with systolic blood pressure, total cholesterol, and triglycerides (p < 0.05). Nevertheless, the mean IOP was not significantly correlated with the Framingham projection. In women, the mean IOP had significant negative correlations with smoking and HDL-cholesterol and positive correlations with age, systolic blood pressure, total cholesterol, triglycerides, and LDL-cholesterol (p < 0.05). Moreover, the mean IOP had a significant positive correlation with the Framingham projection (p < 0.05; Table 2).
Table 2.
Univariate tests for correlation of each parameter with intraocular pressure
SBP, systolic blood pressure; HDL-cholesterol, high-density lipoprotein cholesterol; LDL-cholesterol, low-density lipoprotein cholesterol.
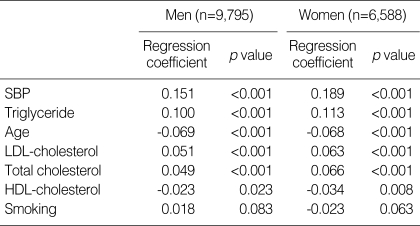
Stepwise multiple regression for correlated factors
After correcting for the other risk factors in men and women, the following were independent risk factors that were related to an elevated IOP in descending order: in men, increased systolic blood pressure, triglycerides, LDL-cholesterol, and total cholesterol, decreased HDL-cholesterol, and age (p < 0.05); in women, increased systolic blood pressure, triglycerides, total cholesterol, and LDL-cholesterol, decreased HDL-cholesterol, and age (p < 0.05; Table 3). In both men and women, the mean IOP of the high-risk CHD group (men 12.7 mmHg, women 13.7 mmHg) was higher than that of the low-risk CHD group (men 12.2 mmHg, women 11.8 mmHg; p < 0.05).
Table 3.
Stepwise multiple regression analysis with intraocular pressure as a dependent variable in men and women
SBP, systolic blood pressure; HDL-cholesterol, high-density lipoprotein cholesterol; LDL-cholesterol, low-density lipoprotein cholesterol.
DISCUSSION
The mean IOP in men (12.3±3.1 mmHg) was higher than that in women (11.8±2.6 mmHg), which agreed with previous reports for Korea (11, 12). This was because the increases in systolic blood pressure, total cholesterol, triglycerides, and LDL-cholesterol and the decrease in HDL-cholesterol, which were factors that influenced the IOP, were much more prominent in men than in women. In contrast, some studies involving other ethnic groups found that the mean IOP in women was higher than that in men (13).
After correcting for all systemic health parameters, the mean IOP decreased as age increased in both sexes, which was consistent with previous reports for Korea and Japan (7, 11). By contrast, in Westerners, even after this correction, the IOP increased with age (13). Ethnic differences may arise because as Orientals grow older, they are less prone to increases in blood pressure, blood lipid concentrations, and obesity than are Westerners. Age had a less effect on the Framingham projections than the other risk factors. The mean IOP in the high-risk CHD group based on the Framingham projections was higher than that of the low-risk group.
Of the risk factors contributing to the Framingham projection, i.e., age, total cholesterol, cigarette smoking, HDL-cholesterol, and systolic blood pressure (BP), the increase in systolic BP had the greatest independent relation to elevated IOP. The association between the increase in the systolic BP and the elevated IOP agreed with previous reports (8, 9). High BP increases the pressure in the ciliary artery and the ultrafiltration component leading to formation of the aqueous humor, thereby increasing the IOP.
We could find a significant association between diabetes, which is not included in the Framingham projection, and elevated IOP (diabetic group [n=2,053]: 12.3±3.2 mmHg, non-diabetic group [n=14,330]: 12.0±2.9 mmHg, p < 0.05). This is consistent with a previous report that diabetes was related with an elevation in IOP (5).
Most of the previous studies used only total cholesterol as the serum lipid marker (14), and some could not show a direct association with an elevated IOP (9). Of the lipid markers, triglycerides, not a component of the Framingham projection, had the greatest relation with the elevated IOP based on the regression coefficients. In addition to total cholesterol and HDL-cholesterol, both of which contribute to the Framingham projection, LDL-cholesterol and triglycerides were independent risk factors of an elevated IOP. These prominent findings strongly support the role of the serum lipid markers in IOP elevation. The increase in blood viscosity and decrease in outflow channel capacity due to hyperlipidemia contribute to the elevation in IOP. We added LDL-cholesterol and triglycerides, CHD risk factors emphasized by NCEPATP III, to the Framingham projection to make a new predictor for IOP elevation.
An increase in total cholesterol and decrease in HDL-cholesterol are high-risk CHD factors that increased the Framingham projection and were both independent risk factors for increasing IOP. Several reports support our results in that hyperlipidemia, which is strongly related to obesity and an increased BMI, was associated with elevated IOP (11, 14).
We could not find any direct significant association between smoking and elevated IOP, even after correcting for the other risk factors. This contrasts with a previous report that smoking was associated with an elevation in IOP, but those studies did not correct for other risk factors and the mechanism of IOP elevation is still not clear (2, 15, 16). Although the Framingham projection includes smoking as one of the main risk factors of CHD, smoking had little relation to IOP elevation.
The mean IOP was significantly higher in the high-risk CHD group (men 12.7 mmHg and women 13.7 mmHg) than in the low-risk CHD group (men 12.2 mmHg and women 11.8 mmHg), when the risk of CHD was based on the Framingham projection. The high-risk CHD group was defined as a 10-yr risk of over 20%, i.e., the Framingham projection was over 16 points in men and over 23 points in women. In terms of systemic parameters that describe or reflect elevation in IOP, the Framingham projection, a major predictor of CHD, best predicted elevation in IOP. In particular, the increase in the Framingham projection due to the increased systolic BP and total cholesterol and decreased HDL-cholesterol best reflects the elevation in IOP. Therefore, we recommend that these parameters be monitored along with regular IOP measurements.
In conclusion, elevated IOP is associated with cardiovascular risk factors. Young age, high systolic BP, total cholesterol, triglycerides, LDL-cholesterol, and low HDL-cholesterol were independent risk factors for elevation in IOP. Therefore, subjects with a high risk of CHD based on the Framingham projection need continuous monitoring for IOP to prevent glaucomatous visual field defects.
References
- 1.Sommer A. Intraocular pressure and glaucoma. Am J Ophthalmol. 1989;107:186–188. doi: 10.1016/0002-9394(89)90221-3. [DOI] [PubMed] [Google Scholar]
- 2.Carel RS, Korczyn AD, Rock M, Goya I. Association between ocular pressure and certain health parameters. Ophthalmology. 1984;91:311–314. doi: 10.1016/s0161-6420(84)34282-8. [DOI] [PubMed] [Google Scholar]
- 3.Kahn HA, Leibowitz HM, Ganley JP, Kini MM, Colton T, Nickerson RS, Dawber TR. The Framingham Eye Study. II. Association of ophthalmic pathology with single variables previously measured in the Framingham Heart Study. Am J Epidemiol. 1977;106:33–41. doi: 10.1093/oxfordjournals.aje.a112429. [DOI] [PubMed] [Google Scholar]
- 4.Wilson MR, Hertzmark E, Walker AM, Childs-Shaw K, Epstein DL. A case-control study of risk factors in open angle glaucoma. Arch Ophthalmol. 1987;105:1066–1071. doi: 10.1001/archopht.1987.01060080068030. [DOI] [PubMed] [Google Scholar]
- 5.Leske MC, Podgor MJ. Intraocular pressure, cardiovascular risk variables, and visual field defects. Am J Epidemiol. 1983;118:280–287. doi: 10.1093/oxfordjournals.aje.a113634. [DOI] [PubMed] [Google Scholar]
- 6.Martin MJ, Sommer A, Gold EB, Diamond EL. Race and primary open-angle glaucoma. Am J Ophthalmol. 1985;99:383–387. doi: 10.1016/0002-9394(85)90001-7. [DOI] [PubMed] [Google Scholar]
- 7.Mori K, Ando F, Nomura H, Sato Y, Shimokata H. Relationship between intraocular pressure and obesity in Japan. Int J Epidemiol. 2000;29:661–666. doi: 10.1093/ije/29.4.661. [DOI] [PubMed] [Google Scholar]
- 8.McLeod SD, West SK, Quigley HA, Fozard JL. A longitudinal study of the relationship between intraocular and blood pressures. Invest Ophthalmol Vis Sci. 1990;31:2361–2366. [PubMed] [Google Scholar]
- 9.Klein BE, Klein R. Intraocular pressure and cardiovascular risk variables. Arch Ophthalmol. 1981;99:837–839. doi: 10.1001/archopht.1981.03930010837009. [DOI] [PubMed] [Google Scholar]
- 10.Stein EA, Myers GL. Tietz textbook of clinical chemistry. 2nd ed. Philadelphia: WB Saunders; 1994. Lipids, Lipoproteins and apolipoproteins; pp. 1002–1094. [Google Scholar]
- 11.Lee JS, Lee SH, Oum BS, Chung JS, Cho BM, Hong JW. Relationship between intraocular pressure and systemic health parameters in a Korean population. Clin Experiment Ophthalmol. 2002;30:237–241. doi: 10.1046/j.1442-9071.2002.00527.x. [DOI] [PubMed] [Google Scholar]
- 12.Jung SC, Choi YR, Lee JS. The Relationship between intraocular pressure and cardiovascular risk factors. J Korean Ophthalmol. 2005;46:1518–1525. [Google Scholar]
- 13.Leske MC, Connell AM, Wu SY, Hyman L, Schachat AP. Distribution of intraocular pressure. The Barbados Eye Study. Arch Ophthalmol. 1997;115:1051–1057. doi: 10.1001/archopht.1997.01100160221012. [DOI] [PubMed] [Google Scholar]
- 14.Klein BE, Klein R, Linton KL. Intraocular pressure in an American community. The Beaver Dam Eye Study. Invest Ophthalmol Vis Sci. 1992;33:2224–2228. [PubMed] [Google Scholar]
- 15.Wu SY, Leske MC. Associations with intraocular pressure in the Barbados Eye Study. Arch Ophthalmol. 1997;115:1572–1576. doi: 10.1001/archopht.1997.01100160742012. [DOI] [PubMed] [Google Scholar]
- 16.Morgan RW, Drance SM. Chronic open-angle glaucoma and ocular hypertension. An epidemiological study. Br J Ophthalmol. 1975;59:211–215. doi: 10.1136/bjo.59.4.211. [DOI] [PMC free article] [PubMed] [Google Scholar]