Abstract
A vibrating dental local anesthesia attachment (Vibraject, LLC, Calif) based on the concept of the gate-control theory has been used in clinical practice. The theoretical advantage of the vibrating needle is that it reduces the injection pain. We evaluated the effectiveness of Vibraject in combination with an electrical injection device. Injections were given into the alveolar mucosa adjacent to the root apex of the maxillary lateral incisor in 10 volunteers. Vibraject was randomly applied to either the left or right side of the injection. No statistically significant decrease in pain scores was found at needle insertion or anesthetic injection. The clinical efficacy of Vibraject remains controversial.
Keywords: Local anesthesia, Injection, Pain, Vibrating needle
A vibrating dental local anesthesia attachment (Vibraject, LLC, Calif) has been introduced in recent years.1 This device was developed on the basis of the gate-control theory,2,3 which states that pain transmission through A-delta and C nociceptive fibers is depressed at the secondary neuronal cell bodies in the dorsal horn if nerve impulses evoked by tactile sensation are simultaneously transmitted through A-beta tactile fibers. It is therefore supposed that vibrating a needle with Vibraject can result in a reduction in injection pain. The instructions for Vibraject indicate that topical anesthesia is generally not required. However, Yoshikawa et al4 reported that injection pain did not decrease when Vibraject was applied with a conventional cartridge type dental syringe with a 30-gauge needle. They suggested that manual injection with these syringes might evoke pain, because relatively strong pressure can be applied even if Vibraject was used in combination. In the present study, we evaluated the injection pain when Vibraject was applied with an automated electric syringe with a 33-gauge dental needle under single-blind randomized conditions.
Methods
Ten healthy adults consented to participate in the present study. The study design met the ethical code of the Tokyo Dental College, and we obtained informed consent from all the volunteers in the study. These volunteers underwent intraoral injections with and without Vibraject application at a sufficient interval. The participants wore eye masks and headphones to create blinded conditions. Intraoral injection was given into the alveolar mucosa adjacent to the root apex of the maxillary lateral incisor using a computer-controlled electric syringe (Anaeject, Nihonshikayakutin, Yamaguchi, Japan) with a 33-gauge needle. Vibraject was randomly applied at either the left or right side of the injection. The Vibraject applied to Anaeject is shown in Figure 1. After patting the participant's shoulder, the investigator inserted the needle approximately 1 mm and maintained this for 10 seconds. Then 0.1 mL of 2% lidocaine that contained 1 : 80,000 epinephrine was injected for 20 seconds. The lowest constant mode injection rate (0.005 mL/s) was used. After the injection was finished, participants evaluated the degree of pain at needle insertion and anesthetic injection on a visual analog scale (VAS; 0–100 mm) and a pain rating score (PRS; painless, pressure sensation, slight pain, painful). Data are given as the mean ± SD. Student's t test for paired sample and Wilcoxon's rank sum test were used for statistical analysis.
Figure 1. Setup for connecting Vibraject to Anaeject.
Results
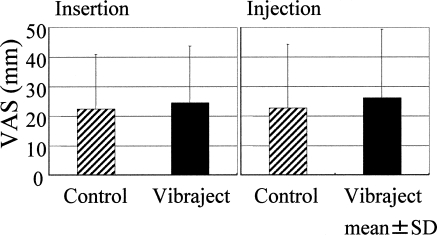
The mean ± SD of the VAS score at needle insertion was 24.6 ± 19.3 mm when Vibraject was used and 22.4 ± 18.6 mm when Vibraject was not used, respectively (P > .05). At anesthetic injection, the mean ± SD of the VAS score was 26.2 ± 23.3 mm when Vibraject was used and 22.7 ± 21.7 mm when Vibraject was not used, respectively (P > .05) (Figure 2).
Figure 2. Pain assessment at needle insertion and anesthetic injection with a visual analog scale. No statistically significant differences occurred between the control and Vibraject groups in either of the 2 conditions.
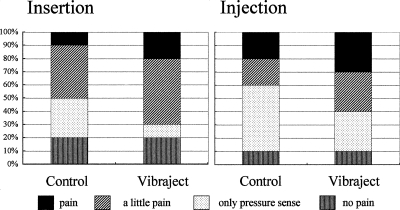
The PRS at needle insertion decreased in 2 participants and increased in 3 participants when applying Vibraject. At anesthetic injection, the PRS increased in 4 participants and decreased in 1 participant when applying Vibraject (Figure 3).
Figure 3. Pain assessment at needle insertion and anesthetic injection with the pain rating score. No statistically significant differences occurred between the control and Vibraject groups in either of the 2 conditions.
Discussion
Regional dental injection without pain, discomfort, or anxiety is important for preventing systemic complications, such as vasovagal syncope or blood pressure elevation. Although improvements in syringes, development of topical anesthesia, and the application of very fine needles5 have been reported in many studies, no conclusive painless injection method has been established.
Vibraject, developed from a new viewpoint, is an interesting device that can be easily applied in routine anesthesia procedures. According to Kakigi and Watanabe,6 interference stimulation such as vibration can relieve pain on the basis of the gate-control theory.2,3 Hutchins et al7 reported that the vibration might be effective in reducing the pain of injection. Blair1 recommended the use of Vibraject for painless injection. In contrast, Yoshikawa et al4 found no significant pain reduction when Vibraject was applied with a conventional dental syringe.
In the present study, the experimental method was improved in 2 points. These points include the use of a computer-controlled electric syringe with the slowest injection rate and a fine 33-gauge needle. However, the present study also failed to detect any pain reduction effects of Vibraject even when the fear of anesthesia equipment evoked by visual and auditory inputs was blocked by eye masks and headphones. Therefore, our pilot study suggests that the effect of Vibraject on pain reduction is insufficient and that topical anesthesia may still be required.
The instructions for Vibraject indicate that the vibration reduces patient discomfort if the patient markedly fears undergoing injection and also state that the hum of the motor seems to have a calming effect. If the injection is performed without blinding after providing sufficient information about the Vibraject, the degree of pain may change. Further studies will be needed to verify whether the vibration and hum of the motor of the Vibraject have calming effects. In conclusion, this pilot study of 10 volunteers suggests that Vibraject does not reduce injection pain when it is applied to a blinded patient using an automated electric syringe with a 33-gauge dental needle.
References
- Blair J. Vibraject from ITL Dental. Dent Econ. 2002;92(12):90. [Google Scholar]
- Melzack R, Wall PD. Pain mechanisms: a new theory. Science. 1965;19:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Melzack R. Recent concepts of pain. J Med. 1982;13:147–160. [PubMed] [Google Scholar]
- Yoshikawa F, Ushito D, Ohe D, Shirasishi Y, Fukayama H, Umino M. Vibrating dental local anesthesia attachment to reduce injection pain. J Jpn Dent Soc Anesthesiol. 2003;31:194–195. [Google Scholar]
- Watanabe T, Koshiba K, Okuda H, et al. Comparison of the pain perception induced by intra oral penetration by a new fine needle and a 30-gauge needle. J Jpn Dent Soc Anes-thesiol. 1995;23:19–30. [Google Scholar]
- Kakigi R, Watanabe S. Pain relief by various kinds of interference stimulation applied to the peripheral skin in humans: pain-related brain potentials following CO2 laser stimulation. J Peripher Nerv Syst. 1996;1:189–198. [PubMed] [Google Scholar]
- Hutchins HS, Jr, Young FA, Lackland DT, Fishburne CP. The effectiveness of topical anesthesia and vibration in alleviating the pain of oral injections. Anesth Prog. 1997;44:87–89. [PMC free article] [PubMed] [Google Scholar]